Ovarian Torsion Can we Save the Ovary Maria

- Slides: 14
Ovarian Torsion: Can we Save the Ovary? Maria Novoa 1, MD, Jonathan Friedman 2, MD, Maximiliano Mayrink 1, DO. 1 Department of Obstetrics and Gynecology, Mount Sinai Medical Center, Miami, Florida. 2 Department of Radiology, Mount Sinai Medical Center, Miami, Florida.
Introduction • Ovarian torsion is considered a surgical emergency. An estimated 2. 5 -7. 4% of all acute abdomen cases represent ovarian torsion. • Once the ovary is twisted, blood flow is blocked resulting in hemorrhage and congestion with further necrosis. The main parameter guiding surgeons’ decision to choose ovary sparing or removal of the adnexa is intraoperative assessment of the ovary. • Surgeons typically associate dark appearing ovaries with necrosis, and this is a common indication for oophorectomy. However, evidence suggests that despite a black appearance during surgery, ovaries recover function over time. • There are no reliable laboratory methods or imaging to predict ovarian necrosis in patients with ovarian torsion.
Objective • The purpose of this study is to analyze the correlation between visually necrotic ovaries and necrosis in histopathology, and to identify factors that could predict ovarian histopathologic necrosis.
Methods • Retrospective study from January 2014 to December 2018. • All women that were admitted to the hospital through the emergency room (ER) and were subsequently discharged with a diagnosis of ovarian torsion were included. Patients that were not admitted through the ER were excluded from the study.
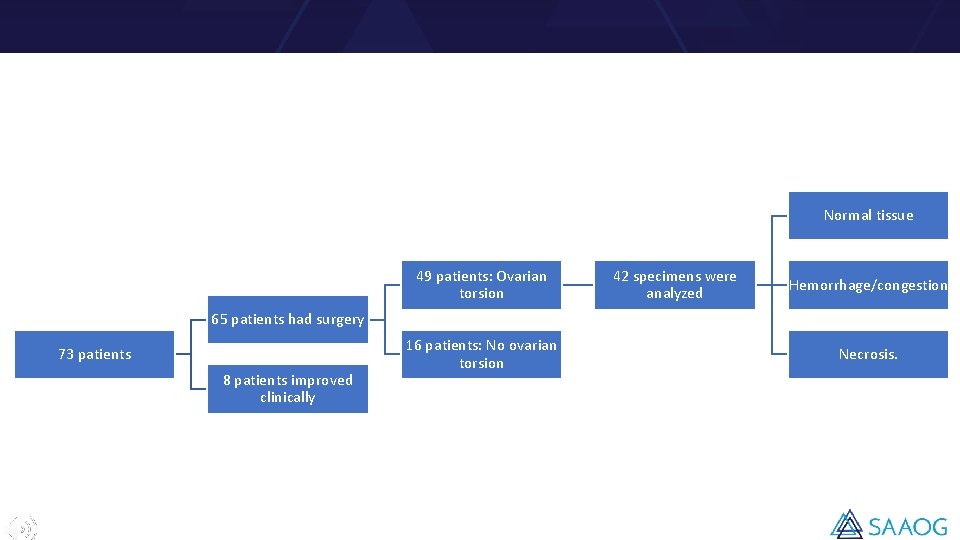
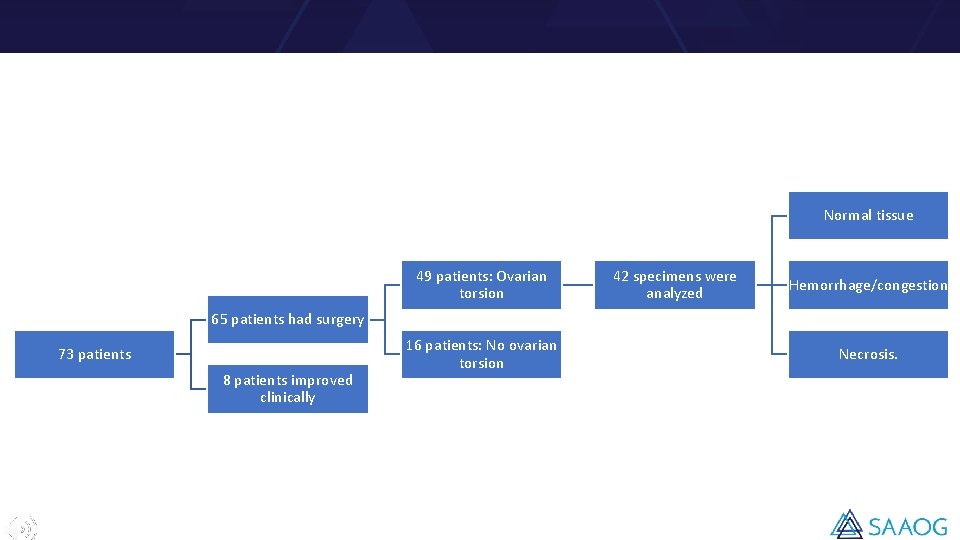
Normal tissue 49 patients: Ovarian torsion 42 specimens were analyzed Hemorrhage/congestion 65 patients had surgery 73 patients 8 patients improved clinically 16 patients: No ovarian torsion Necrosis.
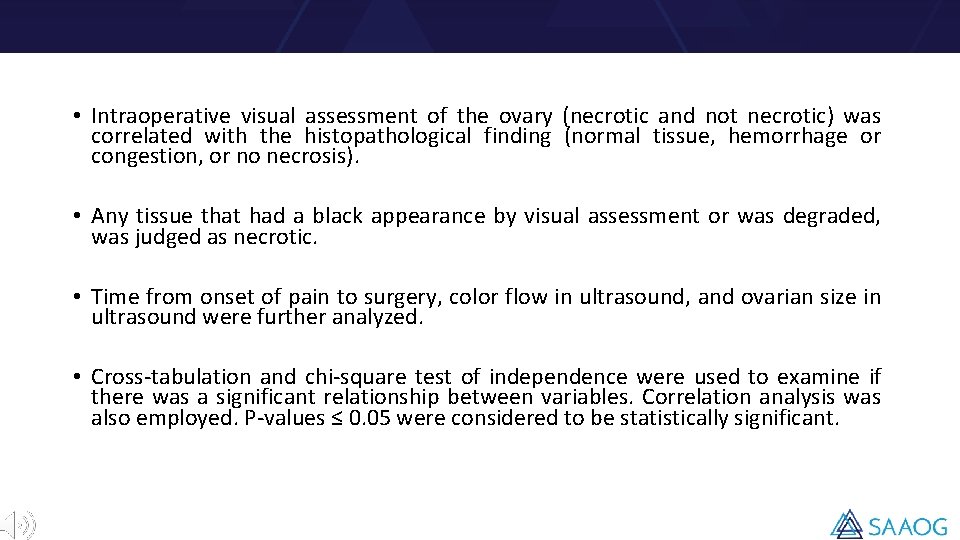
• Intraoperative visual assessment of the ovary (necrotic and not necrotic) was correlated with the histopathological finding (normal tissue, hemorrhage or congestion, or no necrosis). • Any tissue that had a black appearance by visual assessment or was degraded, was judged as necrotic. • Time from onset of pain to surgery, color flow in ultrasound, and ovarian size in ultrasound were further analyzed. • Cross-tabulation and chi-square test of independence were used to examine if there was a significant relationship between variables. Correlation analysis was also employed. P-values ≤ 0. 05 were considered to be statistically significant.
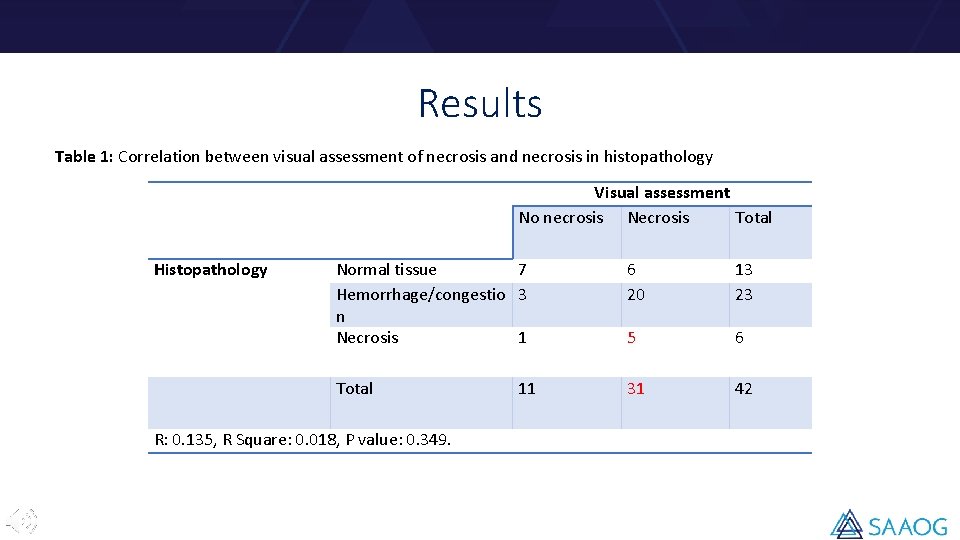
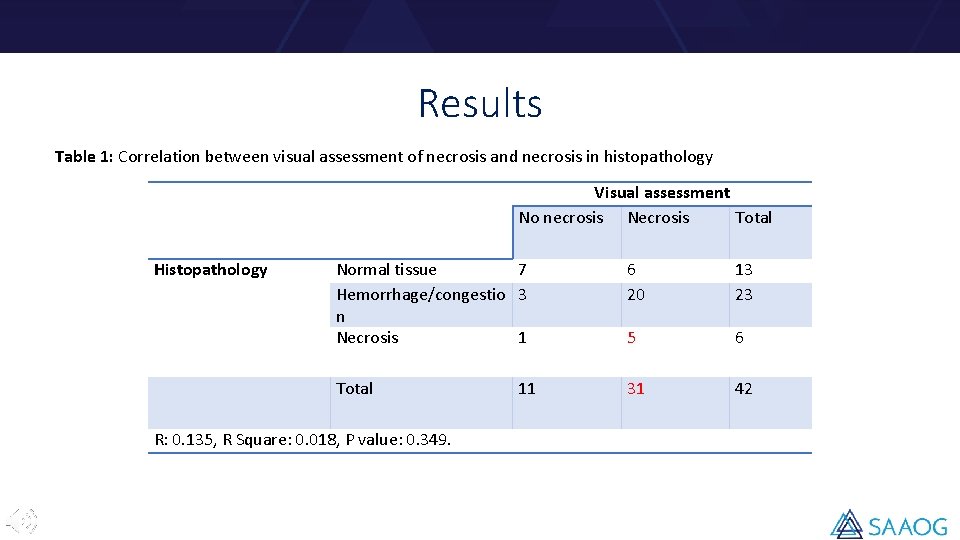
Results Table 1: Correlation between visual assessment of necrosis and necrosis in histopathology Visual assessment No necrosis Necrosis Total Histopathology Normal tissue 7 Hemorrhage/congestio 3 n Necrosis 1 6 20 13 23 5 6 Total 31 42 R: 0. 135, R Square: 0. 018, P value: 0. 349. 11
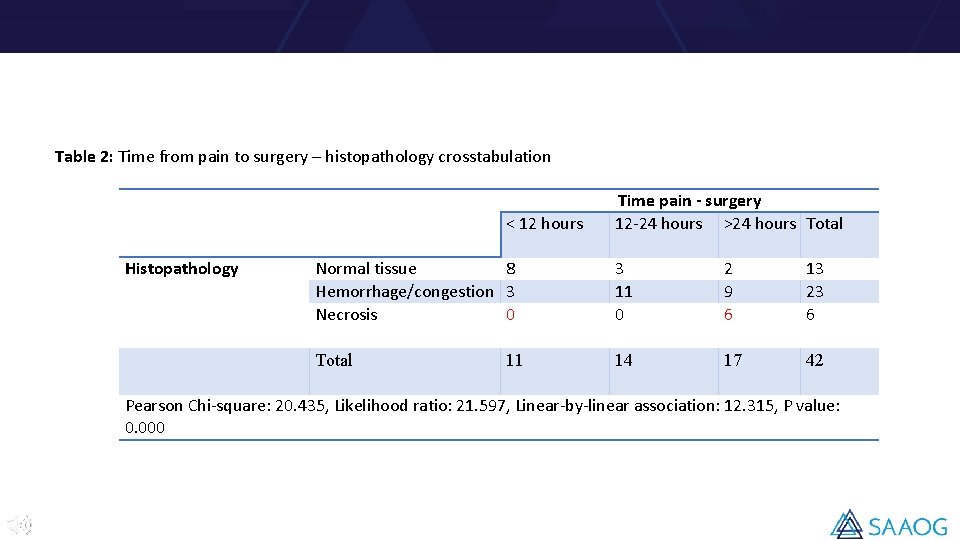
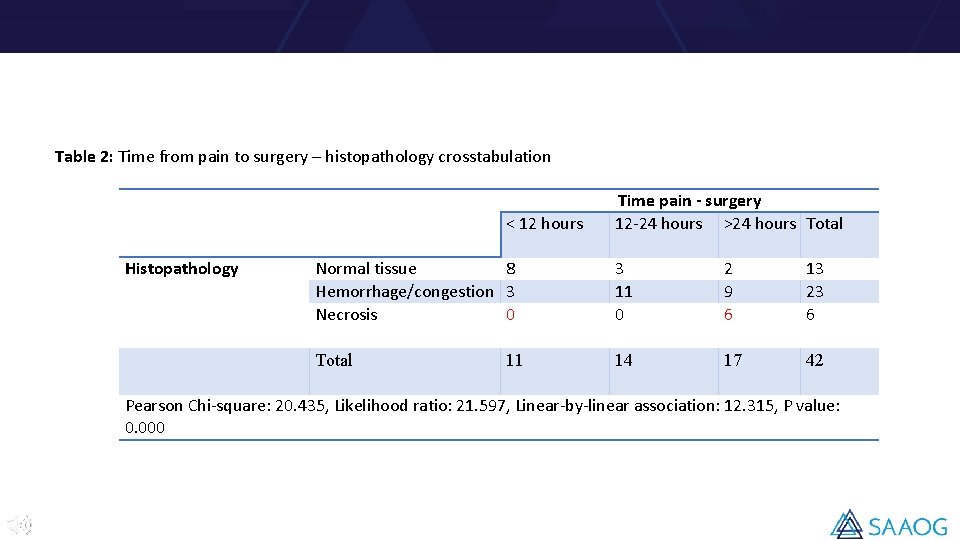
Table 2: Time from pain to surgery – histopathology crosstabulation < 12 hours Histopathology Time pain - surgery 12 -24 hours >24 hours Total Normal tissue 8 Hemorrhage/congestion 3 Necrosis 0 3 11 0 2 9 6 13 23 6 Total 14 17 42 11 Pearson Chi-square: 20. 435, Likelihood ratio: 21. 597, Linear-by-linear association: 12. 315, P value: 0. 000
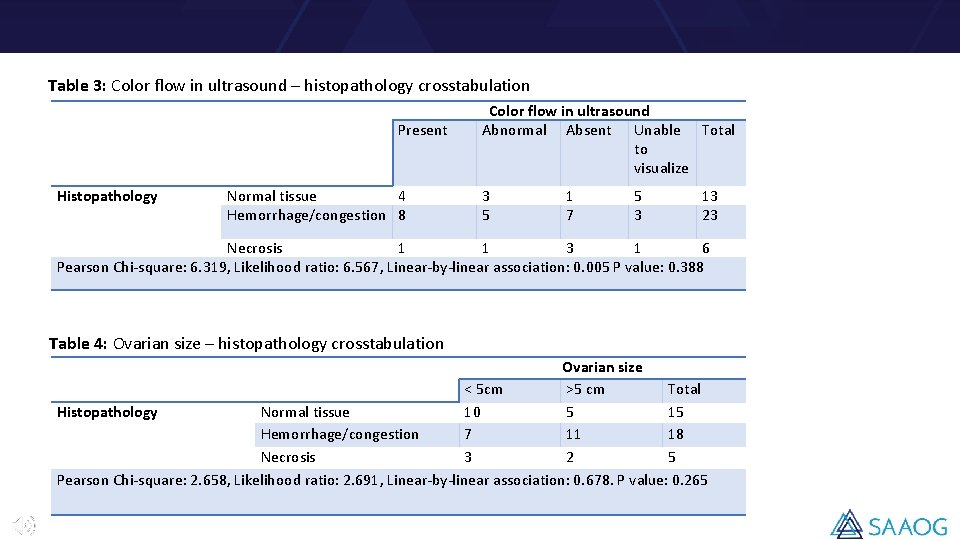
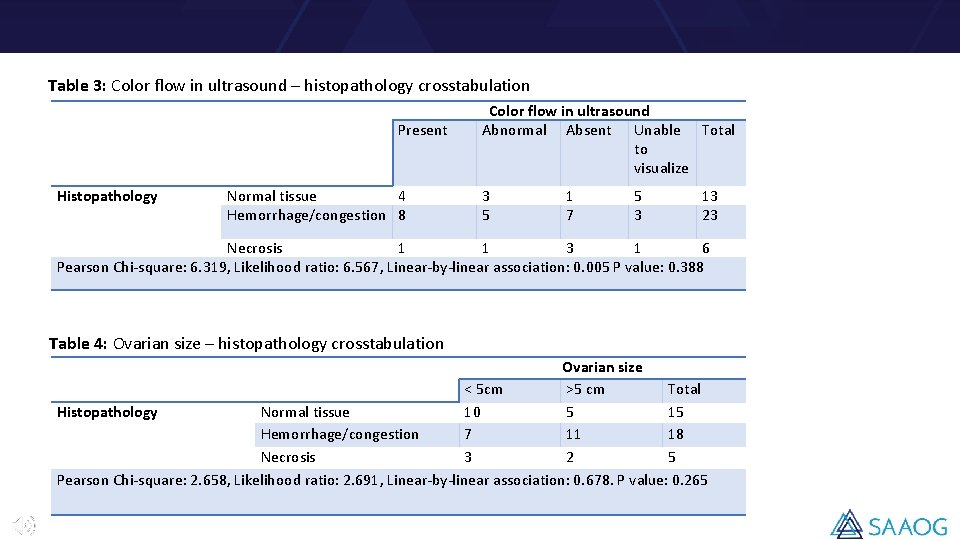
Table 3: Color flow in ultrasound – histopathology crosstabulation Present Histopathology Normal tissue 4 Hemorrhage/congestion 8 Color flow in ultrasound Abnormal Absent Unable Total to visualize 3 5 1 7 5 3 13 23 Necrosis 1 1 3 1 6 Pearson Chi-square: 6. 319, Likelihood ratio: 6. 567, Linear-by-linear association: 0. 005 P value: 0. 388 Table 4: Ovarian size – histopathology crosstabulation Ovarian size < 5 cm >5 cm Total Histopathology Normal tissue 10 5 15 Hemorrhage/congestion 7 11 18 Necrosis 3 2 5 Pearson Chi-square: 2. 658, Likelihood ratio: 2. 691, Linear-by-linear association: 0. 678. P value: 0. 265
Discussion • The diagnosis of ovarian torsion is ultimately confirmed visually during surgery. The surgical management is determined by many factors, including age, clinical and menopausal status, desire for future fertility, presence of additional ovarian pathology, and visual appearance of the ovary at the time of surgery. • Once ovarian torsion occurs, the ovary loses its blood supply, leading to hemorrhage and congestion, followed by ovarian necrosis, resulting in loss of the affected ovary. Ovarian necrosis is very challenging to detect before surgery. Our study demonstrates that even intraoperatively, visual assessment of necrosis is not a good predictor of necrosis in histopathology.
• Ovarian torsion results in decreased venous flow initially. Arterial flow is later compromised due to the less collapsible arterial walls, leading to necrosis. Unfortunately, the time frame in order to develop necrosis in patients with ovarian torsion is unknown. In our study, the time from the onset of abdominal pain to the surgery was significantly longer in the necrotic group when compared with the normal and congestive groups.

Conclusion • Intraoperative visual assessment of ovarian necrosis is not a good predictor of real necrosis in histopathology. • In patients with ovarian torsion, time is crucial. In order to preserve the ovary, surgical management should not be delayed.
Thank you!
 Komanda insert
Komanda insert Difference between save and save as
Difference between save and save as Hakim weatherspoon
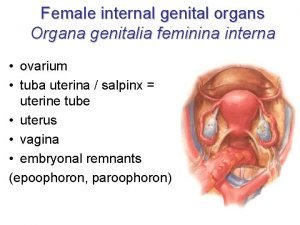
Hakim weatherspoon Funtions of ovary
Funtions of ovary Femaleanatomy
Femaleanatomy Ovarian cancer marker
Ovarian cancer marker Ovarian cyst rupture discharge look like
Ovarian cyst rupture discharge look like Labeled female reproductive system
Labeled female reproductive system Lig. teres uteri
Lig. teres uteri Ovarian cancer causes
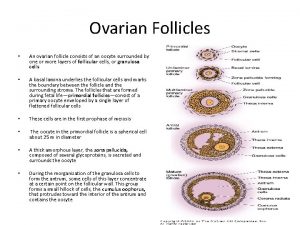
Ovarian cancer causes Ovarian follicle
Ovarian follicle Immature teratoma
Immature teratoma Ovarian cycle
Ovarian cycle Ovarian teratoma
Ovarian teratoma Corona radiata
Corona radiata