Prevalence and associated factors of zinc deficiency among


- Slides: 12

Prevalence and associated factors of zinc deficiency among pregnant women attending antenatal care at Gambella Hospital, southwest of Ethiopia; Institution based cross sectional study, 2016 By : Ataguadil Mekonnen (Bsc, MPHN)
Introduction • Zinc is an essential trace mineral element vital for: – Physiological, biological, and metabolic functions. – 48% of the world’s population are at a high risk of ZD due to inadequate zinc intake (Brown KH et al. 2004). – 82% of all pregnant women are more likely to suffer from ZD worldwide (Caulfield L et al. 2004). – 31 % (4%-73%) across various regions of world’s po. • Highest Sub-Saharan Africa is 50% (37%-62%). • Asia (34 -73%), USA and Europe (4 -7%) is lowest. – Maternal ZD during and later pregnancy has: Devastating and irreversible consequences on mothers (Ramik U 2000). – 21. 1% of Ethiopian population was at risk of inadequate dietary zinc intake (INZi. NCG, 2004) 1
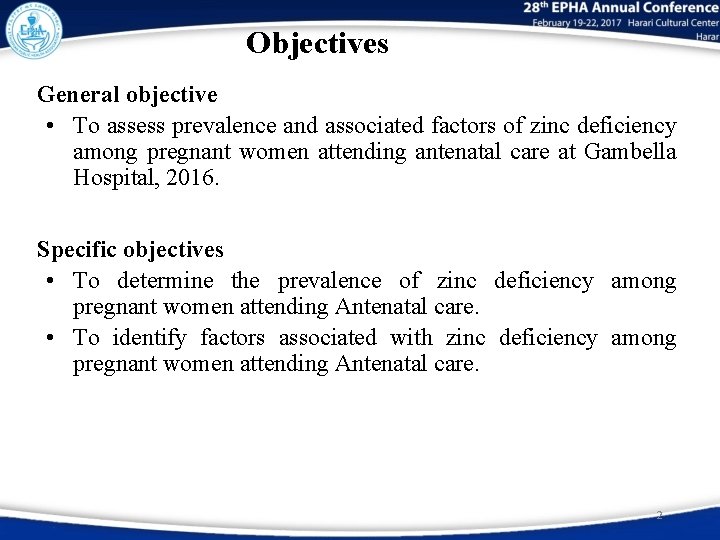
Objectives General objective • To assess prevalence and associated factors of zinc deficiency among pregnant women attending antenatal care at Gambella Hospital, 2016. Specific objectives • To determine the prevalence of zinc deficiency among pregnant women attending Antenatal care. • To identify factors associated with zinc deficiency among pregnant women attending Antenatal care. 2
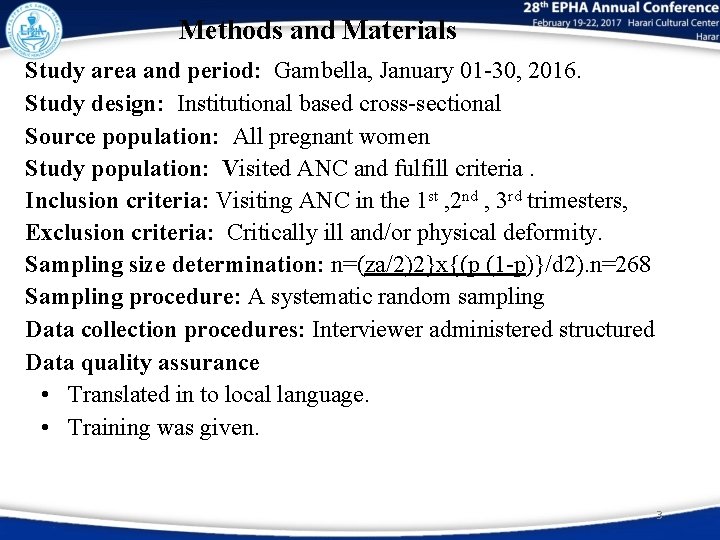
Methods and Materials Study area and period: Gambella, January 01 -30, 2016. Study design: Institutional based cross-sectional Source population: All pregnant women Study population: Visited ANC and fulfill criteria. Inclusion criteria: Visiting ANC in the 1 st , 2 nd , 3 rd trimesters, Exclusion criteria: Critically ill and/or physical deformity. Sampling size determination: n=(za/2)2}x{(p (1 -p)}/d 2). n=268 Sampling procedure: A systematic random sampling Data collection procedures: Interviewer administered structured Data quality assurance • Translated in to local language. • Training was given. 3
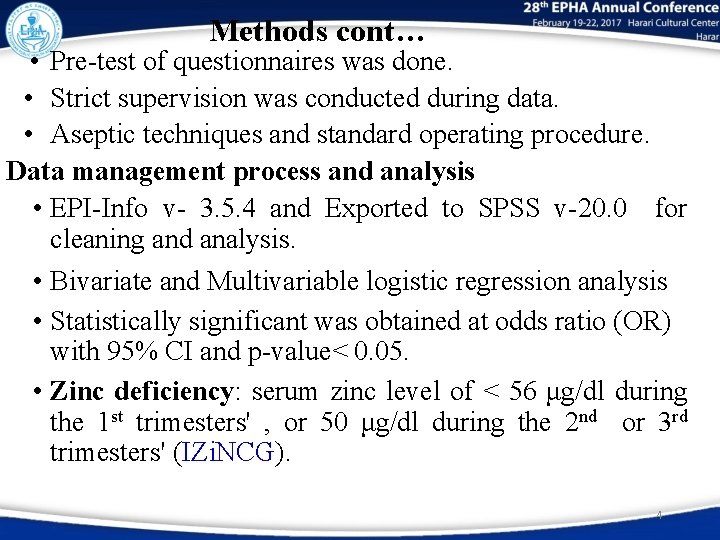
Methods cont… • Pre-test of questionnaires was done. • Strict supervision was conducted during data. • Aseptic techniques and standard operating procedure. Data management process and analysis • EPI-Info v- 3. 5. 4 and Exported to SPSS v-20. 0 for cleaning and analysis. • Bivariate and Multivariable logistic regression analysis • Statistically significant was obtained at odds ratio (OR) with 95% CI and p-value< 0. 05. • Zinc deficiency: serum zinc level of < 56 μg/dl during the 1 st trimesters' , or 50 μg/dl during the 2 nd or 3 rd trimesters' (IZi. NCG). 4
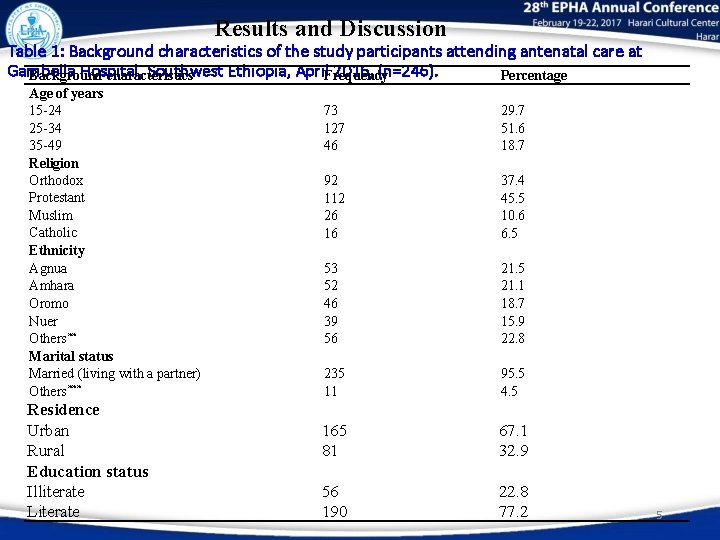
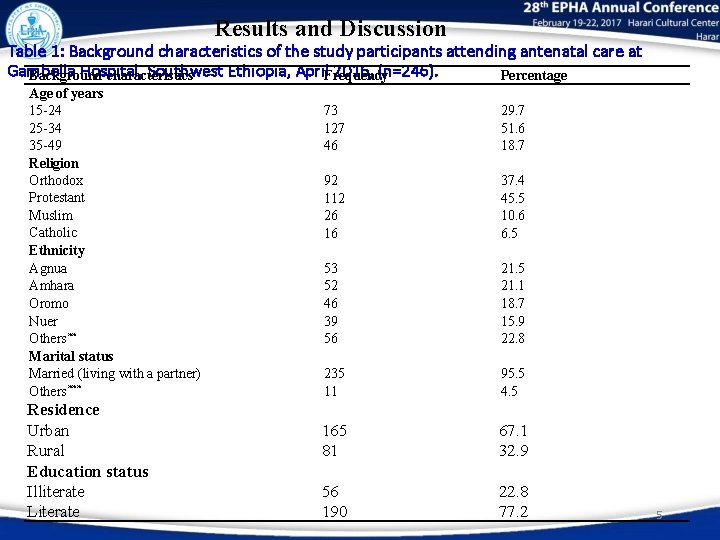
Results and Discussion Table 1: Background characteristics of the study participants attending antenatal care at Gambella Hospital, Southwest Ethiopia, April. Frequency 2016, (n=246). Percentage Background characteristics Age of years 15 -24 25 -34 35 -49 Religion Orthodox Protestant Muslim Catholic Ethnicity Agnua Amhara Oromo Nuer Others** Marital status Married (living with a partner) Others*** Residence Urban Rural Education status Illiterate Literate 73 127 46 29. 7 51. 6 18. 7 92 112 26 16 37. 4 45. 5 10. 6 6. 5 53 52 46 39 56 21. 5 21. 1 18. 7 15. 9 22. 8 235 11 95. 5 4. 5 165 81 67. 1 32. 9 56 190 22. 8 77. 2 5
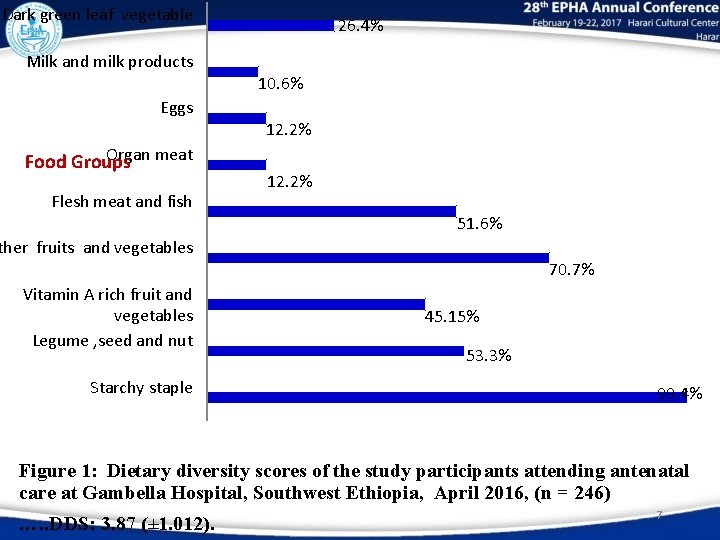
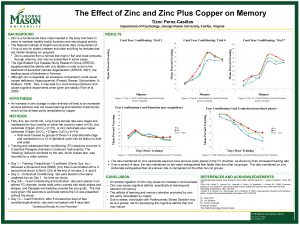
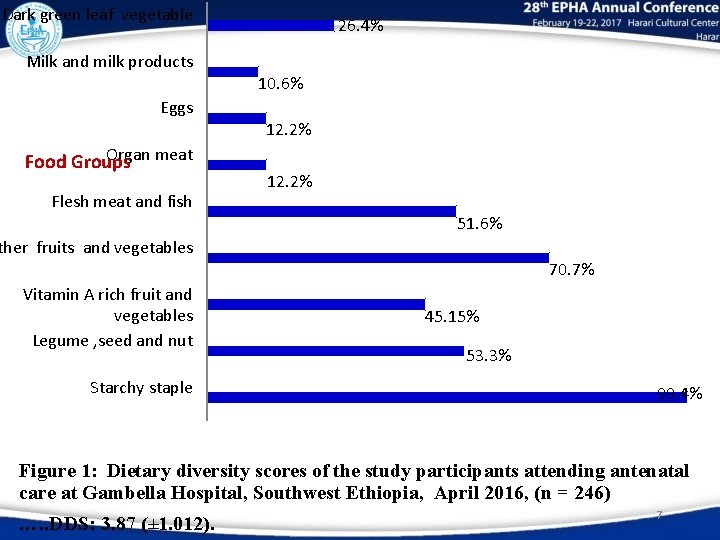
Dark green leaf vegetable 26. 4% Milk and milk products 10. 6% Eggs 12. 2% Organ meat Food Groups Flesh meat and fish 12. 2% 51. 6% ther fruits and vegetables 70. 7% Vitamin A rich fruit and vegetables Legume , seed and nut Starchy staple 45. 15% 53. 3% 99. 4% Figure 1: Dietary diversity scores of the study participants attending antenatal care at Gambella Hospital, Southwest Ethiopia, April 2016, (n = 246) …. . DDS: 3. 87 (± 1. 012). 7
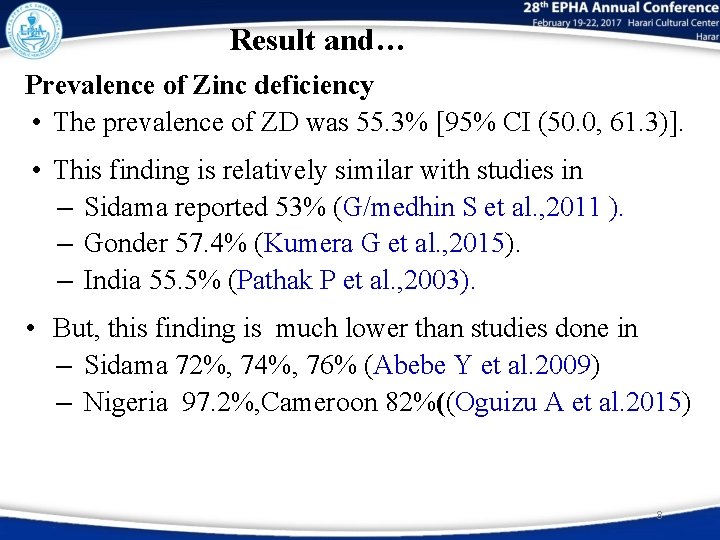
Result and… Prevalence of Zinc deficiency • The prevalence of ZD was 55. 3% [95% CI (50. 0, 61. 3)]. • This finding is relatively similar with studies in – Sidama reported 53% (G/medhin S et al. , 2011 ). – Gonder 57. 4% (Kumera G et al. , 2015). – India 55. 5% (Pathak P et al. , 2003). • But, this finding is much lower than studies done in – Sidama 72%, 74%, 76% (Abebe Y et al. 2009) – Nigeria 97. 2%, Cameroon 82%((Oguizu A et al. 2015) 8
Result and… • This variation could be explained by difference: – Cut-offs of serum zinc levels were used for defining. – Only pregnant women in the 3 rd were included. – Sample size difference and urban-rural. • Relatively higher than reports from other studies: – Sudan 38% (Bushra M et al. 2010). – Bangladesh 14. 7% , Iran 29% (Shamin A et al. 2013). • High prevalence of ZD in the present study might be: ─ Poor pre- and during pregnancy nutritional status. ─ Prone to seasonality bias. 9
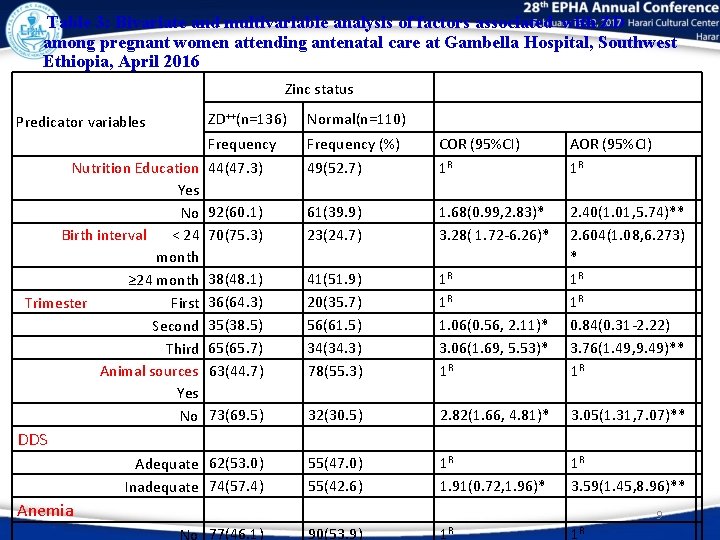
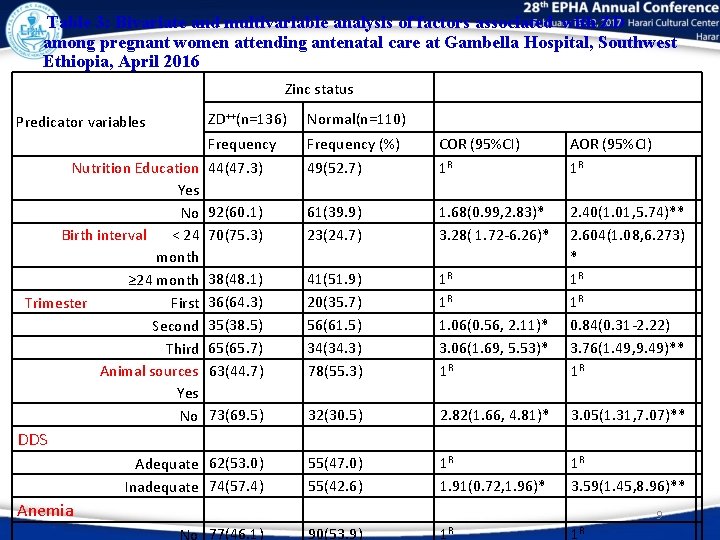
Table 3: Bivariate and multivariable analysis of factors associated with ZD among pregnant women attending antenatal care at Gambella Hospital, Southwest Ethiopia, April 2016 Zinc status ZD++(n=136) Predicator variables Frequency Nutrition Education 44(47. 3) Yes No 92(60. 1) Birth interval < 24 70(75. 3) month ≥ 24 month 38(48. 1) Trimester First 36(64. 3) Second 35(38. 5) Third 65(65. 7) Animal sources 63(44. 7) Yes No 73(69. 5) Normal(n=110) Frequency (%) 49(52. 7) COR (95%CI) 1 R AOR (95%CI) 1 R 61(39. 9) 23(24. 7) 1. 68(0. 99, 2. 83)* 3. 28( 1. 72 -6. 26)* 41(51. 9) 20(35. 7) 56(61. 5) 34(34. 3) 78(55. 3) 1 R 1 R 1. 06(0. 56, 2. 11)* 3. 06(1. 69, 5. 53)* 1 R 2. 40(1. 01, 5. 74)** 2. 604(1. 08, 6. 273) * 1 R 1 R 0. 84(0. 31 -2. 22) 3. 76(1. 49, 9. 49)** 1 R 32(30. 5) 2. 82(1. 66, 4. 81)* Adequate 62(53. 0) Inadequate 74(57. 4) 55(47. 0) 55(42. 6) 1 R 1. 91(0. 72, 1. 96)* No 77(46. 1) 90(53. 9) 1 R DDS Anemia 3. 05(1. 31, 7. 07)** 1 R 3. 59(1. 45, 8. 96)** 9 1 R
Recommendations To policy makers and programmers – Should motivate and attract NGO working with micronutrient deficiencies. To Hospital and Regional health Bureau – Encourage effective methods of family planning implementation – Improving dietary diversity, modified feeding practice – Nutrition education center need to be established to provide nutrition education. – Provide iron or iron-folate supplementation – Treatment of the underlying cause’s anemia. – Promoting and practice the consumption of zinc rich foods. v. Further research should be done on this area using different designs. 11

12
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Defination of proportion
Defination of proportion Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Zinc oxide + nitric acid → zinc nitrate + water
Zinc oxide + nitric acid → zinc nitrate + water Chemical change examples
Chemical change examples Zinc deficiency in india
Zinc deficiency in india Zinc deficiency rash
Zinc deficiency rash Attack rate formula
Attack rate formula Incidence vs prevalence
Incidence vs prevalence Mg +cuo
Mg +cuo Reaction between zinc and acetic acid
Reaction between zinc and acetic acid Minerals sources functions and deficiency chart
Minerals sources functions and deficiency chart