Nama Sofwan Dahlan Sp F K Lahir di
- Slides: 37
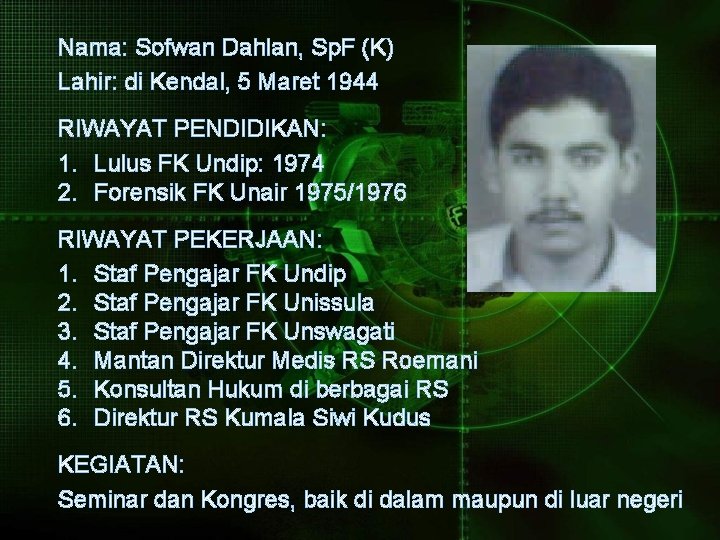
Nama: Sofwan Dahlan, Sp. F (K) Lahir: di Kendal, 5 Maret 1944 RIWAYAT PENDIDIKAN: 1. Lulus FK Undip: 1974 2. Forensik FK Unair 1975/1976 RIWAYAT PEKERJAAN: 1. Staf Pengajar FK Undip 2. Staf Pengajar FK Unissula 3. Staf Pengajar FK Unswagati 4. Mantan Direktur Medis RS Roemani 5. Konsultan Hukum di berbagai RS 6. Direktur RS Kumala Siwi Kudus KEGIATAN: Seminar dan Kongres, baik di dalam maupun di luar negeri
ETHICAL ASPECT IN CARDIOVASCULAR DISEASE AND PATIENT SAFETY Oleh Sofwan Dahlan
Heart Disease The term heart disease is often used interchangeably with the term cardiovascular disease. Cardiovascular disease generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack, chest pain, or stroke. Other heart conditions such as those that affect heart’s muscle, valves or rhythm, also are considered forms of heart disease. Heart disease describes ---- a range of conditions that affect the heart. Timing and accuracy are critical in the diagnosis of a heart condition ……. …. and better diagnosis lead to optimal treatments and outcomes for patients.
We have to realize that major advances of science, technology, and health care during the 50 years have outpaced the abilities of those in ethics and law to solve the problems created by those advances. (Catalano, 1991)
Kemajuan Iptek Kedokteran Kemajuan iptek di bidang kedokteran: a. dipicu oleh kemampuan para Dr dalam memahami bio-molecular; b. diciptakannya alat-alat imaging, computing, dan telecommunication; c. ditemukannya obat-obatan baru, termasuk obat immunosuppressan. Selain memberikan kemudahan, juga menciptakan “Paradoxes of Modern Medicine”
Paradoxes of Modern Medicine Paradox 1: Modern medicine makes it possible !!! Sometimes even necessary, to keep dead people alive. Paradox 2: Modern medicine tries to cure non-illnesses !!! It identifies asymptomatic medical conditions as diseases. Sometimes it even classifies risks as diseases. In general, it tends to blur the distinction between disease and risk, illness and non-illness. (Prof. John Ladd)
Non-Invasive Diagnostic Tests ü Helical CT Scanner ü Stress Electrocardiogram Test ü Trans-esophageal Echocardiogram (TEE) ü Electrocardiogram (ECG) ü Holter Monitoring ü Echocardiogram ü Arterial / Venous Flow Studies
Invasive Diagnostic Tests Invasive tests involve …. . inserting catheters into the blood vessels of the heart in order to get a closer look at the coronary arteries or ……. . to stimulate and the electrical system of the heart. ü Cardiac Catheterization ü Carotid Angiography ü Carotid Stent ü Electrophysiology Study ü Intravascular Ultrasound ü Myocardial Biopsy
Cardiac Procedures & Surgeries o o o o o Artificial Heart Valve Surgery Atherectomy Bypass Surgery Cardiomyoplasty Heart Transplant Minimally Invasive Heart Surgery Radiofrequency Ablation Stent Procedures Transmyocardial Revascularization (TMR)
MEDICAL INTERVENTION Medical intervention may be: a. curative b. offering definite correction of condition or supportive c. offering relief of symptoms d. slowing the progression of diseases that currently are incurable e. for other condition, interventions are less effective in delaying the progression of diseases, but still can be used to palliate symptoms or to treat acute episodes (Johnson; Sigler; Winslade: 2006)
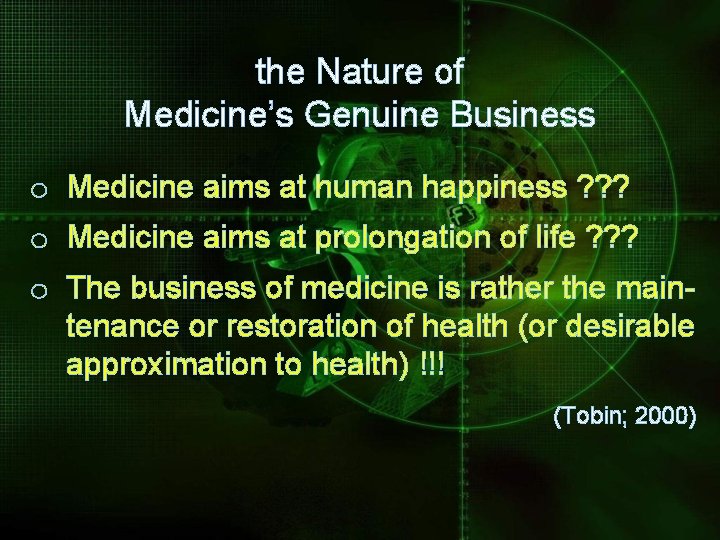
the Nature of Medicine’s Genuine Business o Medicine aims at human happiness ? ? ? o Medicine aims at prolongation of life ? ? ? o The business of medicine is rather the maintenance or restoration of health (or desirable approximation to health) !!! (Tobin; 2000)
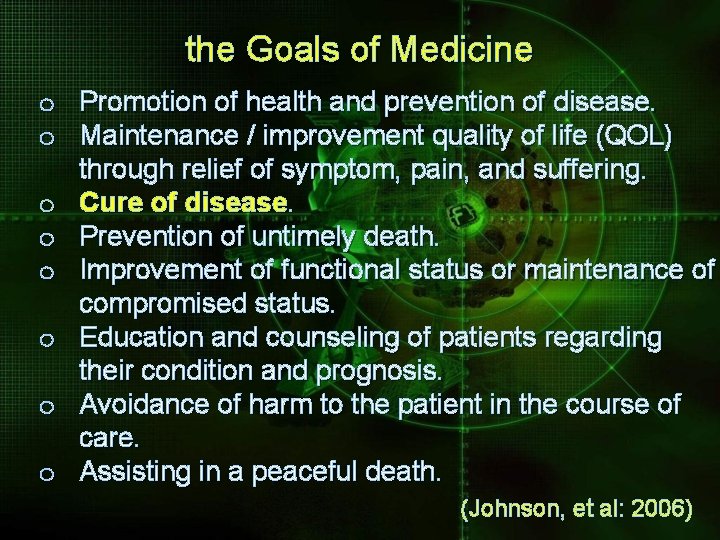
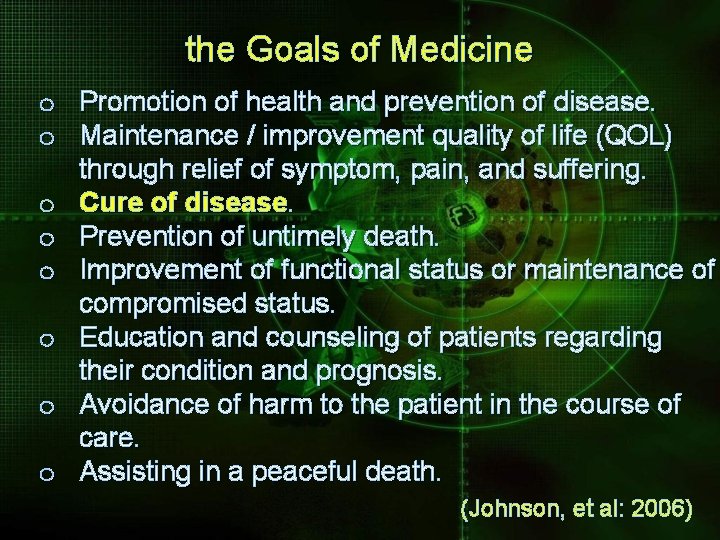
the Goals of Medicine o Promotion of health and prevention of disease. o Maintenance / improvement quality of life (QOL) through relief of symptom, pain, and suffering. o Cure of disease. o Prevention of untimely death. o Improvement of functional status or maintenance of compromised status. o Education and counseling of patients regarding their condition and prognosis. o Avoidance of harm to the patient in the course of care. o Assisting in a peaceful death. (Johnson, et al: 2006)
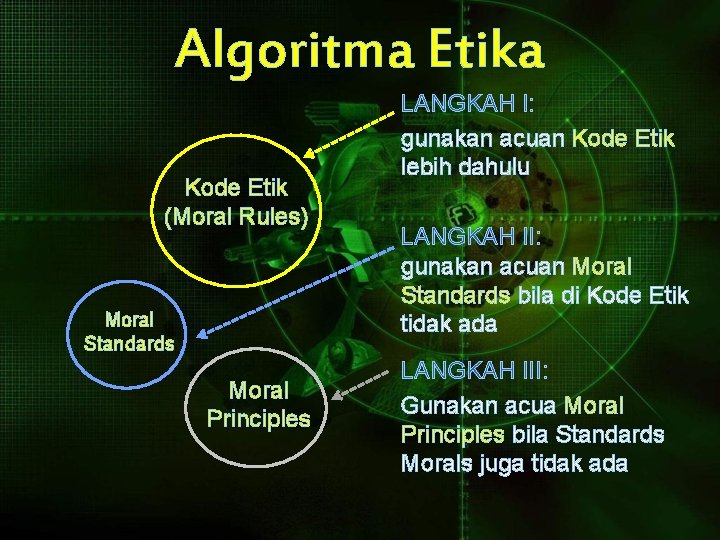
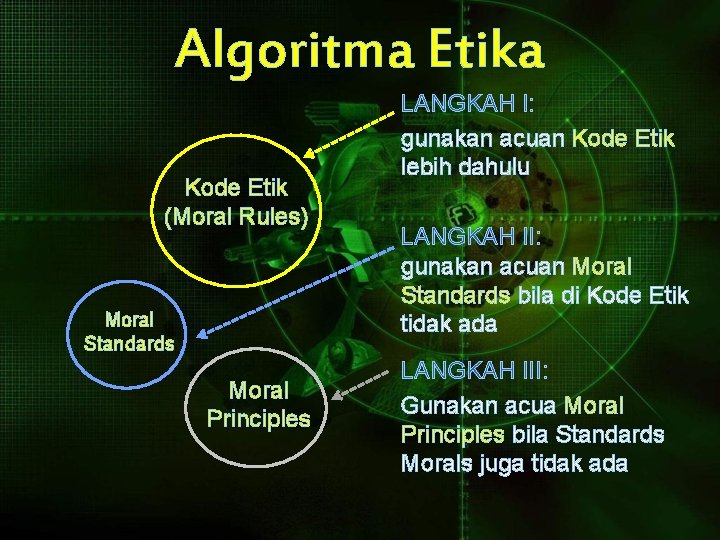
Algoritma Etika Kode Etik (Moral Rules) Moral Standards Moral Principles LANGKAH I: gunakan acuan Kode Etik lebih dahulu LANGKAH II: gunakan acuan Moral Standards bila di Kode Etik tidak ada LANGKAH III: Gunakan acua Moral Principles bila Standards Morals juga tidak ada
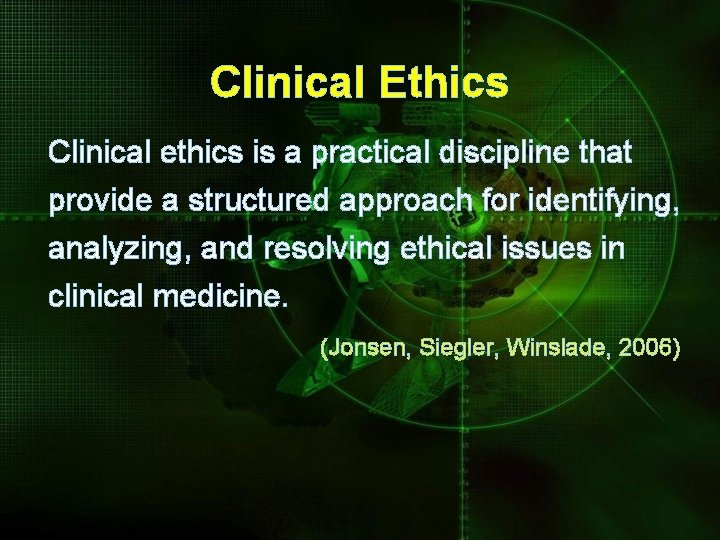
Clinical Ethics Clinical ethics is a practical discipline that provide a structured approach for identifying, analyzing, and resolving ethical issues in clinical medicine. (Jonsen, Siegler, Winslade, 2006)
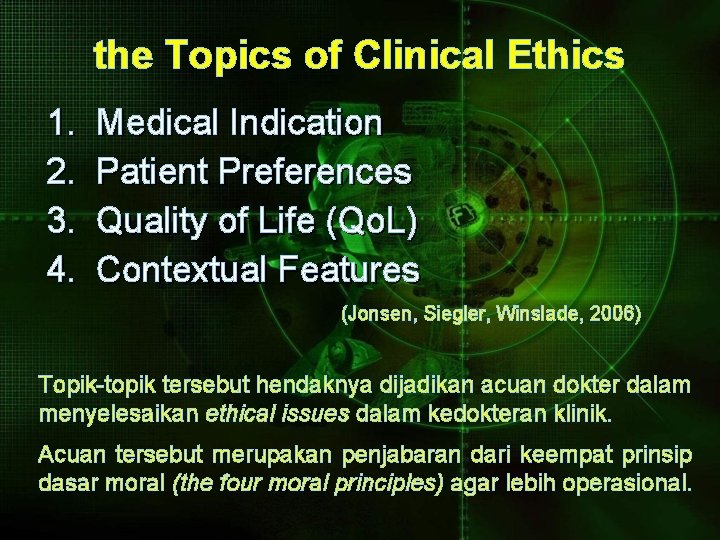
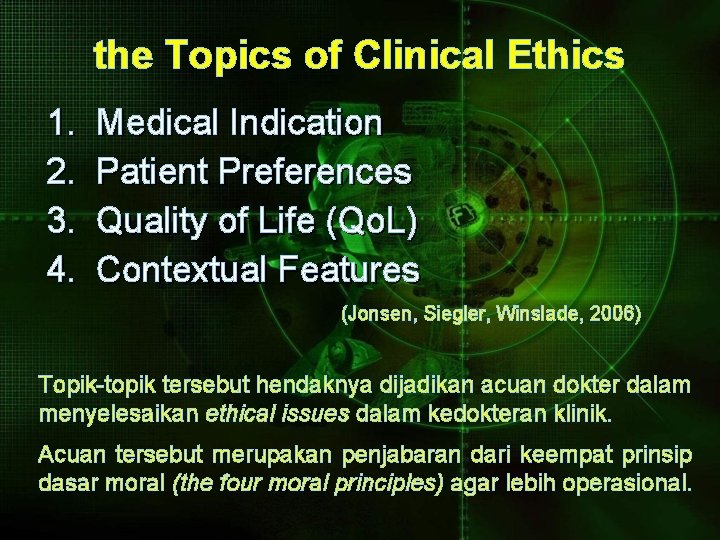
the Topics of Clinical Ethics 1. 2. 3. 4. Medical Indication Patient Preferences Quality of Life (Qo. L) Contextual Features (Jonsen, Siegler, Winslade, 2006) Topik-topik tersebut hendaknya dijadikan acuan dokter dalam menyelesaikan ethical issues dalam kedokteran klinik. Acuan tersebut merupakan penjabaran dari keempat prinsip dasar moral (the four moral principles) agar lebih operasional.
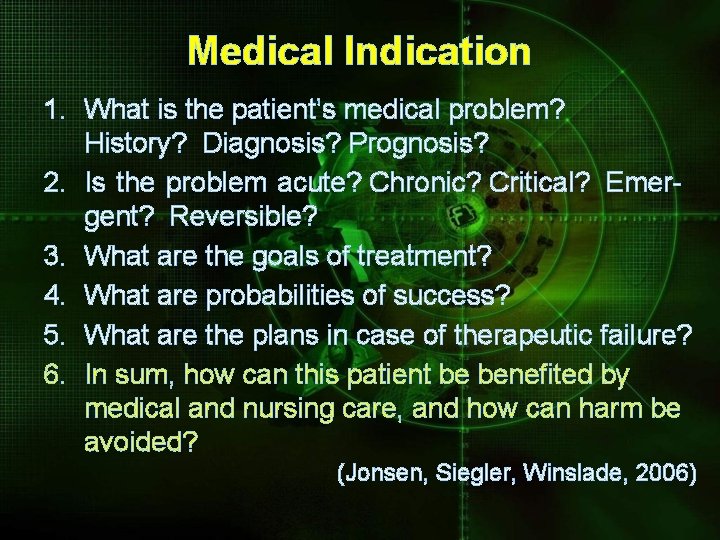
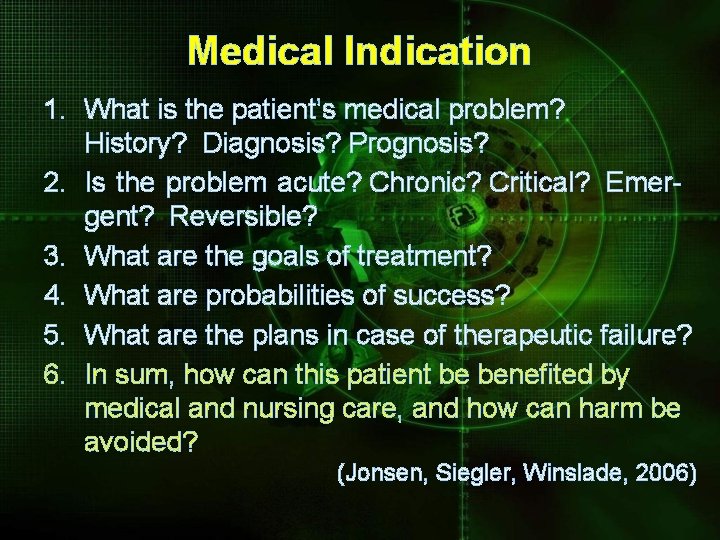
Medical Indication 1. What is the patient’s medical problem? History? Diagnosis? Prognosis? 2. Is the problem acute? Chronic? Critical? Emergent? Reversible? 3. What are the goals of treatment? 4. What are probabilities of success? 5. What are the plans in case of therapeutic failure? 6. In sum, how can this patient be benefited by medical and nursing care, and how can harm be avoided? (Jonsen, Siegler, Winslade, 2006)
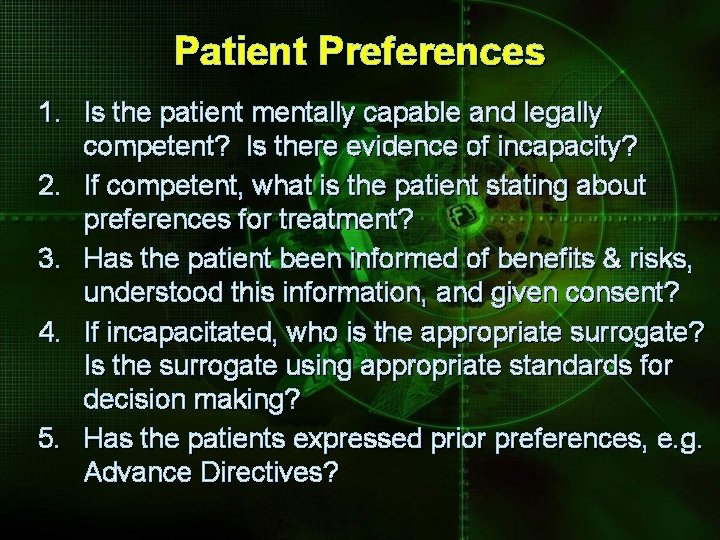
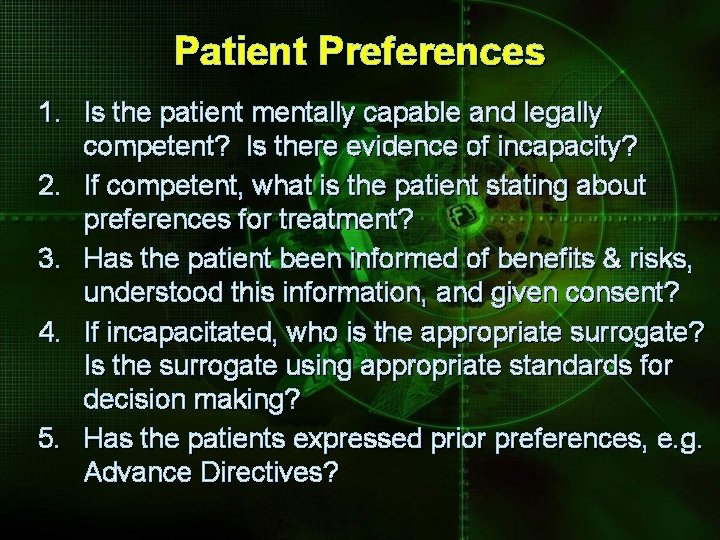
Patient Preferences 1. Is the patient mentally capable and legally competent? Is there evidence of incapacity? 2. If competent, what is the patient stating about preferences for treatment? 3. Has the patient been informed of benefits & risks, understood this information, and given consent? 4. If incapacitated, who is the appropriate surrogate? Is the surrogate using appropriate standards for decision making? 5. Has the patients expressed prior preferences, e. g. Advance Directives?
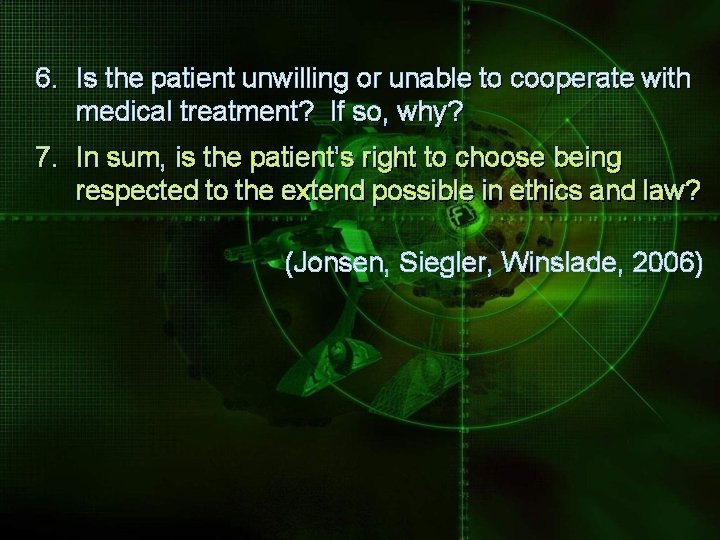
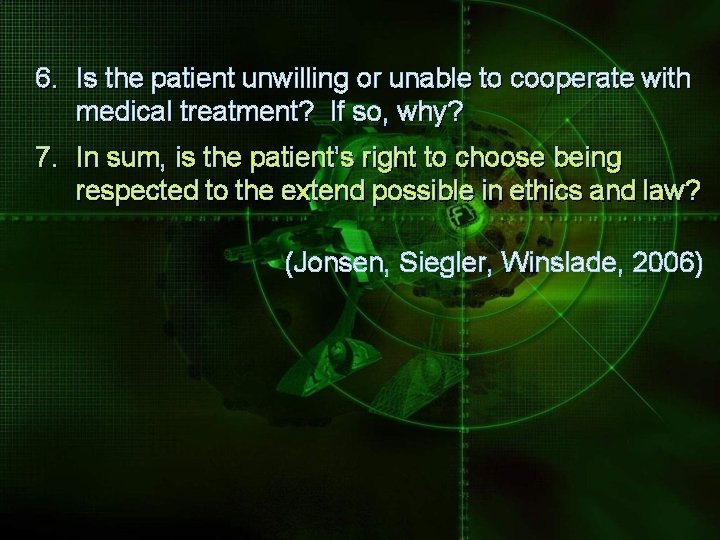
6. Is the patient unwilling or unable to cooperate with medical treatment? If so, why? 7. In sum, is the patient’s right to choose being respected to the extend possible in ethics and law? (Jonsen, Siegler, Winslade, 2006)
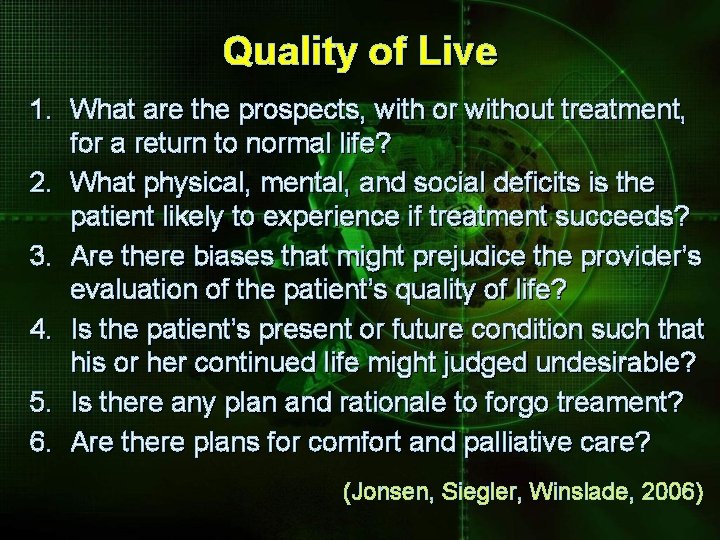
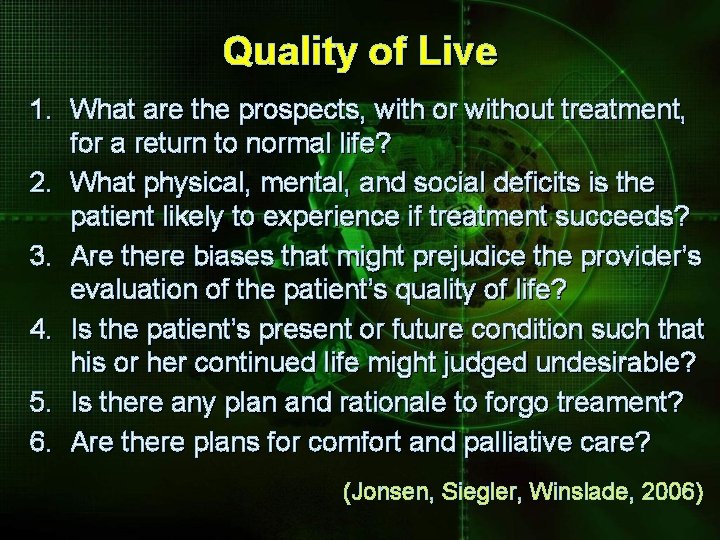
Quality of Live 1. What are the prospects, with or without treatment, for a return to normal life? 2. What physical, mental, and social deficits is the patient likely to experience if treatment succeeds? 3. Are there biases that might prejudice the provider’s evaluation of the patient’s quality of life? 4. Is the patient’s present or future condition such that his or her continued life might judged undesirable? 5. Is there any plan and rationale to forgo treament? 6. Are there plans for comfort and palliative care? (Jonsen, Siegler, Winslade, 2006)
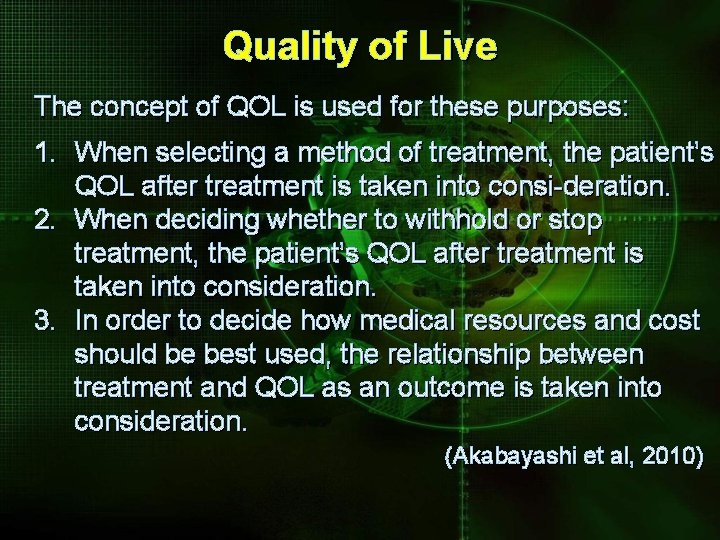
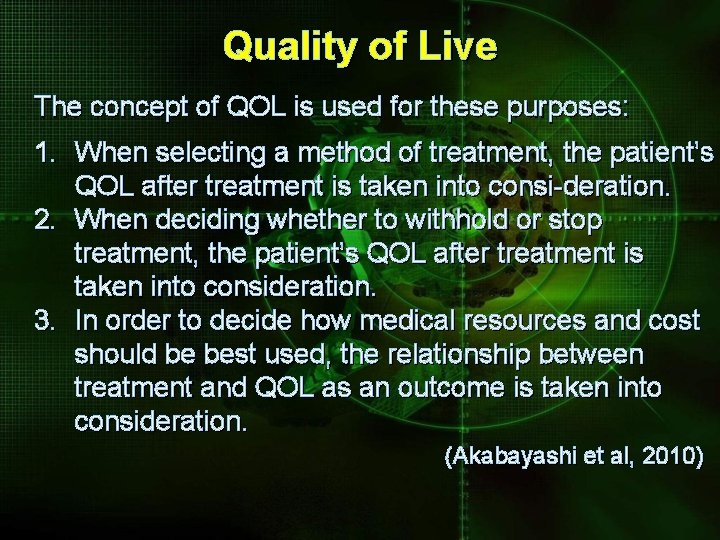
Quality of Live The concept of QOL is used for these purposes: 1. When selecting a method of treatment, the patient’s QOL after treatment is taken into consi-deration. 2. When deciding whether to withhold or stop treatment, the patient’s QOL after treatment is taken into consideration. 3. In order to decide how medical resources and cost should be best used, the relationship between treatment and QOL as an outcome is taken into consideration. (Akabayashi et al, 2010)
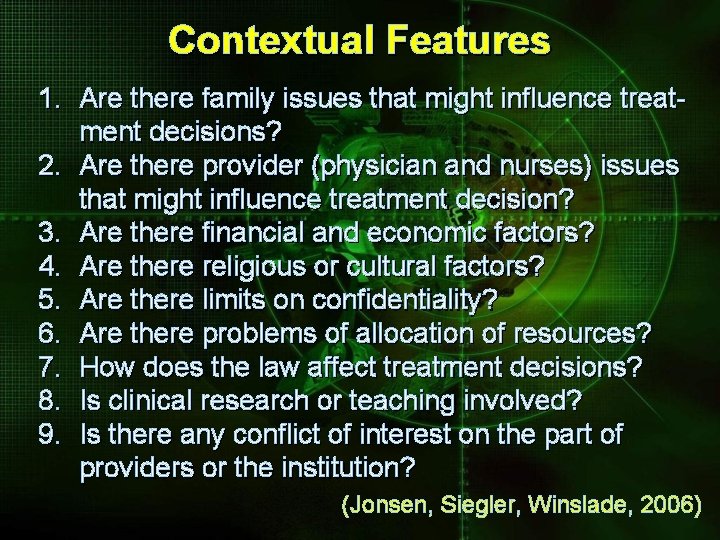
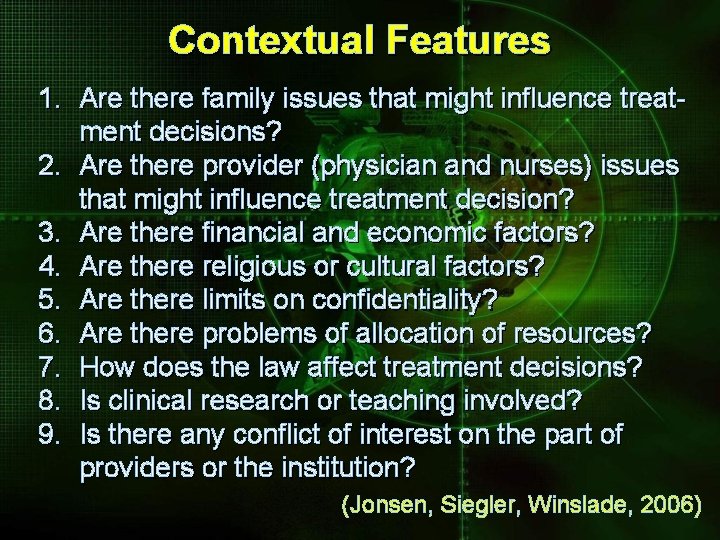
Contextual Features 1. Are there family issues that might influence treatment decisions? 2. Are there provider (physician and nurses) issues that might influence treatment decision? 3. Are there financial and economic factors? 4. Are there religious or cultural factors? 5. Are there limits on confidentiality? 6. Are there problems of allocation of resources? 7. How does the law affect treatment decisions? 8. Is clinical research or teaching involved? 9. Is there any conflict of interest on the part of providers or the institution? (Jonsen, Siegler, Winslade, 2006)
PREVENTION IS STILL THE BEST DEFENS AGAINST THE ACCUSATION OF MALPRACTICE
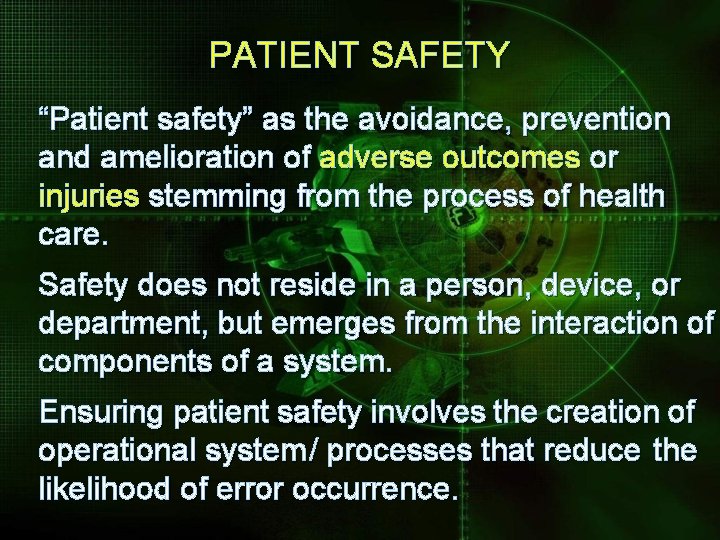
PATIENT SAFETY “Patient safety” as the avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of health care. Safety does not reside in a person, device, or department, but emerges from the interaction of components of a system. Ensuring patient safety involves the creation of operational system / processes that reduce the likelihood of error occurrence.
Adverse Event o IF CAUSED BY ERRORs – IT IS PREVENTABLE o 66% OF ALL ADVERSE EVENTS ARE SURGICAL o 50% OF ALL ADVERSE EVENTS ARE PEVENTABLE
PATIENT SAFETY Overview: 1. Banyak pasien mengalami KTD di RS. 2. Seingkali KTD tersebut sebetulnya bisa dihindari. 3. Penyebab & jenis ancaman terhadap keselamatan tergantung dari metode identifikasi dan klasifikasi. 4. KTD sering mengancam keselamatan pasien, baik pada layanan primer maupun sekunder. 5. Kegagalan atau keterlambatan dalam menentukan diagnosis sering mengancam keselamatan pasien pada layanan primer. (Sandars, J: 2007)
THE NATURE OF ERROR Overview: 1. Paling banyak ancaman terhadap keselamatan pasien disebabkan kombinasi yang komplek dari active error dan latent error. 2. Active error biasanya disebabkan human factor. 3. Latent error utamanya disebabkan oleh problem organisasi …. . . sehingga memudahkan terjadinya active error. 4. Latent error …. …. merupakan akar permasalahan timbulnya ancaman terhadap keselamatan pasien. (Cozens, F, J; Sandars, J: 2007)
COMMUNICATION and SAFETY Overview: 1. Problem komunikasi dengan pasien atau dalam team merupakan ancaman terhadap keselamatan pasien. 2. Komunikasi yang buruk ……. . akan meningkatkan terjadinya potential risk terhadap tuntutan hukum. 3. Specific communication skill training akan dapat meningkatkan keselamatan pasien. 4. Jika KTD telah terjadi …. . seringkali menimbulkan kesulitan dalam berkomunikasi dgn pihak pasien. (Beyer, M; Roche, P, J; Haynes, K; 2007)
PATIENT SAFETY CULTURE Overview: 1. Kultur sangat penting bagi patient safety. 2. Setiap orang dlm organisasi, baik individu maupun kolektif, bertanggungjawab terhadap patient safety. 3. Membangun kultur patient safety …. membutuhkan kepemimpinan yang kuat. 4. Pendekatan team working pada industri penerbangan dapat ditiru untuk meningkatkan kultur patient safety di organisasi pelayanan kesehatan. (Claridge, T; Sandars, J: 2007)
PRINCIPLES of CLINICAL RISK MANAGEMENT Overview: 1. Risiko adalah bagian dari kehidupan yang tak bisa dihindari samasekali, tetapi bisa diminimalkan. 2. Semua aspek dalam layanan kesehatan amat erat hubungannya dengan risiko klinik. 3. Manajemen risiko klinik …… harus secara proaktif disertai sistem terencana untuk mencegah atau mengurangai potential risk. 4. Manajemen risiko klinik …. . … dapat berguna untuk mengatasi potential risk yang sudah bisa dikenali. (Price, J; Niklin, P, J; Haynes, K: 2007)
FUTURE DIRECTIONS Overview: 1. Keselamatan pasien (Patient Safety) masih tetap menjadi masalah besar bagi RS. 2. Rintangan utama meningkatkan Patient Safety masih terletak pada keengganan orgasisasi untuk mengimplementasikannya. 3. Kurangnya evidence base yang membuktikan efektivitas dari program Patient Safety. 4. Riset lebih lanjut sangat dibutuhkan untuk dapat mempengaruhi kebijakan dan praktek. (Sheik, A; Baker, M, Thomson, R: 2007)
PATIENT SAFETY Most importantly, the laboratory director: § must commit to excellence in clinical care § must continually assess competence of cardiologist § should review procedural volume, appropriateness of indication, skill of performance, relationships with other laboratory personnel, and complications § must be responsible for the selection and performance of laboratory equipment and ensure that appropriate quality assurance protocols are in place for equipment § must establish and continually supervise the quality assurance program for the laboratory as it applies to cardiologists, other laboratory personnel, and lab
ETHICS of INVASIVE CARDIOLOGY Codes of medical ethics have existed since the earliest recorded history of medicine. As medical practice has changed, they have been restated and modified with each passing generation. The AMA first adopted a general code of ethics in 1847 and revised it most recently in 1997. With evolving specialization virtually all medical specialties have developed codes of ethics focused on issues specific to their practices, and guidelines for medical research, education and for manufacturing and marketing practices have been addressed by the AMA, the NIH, and the FDA.
The Society for Cardiovascular Angiography and Interventions (SCAI) was established in 1978 to provide a forum promoting excellence, quality, and safety in cardiac catheterizatiion laboratories. It has published numerous guidelines for catheterization laboratories and physicians who perform procedures therein, and many ethical considerations are implicit in these guidelines. More recently, SCAI has joined with the American College of Cardiology and other cardiology organizations in issuing recommendations for cardiac cath. lab. Interventional procedures have changed the face of invasive cardiology and have raised new medical challenges.
Invasive and interventional cardiologists work in a field that is highly dependent on technology in both medical equipment and pharmacology. Both areas have witnessed rapid evolution and rising costs. Because of these technological costs, and because they apply to a very large population of patients with heart disease, their economic impact has become significant.
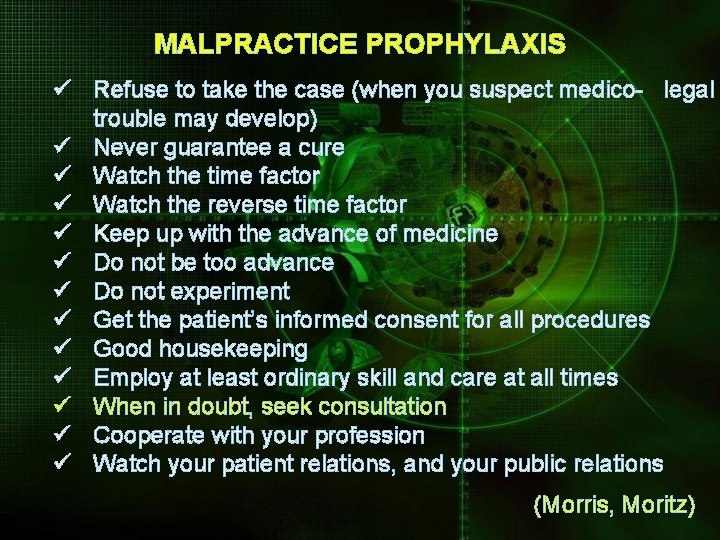
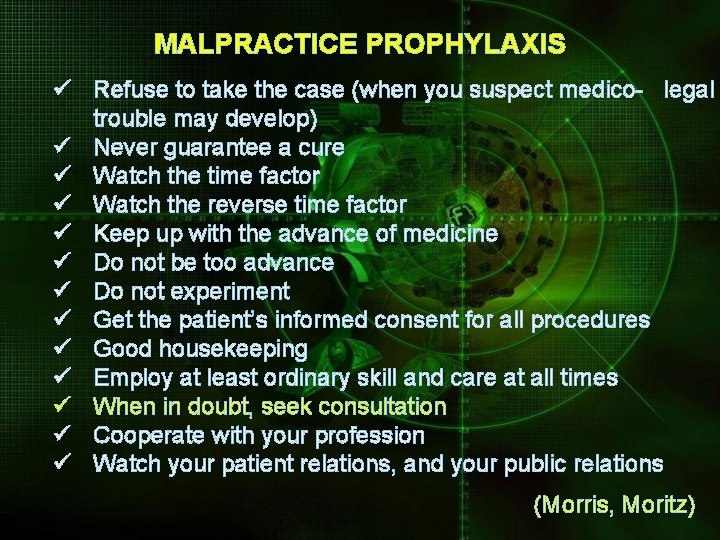
MALPRACTICE PROPHYLAXIS ü Refuse to take the case (when you suspect medico- legal trouble may develop) ü Never guarantee a cure ü Watch the time factor ü Watch the reverse time factor ü Keep up with the advance of medicine ü Do not be too advance ü Do not experiment ü Get the patient’s informed consent for all procedures ü Good housekeeping ü Employ at least ordinary skill and care at all times ü When in doubt, seek consultation ü Cooperate with your profession ü Watch your patient relations, and your public relations (Morris, Moritz)
SUMMARY The invasive cardiologist must balance his primary responsibility to: o his patients with his interactions with colleagues; o his dependency on industry for new technology, his teaching and research interests; o his administrative duties; and o his desire to be connected to advance his career.