Older People in Acute Care Identification of need

- Slides: 12

Older People in Acute Care Identification of need and Care Planning Dr Cesar Rodriguez, NHS Tayside Dr Sridhar Valtheswaran, NHS Grampian Clinical Leads, OPAC Collaborative
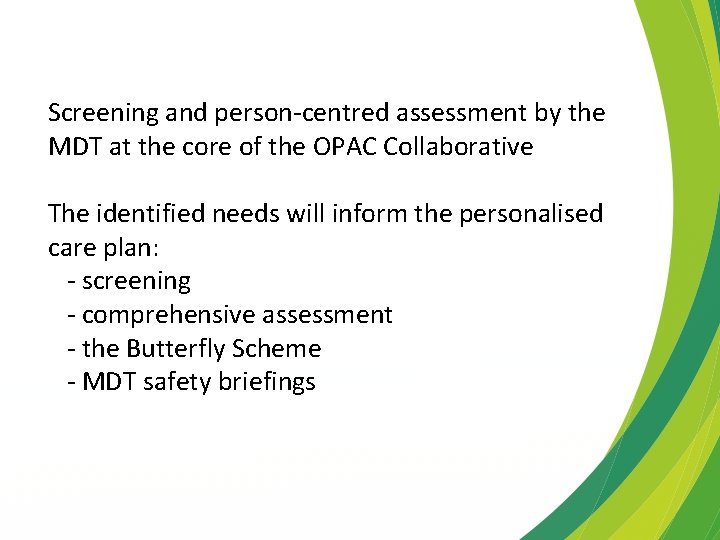
Screening and person-centred assessment by the MDT at the core of the OPAC Collaborative The identified needs will inform the personalised care plan: - screening - comprehensive assessment - the Butterfly Scheme - MDT safety briefings
We will focus on: 1. Screening for Comprehensive Geriatric Assessment 2. Delirium Pathway
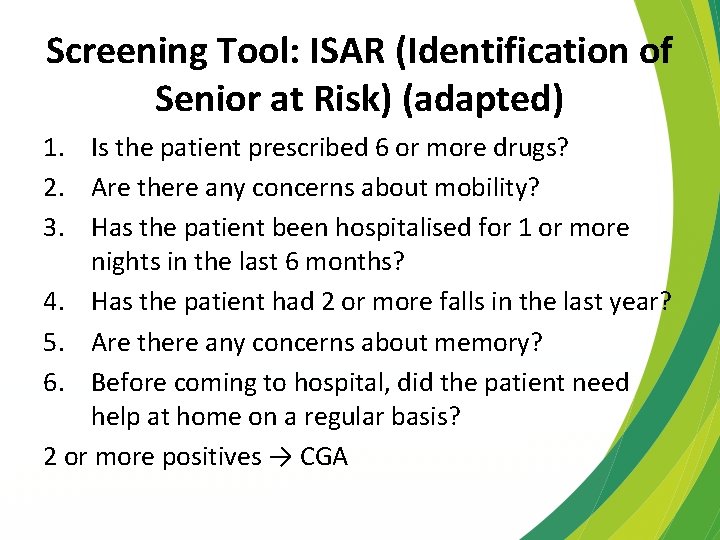
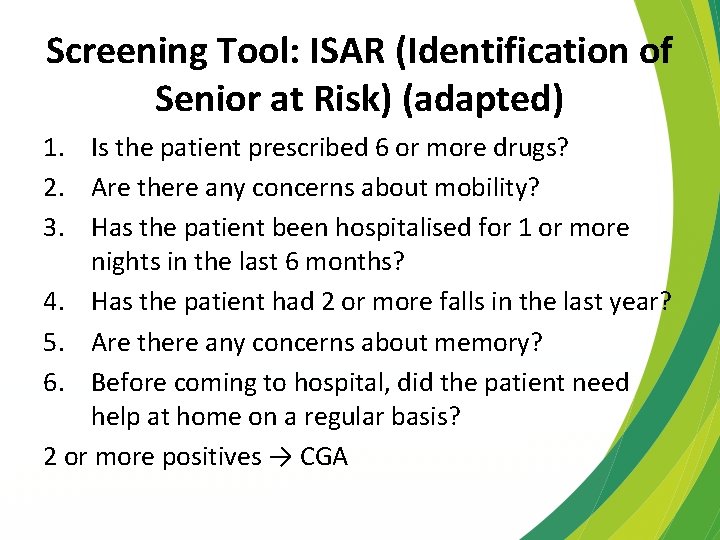
Screening Tool: ISAR (Identification of Senior at Risk) (adapted) 1. Is the patient prescribed 6 or more drugs? 2. Are there any concerns about mobility? 3. Has the patient been hospitalised for 1 or more nights in the last 6 months? 4. Has the patient had 2 or more falls in the last year? 5. Are there any concerns about memory? 6. Before coming to hospital, did the patient need help at home on a regular basis? 2 or more positives → CGA
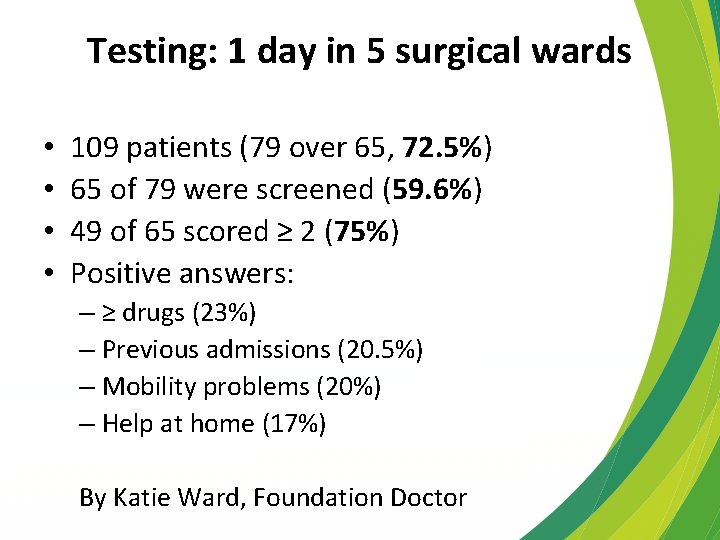
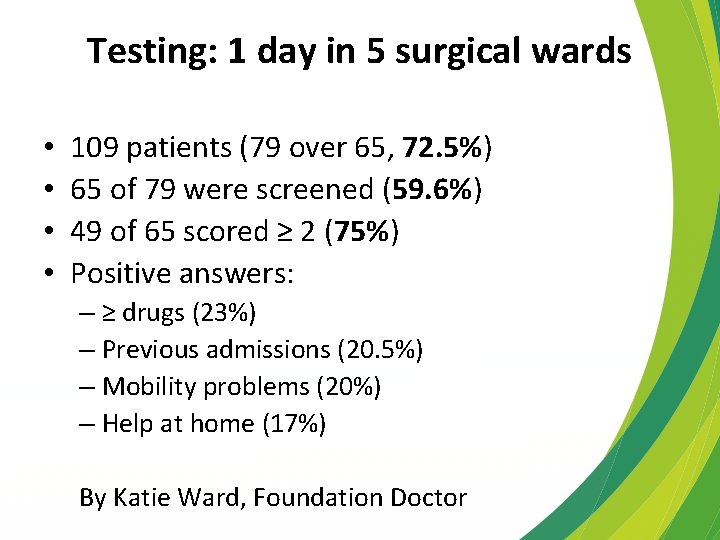
Testing: 1 day in 5 surgical wards • • 109 patients (79 over 65, 72. 5%) 65 of 79 were screened (59. 6%) 49 of 65 scored ≥ 2 (75%) Positive answers: – ≥ drugs (23%) – Previous admissions (20. 5%) – Mobility problems (20%) – Help at home (17%) By Katie Ward, Foundation Doctor
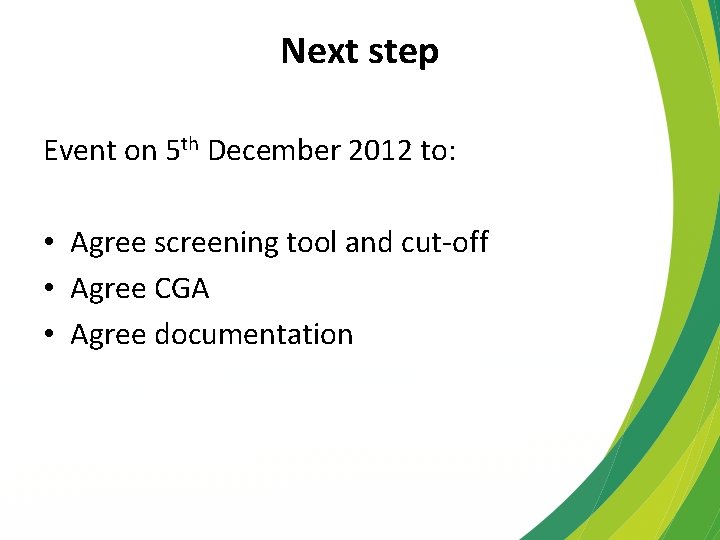
Next step Event on 5 th December 2012 to: • Agree screening tool and cut-off • Agree CGA • Agree documentation
Delirium pathway • Develop a pathway – Incorporate current good practice – Identify areas for improvement – Joint working & co-ordination • Test
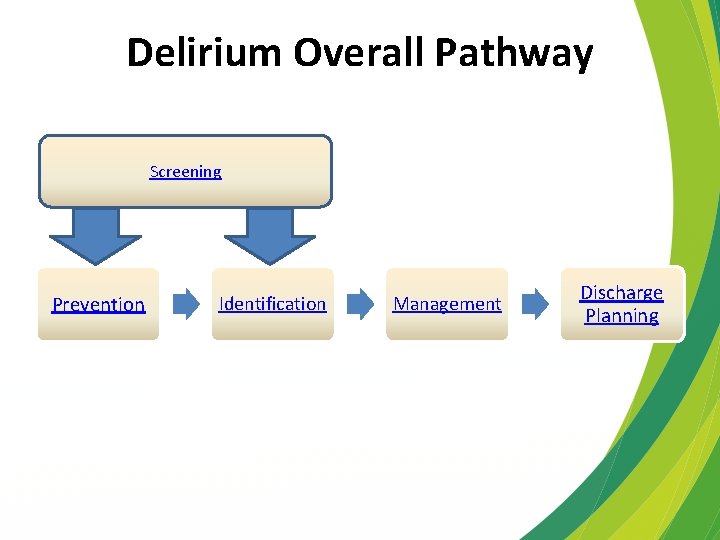
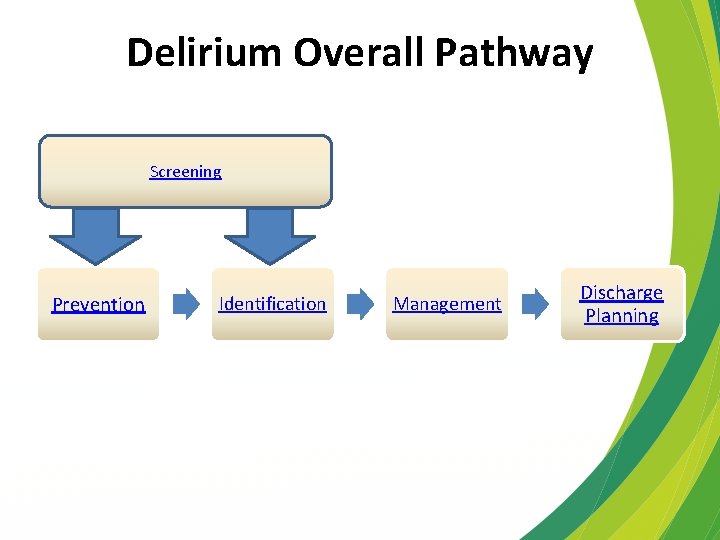
Delirium Overall Pathway Screening Prevention Identification Management Discharge Planning
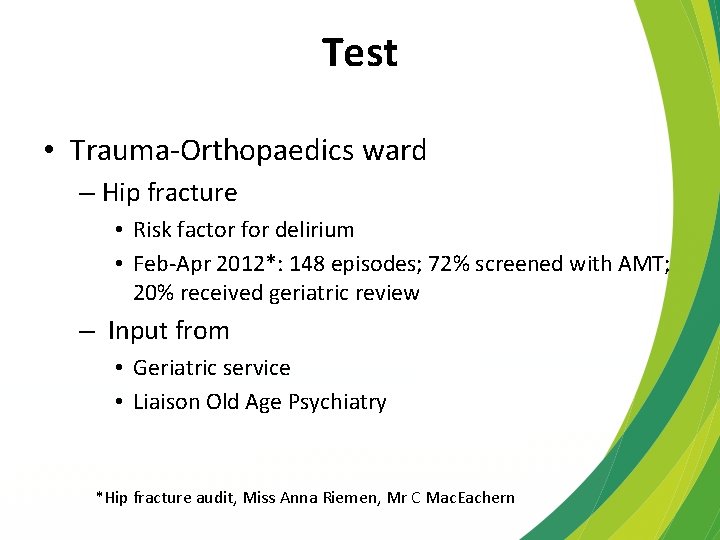
Test • Trauma-Orthopaedics ward – Hip fracture • Risk factor for delirium • Feb-Apr 2012*: 148 episodes; 72% screened with AMT; 20% received geriatric review – Input from • Geriatric service • Liaison Old Age Psychiatry *Hip fracture audit, Miss Anna Riemen, Mr C Mac. Eachern
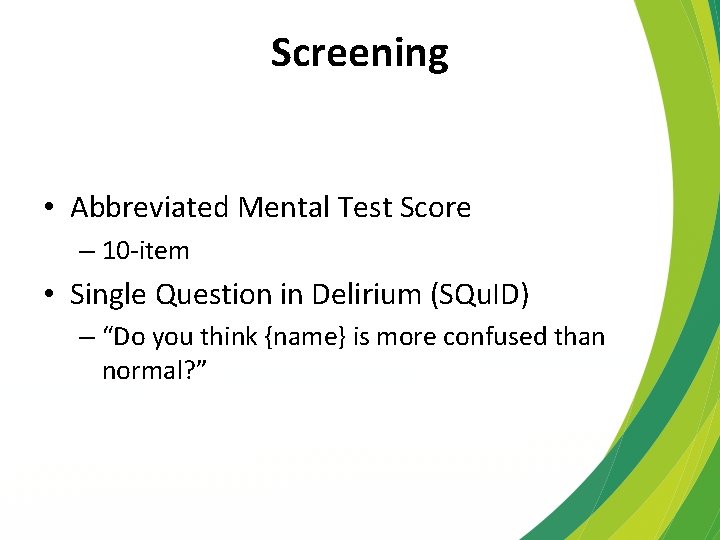
Screening • Abbreviated Mental Test Score – 10 -item • Single Question in Delirium (SQu. ID) – “Do you think {name} is more confused than normal? ”
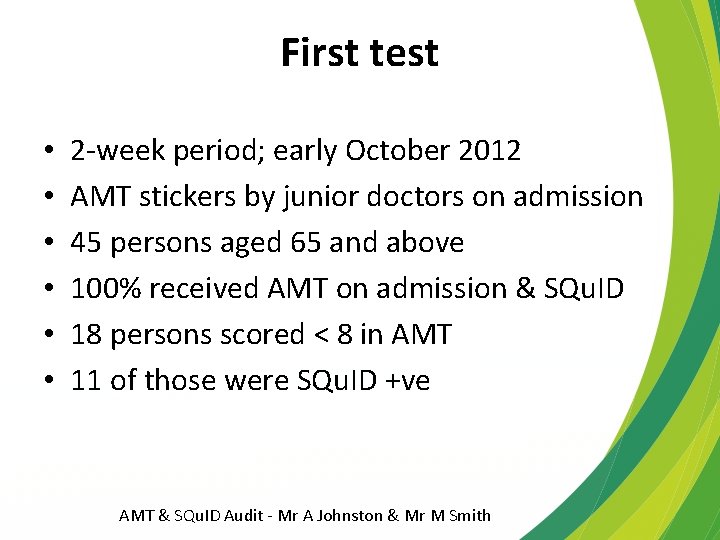
First test • • • 2 -week period; early October 2012 AMT stickers by junior doctors on admission 45 persons aged 65 and above 100% received AMT on admission & SQu. ID 18 persons scored < 8 in AMT 11 of those were SQu. ID +ve AMT & SQu. ID Audit - Mr A Johnston & Mr M Smith
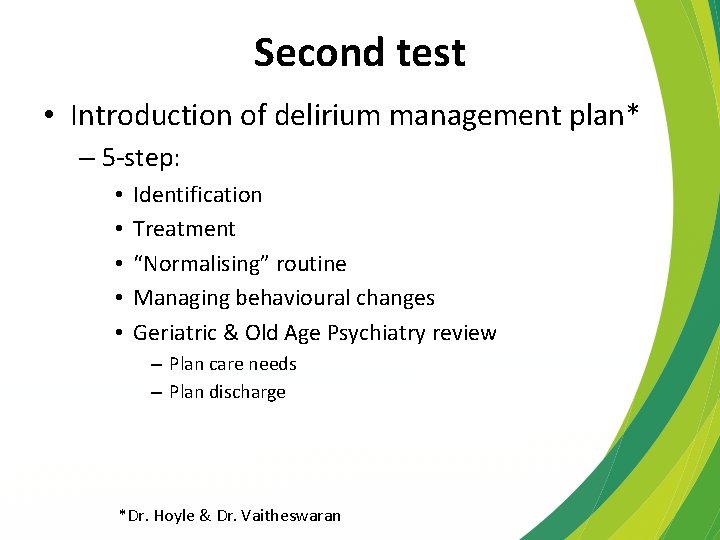
Second test • Introduction of delirium management plan* – 5 -step: • • • Identification Treatment “Normalising” routine Managing behavioural changes Geriatric & Old Age Psychiatry review – Plan care needs – Plan discharge *Dr. Hoyle & Dr. Vaitheswaran
 Life is older than the trees
Life is older than the trees As people grow older
As people grow older Presumptive identification vs positive identification
Presumptive identification vs positive identification Uncg erm
Uncg erm Proses identifying customer needs
Proses identifying customer needs Levels of care primary secondary tertiary
Levels of care primary secondary tertiary Acute care collaboration
Acute care collaboration Rcp acute care toolkit
Rcp acute care toolkit Nursing care plan for acute pancreatitis
Nursing care plan for acute pancreatitis Eschooltoday
Eschooltoday Why do people need information
Why do people need information Why do people need information
Why do people need information People need
People need