Monitor and Manage Payments from ThirdParty Payers Financial


- Slides: 36
Monitor and Manage Payments from Third-Party Payers Financial Management Change Package Best Practice 3
Financial Management Change Package Best Practice Recommendations 1. Charge the correct payer and optimal amount 2. Monitor and manage client fee collections 3. Monitor and manage payments from third-party payers (TPPs) Link: https: //www. fpntc. org/resources/financial-management-change- 2
Meeting Objectives By the end of today, you should be able to: • Describe the importance of monitoring and managing payments from third-party payers • Describe challenges related to monitoring and managing payments from third-party payers • Describe at least one strategy to monitoring and managing payments from third-party payers • Describe one tool available to manage collections 3
Financial Management Change Package: Best Practice 3 Monitor and manage payments from third-party payers 4
Rationale for Monitoring and Managing Payments from TPPs • Monitoring and managing payment from TPPs for services provided is an important component of managing financial health • To ensure you are receiving expected payments in a timely fashion • To identify/resolve issues and trends that are slowing down the reimbursement process 5
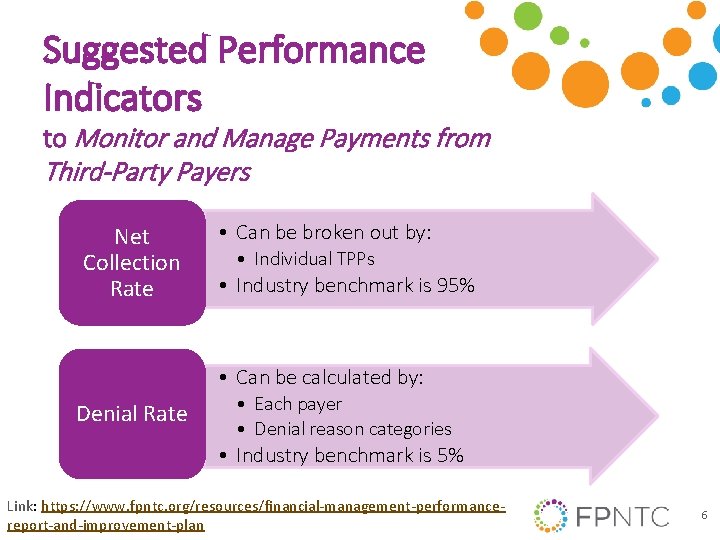
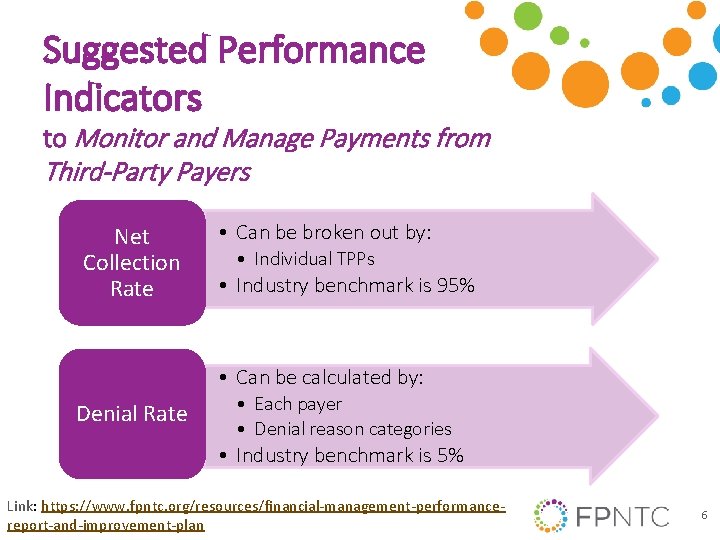
Suggested Performance Indicators to Monitor and Manage Payments from Third-Party Payers Net Collection Rate • Can be broken out by: • Individual TPPs • Industry benchmark is 95% • Can be calculated by: Denial Rate • Each payer • Denial reason categories • Industry benchmark is 5% Link: https: //www. fpntc. org/resources/financial-management-performancereport-and-improvement-plan 6
Suggested Performance Indicators to Monitor and Manage Payments from Third-Party Payers (cont. ) • Can by measured /sorted by: A/R Aging • Site • TPP • Clinician Link: https: //www. fpntc. org/resources/financial-management-performancereport-and-improvement-plan 7
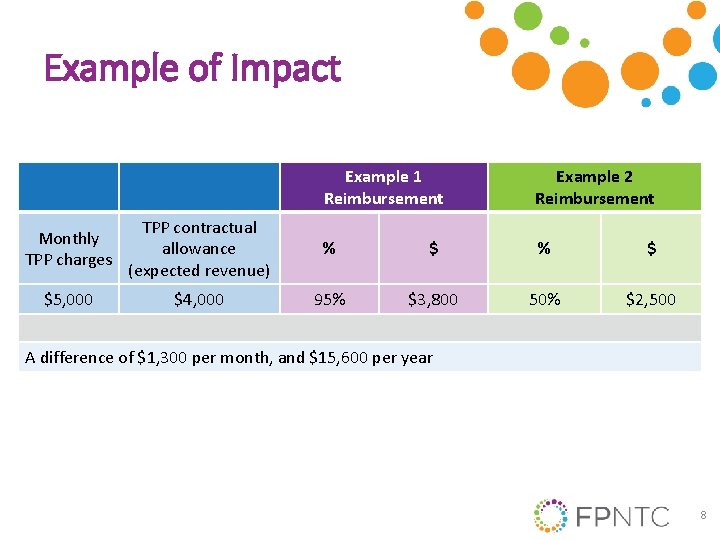
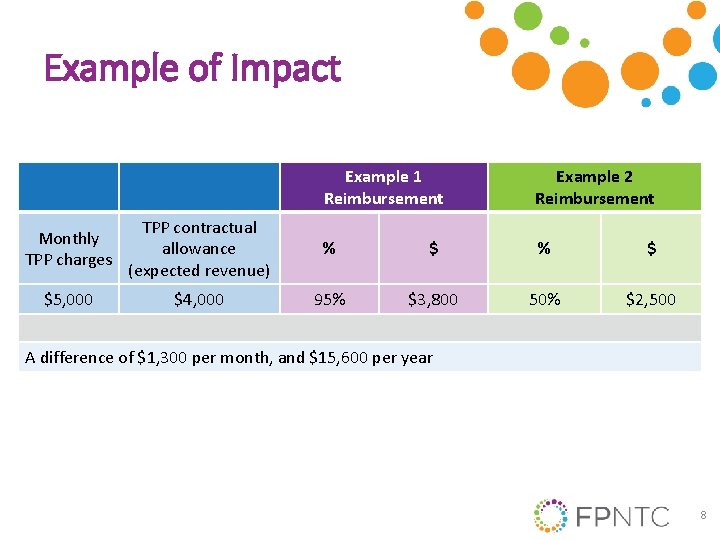
Example of Impact Example 1 Reimbursement Example 2 Reimbursement Monthly TPP charges TPP contractual allowance (expected revenue) % $ $5, 000 $4, 000 95% $3, 800 50% $2, 500 A difference of $1, 300 per month, and $15, 600 per year 8

Discussion of Challenges What are your agency’s challenges related to monitoring and managing payments from third-party payers? 9
Discussion of Challenges (cont. ) • • Time Training Unclear policies and procedures Data extraction issues – User knowledge – System limitations 10
Overview of Strategies for Best Practice 3 • • Develop/implement detailed written policies Analyze accounts receivable (A/R) on a monthly basis Analyze denial rates and trends on a monthly basis Implement strategies to manage TPP contract terms and relationships Link: https: //www. fpntc. org/resources/financial-management-change- 11
Strategies for Developing Policies and Procedures • Think about frequency or approach to reviewing and/or developing polices and procedures • Items to address in agency’s policies and procedures: • • • Gathering TPP insurance information Client communications Insurance verification process Prior authorization process Billing/collecting for TPP client fees Billing frequency 12
Strategies for Developing Policies and Procedures (cont. ) • More items to address: • Follow up on: • pending claims • denials • partial payments • Payment posting • Adjustment/write-off policies • Client acknowledgment of financial policies and procedures • Training and observing team 13
Strategies for A/R Management Accounts receivable (A/R) is the amount of money that is owed to your agency for services provided and for which you billed • A/R management involves running a variety of reports, analyzing data, and resolving A/R issues • Review A/R monthly • Identify information to compile manually, in the event of system or data extraction challenges 14
A/R Management Reports Run reports to analyze the following data: • • A/R aging Claims receivable Charges Insurance payments Denied claims Adjustments/write-offs Payment posting 15
A/R Aging Report • An A/R aging report distributes what is due by how old the money owed is • Allows high-level view/problem identification • Measure expected (contract allowed amount) revenue vs. charges 16
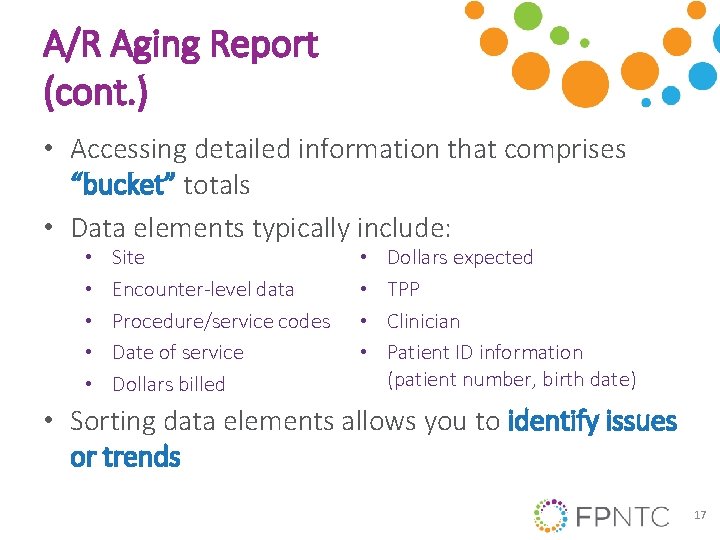
A/R Aging Report (cont. ) • Accessing detailed information that comprises “bucket” totals • Data elements typically include: • • • Site Encounter-level data Procedure/service codes Date of service Dollars billed • • Dollars expected TPP Clinician Patient ID information (patient number, birth date) • Sorting data elements allows you to identify issues or trends 17
Reviewing A/R Aging Report • Identify data that “stand” out • Compare months to determine trends • Assess A/R amounts in each age bucket • Typically largest A/R amounts is in 0 -30 • Overall decrease is good • Uncover reasons for variances between months • Use other reports to determine issues 18
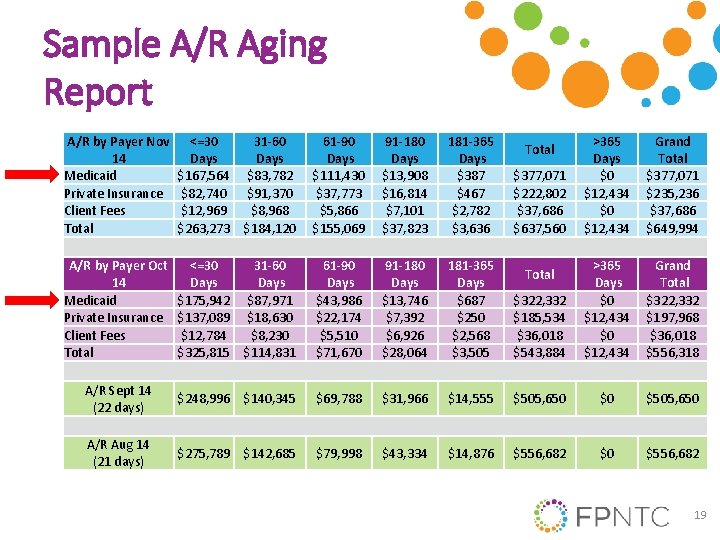
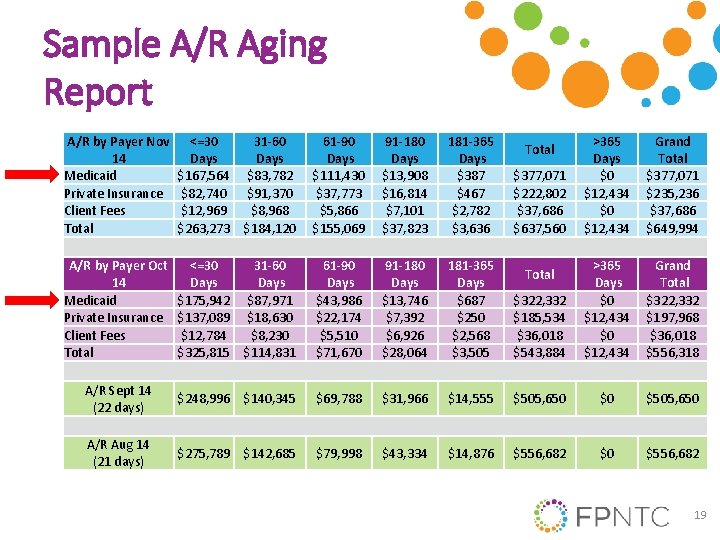
Sample A/R Aging Report A/R by Payer Nov 14 Medicaid Private Insurance Client Fees Total <=30 31 -60 Days $167, 564 $83, 782 $82, 740 $91, 370 $12, 969 $8, 968 $263, 273 $184, 120 61 -90 Days $111, 430 $37, 773 $5, 866 $155, 069 91 -180 Days $13, 908 $16, 814 $7, 101 $37, 823 181 -365 Days $387 $467 $2, 782 $3, 636 >365 Days $0 $12, 434 Grand Total $377, 071 $235, 236 $37, 686 $649, 994 A/R by Payer Oct 14 Medicaid Private Insurance Client Fees Total <=30 31 -60 Days $175, 942 $87, 971 $137, 089 $18, 630 $12, 784 $8, 230 $325, 815 $114, 831 61 -90 Days $43, 986 $22, 174 $5, 510 $71, 670 91 -180 Days $13, 746 $7, 392 $6, 926 $28, 064 181 -365 Days $687 $250 $2, 568 $3, 505 $322, 332 $185, 534 $36, 018 $543, 884 >365 Days $0 $12, 434 Grand Total $322, 332 $197, 968 $36, 018 $556, 318 A/R Sept 14 (22 days) $248, 996 $140, 345 $69, 788 $31, 966 $14, 555 $505, 650 $0 $505, 650 A/R Aug 14 (21 days) $275, 789 $142, 685 $79, 998 $43, 334 $14, 876 $556, 682 $0 $556, 682 Total $377, 071 $222, 802 $37, 686 $637, 560 Total 19
Claims Receivable Report When reviewing a claims receivable report: • Prioritize repeat issues and large dollar unpaid claims • Investigate partial payments • Take actions – Write-offs – Bill a secondary payer – Denial management (rebill) 20
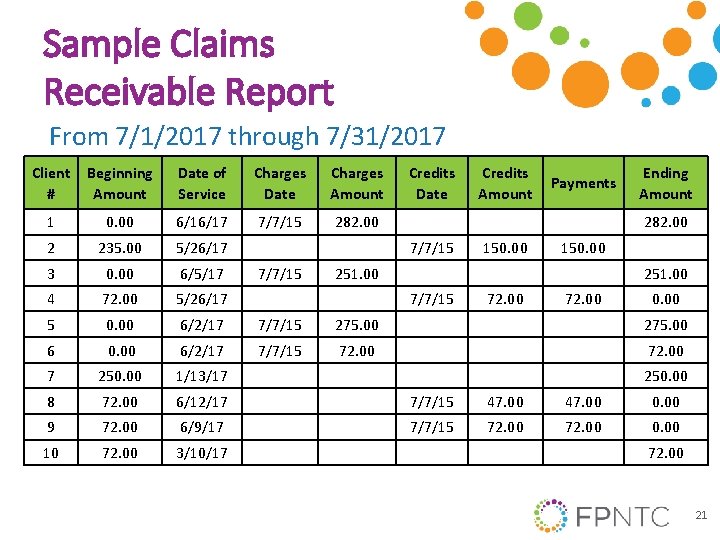
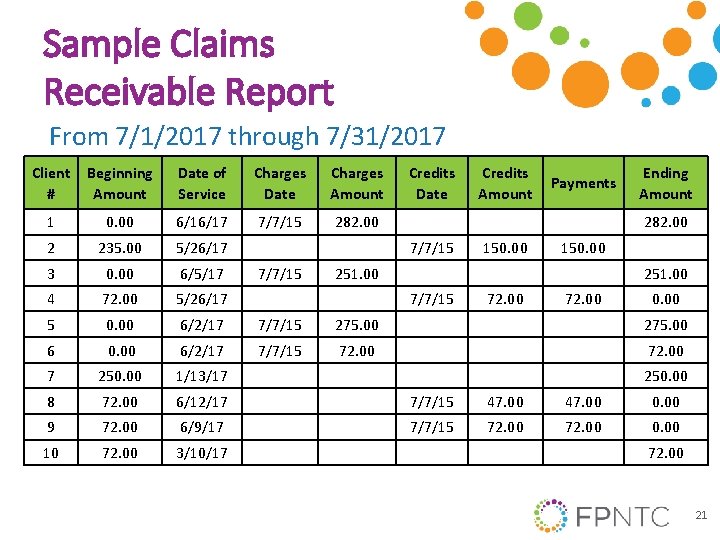
Sample Claims Receivable Report From 7/1/2017 through 7/31/2017 Client # Beginning Amount Date of Service Charges Date Charges Amount Credits Date 1 0. 00 6/16/17 7/7/15 282. 00 2 235. 00 5/26/17 3 0. 00 6/5/17 4 72. 00 5/26/17 5 0. 00 6/2/17 7/7/15 275. 00 6 0. 00 6/2/17 7/7/15 72. 00 7 250. 00 1/13/17 8 72. 00 6/12/17 7/7/15 47. 00 0. 00 9 72. 00 6/9/17 7/7/15 72. 00 0. 00 10 72. 00 3/10/17 Payments Ending Amount 282. 00 7/7/15 Credits Amount 150. 00 251. 00 7/7/15 72. 00 0. 00 250. 00 72. 00 21
Strategies for Denial Management Denial is a refusal by a TPP to pay as a result of a clinician not adhering to the insurance’s policies/procedures or pending receipt of additional information • • Analyze denial rates on a monthly basis Avoid denials* Utilize reports to analyze denials Resolve unpaid or denied claims 22
Avoid Denials Most denial types can be avoided by efforts before filing: • Registration denials Strategy: implement insurance verification processes • Credentialing denials Strategy: maintain credentials • Timely filing denials Strategy: bill weekly; monitor reports • Prior authorization denials Strategy: identify services requiring prior authorization 23
Avoid Denials (cont. ) Most denial types can be avoided by efforts before filing: • Medical necessity/charge entry denials Strategy: chart audits, scrubbing software • Bundled/non-covered denials Strategy: manage contract terms, scrubbing software 24
Analyze Denial Rates on Monthly Basis • Can help identify issues/processes that are affecting revenue and cash flow When denials occur, analyze rates and trends by: • Denied dollars by payer • Number of claims by payer • Denial reason category • For example: registration, charge entry, credentialing, pre-authorization 25
Utilize Reports to Analyze Denials Sample reports: • Denied claims • Client charge/activity file • Electronic remittance advice 26
Resolve Unpaid or Denied Claims • Call claims representative, ask specific questions Foster a good relationship with insurer contact • Document findings to minimize future denials of the type investigated Provide feedback regarding errors and corrections • Claims may have more than one denial reason and require multiple corrections to be paid
Strategies for Managing TPP Contract Relationships Documented processes to provide direction: • • • Identify new TPPs to contract with Assess elements to negotiate Maintain contract Solve problems efficiently Identifying reliable contact at TPP 28
Maintaining relationships with TPPs Why is maintaining relationships with third -party payers important to your agency? 29
Communication Tips Approaches to maintaining TPP relationships: • Build data warehouse reports • Report on HEDIS/other measures • Partner with a TPP to improve its outcomes • Share client survey results • Promptly answer all data requests • Others?
Ongoing Monitoring of TPP Contract Terms • Develop monitoring processes for contract terms to allow for prompt identification and resolution Remember: contract terms do not always translate to effective execution • Be familiar with contract terms and changes, and educate team
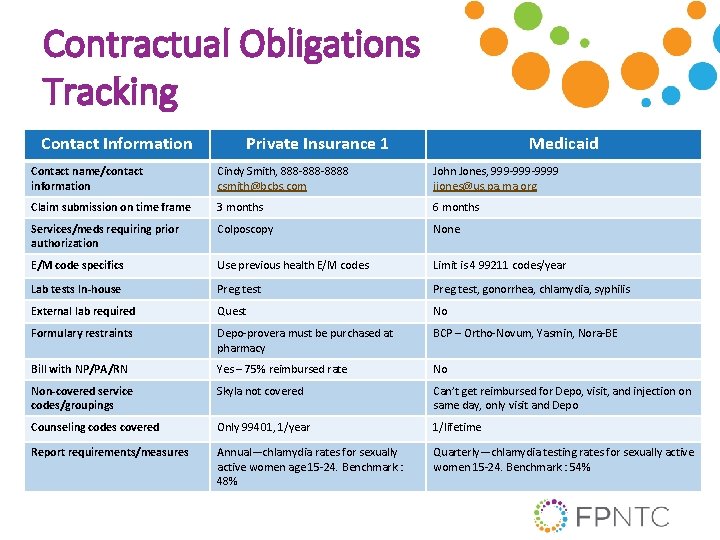
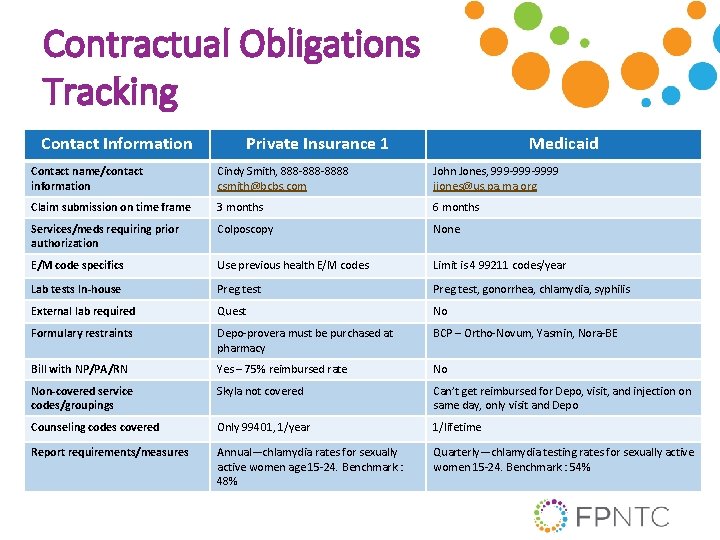
Contractual Obligations Tracking Contact Information Private Insurance 1 Medicaid Contact name/contact information Cindy Smith, 888 -8888 csmith@bcbs. com John Jones, 999 -9999 jjones@us. pa. ma. org Claim submission on time frame 3 months 6 months Services/meds requiring prior authorization Colposcopy None E/M code specifics Use previous health E/M codes Limit is 4 99211 codes/year Lab tests In-house Preg test, gonorrhea, chlamydia, syphilis External lab required Quest No Formulary restraints Depo-provera must be purchased at pharmacy BCP – Ortho-Novum, Yasmin, Nora-BE Bill with NP/PA/RN Yes – 75% reimbursed rate No Non-covered service codes/groupings Skyla not covered Can’t get reimbursed for Depo, visit, and injection on same day, only visit and Depo Counseling codes covered Only 99401, 1/year 1/lifetime Report requirements/measures Annual—chlamydia rates for sexually active women age 15 -24. Benchmark : 48% Quarterly—chlamydia testing rates for sexually active women 15 -24. Benchmark : 54%
Success Story The Louisiana Department of Health, a Title X grantee, identified through analysis that denials were a significant issue, with a baseline of 15%. The department determined eligibility denial types to be the top denial reason and sought to decrease this denial type, and, therefore, the overall denial rate. Actions taken: • Sent a memorandum on when/how to complete eligibility verifications • When denial rates did not improve, grantee sought feedback from network service sites • Based on feedback, conducted a webinar training on the process, provided one-on-one trainings at the clinics with highest rates of eligibility denials • Regional directors were trained to explain eligibility verification process • A second follow-up webinar training is planned 33
Success Story (cont. ) Results: • End-point measure: a 4% decrease in denials by October 2017 Key Points/Lessons Learned: • Be open to changing training methodology related to household assessment and eligibility checks • Include more interaction between staff and adjusting time frames in implementation 34
What other questions do you have? What other issues would you like to discuss? 35

Thank you! Contact: fpntc@jsi. com 36