Partnering with Colleges and Universities to Facilitate the








- Slides: 37
Partnering with Colleges and Universities to Facilitate the PCMH Process R. W. “Chip” Watkins, MD, MPH, FAAFP Conference on Practice Improvement Greenville, SC 1 December 2012

Disclosures It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/ invitation of participation. Disclosure documents are reviewed for potential conflicts of interest and if identified, they are resolved prior to confirmation of participation. Only these participants who have no conflict of interest or who agree to an identified resolution process prior to their participation were involved in this CME activity. The following individual(s) in a position to control content relevant to this activity have disclosed the following relevant financial relationships: R. W. Watkins, MD, MPH, a consultant/employee of CCNC.
Patient-Centered Medical Home The PCMH is a model of primary care re-design intended to improve the quality and efficiency of primary care delivery

What we have… Atul Gawande, MD What we need!!
Features of PCMH Four common features in successful demonstration projects § Dedicated care managers § Expanded access to clinicians § Data-driven analytic tools § Use of incentives
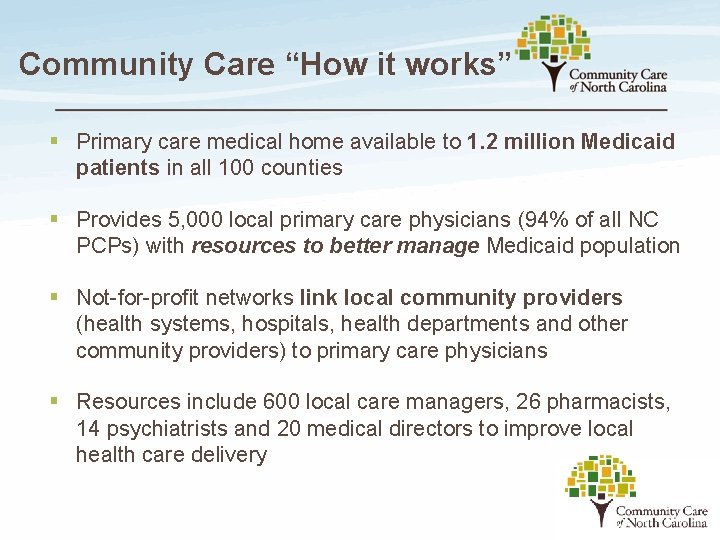
Community Care “How it works” § Primary care medical home available to 1. 2 million Medicaid patients in all 100 counties § Provides 5, 000 local primary care physicians (94% of all NC PCPs) with resources to better manage Medicaid population § Not-for-profit networks link local community providers (health systems, hospitals, health departments and other community providers) to primary care physicians § Resources include 600 local care managers, 26 pharmacists, 14 psychiatrists and 20 medical directors to improve local health care delivery

Community Care: “How it works” § The state identifies priorities and provides financial support through an enhanced PMPM payment to community networks § Networks pilot potential solutions and monitor implementation (physician led) § Networks voluntarily share best practice solutions and best practices are spread to other networks § The state provides the networks (CCNC) access to data § Cost savings/ effectiveness are evaluated by the state and third-party consultants (Treo Solutions, Milliman)
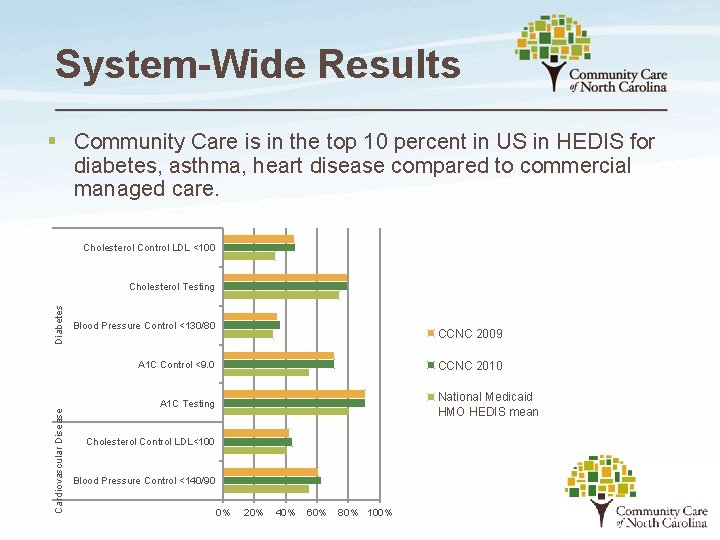
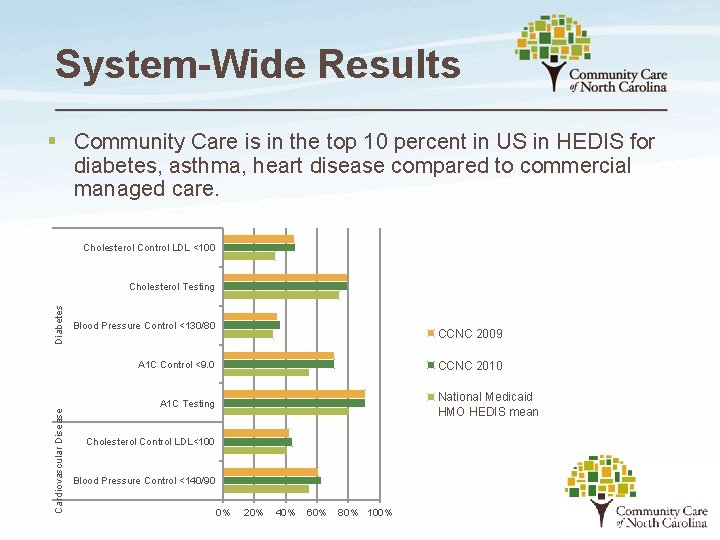
System-Wide Results § Community Care is in the top 10 percent in US in HEDIS for diabetes, asthma, heart disease compared to commercial managed care. Cholesterol Control LDL <100 Diabetes Cholesterol Testing Blood Pressure Control <130/80 CCNC 2009 Cardiovascular Disease A 1 C Control <9. 0 CCNC 2010 National Medicaid HMO HEDIS mean A 1 C Testing Cholesterol Control LDL<100 Blood Pressure Control <140/90 0% 20% 40% 60% 80% 100%
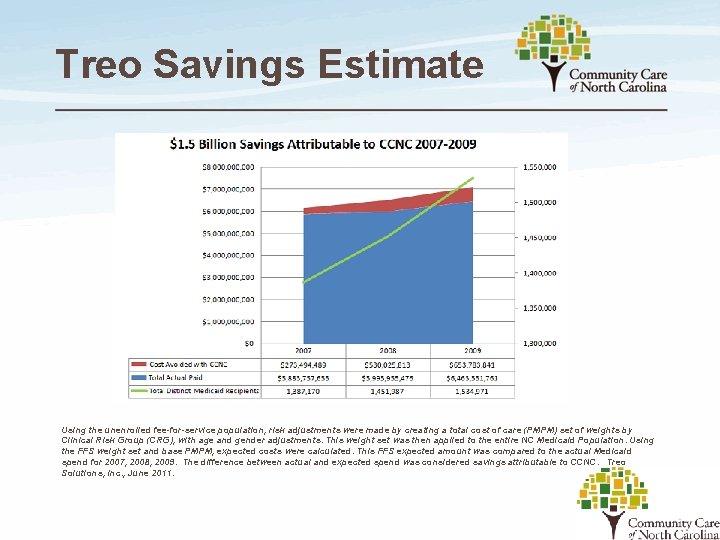
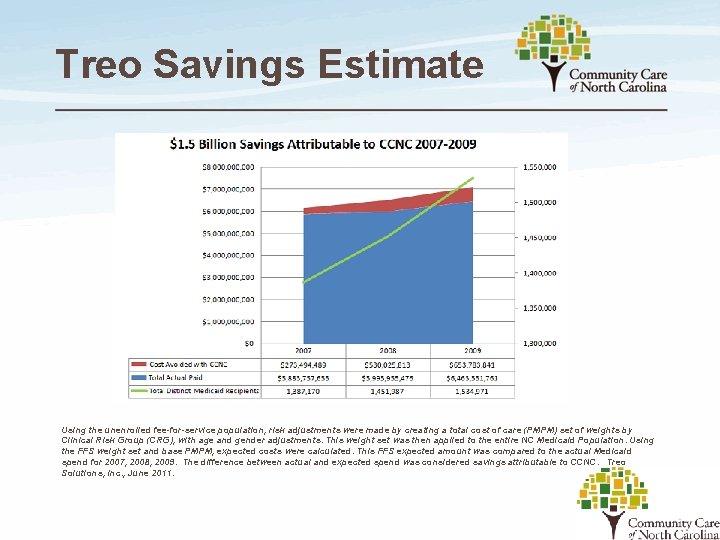
Treo Savings Estimate Using the unenrolled fee-for-service population, risk adjustments were made by creating a total cost of care (PMPM) set of weights by Clinical Risk Group (CRG), with age and gender adjustments. This weight set was then applied to the entire NC Medicaid Population. Using the FFS weight set and base PMPM, expected costs were calculated. This FFS expected amount was compared to the actual Medicaid spend for 2007, 2008, 2009. The difference between actual and expected spend was considered savings attributable to CCNC. Treo Solutions, Inc. , June 2011.
What is the Multi-Payer Advanced Primary Care Practice Demonstration Project (MAPCP)?
What is the Multi-Payer Demo? § The purpose of the Multi-Payer Advanced Primary Care Practice “demonstration project” (MAPCP) is: § To evaluate the effectiveness of the Patient Centered Medical Home (PCMH) model, when supported by both public (Medicaid and Medicare) and private payers (Blue Cross Blue Shield, and State Health Plan) § To utilize care management for these other payer sources
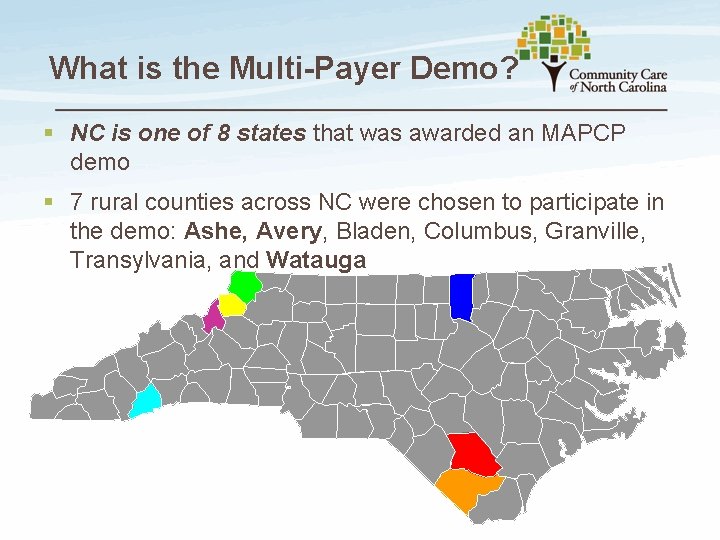
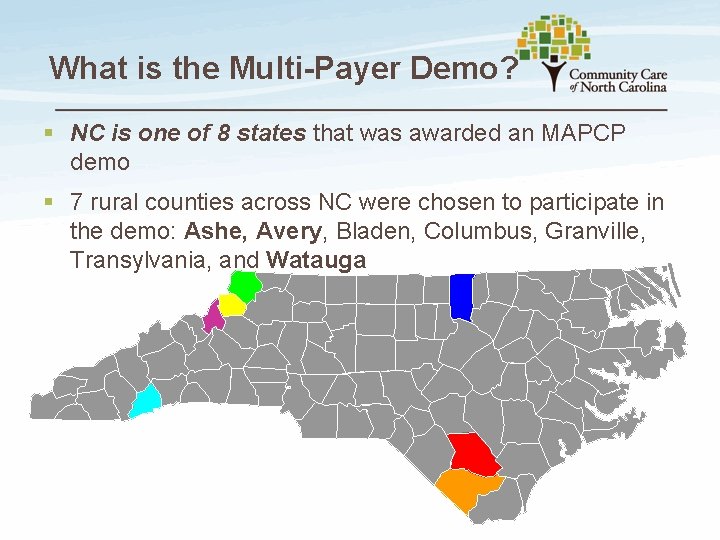
What is the Multi-Payer Demo? § NC is one of 8 states that was awarded an MAPCP demo § 7 rural counties across NC were chosen to participate in the demo: Ashe, Avery, Bladen, Columbus, Granville, Transylvania, and Watauga
What is the Multi-Payer Demo? § To participate, practices in these counties must obtain PCMH recognition from the National Committee for Quality Assurance (NCQA) during their first year of the demo § In return for implementing the PCMH model, practices will earn incentive payments from the largest public and private payers in NC: CMS and BCBS-NC/SHP.

PCMH 2011 Overview (6 standards/27 elements) 1. 2. 3. Enhance Access and Continuity 4. Access During Office Hours Provide Self-Care and Community Resources B. Access After Hours A. Self-Care Process C. Electronic Access B. Referrals to Community Resources D. Continuity (with provider) E. Medical Home Responsibilities A. Test Tracking and Follow-Up F. Culturally/Linguistically Appropriate Services B. Referral Tracking and Follow-Up G. Practice Organization C. Coordinate with Facilities/Care Transitions 5. Identify/Manage Patient Populations 6. Track/Coordinate Care Measure and Improve Performance A. Patient Information A. Measures of Performance B. Clinical Data B. Patient/Family Feedback C. Comprehensive Health Assessment C. Implements Continuous Quality Improvement D. Use Data for Population Management D. Demonstrates Continuous Quality Improvement Plan/Manage Care E. Report Performance A. Implement Evidence-Based Guidelines F. Report Data Externally B. Identify High-Risk Patients C. Manage Care D. Manage Medications E. Electronic Prescribing Optional Patient Experiences Survey
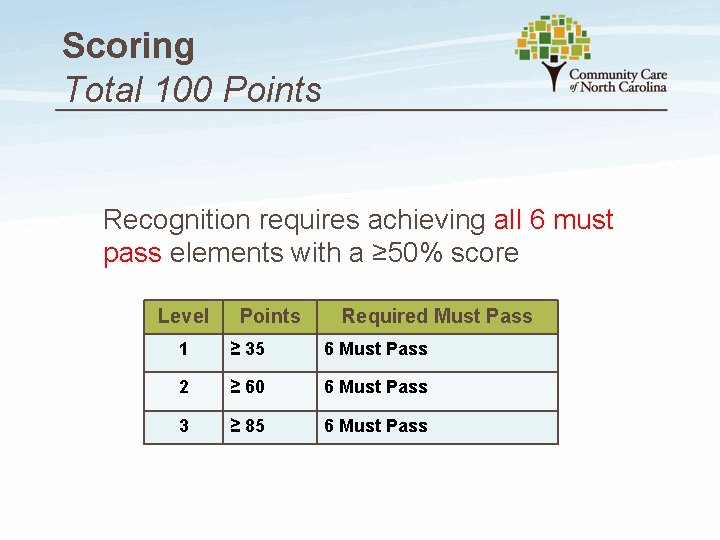
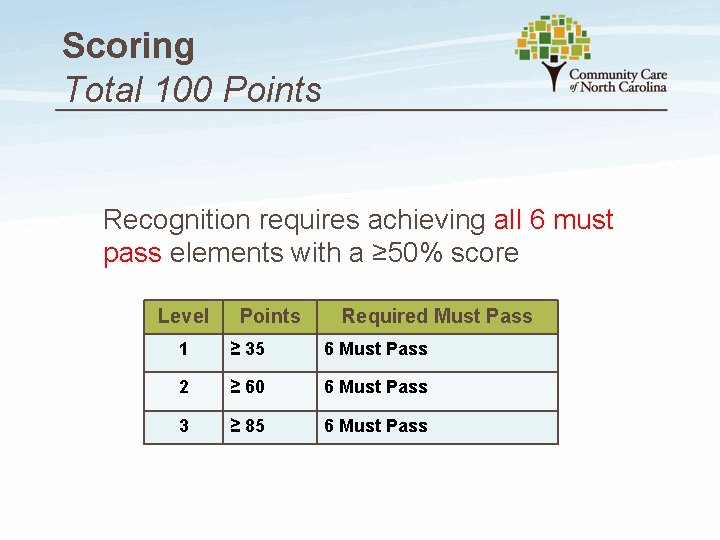
Scoring Total 100 Points Recognition requires achieving all 6 must pass elements with a ≥ 50% score Level Points Required Must Pass 1 ≥ 35 6 Must Pass 2 ≥ 60 6 Must Pass 3 ≥ 85 6 Must Pass
Recognition of Added Value Incentive Payments from Medicare § CMS pays a per member per month fee for each Medicare patient in practices achieving PCMH recognition through NCQA: § Level 1 = $2. 50 PMPM ($30 each year) § Level 2 = $3. 00 PMPM ($36 each year) § Level 3 = $3. 50 PMPM ($42 each year)
Recognition of Added Value Increased Reimbursement from BCBS § Eligibility for the Blue Quality Physicians Program (BQPP), a recognition program for primary care practices that builds on PCMH recognition from NCQA § Once you qualify for the BQPP, BCBS will increase its fee structure by 10% or more for all of your BCBS/SEHP patients
Benefits of the PCMH Model Quality – Outcomes for seven medical home demonstrations § Fewer ER visits (15%-50%) § Fewer hospital admissions (6 -24%) § Lower mortality rates § Better preventive service delivery § Better chronic disease care § Higher patient satisfaction Source: Fields, et al. (2010) and Reid RJ, Coleman K, et al. (2010).
Benefits of the PCMH Model Efficiency – Cost § Lower total costs of care - (6. 5 -22%) § Shorter patient wait times § Less staff burnout/turnover (10% Vs. 30%) § Higher staff satisfaction/productivity Source: Fields, et al. 2010
This is a No-Brainer! § So Why Aren’t Practices RUNNING to implement PCMH for themselves? !? 1. Time 2. Resources 3. Consultants are expensive 4. Fear a) Gov’t interference b) Loss of control/independence c) Change
Watkins. Journal of Medical Practice Management, Sept/Oct 2012, Vol 28: 2, pp. 134 -6.

Linville Gorge, Blowing Rock, NC
ASU Practicum in Primary Care ASU College of Health Science, School of Healthcare Management
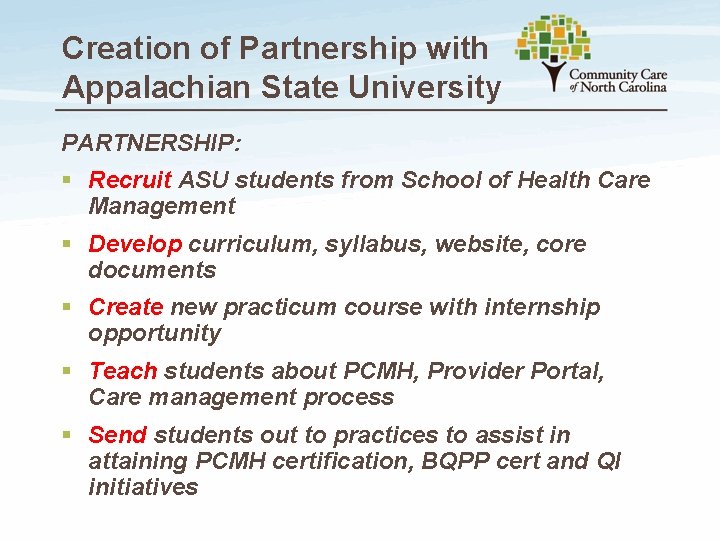
Creation of Partnership with Appalachian State University PARTNERSHIP: § Recruit ASU students from School of Health Care Management § Develop curriculum, syllabus, website, core documents § Create new practicum course with internship opportunity § Teach students about PCMH, Provider Portal, Care management process § Send students out to practices to assist in attaining PCMH certification, BQPP cert and QI initiatives

ASU Practicum in Primary Care § Fall of 2011 – 5 students § Spring 2012 – 9 students – BSBSNC Foundation Grant Obtained § Summer 2012 internship – 8 students § Fall 2012 – 14 students
ASU Practicum in Primary Care § Developed curriculum, core documents, website https: //sites. google. com/site/pcmhprac/
ASU Practicum in Primary Care § Used the CCNC PCMH workbook, webinars § https: //www. communitycarenc. org/emerging-initiatives/pcmh-central 1/2011 -pcmhresources/

ASU Practicum in Primary Care § Worked through curriculum and have weekly didactic meetings on ASU campus § BAA for HIPPA compliance § Students prepare PCMH PPT for “their” practice and give to group § Go through the Standards and hit high points § Students share successes/failures with facilitators/faculty § Placed students in field and worked with the practices § Students give PPT § Work with practices – develop “PCMH Team”, schedule time with team, give weekly assignments, follow-up, etc.
Quotes from Students § “This practicum has served as the keystone to my healthcare management degree. The practical experience I have gained as a student intern is incomparable. This project is on the cutting edge of the future of healthcare delivery. Considering my cross-functional background in psychology and healthcare management and my aspirations to be a primary care physician, this practicum has provided me with the integrative experience and the comprehensive perspective needed to pursue professional school and/or a graduate program with a unique perspective. ” —Delvon Blue § “This internship has afforded me the opportunity to experience the practice management side of healthcare. Also, I had the privilege of working closely with physicians and staff as I learned about their views on patient care and corporate compliance. In addition, I learned how to present information to a team to encourage buy-in, how to work with people of different skill levels and positions, how to implement new processes and improve current processes within the practice, how to draft policies, and how to document the outcomes so the practice could receive the credit they deserve. ” —Ashley Zachary
Program Growth § ASU School of Health Care Management has made the “Practicum in Primary Care” a CORE curriculum class § Students willing to spend 2 semesters with us get full credit for their internship (300 hours) § “Keeping the Medical Home Fires Burning” is a new initiative where practices that have been recognized work with students on QI projects

Program Growth § Remote Learning Initiative § Students work with practices within 3 hours of Boone § MOVI (secure) web-hosting § Face-to-face visits every 3 weeks or so
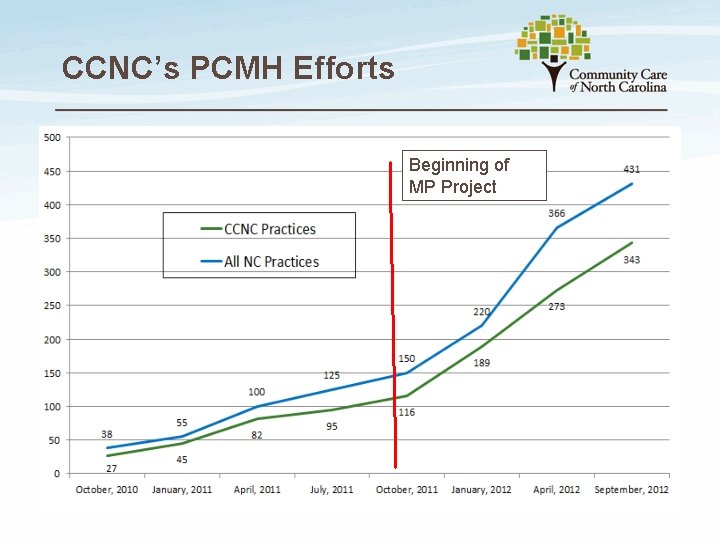
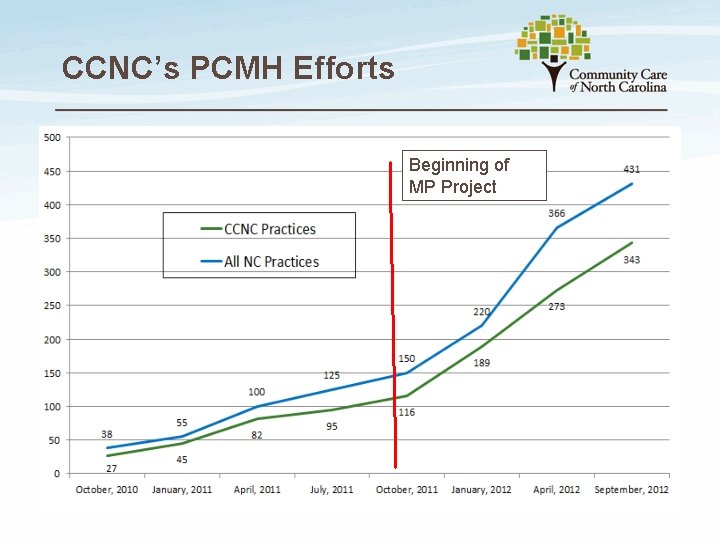
CCNC’s PCMH Efforts Beginning of MP Project
There’s No Place Like…
That’s all folks!
Partnering with Colleges and Universities to Facilitate the PCMH Process R. W. “Chip” Watkins, MD, MPH, FAAFP Conference on Practice Improvement Greenville, SC 1 December 2012
 Pearson
Pearson Styria colleges and universities
Styria colleges and universities Ufa colleges and universities
Ufa colleges and universities Chelyabinsk colleges and universities
Chelyabinsk colleges and universities Chon buri colleges and universities
Chon buri colleges and universities Yaroslavl state technical university
Yaroslavl state technical university Who's who among american college students
Who's who among american college students Mtcu timmins
Mtcu timmins Partnering to build customer relationships
Partnering to build customer relationships The partnering initiative
The partnering initiative Mnos partnering
Mnos partnering Lorna maden
Lorna maden What is partnering
What is partnering Partnering session
Partnering session How to facilitate a group
How to facilitate a group Factors that facilitate successful integrative negotiation
Factors that facilitate successful integrative negotiation How to facilitate a calibration meeting
How to facilitate a calibration meeting Facilitate learning session meaning
Facilitate learning session meaning Agencies that facilitate international flow of funds
Agencies that facilitate international flow of funds Bsbmgt516
Bsbmgt516 Facilitative response
Facilitative response Teamwork in action
Teamwork in action Presales activities
Presales activities World federation of colleges and polytechnics
World federation of colleges and polytechnics Association of schools and colleges of optometry
Association of schools and colleges of optometry Washington state board for community and technical colleges
Washington state board for community and technical colleges Community colleges in south africa
Community colleges in south africa New england association of schools and colleges
New england association of schools and colleges Accrediting commission of career schools and colleges
Accrediting commission of career schools and colleges How many universities in the world
How many universities in the world Sura regional
Sura regional Khazar university ranking
Khazar university ranking Universities that offer pharmacy in nigeria
Universities that offer pharmacy in nigeria Ged testing centers in pakistan
Ged testing centers in pakistan Ontario universities' application centre founded
Ontario universities' application centre founded Pateting
Pateting Should universities departments engineering
Should universities departments engineering Should universities departments engineering
Should universities departments engineering