Noon Report CC Hip pain Peter Fong March










- Slides: 31

Noon Report CC: Hip pain Peter Fong March 23, 2020 Chief Facilitator: Riana Wurzburger
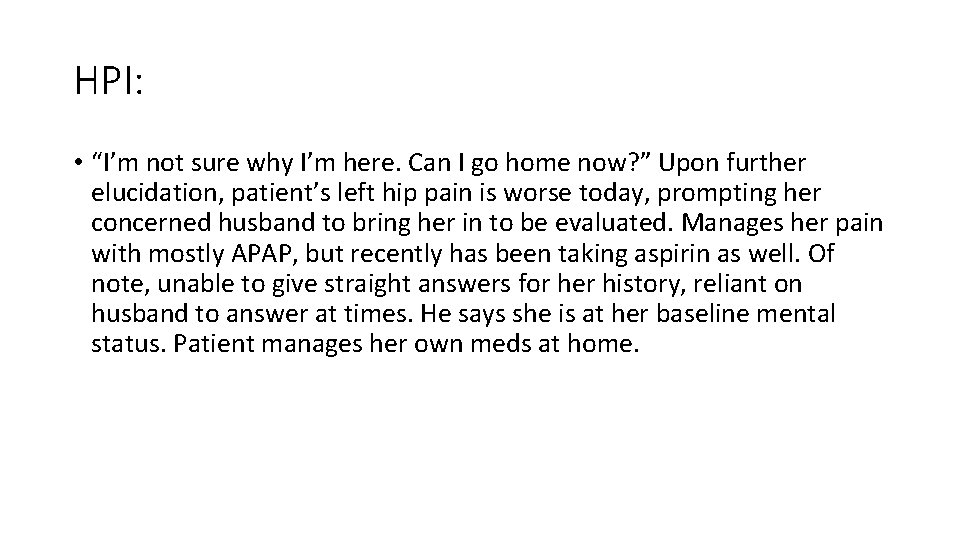
HPI: • “I’m not sure why I’m here. Can I go home now? ” Upon further elucidation, patient’s left hip pain is worse today, prompting her concerned husband to bring her in to be evaluated. Manages her pain with mostly APAP, but recently has been taking aspirin as well. Of note, unable to give straight answers for her history, reliant on husband to answer at times. He says she is at her baseline mental status. Patient manages her own meds at home.
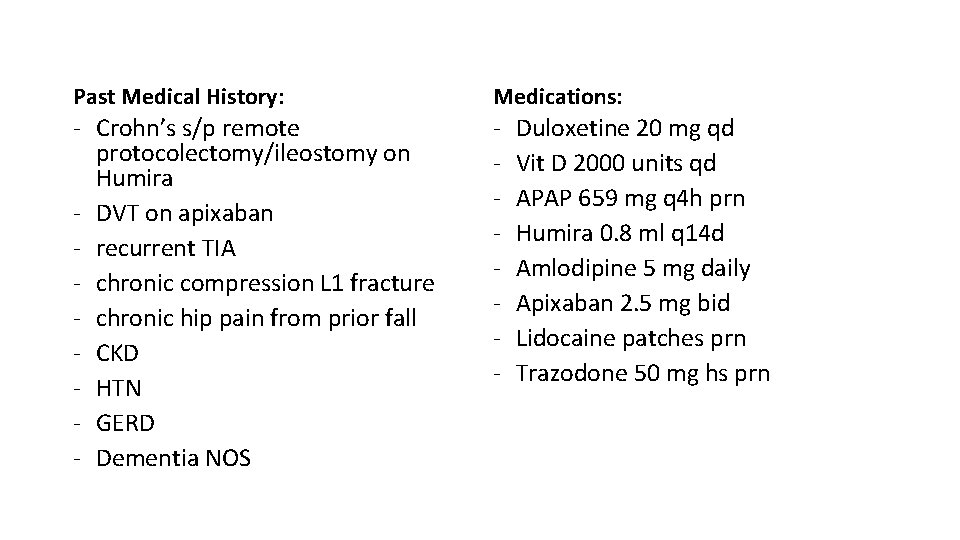
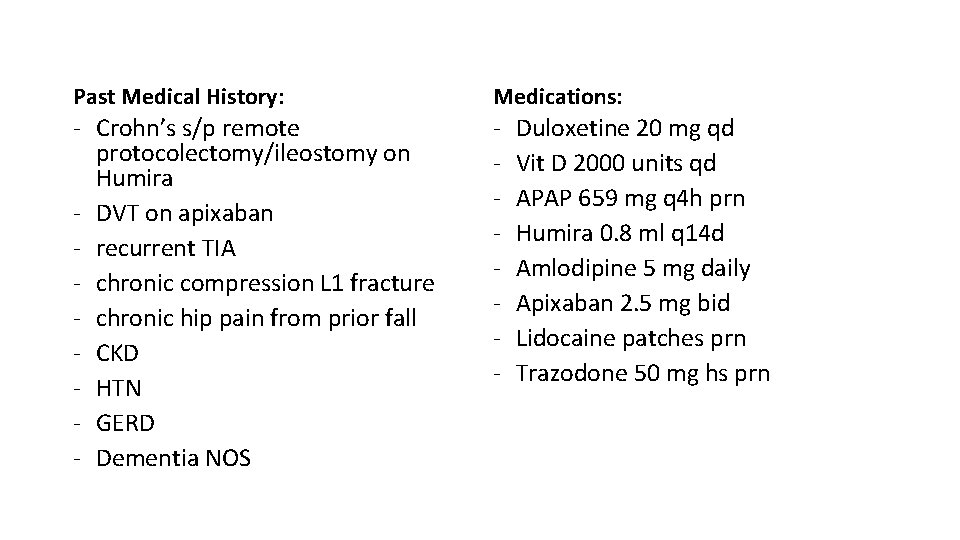
Past Medical History: Medications: - Crohn’s s/p remote protocolectomy/ileostomy on Humira - DVT on apixaban - recurrent TIA - chronic compression L 1 fracture - chronic hip pain from prior fall - CKD - HTN - GERD - Dementia NOS - Duloxetine 20 mg qd Vit D 2000 units qd APAP 659 mg q 4 h prn Humira 0. 8 ml q 14 d Amlodipine 5 mg daily Apixaban 2. 5 mg bid Lidocaine patches prn Trazodone 50 mg hs prn
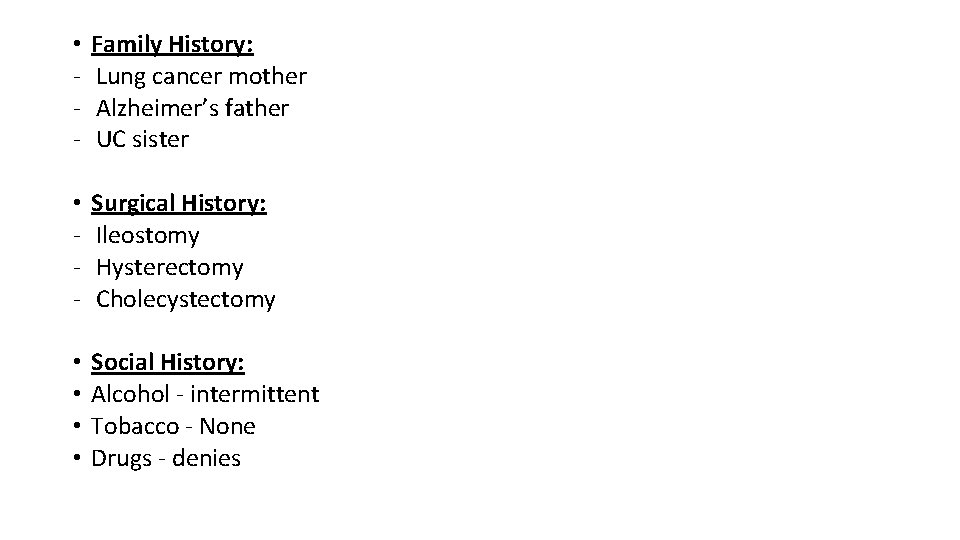
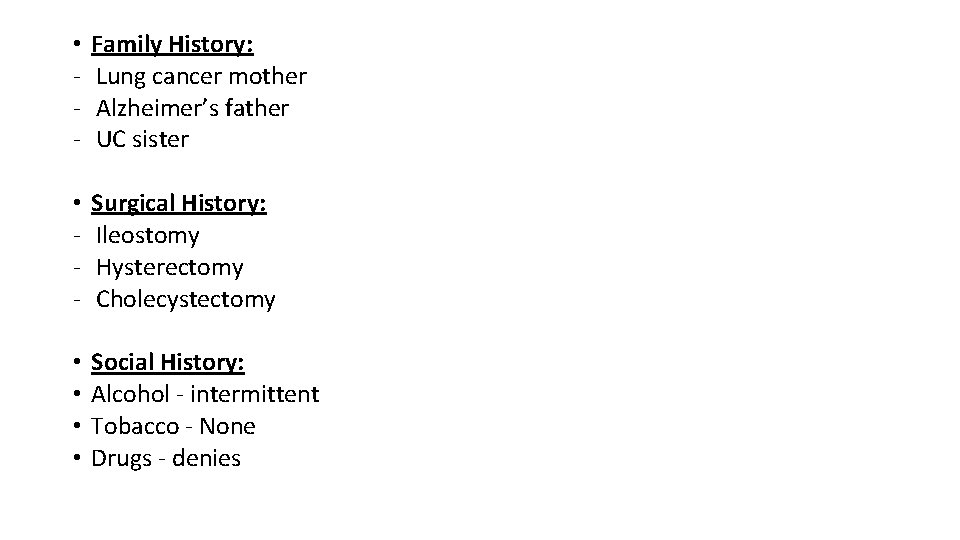
• - Family History: Lung cancer mother Alzheimer’s father UC sister • - Surgical History: Ileostomy Hysterectomy Cholecystectomy • • Social History: Alcohol - intermittent Tobacco - None Drugs - denies

What is your differential diagnosis? YIKES. Quite a broad differential at this point…let’s move on to the exam and see if that helps us narrow a bit.
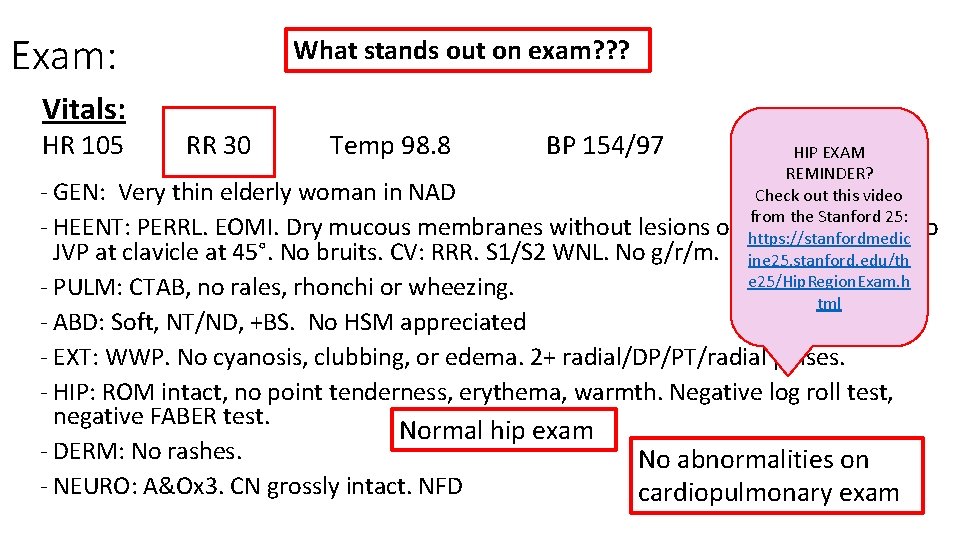
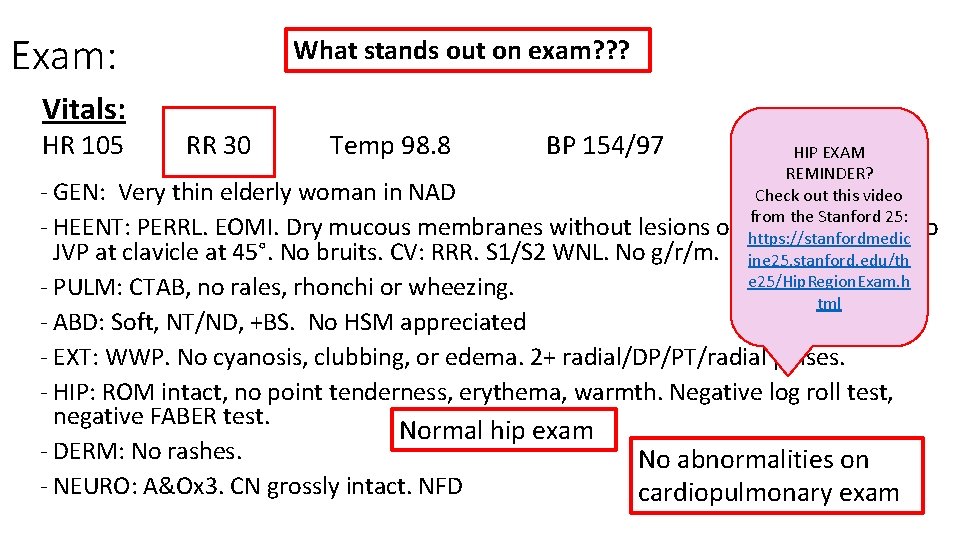
Exam: Vitals: HR 105 What stands out on exam? ? ? RR 30 Temp 98. 8 BP 154/97 O 2 100% HIP EXAM REMINDER? Check out this video from the Stanford 25: exudate. Neck: No https: //stanfordmedic ine 25. stanford. edu/th e 25/Hip. Region. Exam. h tml - GEN: Very thin elderly woman in NAD - HEENT: PERRL. EOMI. Dry mucous membranes without lesions or JVP at clavicle at 45°. No bruits. CV: RRR. S 1/S 2 WNL. No g/r/m. - PULM: CTAB, no rales, rhonchi or wheezing. - ABD: Soft, NT/ND, +BS. No HSM appreciated - EXT: WWP. No cyanosis, clubbing, or edema. 2+ radial/DP/PT/radial pulses. - HIP: ROM intact, no point tenderness, erythema, warmth. Negative log roll test, negative FABER test. Normal hip exam - DERM: No rashes. No abnormalities on - NEURO: A&Ox 3. CN grossly intact. NFD cardiopulmonary exam
How has your differential changed with the exam?

How Do You Approach Tachypnea? (RR >20) • HUGE DIFFERENTIAL (To name a few…) • Metabolic acidosis • Ketoacidosis, lactic acidosis, toxins (salicylates, alcohols) • Pulmonary • Pneumothorax, PE, PNA, exacerbation of chronic lung disease • Cardiac • ACS, arrhythmia, shock • Endocrine • Thyroid • Pain, anxiety, panic
What Labs & Imaging will you order?
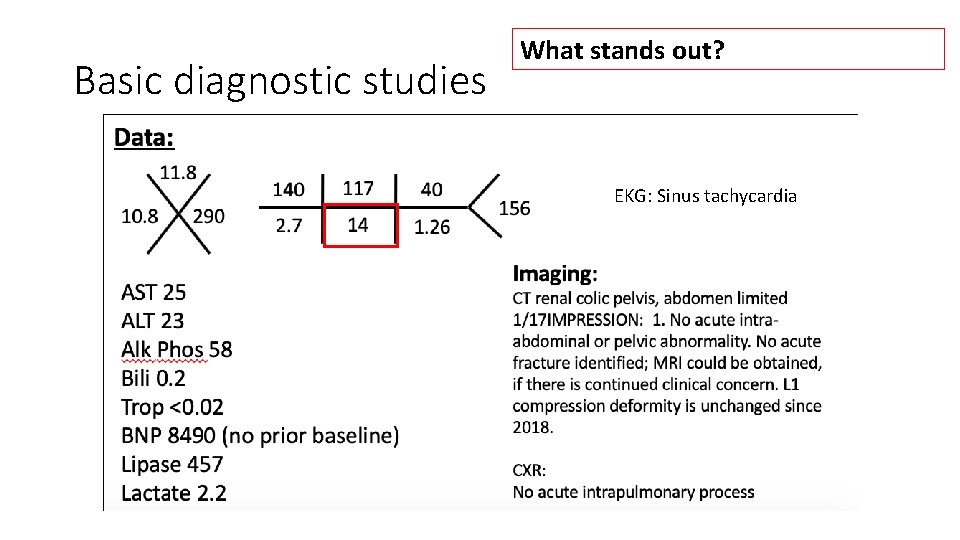
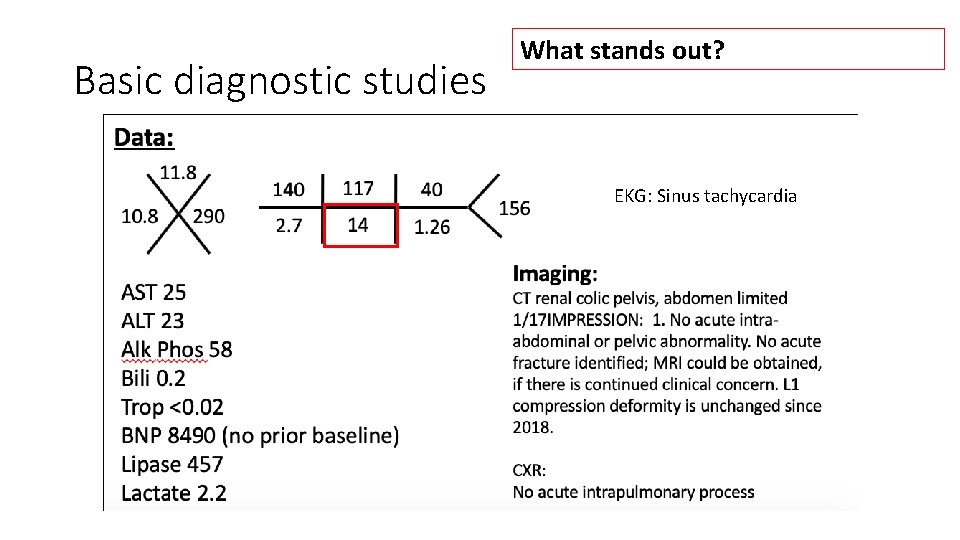
Basic diagnostic studies What stands out? EKG: Sinus tachycardia
Use the Following Slide to Put Together Your Summary Statement…

Past Medical History: - Crohn’s s/p remote protocolectomy/ileostomy on Humira DVT on apixaban recurrent TIA chronic compression L 1 fracture chronic hip pain CKD HTN GERD Dementia NOS Medications: - Duloxetine 20 mg qd Vit D 2000 units qd APAP 659 mg q 4 h prn Humira 0. 8 ml q 14 d Amlodipine 5 mg daily Apixaban 2. 5 mg bid Lidocaine patches prn Trazodone 50 mg hs prn 77 year old F CC: left hip pain Family History: HPI: -- “I’m not sure why I’m here. Can I go home now? ” Upon further elucidation, patient’s left hip pain is worse today, prompting her concerned husband to bring her in to be evaluated. Manages her pain with mostly APAP, but recently has been taking aspirin as well. Of note, unable to give straight answers for her history, reliant on husband to answer at times. He says she is at her baseline mental status. Patient manages her own meds at home. Vitals: HR 105 RR 30 Temp 98. 7 BP 154/97 O 2 100% Physical Exam: - GEN: Very thin elderly woman in NAD - HEENT: PERRL. EOMI. Dry mucous membranes without lesions or exudate. Neck: No JVP at clavicle at 45°. No bruits. CV: RRR. S 1/S 2 WNL. No g/r/m. - PULM: CTAB, no rales, rhonchi or wheezing. - ABD: Soft, NT/ND, +BS. No HSM appreciated - EXT: WWP. No cyanosis, clubbing, or edema. 2+ radial/DP/PT/radial pulses. - DERM: No rashes. - NEURO: A&Ox 3. CN grossly intact. NFD - Lung cancer mother Alzheimers father UC sister - Ileostomy Hysterectomy Cholecystectomy Surgical History: Social History: Alcohol - intermittent Tobacco - None Drugs - denies Data: 11. 8 10. 8 290 140 117 40 2. 7 14 1. 26 AST 25 ALT 23 Alk Phos 58 Bili 0. 2 Trop <0. 02 BNP 8490 (no prior baseline) Lipase 457 Lactate 2. 2 156 EKG: Sinus tachycardia Imaging: CT renal colic pelvis, abdomen limited 1/17 IMPRESSION: 1. No acute intraabdominal or pelvic abnormality. No acute fracture identified; MRI could be obtained, if there is continued clinical concern. L 1 compression deformity is unchanged since 2018. CXR: No acute intrapulmonary process

Key Features: • Unreliable historian who manages her own meds, with acute pain flare, taking aspirin • RR high at 30, CO 2 14

Summary Statement: An elderly woman with dementia presents with acute on chronic hip pain self-managed with APAP and Aspirin, found to have tachypnea without other evidence of respiratory distress, acidosis, and no abnormalities on pelvic imaging…
What Additional Labs Do You Want?

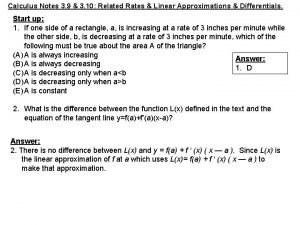
VBG 7. 37/ PCO 2 <20 / PO 2 <41 / HCO 3 11 (HCO 3 from the BMP was 14) What’s the primary acid-base disturbance? Is it appropriately compensated?

• VBG suggestive of a metabolic acidosis with a concurrent respiratory alkalosis • REMINDER: The Winters' Formula for Metabolic Acidosis Compensation Calculates the expected p. CO 2 compensation for a purely metabolic acidosis • 1. 5 x HCO 3 + 8 +/- 2 • Preferred ABG but we’ll use what we’ve got • Using Winter’s Formula in this case, an appropriate compensation would be PCO 2 of ~ 30 (not <20) In need of an acid-base reminder? Check out this curbsider’s episode!
Case continued…Just as you suspected… salicylate toxicity • Patient’s salicylate level of 42. 6 mg/d. L (ref range 15 to 30) • But hang on…I thought there would be an anion gap metabolic acidosis? • Anion gap calculated at 9 • You would typically expect to see a gap in acute cases of salicylate poisoning • However, in this case hyperchloremia/dehydration and sub-acute/chronic salicylate poisoning was confounding

Salicylate Toxicity, a quick review • SYMPTOMS: AMS, tinnitus, N/V, diarrhea, hyperpyrexia, noncardiac pulmonary edema, hypovolemia, arrhythmia, and coma • Peak 4 -6 hours, but may be delayed in cases of pylorospasm, bezoar formation, EC formulations. Reports of 35 hour peak level in one case • Intoxication >40 to 50 mg/d. L (2. 9 to 3. 6 mmol/L) • Therapeutic range is 10 to 30 mg/d. L (0. 7 to 2. 2 mmol/L) • Lower threshold for chronic poisoning • Fatal level approx. 10 to 30 g in adults and as little as 3 g by children (this references aspirin in particular)
Salicylate Toxicity, a quick review • Mechanism of toxicity • Inhibits cellular metabolism, krebs, oxidation metabolic acidosis • Activates respiratory center in medulla increase RR respiratory alkalosis • Stimulation of CTZ in medulla nausea and vomiting • Inhibits prostaglandins, prostacyclin, thomboxanes platelet dysfunction and GI mucosa injury
Salicylate Toxicity, a quick review • Other formulations • Oil of Wintergreen (methyl salicylate) • 1 teaspoon (5 ml) the equivalent of 21. 7 adult aspirin tabs • Used in Ben Gay, flavoring agent, Listerine mouthwash • Reportedly caused cross country runner’s death due to excessive application, a number pf case reports of toxicity with topicals • Salicylic acid topical for warts • Pepto-Bismol (bismuth subsalicylate) • 8. 7 mg of salicylic acid per ml
PAUSE. What Complications Are You Worried About? How Do You Treat Salicylate Poisoning?
Salicylate Toxicity: Therapeutic Considerations • Aspirin intoxication may cause cerebral glycopenia, despite a normal serum glucose, consider amp of dextrose initially, drip afterwards if any concern for altered mental status • Bicarb drip to alkalinize serum and urine, as salicylates are weak acids • Back off p. H >7. 6, otherwise alkalemia not a contraindication • May be limited by hypokalemia, as K+/H+ exchange in kidneys would limit alkalinization of urine, be aggressive in repleting • Hemodialysis if conservative measures not effective, or if serum levels exceed 100 mg/d. L suggestive of severe toxicity, lower thresholds may be considered in chronic toxicity
Salicylate Poisoning: Therapeutic Considerations • Other considerations for hemodialysis • • • AMS Pulmonary edema Cerebral edema AKI/CKD that impairs elimination Fluid overload that limits use of a bicarb drip p. H <7. 2 • Volume resuscitation, as these patients may be volume down 4 -6 L due to n/v, poor po intake, hyperthermia, hyperpnea, osmotic diuresis
Salicylate Poisoning: Therapeutic Considerations • Try to avoid intubation if possible, as difficult to match minute ventilation • Respiratory alkalosis helps prevent salicylates from traversing into CNS • Even short periods of hypoventilation can lead to clinical deterioration • Reserve for only patients hypoventilating, or w/ clear respiratory failure, match minute ventilation prior to intubation, up to 20 -30 L or more
Case Revisited: What Happened to our Patient? • Sodium Bicarb 150 m. Eq/1 L in D 5 W, run over 200 cc/hr • Salicylate levels down-trended down to 29 mg/d. L, “therapeutic range” within 12 hours, then to 19 mg/d. L at 18 hours, at which point bicarb drip was discontinued • Caution given BNP elevation, but no hx of heart failure, clinically appears volume down, CXR clear initially, but again, aspirin toxicity at risk for pulmonary edema • Aggressively repleted K+ to maintain alkaline urine • Did fine, discharged home with plan for medication assistance at home
A Brief Interlude into the Extracorporeal Removal of Toxins • Hemoperfusion (HP) in the past • Blood passing over charcoal cartridges • More time consuming, cartridges must be changed 2 -3 hours, etc • Disadvantages – can’t correct for acid-base • Molecular Adsorbent Recirculating System (MARS) • • Albumin circuit in addition to hemodialysis circuit More protein bound toxins May become more prevalent in future, too costly/cumbersome for now Limited data • CRRT vs intermittent HD • Less gradient with CRRT, avoid if at all possible, up to 50 -80% less effective than preferred HD

A Brief Interlude into the Extracorporeal Removal of Toxins • Drug criteria for dialysis • • Low volume of distribution <1 L/kg Molecular weight, typically lower ~ 15, 000 daltons, up to 50, 000 daltons Weak protein binding, not effective if >80% protein bound’ Endogenous clearance rate vs. hemodialysis removal rate • Dialysis can be run over 10 hours, as less risk for dialysis disequilibrium for these acute intoxications
Other toxins to consider for hemodialysis • APAP • TCA • Alcohols, i. e. methanol, ethylene glycol (antifreeze) • Consider fomepizole • Think high osmolar gap in unexplained gap acidosis • Lithium • Barbituates • Case reports in baclofen, dagibatran
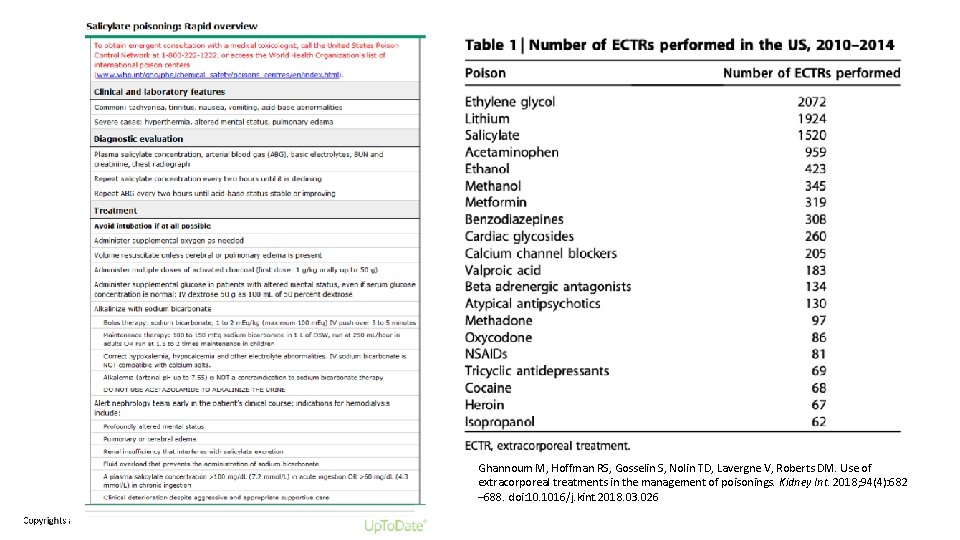
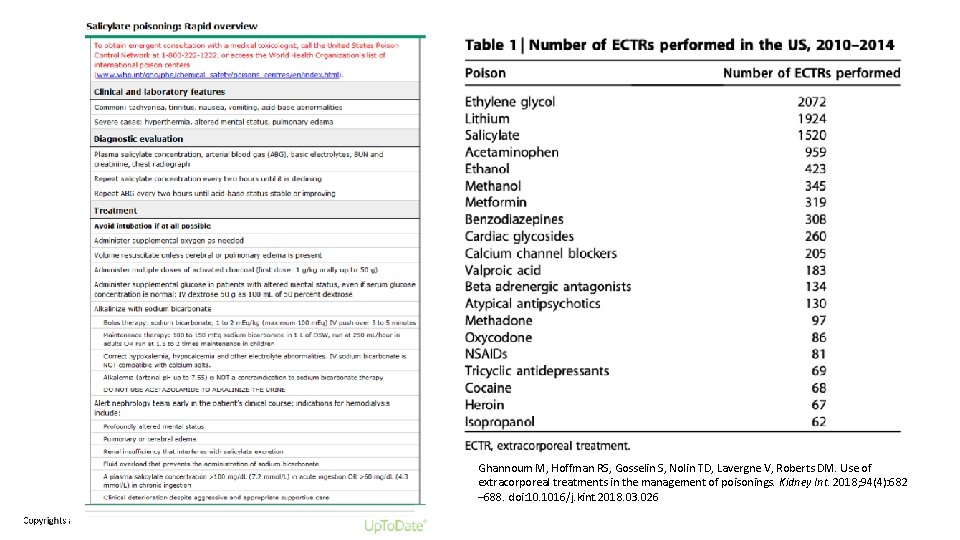
Ghannoum M, Hoffman RS, Gosselin S, Nolin TD, Lavergne V, Roberts DM. Use of extracorporeal treatments in the management of poisonings. Kidney Int. 2018; 94(4): 682 – 688. doi: 10. 1016/j. kint. 2018. 03. 026 Copyrights apply
References • Edward W Boyer, MD, Ph. D, Kathryn W Weibrecht, MD. Salicylate (aspirin) poisoning in adults. In: Up. To. Date, Stephen J Traub, MD (Ed), Up. To. Date, Waltham, MA, 2020. • Ghannoum M, Hoffman RS, Gosselin S, Nolin TD, Lavergne V, Roberts DM. Use of extracorporeal treatments in the management of poisonings. Kidney Int. 2018; 94(4): 682– 688. doi: 10. 1016/j. kint. 2018. 03. 026 • Approach to the hip region exam. Stanford Medicine 25. http: //stanfordmedicine 25. stanford. edu/the 25/Hip. Region. Exam. html • Matthew Watto. Acid base, boy bands, and grandfather clocks with Joel Topf. The Curbsiders Podcast. March 26, 2018. https: //thecurbsiders. com/show-notes/88 -acid-base-boy-bandsgrandfather-clocks-joel-topf-md
 Anthem of poland
Anthem of poland Hip hop hip to the hippity
Hip hop hip to the hippity Hip hop hip to the hippity
Hip hop hip to the hippity Mad pain
Mad pain Menstruation during pregnancy symptoms
Menstruation during pregnancy symptoms Pms or pregnancy
Pms or pregnancy Timothy fong ucla
Timothy fong ucla Eugene fong
Eugene fong Bruce fong dts
Bruce fong dts Disguises by jean fong kwok
Disguises by jean fong kwok Caroline fong
Caroline fong Moy fong menu
Moy fong menu Google translaze
Google translaze Swi prolog examples
Swi prolog examples Sandiway fong
Sandiway fong Fion fong
Fion fong Irene fong
Irene fong Dr warren fong
Dr warren fong Hwu timetable
Hwu timetable Ntu course induction
Ntu course induction Kristine fong
Kristine fong Metaphors about summer
Metaphors about summer High noon charmasson
High noon charmasson Magic tree house pirates past noon summary
Magic tree house pirates past noon summary What happens here
What happens here La loba negra tagalog
La loba negra tagalog Long term impacts of the industrial revolution
Long term impacts of the industrial revolution Jungle glade at hot high noon
Jungle glade at hot high noon Rules of noon sakinah
Rules of noon sakinah At noon ship a is 150 km west
At noon ship a is 150 km west Dumas lions club
Dumas lions club Mid day meal scheme poster
Mid day meal scheme poster