Preterm infants prematurity Definitions Preterm infant Is the
- Slides: 32
Preterm infants (prematurity)
Definitions: Preterm infant: Is the live born infant delivered before 37 weak from the first day of the last menstrual period. Low birth weight infant(LBW): Is life born infant with birth weight below the 5 th percentile of weight for gestational age, they are might be preterm infants or full term infants with intrauterine growth retardation (IUGR) Very low birth weight infant: Is infant with birth weight less than 1500 gm. Extremely low birth weight infant: Is infant with birth weight less than 1000 gm.
Causes of prematurity : I. Fetal causes: 1. Fetal distress. 2. Multiple pregnancy. 3. Erythroblastosis fetalis. 4. Non immune hydrops. II. Placental causes: 1. Placental dysfunction. 2. Placenta previa. 3. Abruptio placentae.
III. Uterine causes: 1. Bicornate uterus. 2. Cervical incompetence (premature dilation). IV. Maternal causes: 1. Preeclampsia. Chronic medical illnesses (e. g. cyanotic heart diseases, renal diseases). ction (e. g. group B streptococcus, UTI, bacterial vaginosis, chorioamnionitis) 4. Drugs abuse (e. g. cocaine).
V. Others: 1. Premature rapture of membranes. 2. Polyhydramnios. 3. Iatrogenic (poorly timed cesarean section, surgery).
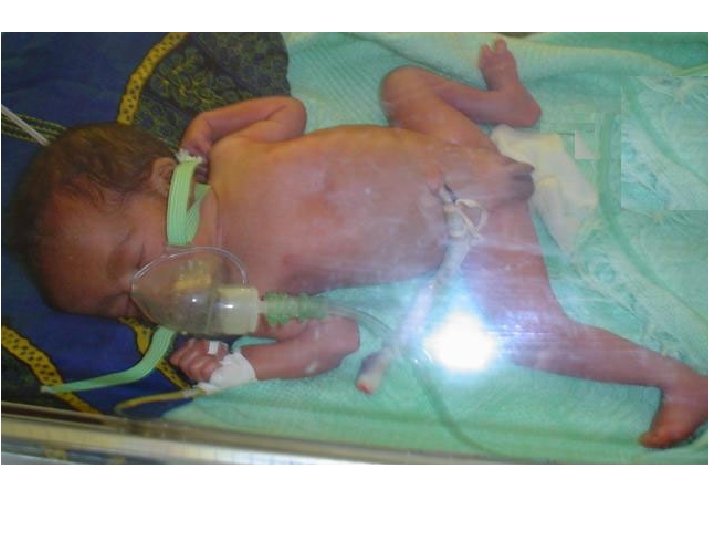
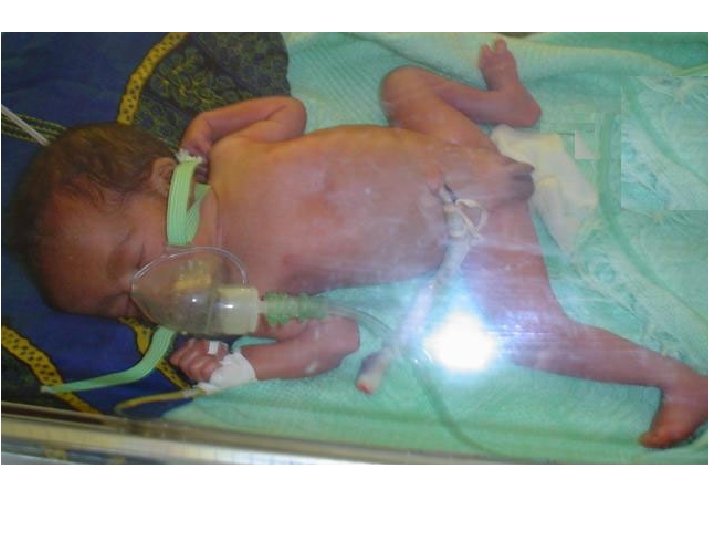
Clinical features: 1. Large head compare to the body head. 2. Pink, thin, or transparent skin. 3. Sleepy most of the time (full term baby sleeps about 14 hr/day). 4. Hypotonic with fully extended limbs (frog-like posture). 5. Non palpable breast tissues. 6. Soft pinna of the ear with no cartilage.
ndescended testis in the males and widely separated labia in the females. 8. Weak cry, sucking, coughing, and swallowing. 9. Little or no subcutaneous tissues. Excessive lanugo hair (black, soft, and brittle hair over the back and shoulders).
Problems of prematurity: 1. Thermal instability: due to: mmaturity of heat regulatory center in the brain. oor muscle movements (heat production required active muscle movements). c. Little or no subcutaneous fat. d. Poor sweating mechanism. ge surface area compared to the body weight. f. Low glycogen stores in their bodies.
2. feeding problems: term infant have incoordinate sucking, owing, and breathing (coordination not ed until 34 -36 wks of gestation), so liable for aspiration and enteral ding must be provided by gavage, also the fant frequently have gastrohageal reflux and immature gag reflex which increases the risk of aspiration.
3. Respiratory problems: DS (most common), pneumothorax (either ous or during resuscitation by g oxygen pressure more than eded), apnea, bradycardia, and chronic lung ease (bronchopulmonary dysplasia) due to high oxygen concentration usage.
th asphyxia: The preterm infants are unable to take the 1 st breath due to: a. Immaturity of respiratory center in the brain. b. Surfactant deficiency. lail chest of newborn due to thin chest wall and weak intercostal muscles. CVS problems: PDA, bradycardia (with apnea) and congenital malformations.
Hematological problems: Anemia (early onset), indirect hyperbilirubinemia, cutaneous or internal hemorrhage), vitamin K deficiency. Gastrointestinal problems: Poor motility, olitis, direct congenital anomalies, gastro-esophageal reflux. olic-endocrine problems: hypocalcemia, hypoglycemia, hyperglycemia.
blems: intraventricular rhage, HIE, seizures, retinopathy of prematurity, deafness, hypotonia, kernicterus. blems: hyponatremia, hyperkalemia, renal tubular acidosis. 11. Infections: Congenital, Perinatal or nosocomial infections. utritional problems: Iron, folic acid, phosphorus and vitamin K deficiency.
Management of preterm infants: 1. Respiratory support: n therapy: by nasal prong, and if ary, by Ambu bag or endotracheal intubation. Its should be monitored by pulse oximeter or utaneous Pa. O 2 or blood gasses analysis. B. Surfactant therapy for RDS. C. Treatment of apnea of prematurity.
2. Thermal regulation "the most important": Infants should be dried well after birth and put in an overhead radiant heater then transferred to the incubator. 3. Monitoring: By pulse oximeter (put to the ear or fingers) to monitor oxygen saturation, also monitor the pulse rate, respiratory rate, blood gasses and p. H and serum electrolytes.
4. CXR: For the diagnosis of respiratory problems (RDS, pneumothorax, emphysema) and to confirm the position of endotracheal tube or umbilical catheter. 5. Treatment of metabolic disturbances especially hypoglycemia and hypocalcemia. 6. Minimal handling of the infants: because vigorously handled infant may developed apnea or cardiac arrest.
7. Fluid and nutritional support: The average caloric requirement for the growing premature infant is 120 Kcal/kg/24 hr Expected weight gain for the adequately nourished preterm infant is 10 -30 gm/day. Initially the preterm infant required 60 -70 ml/kg/24 hr of 10% dextrose water for the first 24 hr of life to maintain blood glucose concentration between 60 -100 mg/dl. Then added electrolyte in form of 1/5 th glucose saline solution on the second day of life at a rate of 120 -150 ml/kg/24 hr.
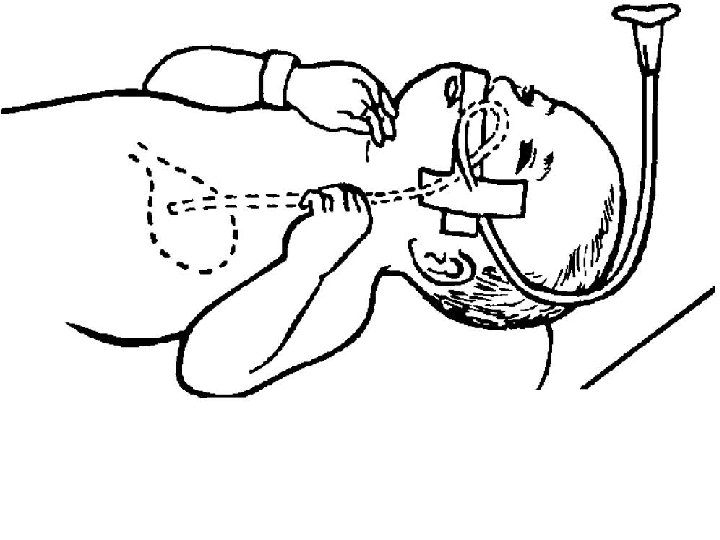
Nutritional support for preterm infant started as soon as possible after stabilization of respiration to avoid aspiration by gavage feeding of small volumes of breast milk or 20 kcal/oz of premature formula (10 -25% of total infant nutritional need) and slowly advanced to full caloric needs over 3 -7 days once the infant is stable.
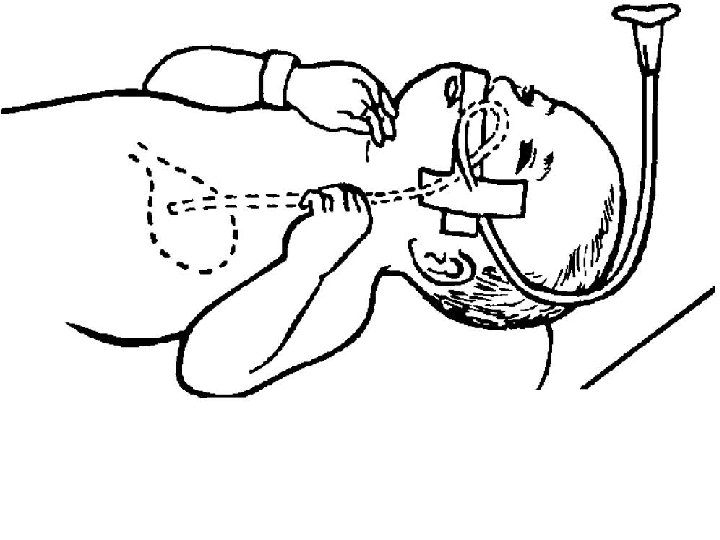
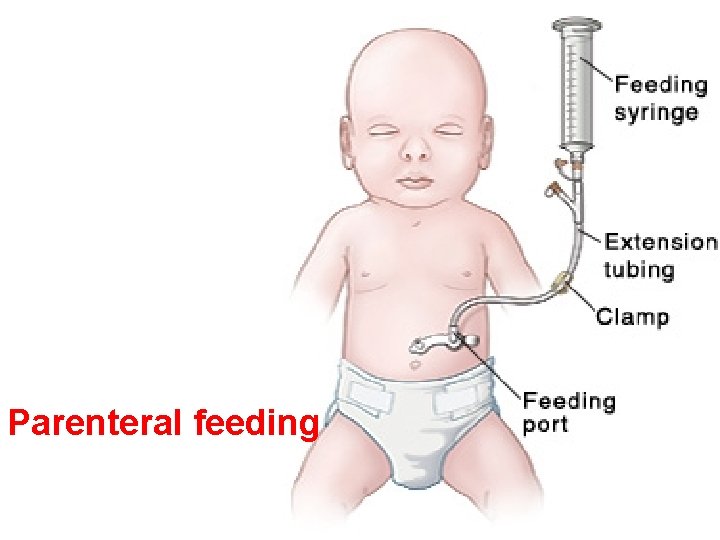
Intermittent bolus gavage feeding is preferable over continuous feeding because is stimulate the release of intestinal hormones and may accelerate the maturation of GIT, but continuous feeding by continuous drip is more safe in extremely LBW infants Nutritional support in VLBW infants is started at 24 -48 hr of age with paranteral alimentation solutions given either peripherally or centrally via an umbilical vein. Supplementation of iron, Ca, Ph, folic acid and Vitamin D are usually started after 4 -6 wks of life.
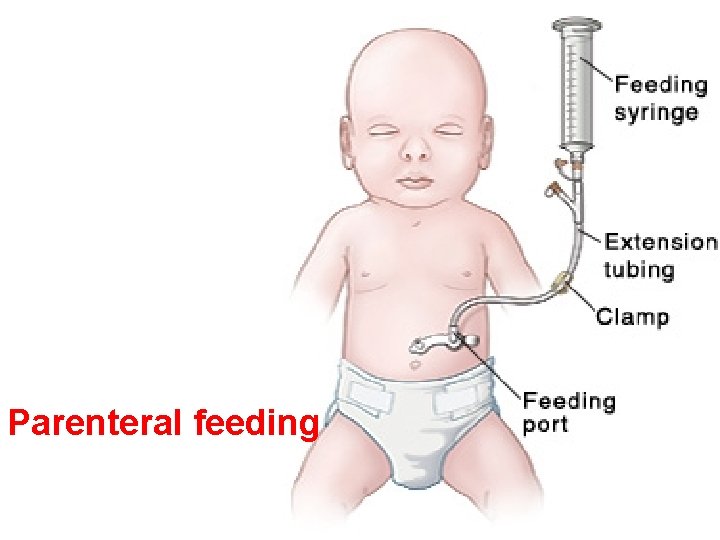
Parenteral feeding
8. Management of infection: A. Screening for infection: by: a. CBC. b. C-reactive protein. c. WBC count and differential counts. e. Urine examination and culture. f. CSF examination and culture. atment of any documented infection by appropriate antibiotics therapy.
C. Prevention of infection: by: nd washing and health education to the staff. reful cleaning of incubators and all other instruments. voidance of nosocomial infections by using e equipments and isolation of affected infants. ntibiotics should be used according to the culture and sensitivity tests. e. Avoid overcrowding and maintain appropriate patient-staff ratio. f. Immunization.
Long term complications of prematurity: g disease (CLD) or bronchopulmonary dysplasia: 2. Retrolental fibroplasia or retinopathy of prematurity: Its interruption of normal progression of retinal vasculature due to administration of high oxygen concentration for preterm infants. Its responsible for many cases of blindness. So retinal examination should be done at 2 -4 wks intervals in any premature infant until the retina is fully vascularized. Treatment is by laser therapy
3. Late anemia of prematurity: The Hb level in preterm infant decrease rapidly after birth to reaches its nadir level at 8 -12 wks of age and is 2 -3 g/dl lower than that in term infant. This lower Hb level in preterm infant is due to decreased erythropoietin response to the low RBC mass. Treatment by: 1. Blood transfusion of backed RBC in severe anemia. poietin 250 Unit/kg given S. C. 3 mes/week with iron supplementation in a dose of 4 -8 mg/kg/day.
4. Necrotizing enterocolitis: It’s the most common acquired G. I. emergency in the newborn infants, its most often affect preterm infants, with an incidence of 10% in infants of birth weight less than 1500 g. In term infants its occurs in association with polycythemia, CHD and birth asphyxia. Pathogenesis: is multifactorial interaction between immaturity of GIT , mucosal injury, and potentially injurious factors in the intestinal lumen like milk protein.
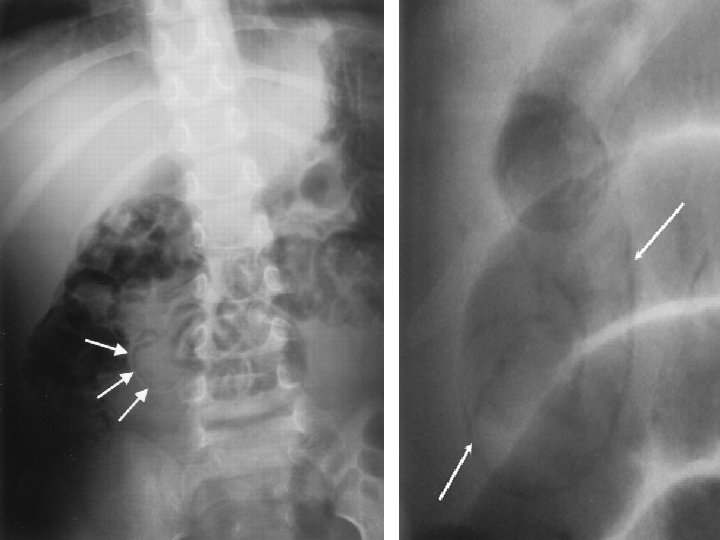
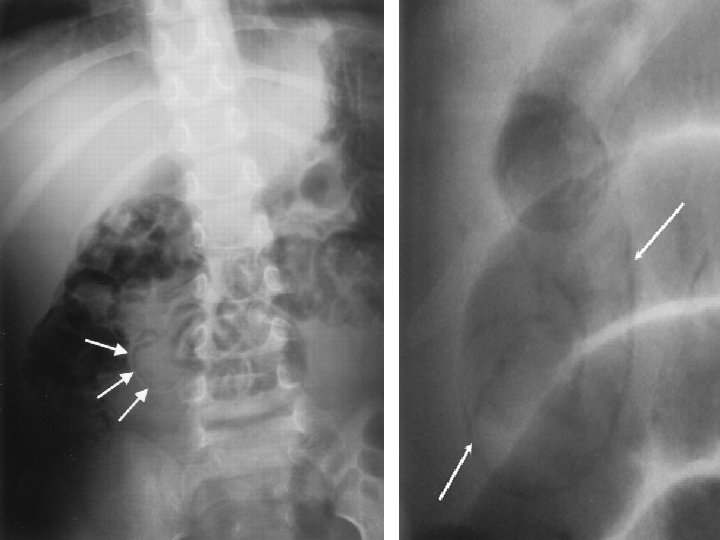
Clinical features: abdominal distension (the most common presenting sign), vomiting, bloody stool, abdominal tenderness, temperature instability, apnea, bradycardia, sepsis, decrease COP and poor perfusion. Investigations: BC shows low Hb concentration, increased C count or absolute neutropenia in severe disease and thrombocytopenia. 2. Stress-induced hyperglycemia 3. Metabolic acidosis. Abdominal X-ray (diagnostic) shows presence bowel wall (pneumatosis intestinalis).
Treatment: A. Medical treatment: 1. Decompression of the intestine by N/G. gen supplementation or mechanical ventilation if necessary. 3. IVF and broad spectrum antibiotics. e monitoring of vital signs, physical ation and lab. tests (WBC, platlate, s, and serial abdominal Xrays).
B. Surgical treatment: indicated in: 1. Evidence of perforation. 2. Fixed dilated bowel lope on serial X-rays. 3. Abdominal wall cellulitis. 4. Failure of medical treatment. Surgical treatment include resection of necrotic bowel segment and create colostomy, then reanastomosis and closure of colostomy done after resolution of the disease and the infant is growing (usually >2 kg body wt after 4 -6 wks of age).
5. PDA 6. Rickets. 7. CNS complications: a. Behavioral problems. b. Mental retardation. c. Progressive hydrocephaly. d. Cerebral palsy. e. Learning problems.