MOYA Terminology Progressive narrowing of distal ICA and


- Slides: 15
MOYA
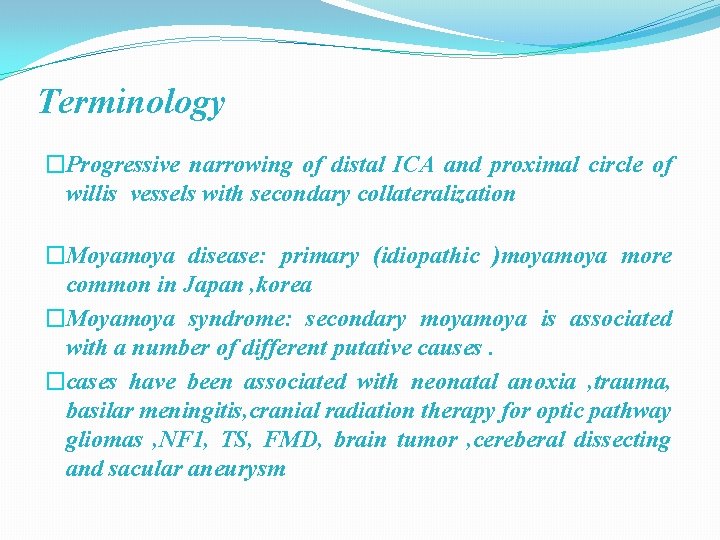
Terminology �Progressive narrowing of distal ICA and proximal circle of willis vessels with secondary collateralization �Moyamoya disease: primary (idiopathic )moya more common in Japan , korea �Moyamoya syndrome: secondary moya is associated with a number of different putative causes. �cases have been associated with neonatal anoxia , trauma, basilar meningitis, cranial radiation therapy for optic pathway gliomas , NF 1, TS, FMD, brain tumor , cereberal dissecting and sacular aneurysm
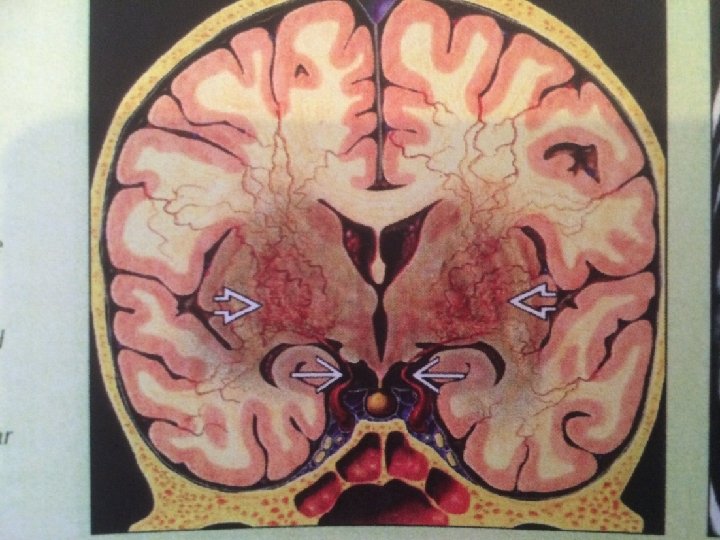
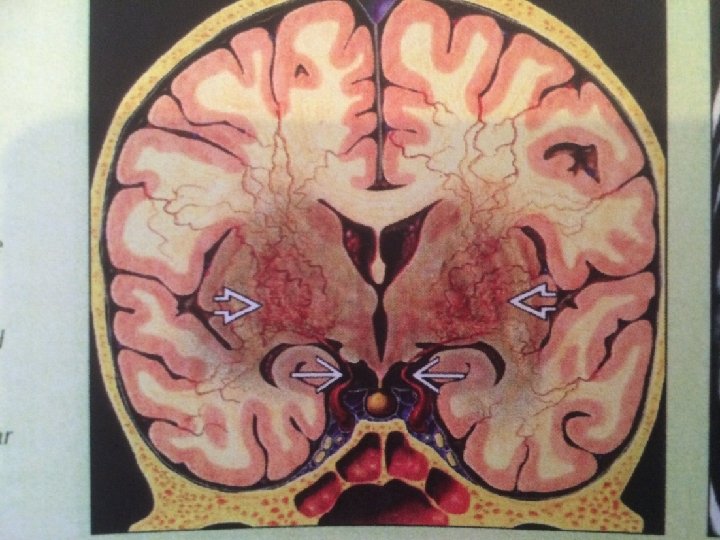
Pathology • Moyamoya is a chronic progressive nonatherosclerotic , non inflammatory , nonamyloid occlusive intracranial vasculopathy of unknown cause • Pathologically , there is fibrocellular intimal thickening , smooth muscle cell proliferation and increased elastin accumulation , resulting in stenosis of the suprasellar intracranial internal carotid arteries. Thrombotic lesions may be seen in major cerebral arteries. There also numerous perforating and anastomotic branches around the circle of willis.
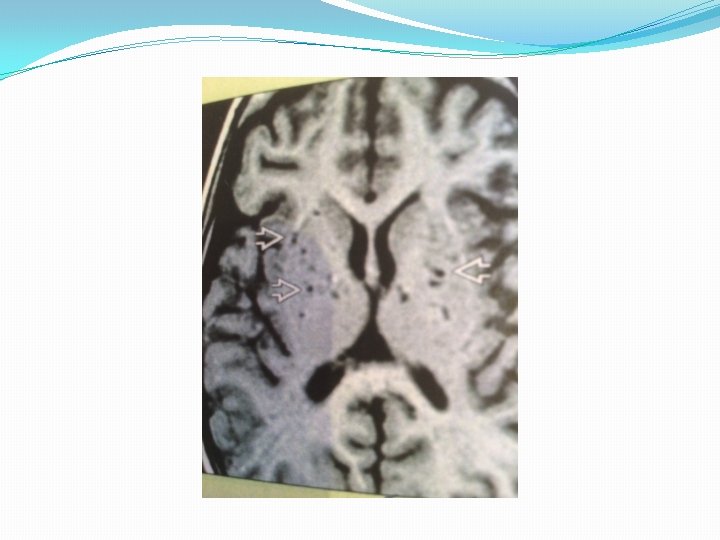
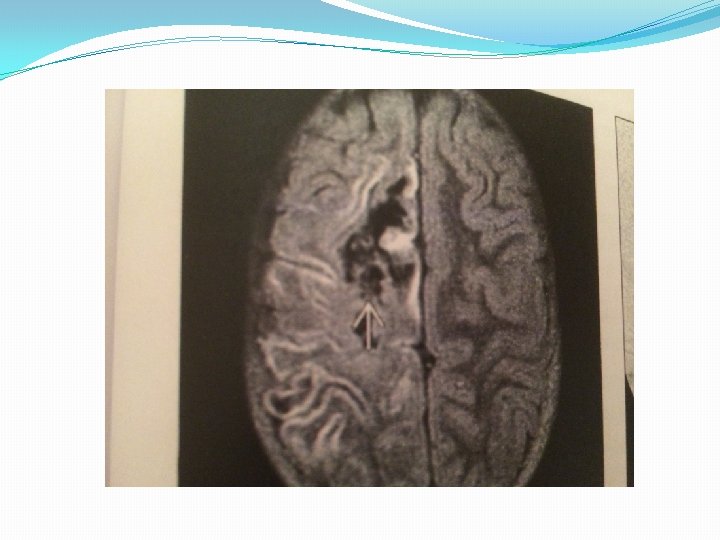
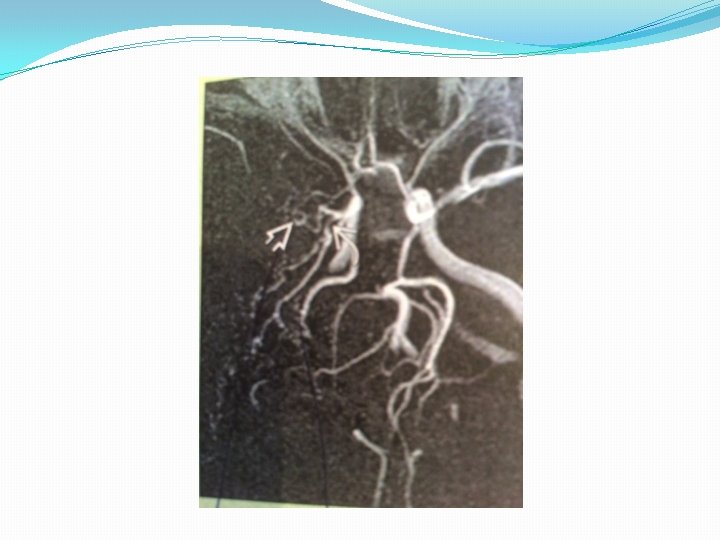
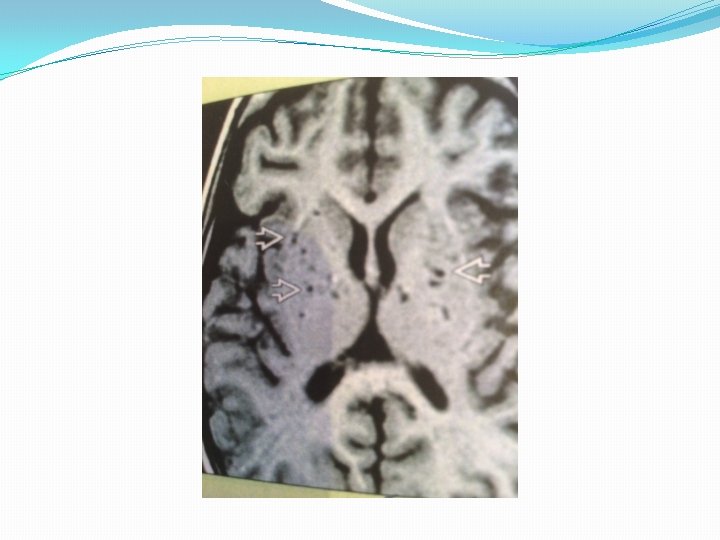
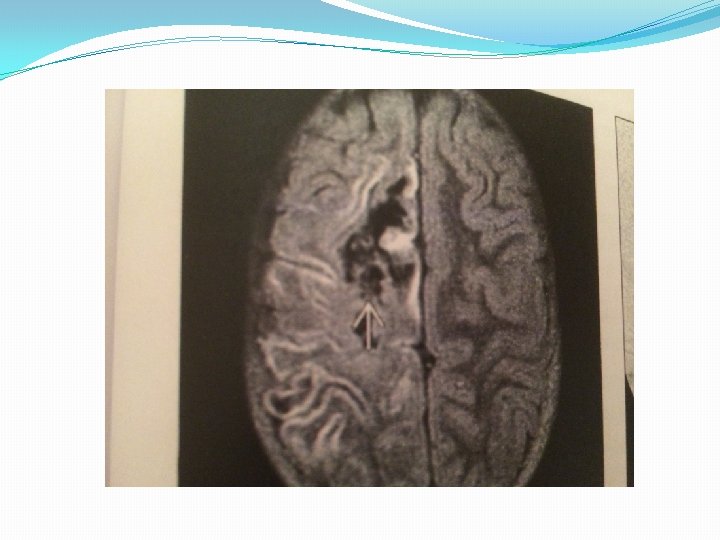
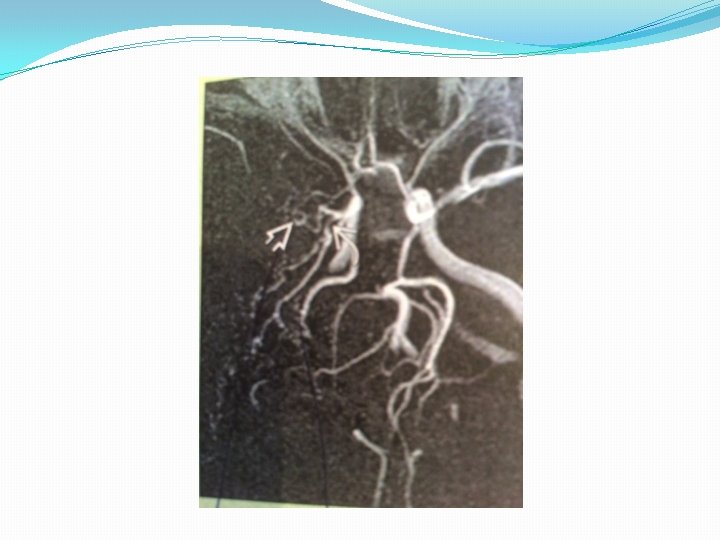
Imaging �Best diagnostic clue: multiple punctate dots (CECT) and flow voids(MR) in basal ganglia �Location : circle of willis ; anterior>>> posterior circulation �Morphology: “puff of smoke” cloud like lenticulostriate and thalamosrtiate collaterals on angiography
Imaging MRI finding �T 1 WI: Multiple dot like flow voids in BG �T 2 WI: Increased signal of small vessel and cortical and white matter infarct �FLAIR: Bright sulci=leptomeningeal “ivy” sign (slow flowing engorged pial vessels , thickened arachnoid membrane �T 1 WI C+: Enhancing dots in BG correlates with lenticulostriate and thalamostriate collaterals
Imaging Angiographic finding Suzuki’s 6 angiographic stages (1) stenosis of the carotid fork (2) initial appearance of moya vessels at the base of the brain (3) intensification of moya vessels (4) minimization of moya vessels (5) reduction of moya vessels (6) disappearance of moya vessels (collaterals only from external carotid arteries)

Epidemiology Moyamoya disease has a bimodal age distribution with peaks in the first and fourth decades of life. Moyamoya affects children, adolescents, and young adults most frequently

Clinical sign And symptom �Childhood moya is characterized by ischemic manifestations, whereas adult moya disease presents with hemorrhagic manifestations �Moyamoya disease may cause TIAs, including hemodynamic paraparetic TIAs secondary to watershed paracentral lobule ischemia. TIAs are often precipitated by crying, blowing, or hyperventilation. �Other sign and symptos are headaches, seizures , movement disorders (chorea, hemidystonia, hemichoreoathetosis), mental deterioration, cerebral infarction, or intracranial hemorrhage
Treatment �The optimal treatment of ischemic moya has not been determined. Platelet antiaggregants, vasodilators, calciumchannel blockers, and corticosteroids have been used with variable results. �Anticoagulants are not useful. �Good results have been reported with superficial temporal artery to MCA anastomosis and other indirect or combined surgical revascularization procedures. �No clear superior therapy to prevent rebleeding has been shown in the hemorrhagic type of moya disease. �
THE END
 Moyamoya mra
Moyamoya mra Choosing and narrowing a topic
Choosing and narrowing a topic Broadening and narrowing
Broadening and narrowing Narrowing topic
Narrowing topic Examples of pejoration
Examples of pejoration Peristaltic contraction
Peristaltic contraction Semantic narrowing
Semantic narrowing Foraminotomy icd 10
Foraminotomy icd 10 Reciprocal narrowing
Reciprocal narrowing What is thesis statement
What is thesis statement Broad topic and specific topic examples
Broad topic and specific topic examples Aanimin
Aanimin Mike filsaime
Mike filsaime Jose moya otero
Jose moya otero Moya teklu
Moya teklu Javier royo psiquiatra consulta
Javier royo psiquiatra consulta