PHM 456 Common Infectious Diseases of Childhood James










- Slides: 41
PHM 456 Common Infectious Diseases of Childhood James Tjon, BSPhm, Pharm. D, RPh Department of Pharmacy The Hospital for Sick Children October 21, 2004
Objectives Review the epidemiology, etiology, pathophysiology, clinical presentation, treatment and prevention associated with the following pediatric infectious diseases: Ø Croup Ø Pertussis Ø Bronchiolitis Ø
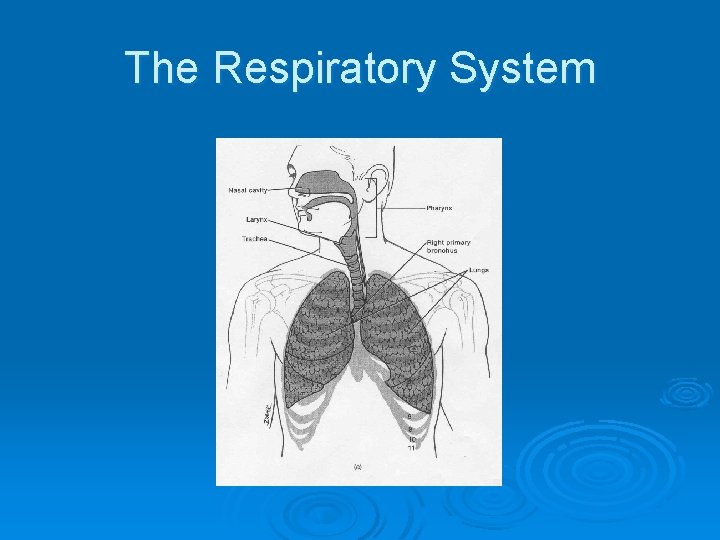
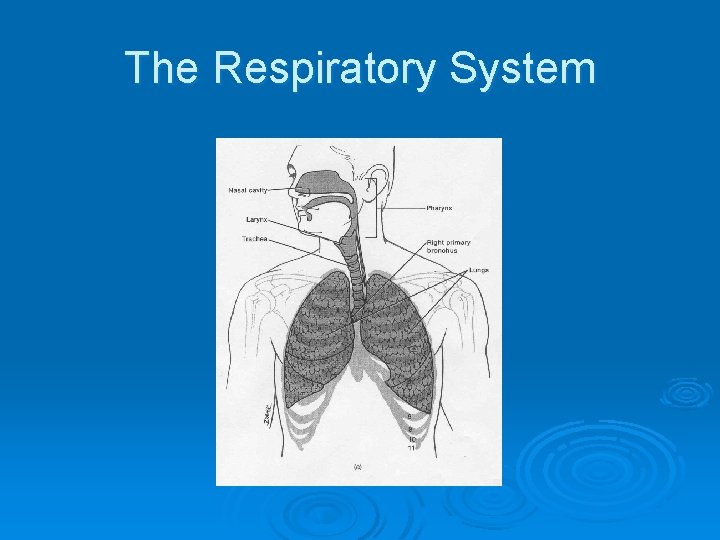
The Respiratory System
Croup Ø 4 different classifications of Croup Syndrome: l l Laryngotracheitis Spasmodic Bacterial tracheitis Epiglottitis
Croup Ø Definition Involves inflammation and edema of the larynx, subglottic tissues and trachea, causing airway obstruction and is due to an infectious agent
Croup Ø Epidemiology l l l > 15% of respiratory tract disease in pediatric practice Age: 6 months to 3 years Peak age: 2 years More common in boys Late fall and winter
Croup Ø Microbiology l l l Primarily viral Parainfluenza (types 1, 2 & 3) Influenza A & B Adenovirus, Respiratory Syncytial Virus (RSV), measles Bacterial
Croup Ø Pathophysiology l l Begins in nasopharynx Spreads to larynx and trachea Inflammation, erythema and edema in trachea Subglottic area is major site of airway obstruction

Croup: Chest X-Ray
Croup Ø Clinical Presentation l l l l Gradual onset Duration normally 5 days Low grade fever Classic “barking” cough Hoarse voice Stridor Dyspnea Sore throat

Croup Ø Clinical Presentation l l Worsening of breathing difficulty Cyanosis Difficulty swallowing Possible hospital admission

Croup Ø Treatment l l Cold air Humidified air • cool mist vaporizer • steamy bathroom • humidified oxygen l Croup tents


Croup Ø Treatment l Epinephrine • anti-inflammatory activity decreases subglottic edema • can improve stridor, decrease need for hospitalization & intubation and decrease mortality rates • onset: 10 to 30 minutes • duration of effect: 2 hours
Croup Ø Treatment l Racemic epinephrine inhalation • Dose: 0. 5 m. L of 2. 25% solution in 3 m. L 0. 9% Na. Cl q 1 -2 h up to q 20 minutes l l-epinephrine inhalation • • • l 1: 1, 000 solution (1 mg/m. L) dose: 2 -5 m. L q 1 -4 hours as effective as racemic epinephrine Side effects
Croup Ø Treatment l • Corticosteroids (moderate-severe Croup) Dexamethasone 0. 6 mg/kg IV/IM x 1 • oral versus parenteral • Budesonide inhalation • strong topical effects with low systemic activity • 2 mg x 1, repeated q 12 -24 h prn
Croup: Canadian Study N Engl J Med 2004; 351: 1306 -13 Ø Randomized, double-blind, multi-centre study (n= 720 children, mild Croup) Ø Dexamethasone 0. 6 mg/kg oral or placebo Ø Primary & secondary outcomes Ø Dexamethasone effective treatment for mild Croup Ø

Pertussis Whooping cough syndrome Ø 100 Day Cough Ø “Intense cough” Ø Epidemiology Ø l l l Seasonal, fall and winter Transmission by coughing All ages, 60% under 5 years
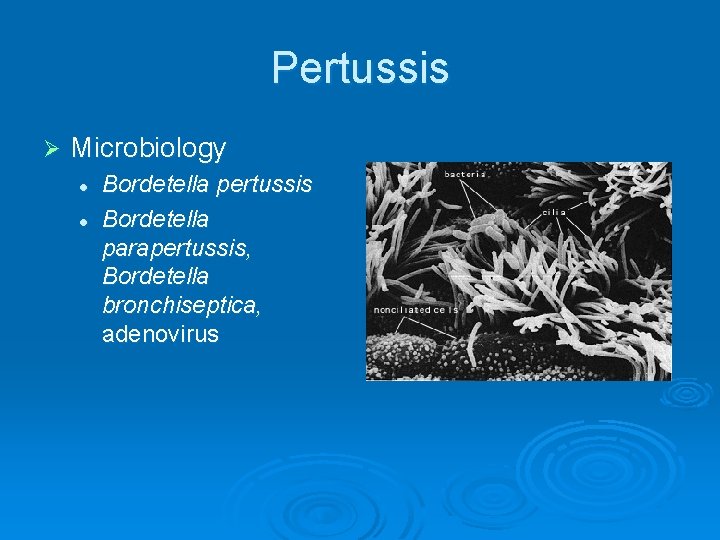
Pertussis Ø Microbiology l l Bordetella pertussis Bordetella parapertussis, Bordetella bronchiseptica, adenovirus

Pertussis Ø Pathophysiology: l l l Inhalation of organism Adherence to ciliated cells Proliferation and spread Paralysis of cilia Production and accumulation of mucous Possible progression to pneumonia

Pertussis Ø Complications l l l Hospitalization Pneumonia Central nervous system • encephalopathy • seizures l Mortality
Pertussis Complications by Age *Cases reported to CDC 1997 -2000 (N=28, 187)
Pertussis Ø Treatment • Supportive • oxygen • suctioning • Antibiotics

Pertussis Ø Antibiotics l l Erythromycin estolate 40 mg/kg/day po QID x 10 -14 days Clarithromycin 15 mg/kg/day po BID X 10 days Azithromycin 10 mg/kg/day po x 1 day, then 5 mg/kg/day po daily x 4 days Cotrimoxazole 8 mg TMP /kg/day po BID
Pertussis: Canadian Study Pediatrics 2004; 114(1): e 96 Ø Randomized, multi-centre study comparing azithromycin and erythromycin estolate (n=477, 6 months - 16 years) Ø Outcomes: bacterial cultures, serology & PCR, ADRs, compliance and symptoms Ø As effective, fewer ADRs & good compliance Ø
Pertussis Ø Prevention l l l Highly communicable Household contacts Same drugs as for treatment
Pertussis Ø Prevention l l l Acellular pertussis vaccine (DTa. P) Part of routine immunization schedule: Administration: 2, 4, 6 and 18 months with booster at 4 to 6 years
Bronchiolitis Ø Definition: acute respiratory illness resulting from inflammation of small airways, characterized by wheezing and caused by viral infection
Bronchiolitis Ø Epidemiology l l l Young children Peak incidence between 2 to 6 months Winter and early spring
Bronchiolitis Ø Microbiology l l l Respiratory syncytial virus (RSV) Parainfluenza Influenza A & B Adenoviruses Transmission by direct contamination
Bronchiolitis Ø Pathophysiology l l l Viral replication in bronchioles Necrosis of ciliated cells Increased mucous secretions Bronchial plugging with obstruction Hypoxia
Bronchiolitis Ø Clinical Presentation l l l Fever Nasal discharge Dry cough Wheeze Usually self-limiting Asthma, pneumonia, CHF, cystic fibrosis
Bronchiolitis Ø Progression l l l Risk factors Tachypnea Irregular breathing Cyanosis or pallor Apnea Mortality
Bronchiolitis Ø Treatment l Supportive • • • l oxygen hydration suctioning Inhaled beta-agonists (salbutamol) • controversial l Racemic or l-epinephrine • vasoconstricts mucosa to reduce edema
Bronchiolitis Ø Treatment l Corticosteroids • oral versus inhaled l Ribavirin • controversial • modest clinical benefit • no effect on hospital stay
Bronchiolitis Ø Prevention l Passive immunization • given monthly through RSV season • RSV Immune Globulin (RSVIVIG, Respigam): blood product l Palivizumab • monoclonal antibody • IM injection monthly during RSV season • costly
Bronchiolitis Ø Palivizumab (Synagis®) l l l Approved in Canada in June of 2002 Formerly required Special Access Programme authorization Manufacturer: Med. Immune Inc. Distributor: Abbott Laboratories Funding provided by Canadian Blood Services (CBS) if patients meet high risk criteria
Bronchiolitis Ø Palivizumab Criteria l l Children < 24 months of age with BPD/CLD and who have required oxygen or medical treatment within 6 months of RSV season Premature infants born at 32 weeks gestation and aged 6 months at start of RSV season Children < 24 months of age with hemodynamically significant heart disease Other: 33 -35 week gestation infants at risk, immune deficiency Canadian Paediatric Society Guidelines
Bronchiolitis Ø Prevention l Active immunization • RSV vaccine • Being researched

Pediatric Infectious Disease References Ø Red Book Ø http: //www. cps. ca Ø The Hospital for Sick Children Formulary Ø Pediatric Dosage Handbook Ø Infectious Diseases Handbook Ø Nelson’s Pocket Book of Pediatric Antimicrobial Therapy Ø Nelson Essentials of Pediatrics
QUESTIONS?
 Epidemiological triad of malaria
Epidemiological triad of malaria Icd 10 morbus hansen
Icd 10 morbus hansen Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Interdental clefts in primary teeth
Interdental clefts in primary teeth Phm sax
Phm sax Proccom phm pertamina
Proccom phm pertamina Dimercaperol
Dimercaperol Phm hai
Phm hai Early middle childhood
Early middle childhood Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Non common communicable diseases
Non common communicable diseases Nilai gcs
Nilai gcs 123 + 456 + 789
123 + 456 + 789 Altyazi123
Altyazi123 Difference between one & two way slab
Difference between one & two way slab Qualitative test for ester
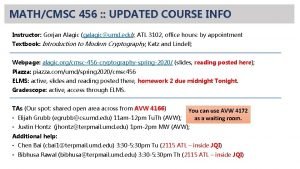
Qualitative test for ester Cmsc 456 3 cryptology
Cmsc 456 3 cryptology Gcs 456
Gcs 456 123456+789
123456+789 Katz cryptography
Katz cryptography 123456789 xxxx
123456789 xxxx Find the local tax deducted: $456 biweekly, 2 1/2 % tax.
Find the local tax deducted: $456 biweekly, 2 1/2 % tax. Bbm456
Bbm456 Blood gangs in oklahoma
Blood gangs in oklahoma 456 name
456 name Slump value as per is 456
Slump value as per is 456 Ee-456
Ee-456 Non stationary process
Non stationary process 123 12345678
123 12345678 Write number in expanded form. 456
Write number in expanded form. 456 8773522583
8773522583 800 456 3355
800 456 3355 Water cement ratio table
Water cement ratio table Smallest infectious agent
Smallest infectious agent Infectious waste in hiligaynon
Infectious waste in hiligaynon Infectious disease
Infectious disease Snc set symbol
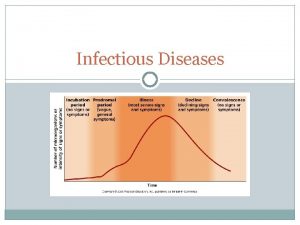
Snc set symbol Stages of infectious disease
Stages of infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease quality controls
Infectious disease quality controls Quizlet
Quizlet Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs