Palliative Nutrition and Hydration Santhna Letchmi Panduragan Dept

- Slides: 13
Palliative Nutrition and Hydration Santhna Letchmi Panduragan Dept of Nursing UKMMC
Learning outcome �Define Palliative nutrition and hydration. �Carry out family teaching on Palliative nutrition. �Discuss the moral, medical and ethical issues surrounding proviion of artificial nutrition in terminal stages.
Satisfying Patient desires �The primary goal of nutrition in terminal illness is pt comfort �Achievement of ideal weight with metabolic balance is not realistic in progressive end-stage disease. �Diet restriction is rarely necessary. �It is common for patients sweets to proteins and fats.
Optimizing intake and comfort �Pts who are ill will have early satiety. �Offering small but more frequent feeding will optimize intake and result in increased comfort. . �Encourage high protein/high-calorie diet, such as eggs, milk shakes, custards, cream soups etc. �Powdered nutritional supplements can be added to other foods without adding volume. �Do not force foods that cause a metalic or bitter taste. These are usually red meat; fish or poultry can be offered.
Con’t �If pt can’t take meat, try eggs, cheese, or beans for protein. �Provide food whenever the pt expresses hunger; do not wait for mealtime or expect the pt to eat three meals a day. �Encourage intake gently without pressure. �Remove food from patient when the pt I finished. �Offer favorite foods; except changes from previous preferences. �Make atmosphere and food presentation as pleasant as possible. �To conserve energy and/or reduce frustration, use “sippy cups” or large straws.
Con’t �Steroids may stimulate appetite; discontinue if side effects outweigh benefits. �Have ill-fitting dentures relined if this is a problem
Pt on tube feeding �The most common and serious complication of tube feeding is aspiration into the lungs. �Aspiration may be due to stomach overloading, vomiting, poor sphincter control, or tube migration. �Frequent testing of residual in the stomach is necessary to determine the amount and frequency of feeding possible without overloading. �Elevation of the head after feeding is helpful. �Other complications can be erosion and inflammation of tissues around the tubing.
Pt control �Permitting pt to be in control is the best way to maximize intake while minimizing discomfort. �The hospice team can assist in three ways: a. Establishing patient’s wishes b. Planning interventions and ameliorating distressing symptoms. c. Providing supportive teaching to family and friends. The distresses of forced feeding can result in discomfort and poor quality of life
Relieving symptoms with parental hydration �Confusion and mental cloudiness from long-acting metabolites of morphine may be alleviated with hydration. �Parental nutrition is preferable over intravenous of administration of fluids because it has less potential for infection.
Family teaching �Giving of food and fluid has a symbolic importance of love. �It is difficult for family members to accept the changes in the nutritional in take of the patients. For most caregivers and family members it involves an adjustment process. �It is important to discuss and have printed handout with following information: - Nutritional needs change as illness advances - Taste and smell changes – avoid offensive odors - provide good hygiene - Dry mouth – serve moist food - liquids may be sipped as desired - frozen juice pops may be appealing
Con’t � Sore throat and mouth - Provide soft cold food, avoid hot food - Avoid acidic , salty, spicy or hard and crunchy food - Assess and treat infections - Use topical analgesic medicine � Dysphagia - Feed the portion that best facilitates swallowing � Nausea and vomiting - Administer indicated medication - Avoid fatty, spicy, odorous or bulky food - Avoid talking abt food in the presence of a person who is nauseous.
Con’t �Early Satiety or Bloating - Offer small, frequent feedings - Avoid carbonated beverages and gas producing foods �Diarrhea - Investigate the cause for diarrhea - Serve lomotil if necssary

THANK YOU
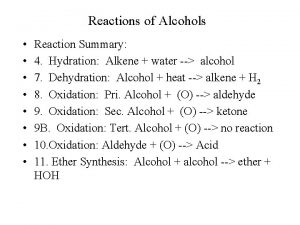
 Pros and cons of artificial nutrition and hydration
Pros and cons of artificial nutrition and hydration How can an na best help residents with eating?
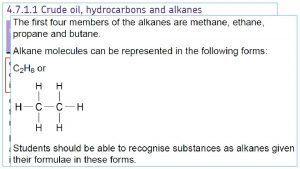
How can an na best help residents with eating? Chapter 8 nutrition and hydration
Chapter 8 nutrition and hydration Hydration of aldehydes and ketones
Hydration of aldehydes and ketones Hydration vs hydrogenation
Hydration vs hydrogenation Hydration alkene
Hydration alkene Covalent bond of ethanol
Covalent bond of ethanol Hydration level chart
Hydration level chart Is acid catalyzed hydration syn or anti
Is acid catalyzed hydration syn or anti Hydrogen halide example
Hydrogen halide example Is acid catalyzed hydration syn or anti
Is acid catalyzed hydration syn or anti Mercury catalyzed hydration of alkynes
Mercury catalyzed hydration of alkynes Mercury catalyzed hydration of alkynes
Mercury catalyzed hydration of alkynes Is acid catalyzed hydration syn or anti
Is acid catalyzed hydration syn or anti