Natural History of Tricuspid Regurgitation Primary vs Secondary
- Slides: 16
Natural History of Tricuspid Regurgitation: Primary vs Secondary Jo. Ann Lindenfeld, MD Professor of Medicine Director , Heart Failures and Transplantation Vanderbilt Heart and Vascular Institute
Jo. Ann Lindenfeld, MD I have relevant financial relationships < Consultant: Relypsa, Resmed, Abbott, St. Jude, VWave, CVRx, Novartis, <Grants: Novartis, Astra Zeneca, NIH, AHA
Natural History of Tricuspid Regurgitation(TR) • Is TR associated with poorer survival? • Is the poorer survival associated due to the TR or the associated comorbidities or both? Primary TR Secondary TR
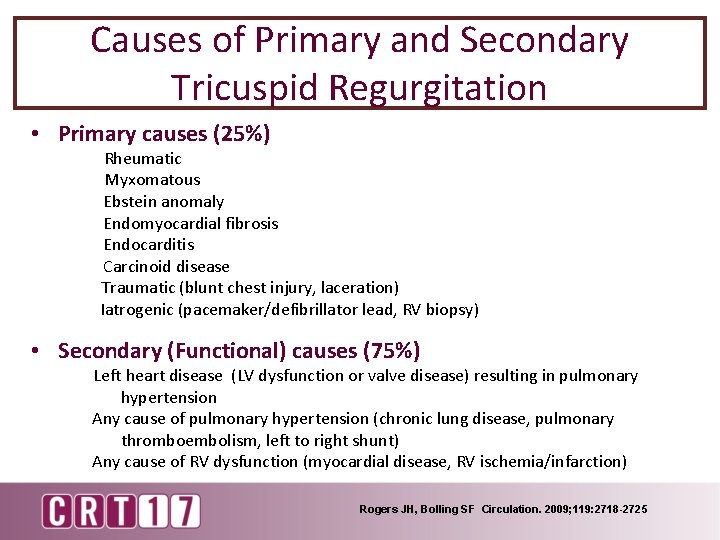
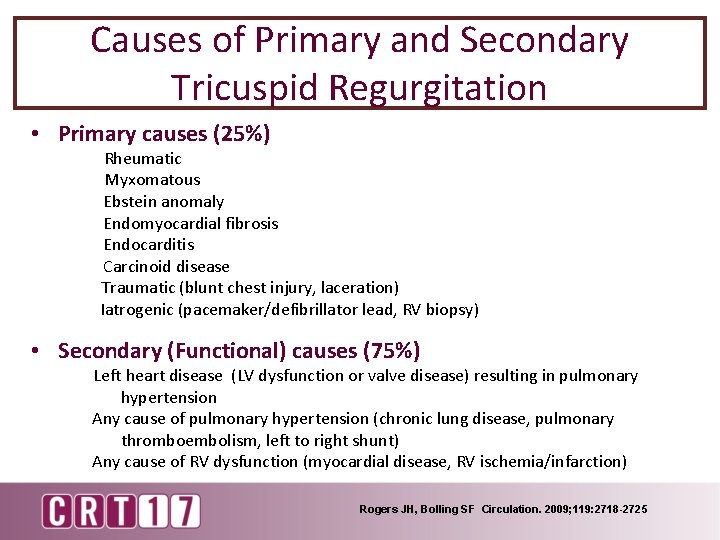
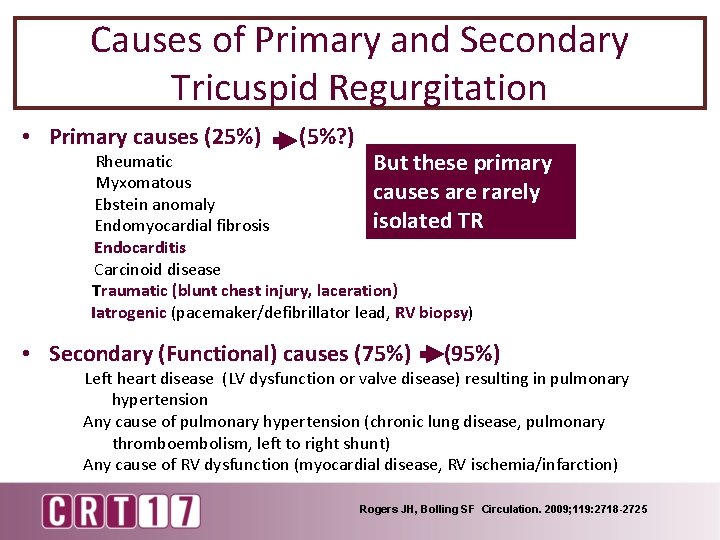
Causes of Primary and Secondary Tricuspid Regurgitation • Primary causes (25%) Rheumatic Myxomatous Ebstein anomaly Endomyocardial fibrosis Endocarditis Carcinoid disease Traumatic (blunt chest injury, laceration) Iatrogenic (pacemaker/defibrillator lead, RV biopsy) • Secondary (Functional) causes (75%) Left heart disease (LV dysfunction or valve disease) resulting in pulmonary hypertension Any cause of pulmonary hypertension (chronic lung disease, pulmonary thromboembolism, left to right shunt) Any cause of RV dysfunction (myocardial disease, RV ischemia/infarction) Rogers JH, Bolling SF Circulation. 2009; 119: 2718 -2725
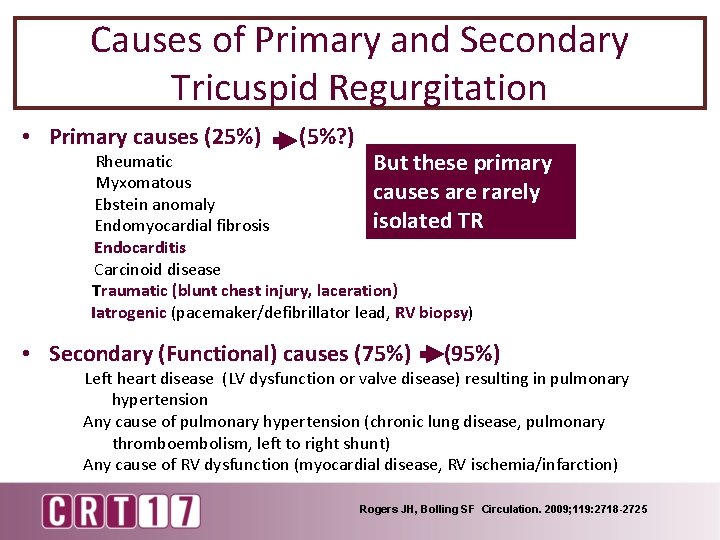
Causes of Primary and Secondary Tricuspid Regurgitation • Primary causes (25%) (5%? ) Rheumatic But these primary Myxomatous causes are rarely Ebstein anomaly isolated TR Endomyocardial fibrosis Endocarditis Carcinoid disease Traumatic (blunt chest injury, laceration) Iatrogenic (pacemaker/defibrillator lead, RV biopsy) • Secondary (Functional) causes (75%) (95%) Left heart disease (LV dysfunction or valve disease) resulting in pulmonary hypertension Any cause of pulmonary hypertension (chronic lung disease, pulmonary thromboembolism, left to right shunt) Any cause of RV dysfunction (myocardial disease, RV ischemia/infarction) Rogers JH, Bolling SF Circulation. 2009; 119: 2718 -2725
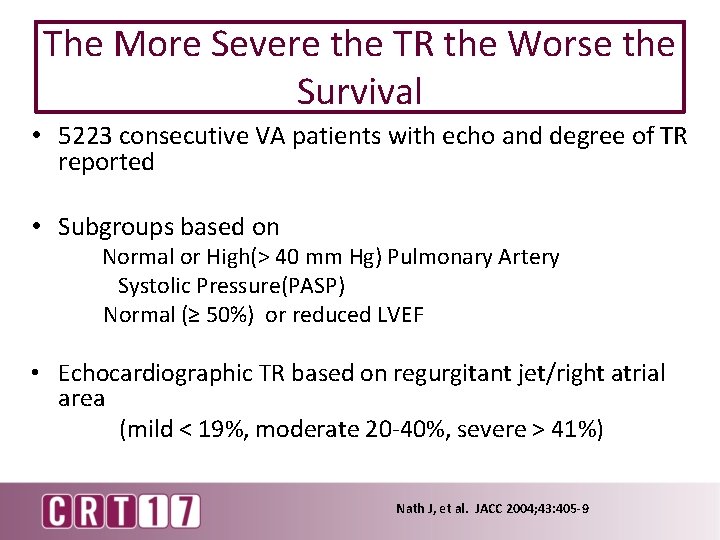
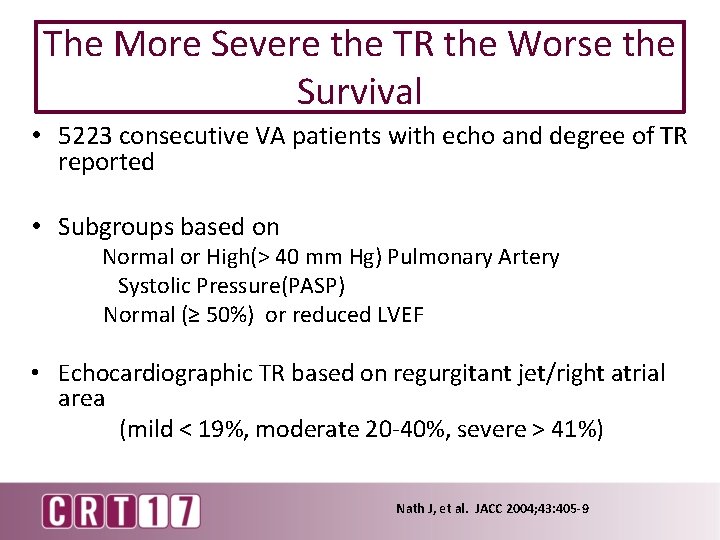
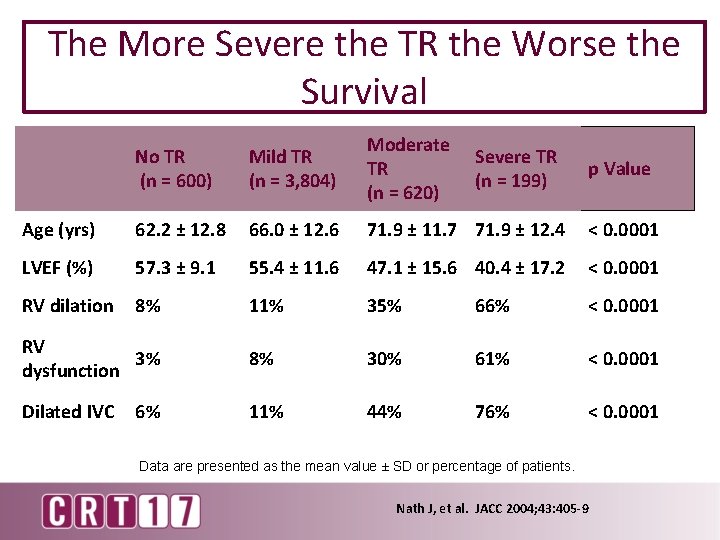
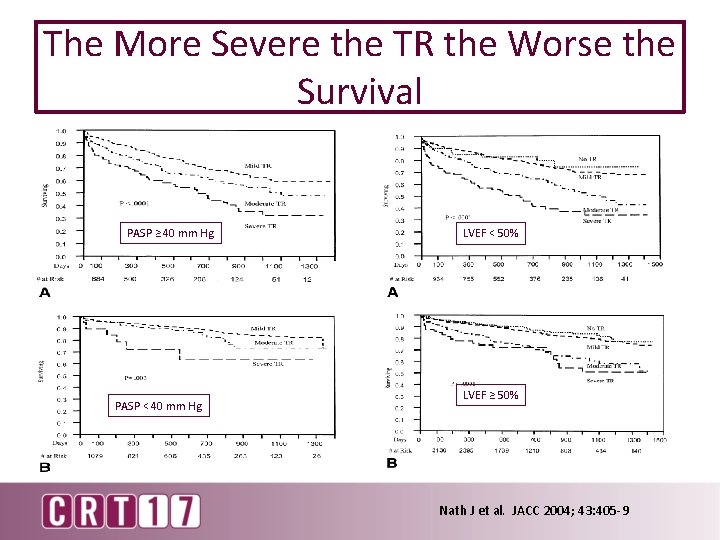
The More Severe the TR the Worse the Survival • 5223 consecutive VA patients with echo and degree of TR reported • Subgroups based on Normal or High(> 40 mm Hg) Pulmonary Artery Systolic Pressure(PASP) Normal (≥ 50%) or reduced LVEF • Echocardiographic TR based on regurgitant jet/right atrial area (mild < 19%, moderate 20 -40%, severe > 41%) Nath J, et al. JACC 2004; 43: 405 -9
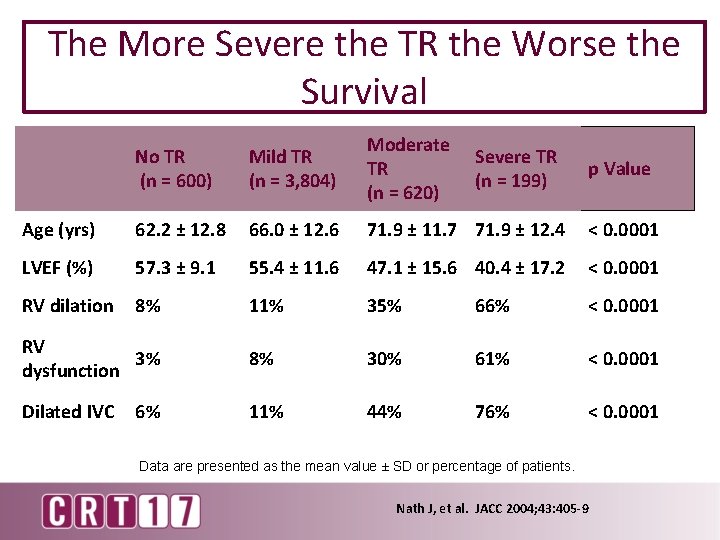
The More Severe the TR the Worse the Survival No TR (n = 600) Mild TR (n = 3, 804) Moderate TR (n = 620) Age (yrs) 62. 2 ± 12. 8 66. 0 ± 12. 6 71. 9 ± 11. 7 71. 9 ± 12. 4 < 0. 0001 LVEF (%) 57. 3 ± 9. 1 55. 4 ± 11. 6 47. 1 ± 15. 6 40. 4 ± 17. 2 < 0. 0001 RV dilation 8% 11% 35% 66% < 0. 0001 RV 3% dysfunction 8% 30% 61% < 0. 0001 Dilated IVC 11% 44% 76% < 0. 0001 6% Severe TR (n = 199) p Value Data are presented as the mean value ± SD or percentage of patients. Nath J, et al. JACC 2004; 43: 405 -9
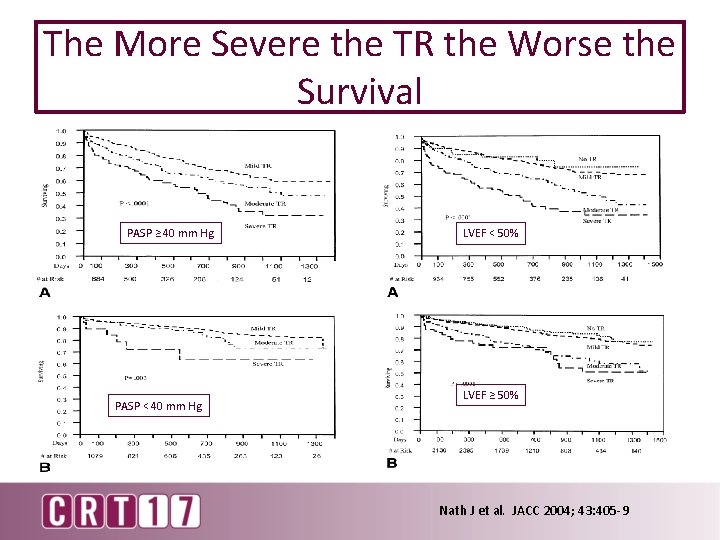
The More Severe the TR the Worse the Survival PASP ≥ 40 mm Hg PASP < 40 mm Hg LVEF < 50% LVEF ≥ 50% Nath J et al. JACC 2004; 43: 405 -9
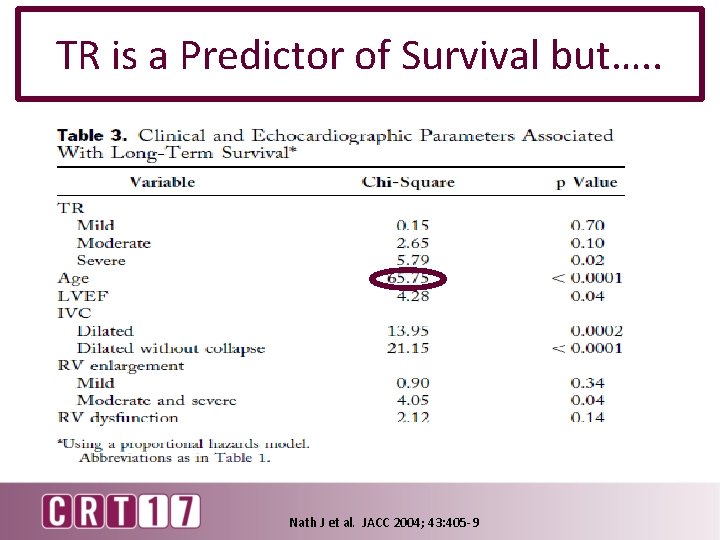
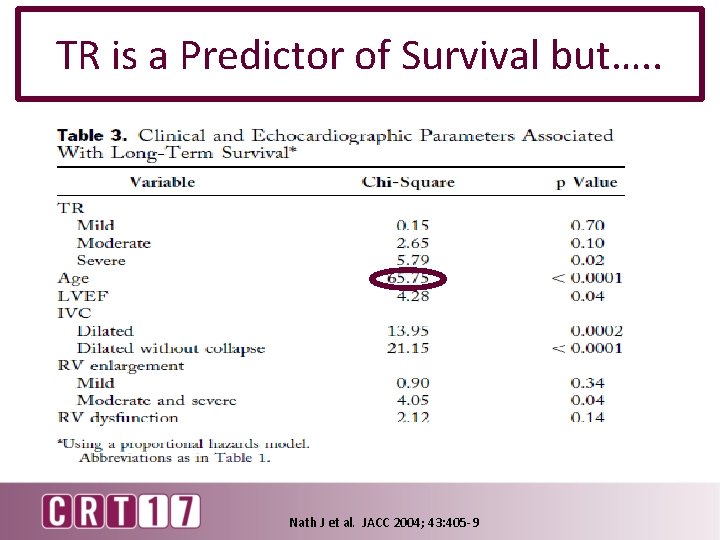
TR is a Predictor of Survival but…. . Nath J et al. JACC 2004; 43: 405 -9
Toplinsky Y et al. JACC: Cardiovascular Imaging, 2014: 7: 1186 -94
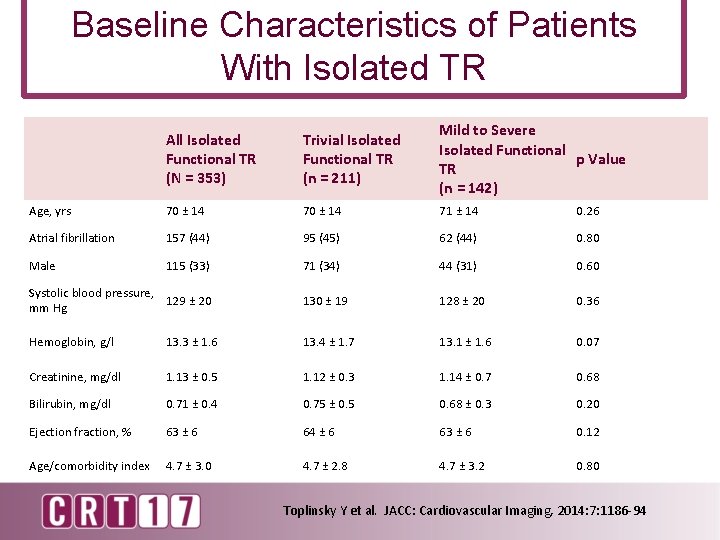
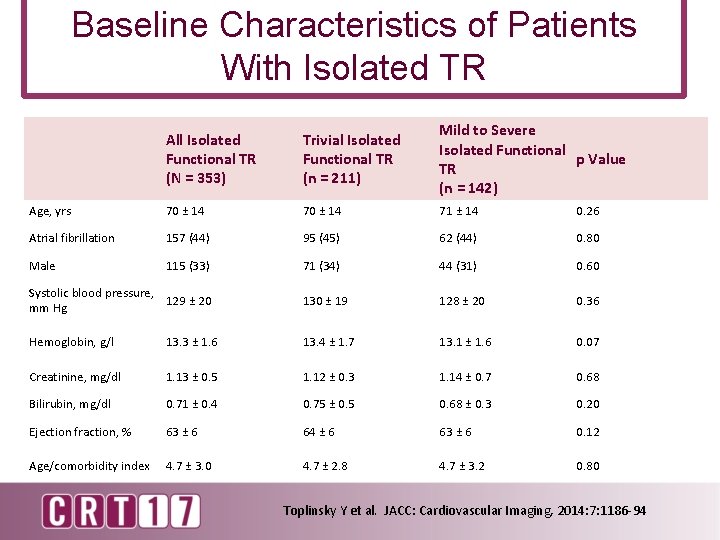
Baseline Characteristics of Patients With Isolated TR All Isolated Functional TR (N = 353) Trivial Isolated Functional TR (n = 211) Mild to Severe Isolated Functional p Value TR (n = 142) Age, yrs 70 ± 14 71 ± 14 0. 26 Atrial fibrillation 157 (44) 95 (45) 62 (44) 0. 80 Male 115 (33) 71 (34) 44 (31) 0. 60 Systolic blood pressure, 129 ± 20 mm Hg 130 ± 19 128 ± 20 0. 36 Hemoglobin, g/l 13. 3 ± 1. 6 13. 4 ± 1. 7 13. 1 ± 1. 6 0. 07 Creatinine, mg/dl 1. 13 ± 0. 5 1. 12 ± 0. 3 1. 14 ± 0. 7 0. 68 Bilirubin, mg/dl 0. 71 ± 0. 4 0. 75 ± 0. 5 0. 68 ± 0. 3 0. 20 Ejection fraction, % 63 ± 6 64 ± 6 63 ± 6 0. 12 Age/comorbidity index 4. 7 ± 3. 0 4. 7 ± 2. 8 4. 7 ± 3. 2 0. 80 Toplinsky Y et al. JACC: Cardiovascular Imaging, 2014: 7: 1186 -94
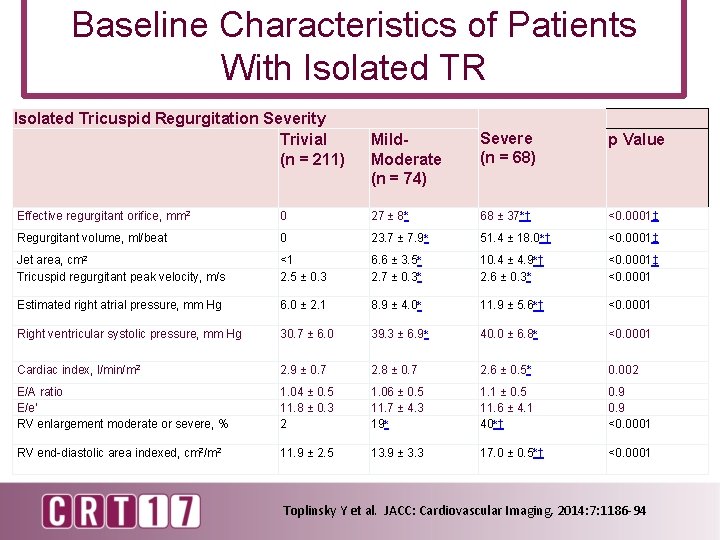
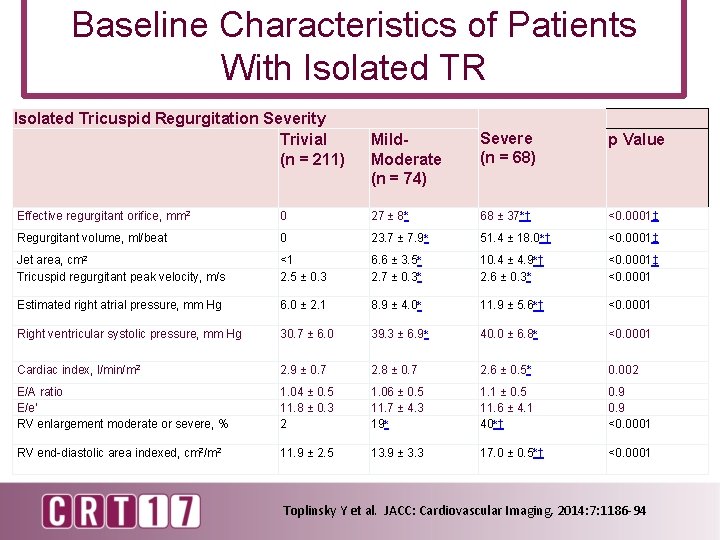
Baseline Characteristics of Patients With Isolated TR Isolated Tricuspid Regurgitation Severity Trivial (n = 211) Mild. Moderate (n = 74) Severe (n = 68) p Value Effective regurgitant orifice, mm 2 0 27 ± 8∗ 68 ± 37∗† <0. 0001‡ Regurgitant volume, ml/beat 0 23. 7 ± 7. 9∗ 51. 4 ± 18. 0∗† <0. 0001‡ Jet area, cm 2 Tricuspid regurgitant peak velocity, m/s <1 2. 5 ± 0. 3 6. 6 ± 3. 5∗ 2. 7 ± 0. 3∗ 10. 4 ± 4. 9∗† 2. 6 ± 0. 3∗ <0. 0001‡ <0. 0001 Estimated right atrial pressure, mm Hg 6. 0 ± 2. 1 8. 9 ± 4. 0∗ 11. 9 ± 5. 6∗† <0. 0001 Right ventricular systolic pressure, mm Hg 30. 7 ± 6. 0 39. 3 ± 6. 9∗ 40. 0 ± 6. 8∗ <0. 0001 Cardiac index, l/min/m 2 2. 9 ± 0. 7 2. 8 ± 0. 7 2. 6 ± 0. 5∗ 0. 002 E/A ratio E/e′ RV enlargement moderate or severe, % 1. 04 ± 0. 5 11. 8 ± 0. 3 2 1. 06 ± 0. 5 11. 7 ± 4. 3 19∗ 1. 1 ± 0. 5 11. 6 ± 4. 1 40∗† 0. 9 <0. 0001 RV end-diastolic area indexed, cm 2/m 2 11. 9 ± 2. 5 13. 9 ± 3. 3 17. 0 ± 0. 5∗† <0. 0001 Toplinsky Y et al. JACC: Cardiovascular Imaging, 2014: 7: 1186 -94
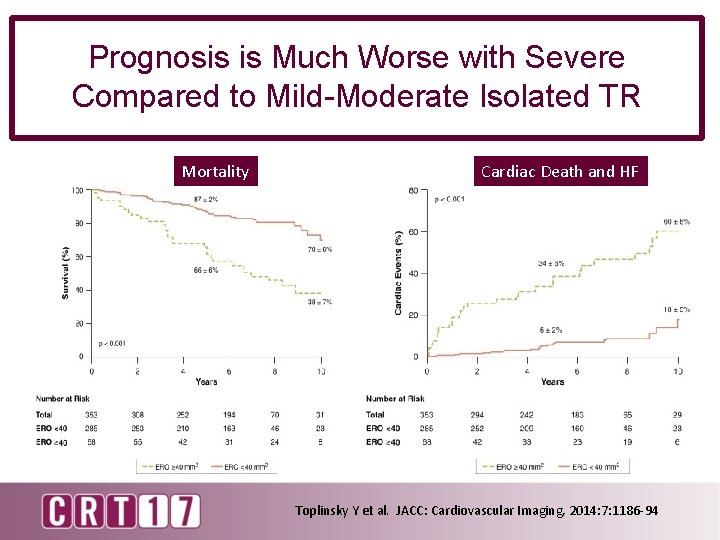
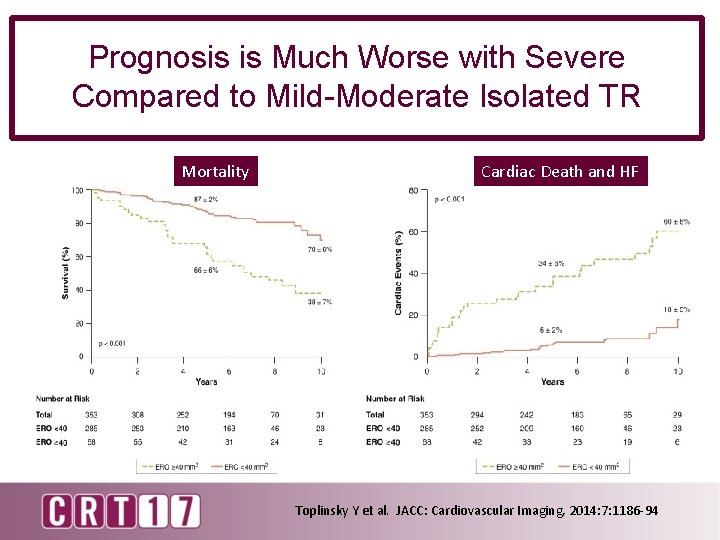
Prognosis is Much Worse with Severe Compared to Mild-Moderate Isolated TR Mortality Cardiac Death and HF Toplinsky Y et al. JACC: Cardiovascular Imaging, 2014: 7: 1186 -94
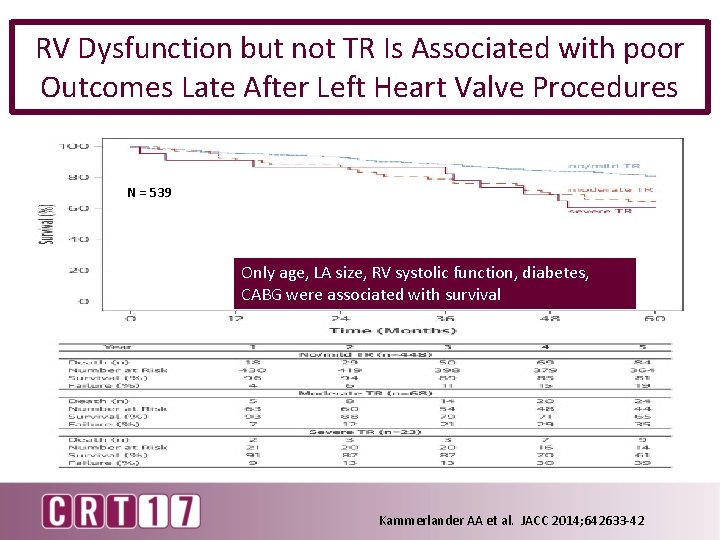
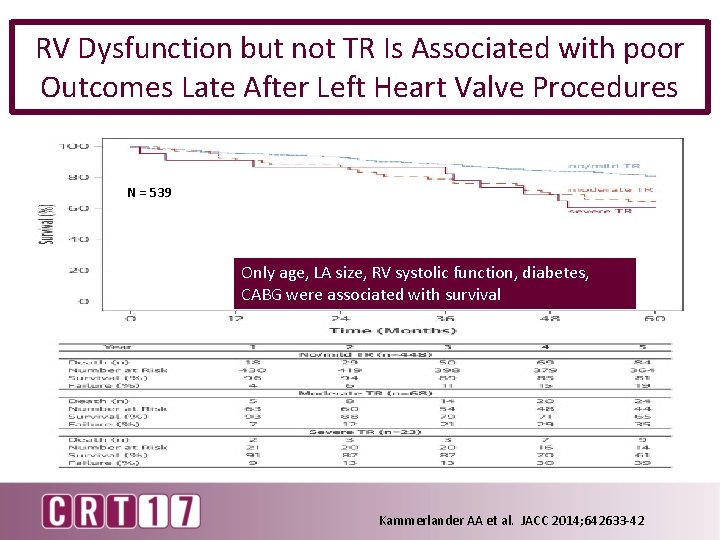
RV Dysfunction but not TR Is Associated with poor Outcomes Late After Left Heart Valve Procedures N = 539 Only age, LA size, RV systolic function, diabetes, CABG were associated with survival Kammerlander AA et al. JACC 2014; 642633 -42
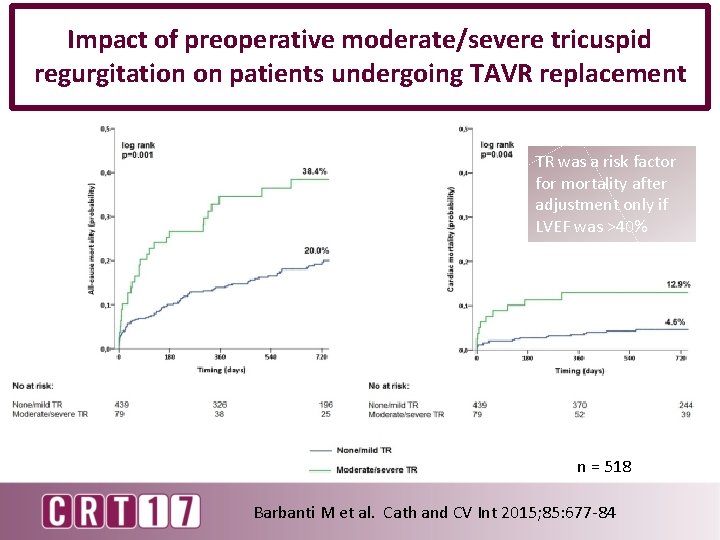
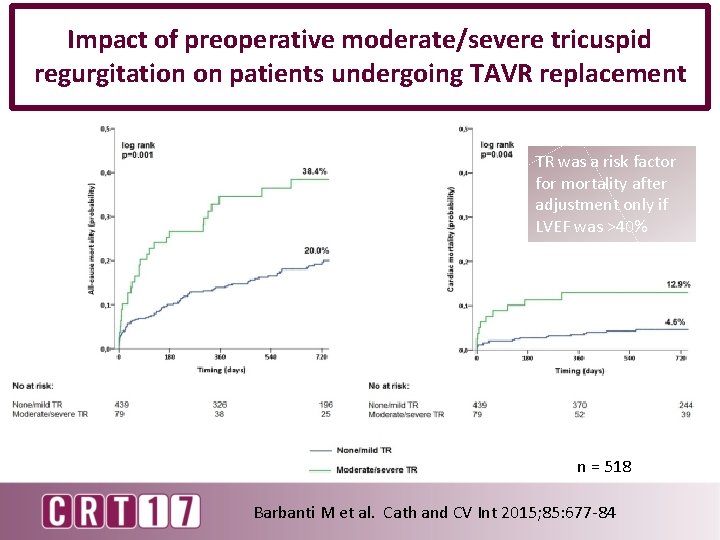
Impact of preoperative moderate/severe tricuspid regurgitation on patients undergoing TAVR replacement TR was a risk factor for mortality after adjustment only if LVEF was >40% n = 518 Barbanti M et al. Cath and CV Int 2015; 85: 677 -84
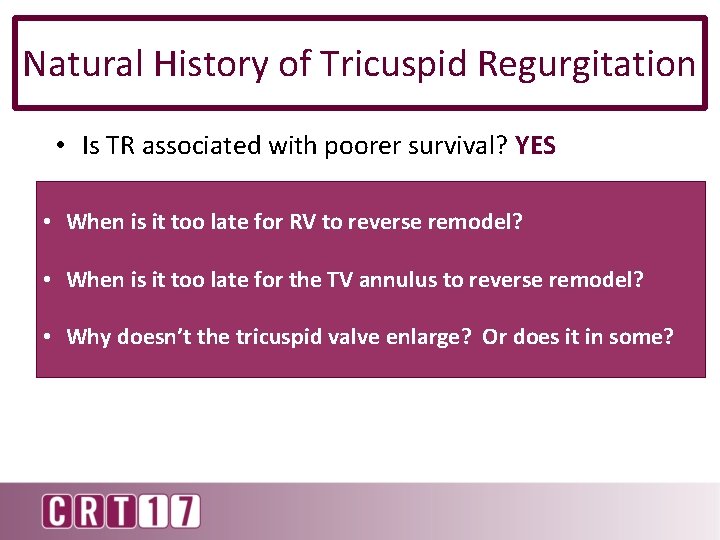
Natural History of Tricuspid Regurgitation • Is TR associated with poorer survival? YES • • When it too late for RV to reverse remodel? Is theis poorer survival associated due to the TR or the associated comorbidities or both? • When is it too late for the TV annulus to reverse remodel? Primary due to TR • Why doesn’t the tricuspid In secondary ? ? ? valve enlarge? Or does it in some?
 Primary tricuspid regurgitation
Primary tricuspid regurgitation Tricuspid regurgitation echo assessment
Tricuspid regurgitation echo assessment Tricuspid regurgitation
Tricuspid regurgitation Nrga in echo
Nrga in echo Cusps of tricuspid valve
Cusps of tricuspid valve Arteriosum
Arteriosum Left lung
Left lung Parts of the heart diagram
Parts of the heart diagram Mitral regurgitation symptoms
Mitral regurgitation symptoms Pulmonic regurgitation
Pulmonic regurgitation Pannus
Pannus Mitral regurgitation murmur
Mitral regurgitation murmur Apex beat
Apex beat Dicrotic pulse
Dicrotic pulse Regurgitation test
Regurgitation test Lacrimal sac
Lacrimal sac Heart sounds location
Heart sounds location