Prevalence of anemia and associated factors among pregnant
- Slides: 15
Prevalence of anemia and associated factors among pregnant women attending antenatal care at Debre Markos Referral Hospital, Northwest Ethiopia By Moges Wubie Researchers - Haimanot Ayele (MPH in Nutrition) - Moges Wubie (Assis. Professor in TRID) - Fentaw Tadesse (MPH in
Introduction üAnemia is a global public health problem affecting both developed and developing countries. üWorldwide, it is estimated that 58 million women are anemic during pregnancy, of whom 55 million (95. 7%) live in developing countries. üRecent estimates suggest that up to 60% of pregnant women in developing countries may be anemic (WHO, 2008).
Introduction…. ü Even though some researches were done in different areas of the country there is no any documented evidence about the concern in the study area. üIn addition, with in the area there is a habit of walking on bare foot(especially in rural areas) and üOn the contrary the population are high Teff producer. üSo this research assumed to fill this gap.
Objectives v. General objective üTo assess the prevalence of anemia and associated factors among pregnant women attending ANC at DMRH, Northwest Ethiopia, 2015. v Specific objectives üTo determine the prevalence of anemia üTo identify associated factors for anemia
Materials and Method üInstitution based cross-sectional study design was used. üThis study was conducted at DMRH from August to September, 2015. üSource population was all pregnant women who attend at DMRH. üAll pregnant women who came for ANC service in the study period was included, but üMentally ill and those seriously sick was excluded.
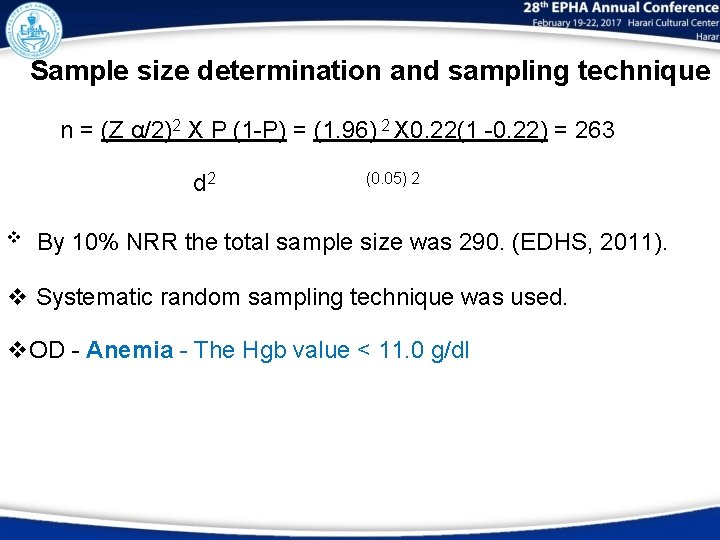
Sample size determination and sampling technique n = (Z α/2)2 X P (1 -P) = (1. 96) 2 X 0. 22(1 -0. 22) = 263 d 2 v (0. 05) 2 By 10% NRR the total sample size was 290. (EDHS, 2011). v Systematic random sampling technique was used. v. OD - Anemia - The Hgb value < 11. 0 g/dl
Data collection procedures üData collection was done by trained Midwifes. ü Sample collection was done by trained laboratory technician. üFor each client, blood sample was collected for complete blood count, HIV test, syphilis, HBSAg, blood film, RBS/FBS. ü Stool sample was collected for examination of intestinal parasitosis.
Data Quality control, Analysis & Ethical clearance üOne day training was given, SOP implemented and filled data were checked every day. üEpi data software version 3. 1 used for data entry and analysis was performed using SPSS Version- 20 software. ü Analysis of variables was made using descriptive statistics and logistic regression at 95% CI and p value < 0. 05. üEthical clearance secured from ECRC of MHSC, DMU.
Result and Discussion üThe mean age was 26 years with SD ± 5 ü 261(90%) were urban residents, ü 251(86. 6%) had habit of wearing shoe. ü 14 (4. 8%) had history of abnormal blood loss. ü 85(29. 3%) were infected with intestinal parasites. ü 10(3. 4%) were positive for HIV status. ü 222 (76. 5%) used Teff as their staple cereal.
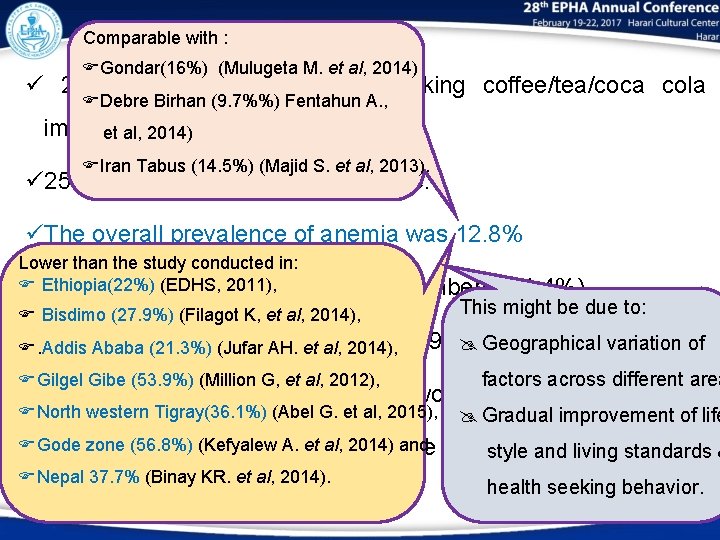
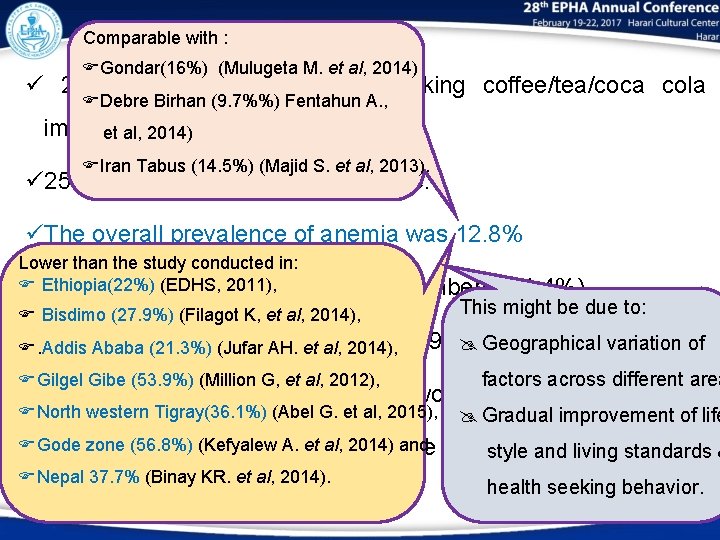
Comparable with : Cont…. Gondar(16%) (Mulugeta M. et al, 2014) ü 237 (81. 7%) had habit of drinking coffee/tea/coca cola Debre Birhan (9. 7%%) Fentahun A. , immediately after meal. et al, 2014) Iran Tabus (14. 5%) (Majid S. et al, 2013). ü 253(87. 2%) had taken iron sulphate. üThe overall prevalence of anemia was 12. 8% Lower than the study conducted in: (EDHS, 2011), 3 üEthiopia(22%) From those anemic, 5 family members (51. 4%), This might be due to: Bisdimo (27. 9%) (Filagot K, et al, 2014), ü. Addis Monthly Ababafamily (21. 3%)income (Jufar AH. <et 1500 EB al, 2014), (59. 5%). @ Geographical variation of Gilgel Gibe (53. 9%) (Million G, et al, 2012), factors across different area üHIV sero-positive (50%) and Hookworm infected (45. 5%) North western Tigray(36. 1%) (Abel G. et al, 2015), @ Gradual improvement of life zonewho (56. 8%) et al, sulphate 2014) and üGode Those did(Kefyalew not take. A. iron (33. 3%) style and living standards & Nepal 37. 7% (Binay KR. et al, 2014). health seeking behavior.
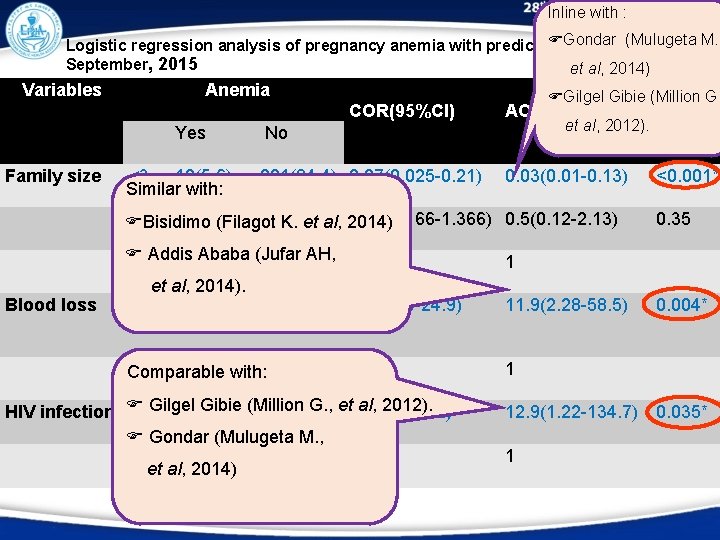
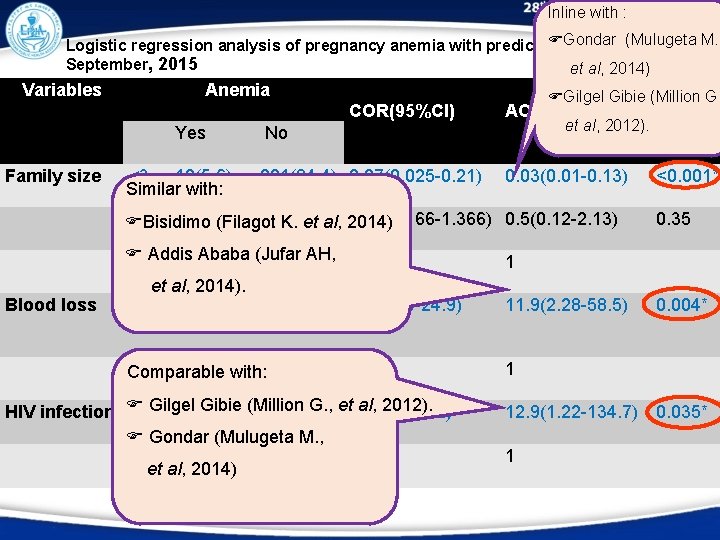
Inline with : Gondar August(Mulugeta M. Logistic regression analysis of pregnancy anemia with predictor variable September, 2015 et al, 2014) Variables Anemia COR(95%Cl) Yes Family size Blood loss <3 12(5. 6) Similar with: Gilgel Gibie (Million G, AOR(95%Cl) p-value 0. 03(0. 01 -0. 13) <0. 001* et al, 2012). No 201(94. 4) 0. 07(0. 025 -0. 21) 3 -5 16(28) 41(72) 0. 47(0. 166 -1. 366) 0. 5(0. 12 -2. 13) Bisidimo (Filagot K. et al, 2014) 0. 35 Ababa (Jufar 6 -8 Addis 9(45) 11(55)AH, 1 et al, 2014). Yes 7(50) 8. 2(2. 69 -24. 9) 1 0. 004* No 30(10. 9) Comparable with: 246(89. 1) 1 1 Gilgel Gibie (Million al, 2012). HIV infection Yes 5(50) G. , et 7. 7(2. 1 -28. 2) Gondar (Mulugeta M. , No 32(11. 5) 248(88. 5) 1 et al, 2014) 11. 9(2. 28 -58. 5) 12. 9(1. 22 -134. 7) 1 0. 035*
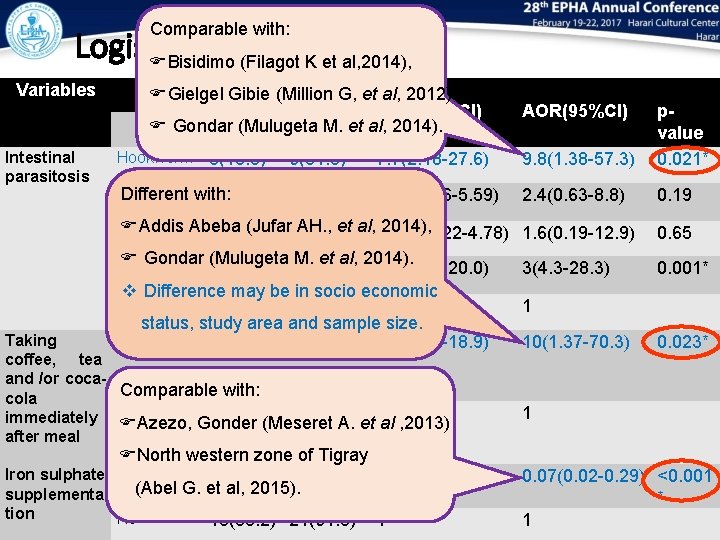
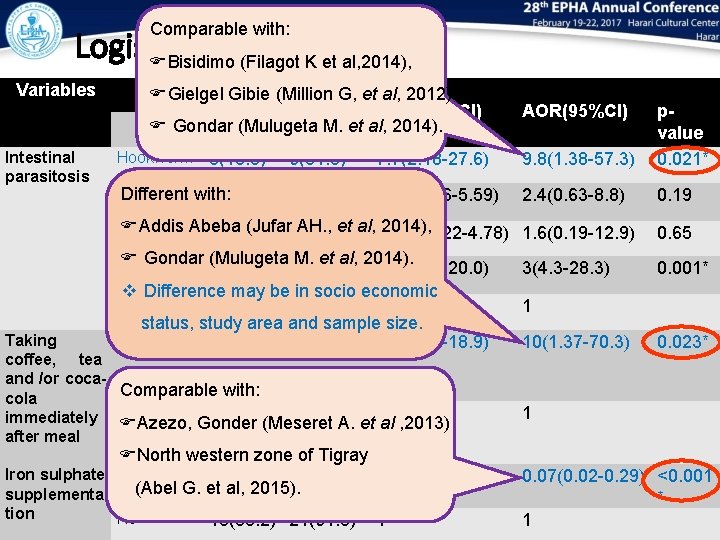
Comparable with: Logistic…. . Bisidimo (Filagot K et al, 2014), Variables Intestinal parasitosis Anemia Gielgel Gibie (Million G, et al, 2012), COR(95%Cl) Yes No Gondar (Mulugeta M. et al, 2014). Hookworm 5(45. 5) 6(54. 5) 7. 7(2. 18 -27. 6) 9. 8(1. 38 -57. 3) E. Different with: 6(18. 2) 27(81. 8) 2. 07(0. 76 -5. 59) 2. 4(0. 63 -8. 8) histolitica lambilie Addis Abeba AH. , et al, 1. 037(0. 22 -4. 78) 2014), G. 2(10)(Jufar 18(90) 1. 6(0. 19 -12. 9) Gondar (Mulugeta M. et al, 2014). S. 3(33. 3) 6(66. 7) 4. 6(1. 08 -20. 0) stercoralis v Difference may be in socio economic No O/P 21(9. 7) 196(90. 3) 1 status, study area and sample size. Yes 35(14. 8) 202(85. 2) 4. 4(1. 03 -18. 9) Taking coffee, tea and /or coca. Comparable with: cola 2(3. 8) 51(96. 2) 1 immediately No Azezo, Gonder (Meseret A. et al , 2013) after meal North western zone of Tigray Iron sulphate Yes 24(9. 5) 229(90. 5) 0. 19(0. 09 -0. 43) (Abel G. et al, 2015). supplementa tion AOR(95%Cl) No 13(35. 2) 24(64. 8) 1 3(4. 3 -28. 3) pvalue 0. 021* 0. 19 0. 65 0. 001* 1 10(1. 37 -70. 3) 0. 023* 1 0. 07(0. 02 -0. 29) <0. 001 * 1
Conclusion v The prevalence of anemia was found to be lower problem in the study participants. v Main predictors of anemia prevalence were üHigh family size üHistory of abnormal blood loss üHookworm infection üIron sulphate supplementation üLiving with HIV/AIDS üHabit of drinking coffee, tea, and coca-cola immediately after meal.
Recommendation • Need to encourage family planning • Early Dx & Rx of intestinal parasites especially hookworm. • There should be strong/nutrition information/ health education system in health institutions. • Supplementation of Iron sulphate for pregnant mothers should be strengthened.
a h k n ! !
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Defination of prevalence
Defination of prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Megaloblastic anemia lab values
Megaloblastic anemia lab values Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Signs of period vs pregnancy
Signs of period vs pregnancy Prevalence calculation formula
Prevalence calculation formula Incidence vs prevalence
Incidence vs prevalence The crucible unit test
The crucible unit test 3 weeks pregnant ultrasound
3 weeks pregnant ultrasound Logical fallacies in the crucible
Logical fallacies in the crucible How long do mosquito fish live
How long do mosquito fish live đầu ối phồng
đầu ối phồng Prayer point for expectations
Prayer point for expectations