Nutrition and Hydration 24 April 2020 Chido Muchaneta




- Slides: 17
Nutrition and Hydration 24 April 2020 Chido Muchaneta, Clinical and Professional Educator

National statistics One in ten people over 65 years in the UK are malnourished.
What is malnutrition? Malnutrition is a serious condition that happens when your diet does not contain the right amount of nutrients, ‘poor nutrition’ and can refer to: • Undernutrition – not getting enough nutrients • Over nutrition – getting more nutrients than needed Undernutrition can occur in those that are not underweight but do not have enough of some nutrients so do not have a balanced diet. 3
BMI and how to calculate Resources: • What is BMI https: //www. nhs. uk/common-health-questions/lifestyle/what -is-the-body-mass-index-bmi/ • Calculating BMI https: //www. nhs. uk/live-well/healthy-weight/bmi-calculator/ 4
Symptoms of malnutrition Weight loss Most people who are malnourished will lose weight, but it's possible to be a healthy weight or even overweight and still be malnourished. For example, this can happen if you're not getting enough nutrients, such as some types of vitamins and minerals, through your diet. You could be malnourished if: • you unintentionally lose 5 to 10% of your body weight within 3 to 6 months • your BMI is under 18. 5 (although a person with a BMI under 20 could also be at risk) • clothes, belts and jewellery seem to become looser over time • You should see a GP/ Doctor if you have unintentionally lost a lot of weight over the past few months, as it may be a symptom of an underlying health condition • If a friend or family member has lost a lot of weight, talk to them about your concerns and encourage them to get help. 5
Other symptoms of malnutrition include: • • • reduced appetite lack of interest in food and drink feeling tired all the time feeling weaker getting ill often and taking a long time to recover wounds taking a long time to heal poor concentration feeling cold most of the time low mood or depression 6
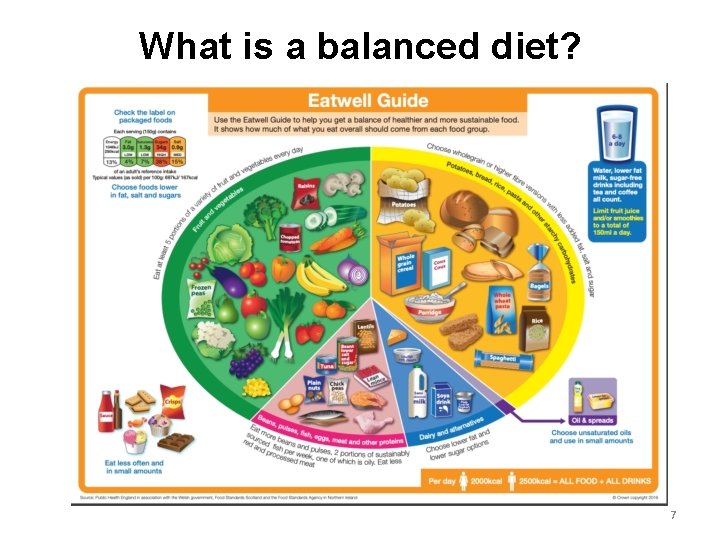
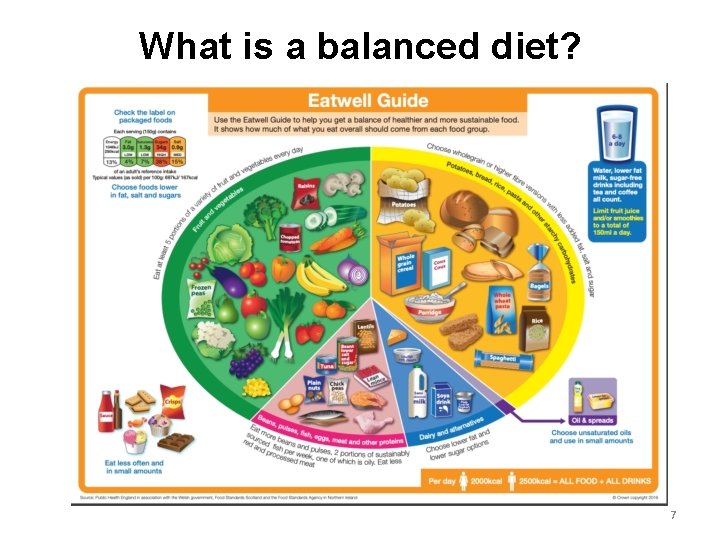
What is a balanced diet? 7
What is the current NHS advice? Visit the NHS Eat well page to read what the latest advice is: https: //www. nhs. uk/live-well/eat-well/theeatwell-guide/ 8

Malnutrition: snacking Snacking (eating small amounts regularly) to manage patients who are malnourished or at risk of malnourishment. • A good option for patients with poor appetite or feeling full too quickly. • Snacks high in fat, protein and carbohydrates are good options. • Mixed messages: snacking often seen negatively but is often essential for this patient group.
Importance of hydration ~ 70% of the body is water ~ 93% of blood is water
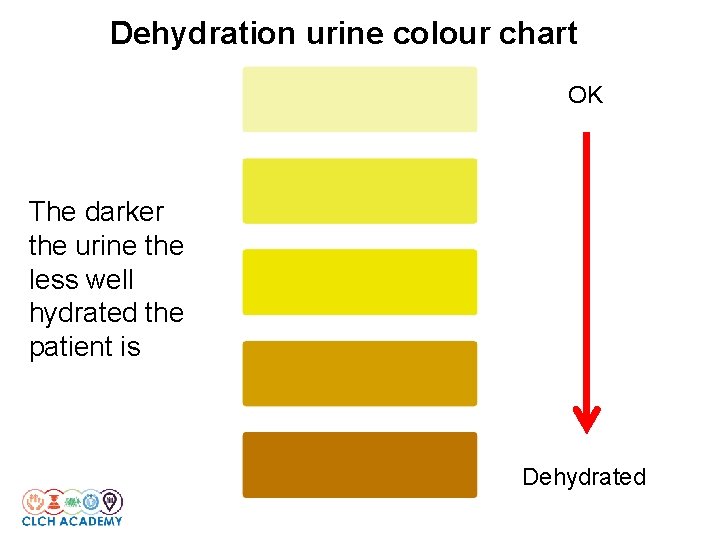
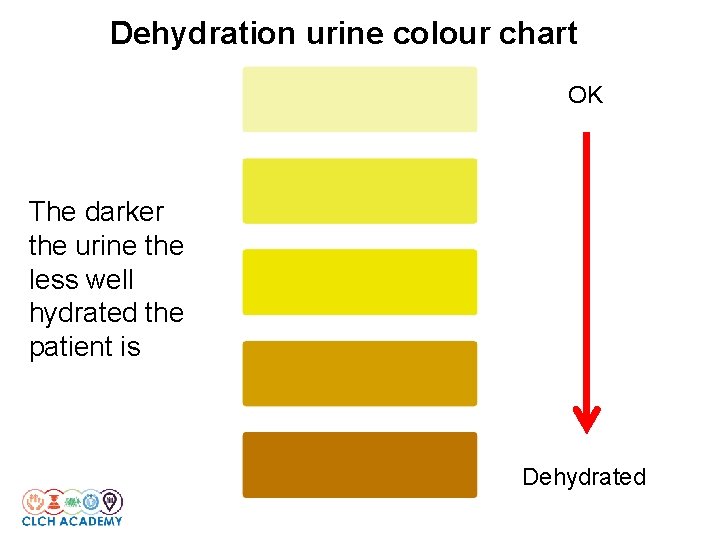
Dehydration urine colour chart OK The darker the urine the less well hydrated the patient is Dehydrated

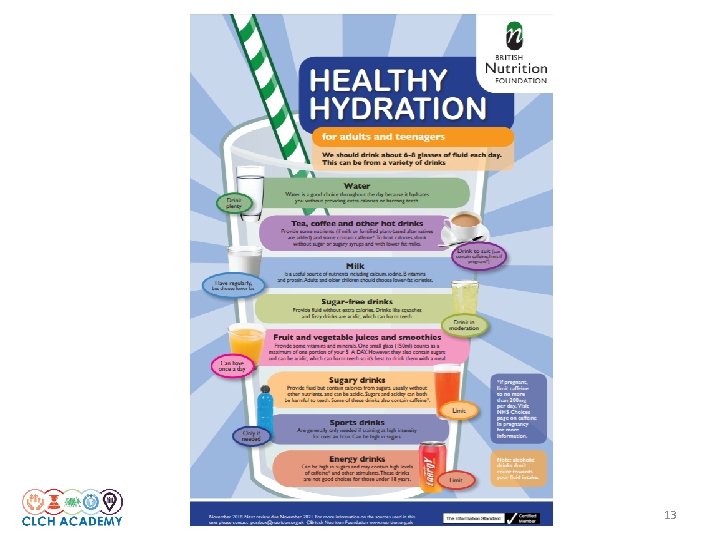
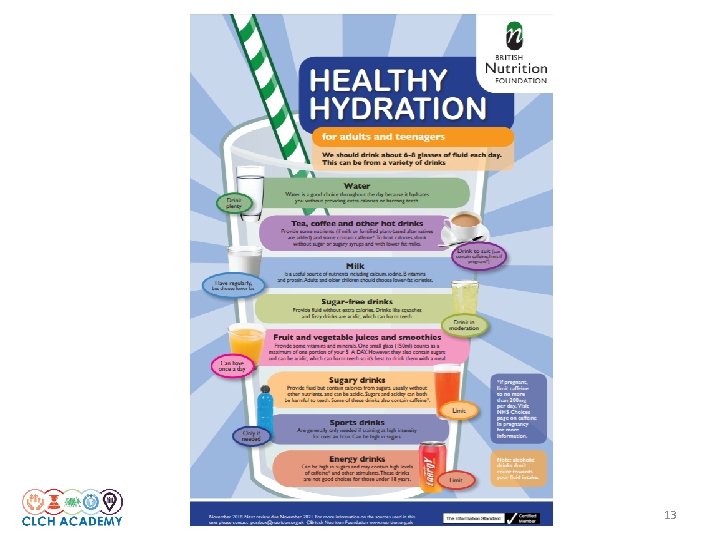
Hydration recommendation 6 to 8 glasses (1. 5 litres) minimum of fluids everyday
13
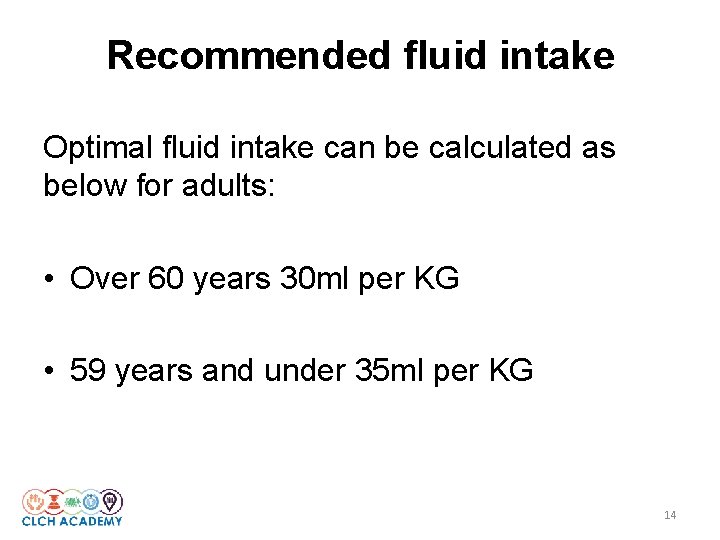
Recommended fluid intake Optimal fluid intake can be calculated as below for adults: • Over 60 years 30 ml per KG • 59 years and under 35 ml per KG 14
Monitoring fluid intake • Monitoring fluid intake and urine out put differs based on setting • In a formal clinical setting this should be recorded and documented • Drinks taken should be recorded, daily intake can then be compared with the recommended fluid intake and advice given accordingly • Every time the catheter bag is emptied the urine should be measured and recorded. • Reduction in urine output can be a sign of underlying heath concern – examples can be urinary tract infection, renal impairment, dehydration or sepsis (consider NEWS) 15
Food safety • Food hygiene and safety should apply in any settings where food is consumed, but particularly where there are vulnerable individuals who may suffer nutritional harm. • It is important to maintain nutritional vigilance at all times to ensure optimum health outcomes • Eat well, live well… 16

Five keys to safer food
 Pros and cons of artificial nutrition and hydration
Pros and cons of artificial nutrition and hydration Chido rodgers
Chido rodgers Nutrition and hydration chapter 15
Nutrition and hydration chapter 15 Chapter 8 nutrition and hydration
Chapter 8 nutrition and hydration Hydration of aldehydes and ketones
Hydration of aldehydes and ketones Hydration vs hydrogenation
Hydration vs hydrogenation Alkene reactions summary
Alkene reactions summary Dibromoethane
Dibromoethane Hydration level chart
Hydration level chart Is acid catalyzed hydration syn or anti
Is acid catalyzed hydration syn or anti Alkene reactions
Alkene reactions Syn addition
Syn addition Mercury catalyzed hydration of alkynes
Mercury catalyzed hydration of alkynes Mercury catalyzed hydration of alkynes
Mercury catalyzed hydration of alkynes Is acid catalyzed hydration syn or anti
Is acid catalyzed hydration syn or anti Oxidation weathering
Oxidation weathering Tors
Tors Wrestling weight certification calculator
Wrestling weight certification calculator