MedicalSurgical Nursing Concepts Practice 3 rd edition Chapter



























- Slides: 98
Medical-Surgical Nursing: Concepts & Practice 3 rd edition Chapter 42 Care of Patients with Integumentary Disorders and Burns Copyright © 2017, Elsevier Inc. All rights reserved.
Theory Objectives Describe the etiology of dermatitis. Plan psychosocial interventions for the patient who has psoriasis. Compare and contrast the treatment of fungal skin or nail disorders to the treatment of bacterial skin disorders. List the main nursing care points for patients with herpes virus infections. Copyright © 2017, Elsevier Inc. All rights reserved. 2

Theory Objectives (Cont. ) Discuss the types of acne and their treatment. Compare the characteristics of the various types of skin cancer. Analyze the important points of caring for an immobile patient to prevent pressure ulcers. Prepare care plan interventions for each stage of a pressure ulcer. Copyright © 2017, Elsevier Inc. All rights reserved. 3
Theory Objectives (Cont. ) Summarize important assessment points for the patient who has sustained a burn. Evaluate the nurse’s role in emergency burn care. Evaluate the psychosocial needs and interventions for burn patients. Describe the process of rehabilitation for the patient with a major burn. Copyright © 2017, Elsevier Inc. All rights reserved. 4
Clinical Practice Objectives Teach a family about care for the patient and home when scabies is present. Assess the skin of family members for signs of skin cancer. Provide care for a patient with stage III or stage IV pressure ulcer. Apply Standard Precautions and sterile techniques for the care of a burn. Visit a burn intensive care unit and observe the wound care of a patient who is in acute stage of a major burn. Copyright © 2017, Elsevier Inc. All rights reserved. 5
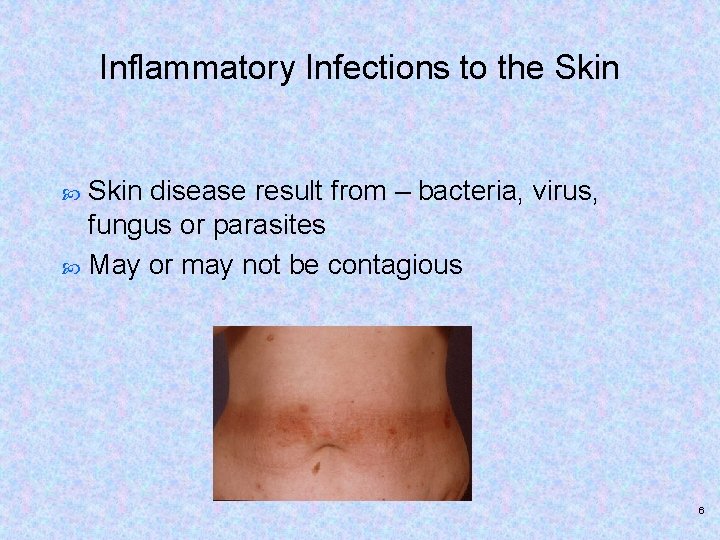
Inflammatory Infections to the Skin disease result from – bacteria, virus, fungus or parasites May or may not be contagious 6

Dermatitis Not contagious unless there is a secondary infection in the lesions Ø Contact dermatitis – cell mediated immunity= allergen bound to protein carrier forms antigen then T cells become sensitized to the antigen. Cosmetics, soaps, latex, poison ivy, chemical irritants cause such a reaction Copyright © 2017, Elsevier Inc. All rights reserved. 7

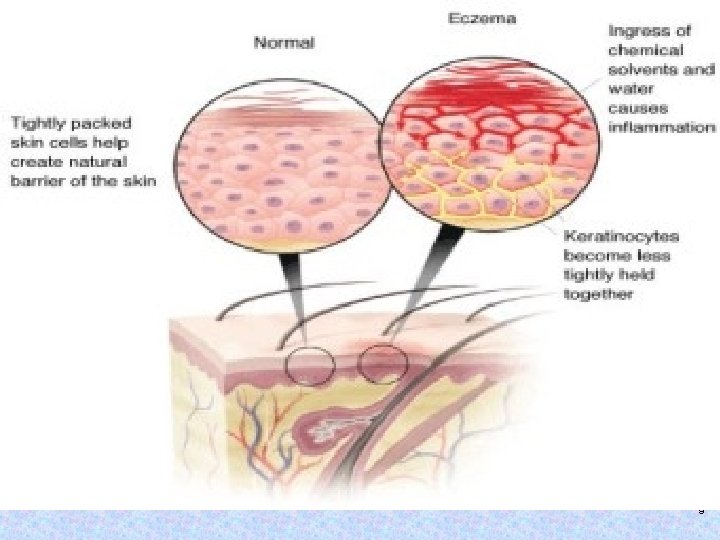
Atopic dermatitis – common with infants/children Complex activation process – more prevalent in families 8
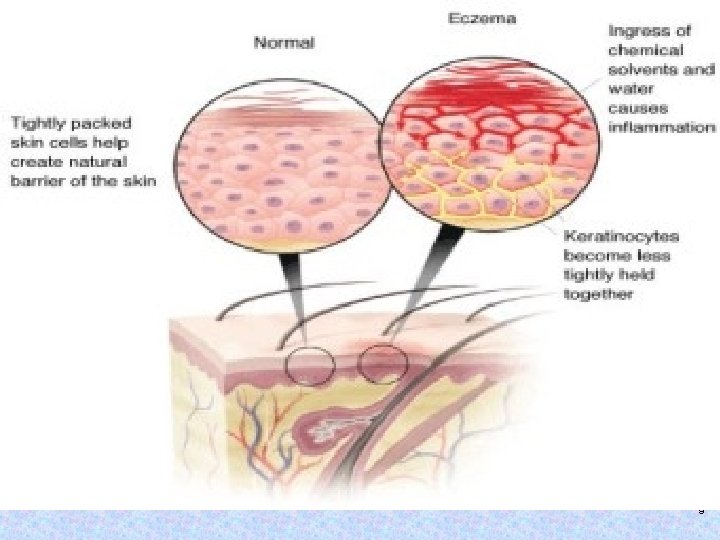
9

Stasis dermatitis – occurs in legs as a result of venous statis and edema –varicosities, phlebitis and vascular trauma. Develop lesions which may become ulcerated 10
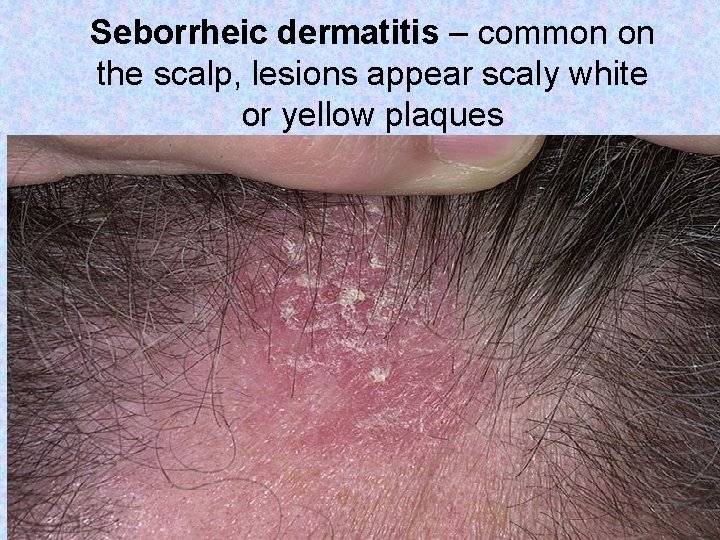
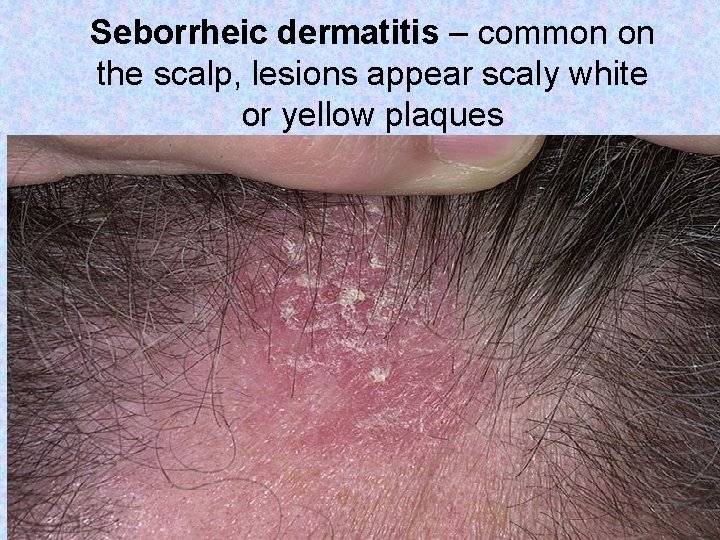
Seborrheic dermatitis – common on the scalp, lesions appear scaly white or yellow plaques 11

Dermatitis Diagnosis and treatment – visual inspection, hx looking for possible causative substances Nursing management – avoidance of substance, applying ointments correctly and good skin care. If the patient has pruritus – avoid getting hot, bathe in tepid water and don’t puncture vesicles. 12
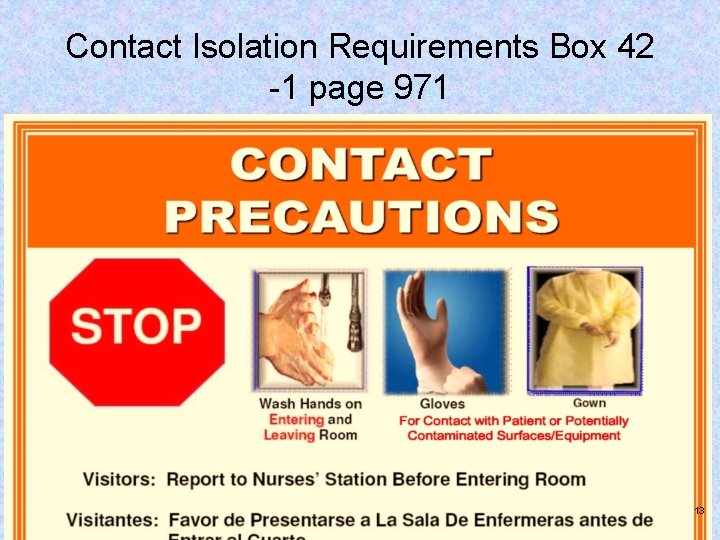
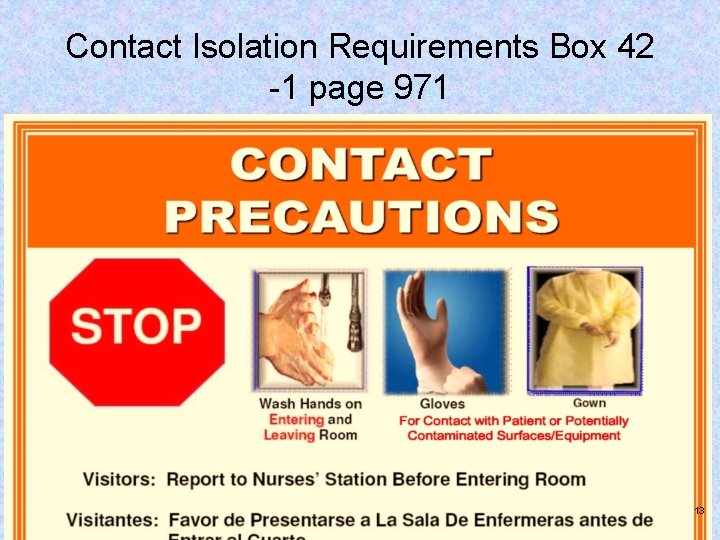
Contact Isolation Requirements Box 42 -1 page 971 13

Audience Response Question 1 In managing dermatitis, the nurse provides which instruction(s)? (Select all that apply. ) 1. 2. 3. 4. 5. Avoid the irritant or allergen. Provide adequate skin lubrication. Wash skin frequently with germicidal soaps. Maintain skin moisture. Apply steroid-based preparations. Copyright © 2017, Elsevier Inc. All rights reserved. 14
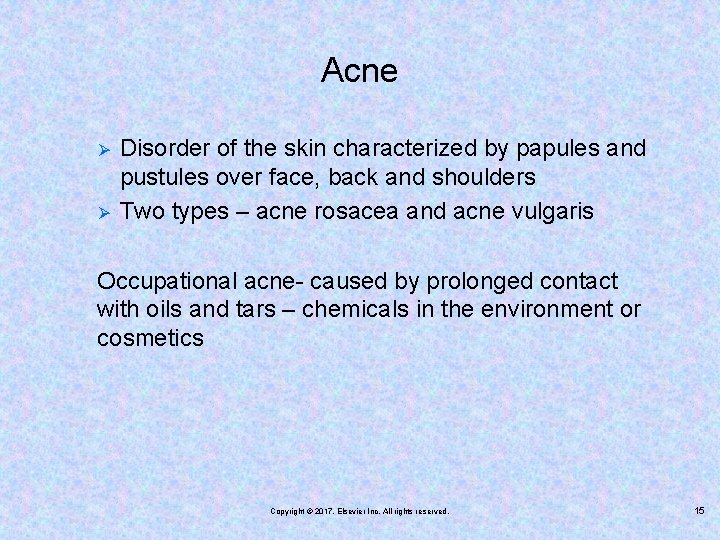
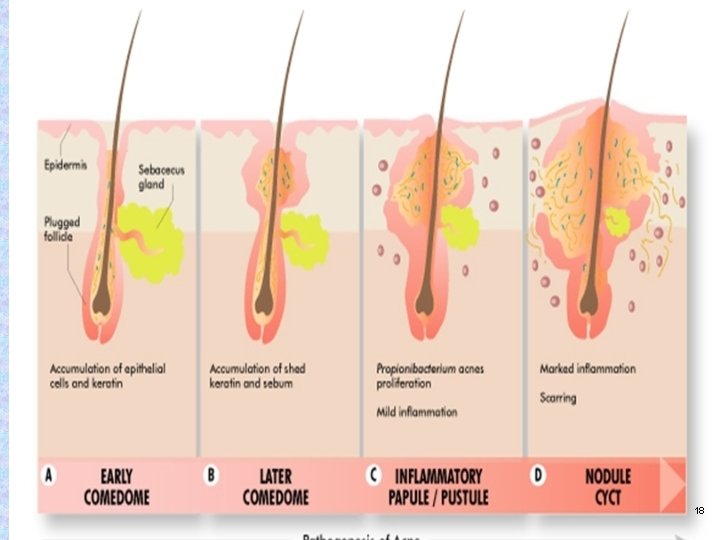
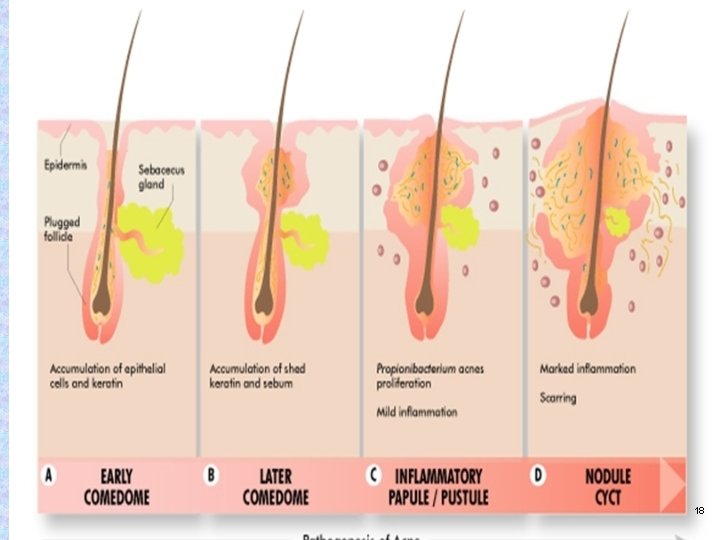
Acne Ø Ø Disorder of the skin characterized by papules and pustules over face, back and shoulders Two types – acne rosacea and acne vulgaris Occupational acne- caused by prolonged contact with oils and tars – chemicals in the environment or cosmetics Copyright © 2017, Elsevier Inc. All rights reserved. 15
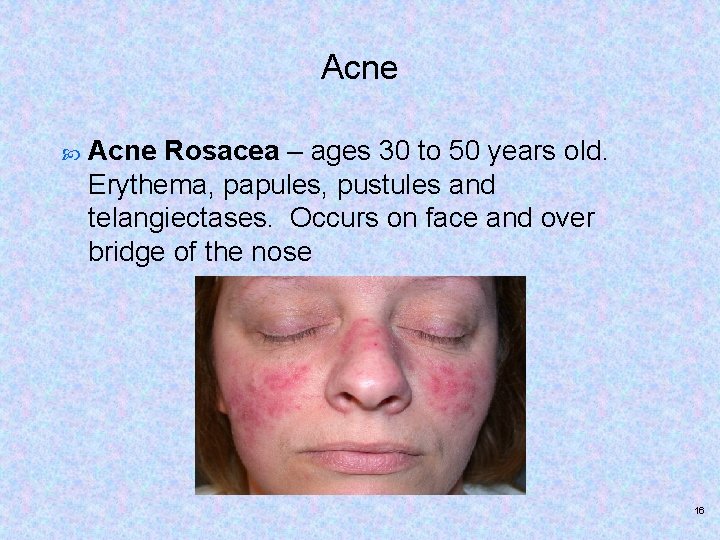
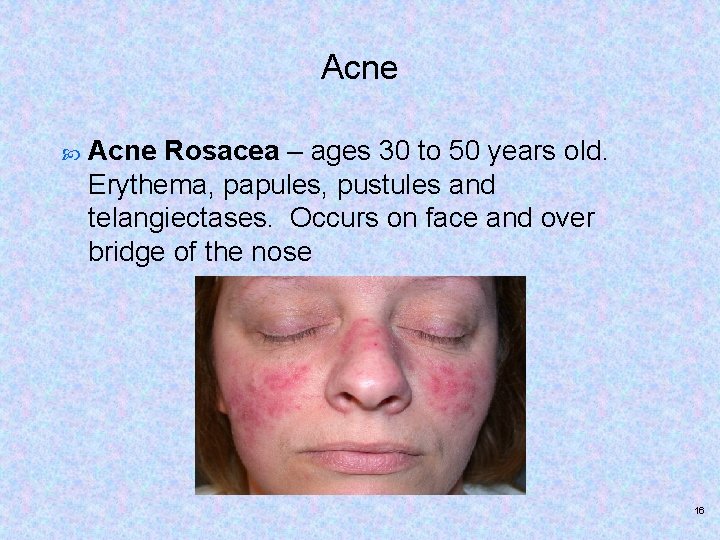
Acne Rosacea – ages 30 to 50 years old. Erythema, papules, pustules and telangiectases. Occurs on face and over bridge of the nose 16
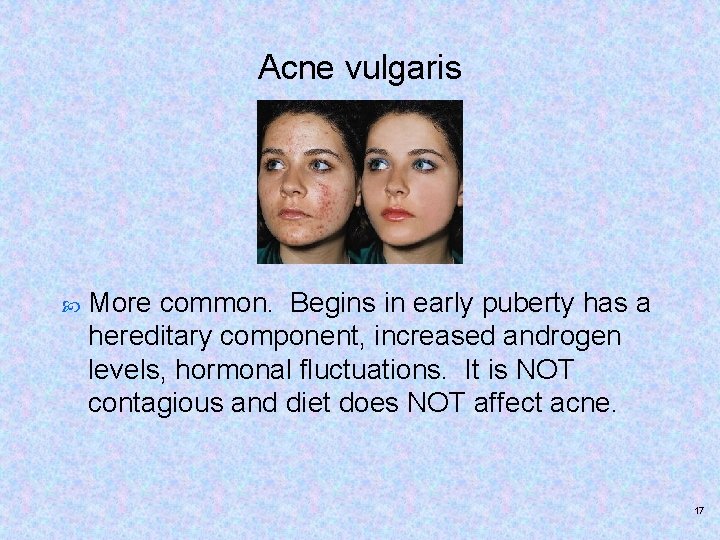
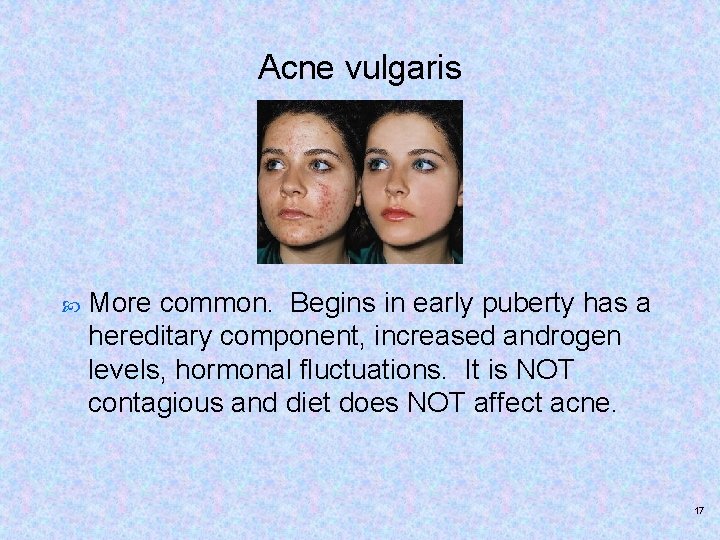
Acne vulgaris More common. Begins in early puberty has a hereditary component, increased androgen levels, hormonal fluctuations. It is NOT contagious and diet does NOT affect acne. 17
18
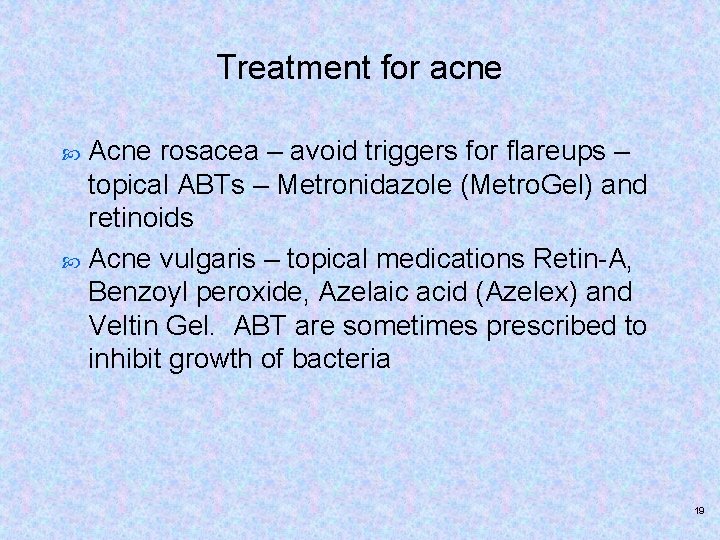
Treatment for acne Acne rosacea – avoid triggers for flareups – topical ABTs – Metronidazole (Metro. Gel) and retinoids Acne vulgaris – topical medications Retin-A, Benzoyl peroxide, Azelaic acid (Azelex) and Veltin Gel. ABT are sometimes prescribed to inhibit growth of bacteria 19
Acne- Nursing Managment Patient and families need support for physiologic and psychosocial support Wash face with mild soap, scrubbing skin not recommended, if hair is oily wash frequently and keep off the face, squeezing outbreaks may press sebum into the clogged duct increasing chances of inflammation and possibly spreading infection 20

Accutane – side effects Accutane – effective in control of cystic acne found to have many severe side effects. Accutane discontinued in 2009, but still available in generic form Should only be used for severe cystic acne-side effects include organ damage and mental problems Almost all patients experienced some side effect to this drug 21
Audience Response Question 2 A teenager asks the nurse at the dermatologist’s office, “What is acne vulgaris? ” Which statement(s) would be true? (Select all that apply. ) 1. 2. 3. 4. 5. “Accumulations of sebum in occluded sebaceous glands. ” “It is caused by increased androgens and fluctuating premenstrual hormones. ” “Application of heavy creams and heat exposure contribute to the development of acne. ” “Alcohol, caffeine-containing foods, spicy foods, sunlight, and emotional stress cause flare-ups. ” “These lesions are not a sign of uncleanliness. ” Copyright © 2017, Elsevier Inc. All rights reserved. 22
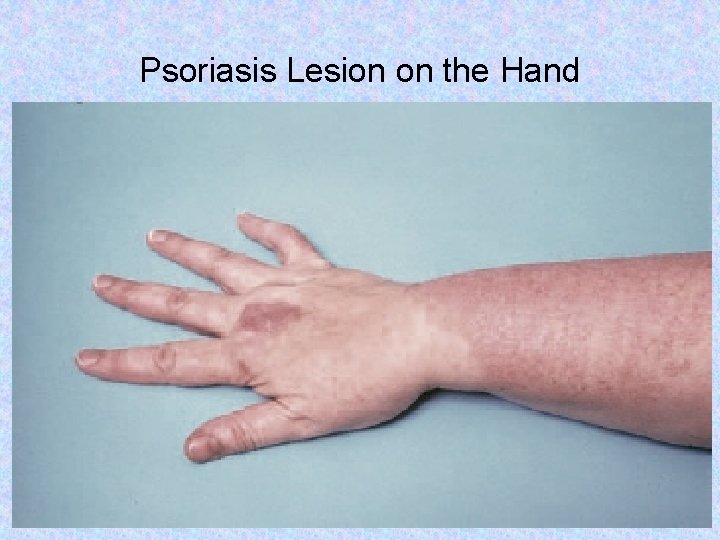
Psoriasis Not contagious Chronic Affects 2% of U. S. population, family component Inflammed, edematous skin lesions covered with scales Scales are a result of abnormal rapid rate of proliferation of skin cells. Appear on elbows, fingernails, knees and base of the spine. May also appear on palms and soles of feetaffected patient’s ability to perform ADLs. Copyright © 2017, Elsevier Inc. All rights reserved. 23
Psoriasis Dx and Tx Dx determined by physical exam to rule out other skin disorders Steroids creams triamcinolone acetonide (Kenalog) UV light slows down rate cells are produced Calcipotriene (Dovonex) Vit D analog cream regulates skin cell production Coal tar products with UV radiation PUVA therapy 24
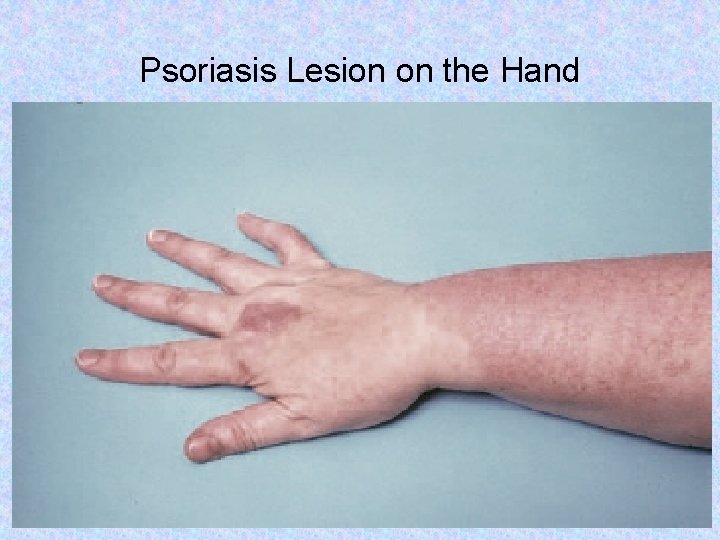
Psoriasis Lesion on the Hand From Ignatavicius DD, Workman ML: Medical-surgical nursing: patient-centered collaborative care, ed. 6, Philadelphia, 2010, Saunders. Copyright © 2017, Elsevier Inc. All rights reserved. 25
Nursing Management Skin kept moist – humidifiers used to keep moisture in environment Lotions and creams applied three min after showering Caution against abrasions – may lead to additional growth of psoriatic plaques 26
Stevens-Johnson Syndrome Signs and symptoms –allergic reaction with skin manifestations within 14 days of starting a drug therapy Ø Ø Anticonvulsants carbamazepine (Tegretol) and phenytoin (Dilantin), the antimalarial sulfadoxine– pyrimethamine (Fansidar), and the antibiotic Sulfamethoxazole- sulfamethoxazole (Bactrim, Septra) OTC medications can also cause SJS Copyright © 2017, Elsevier Inc. All rights reserved. 27
Stevens-Johnson Syndrome Nursing interventions…. Discontinue the drug. Provide supportive care – fluids & nutrition Provide wound care – similar to that of a burn. 28
Bacterial Infections of the Skin Cellulitis – infection of dermis and subcutaneous tissue – generally caused by Staphylococcus. Cellulitis appears as a swollen, red area of skin that feels hot and tender. It can spread rapidly to other parts of the body. Skin on lower legs is most commonly affected it may also affect tissues underlying your skin and can spread to your lymph nodes and bloodstream. If untreated, can be life-threatening. Copyright © 2017, Elsevier Inc. All rights reserved. 29
Cellulitis 30
Cellulitis Treatment Risk factors for developing cellulitis include intravenous drug use, chronic skin conditions that weaken the skin surface, fungal skin infections and lowered immunity. 31

Bacterial infections of the skin Furuncles (boils) – inflammation of hair follicles usually staphylococcus aureus Carbuncles – collection of infected hair follicles Tx: warm compresses, incision and drainage antibiotics for recurrent episodes 32
Viral Infections of the Skin Herpes Simplex Herpes simplex virus type 1 (HSV-1) lesions are primarily nongenital most commonly causes cold sores. Herpes simplex virus type 2 (HSV-2) is most often associated with genital herpes. This is a STD virus. Can be transmitted without lesions visible. Contagion is possible up to 5 days after appearance of the lesion Copyright © 2017, Elsevier Inc. All rights reserved. 33
Herpes simplex 34

Herpes Simplex (Cont. ) Copyright © 2017, Elsevier Inc. All rights reserved. 35
Herpes Simplex (Cont. ) Etiology and pathophysiology – virus infects and imbeds the nerve ganglion on the site of the lesion, can be reactivated by stress, light, skin irritation, fatigue or stress Diagnosis Ø History and physical examination Treatment – topical or oral acyclovir (Zovirax), famciclovir (Famvir) or valacyclovir (Valtrex) Nursing management Ø Good personal hygiene helpful to prevent spread of the virus Copyright © 2017, Elsevier Inc. All rights reserved. 36
Herpes Zoster (Shingles) chickenpox virus Etiology and pathophysiology Ø Ø Ø Dormant in peripheral nerve ganglia and can be reactivated by trauma, malignancy, or local radiation High risk: immunocompromised individuals (HIV/AIDs, cancer patients) Vaccine available Zostavax is 50% effective for 6 years Signs and symptoms Ø Ø Ø Low grade temp Aching or discomfort along the nerve pathway 3 to 5 days after onset, vesicles found on trunk following nerve pathway Copyright © 2017, Elsevier Inc. All rights reserved. 37

Herpes Zoster (Shingles) (Cont. ) Copyright © 2017, Elsevier Inc. All rights reserved. 38
Diagnosis and Treatment History and physical examination Symptomatic treatment – very painful for several days or weeks after the skin lesions are healed. Topic analgesic 5 x a day. Antibiotics against secondary bacterial infection – acyclovir (Zovirax), famciclovir (Famvir) valacyclovir (Valtrex) Systemic corticosteroids to reduce inflammation Copyright © 2017, Elsevier Inc. All rights reserved. 39
Herpes Zoster - Precautions Visitors, health care workers should NOT be in contact with patient if they have never had the virus Pregnant health care workers should not care for a patient with the virus – can harm fetus Initiate isolation procedures based on symptoms rather than wait for diagnosis Transmission precautions until all blisters are crusted 40
Fungal Infections of the Skin Fungal infections are called mycoses 41
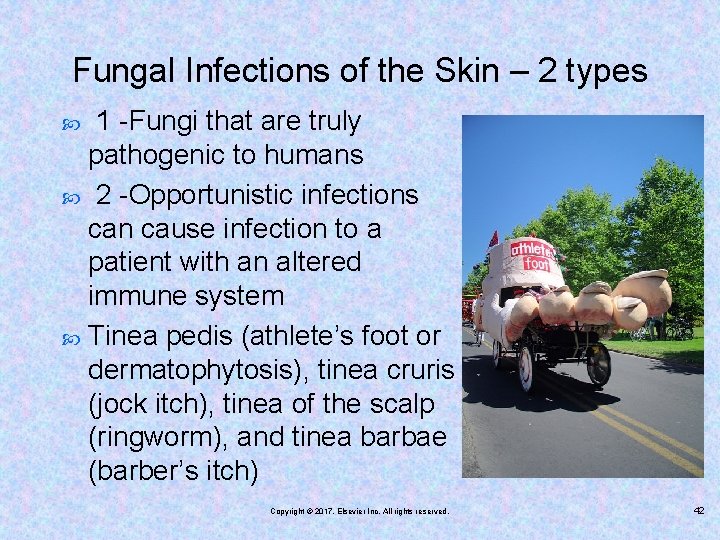
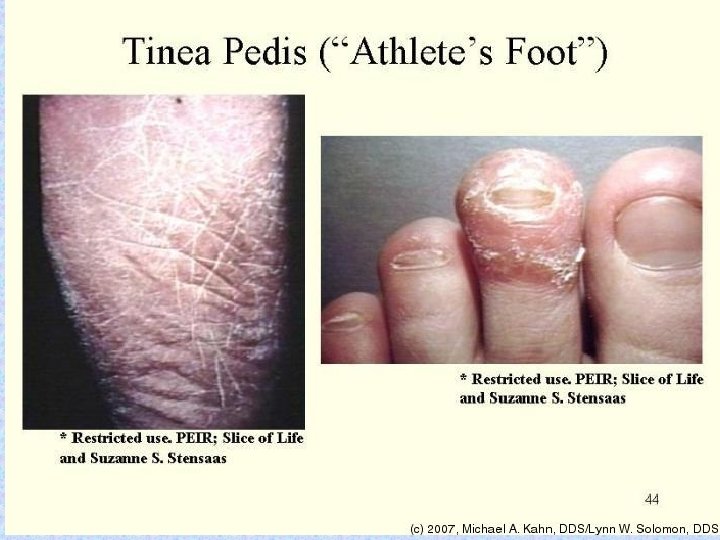
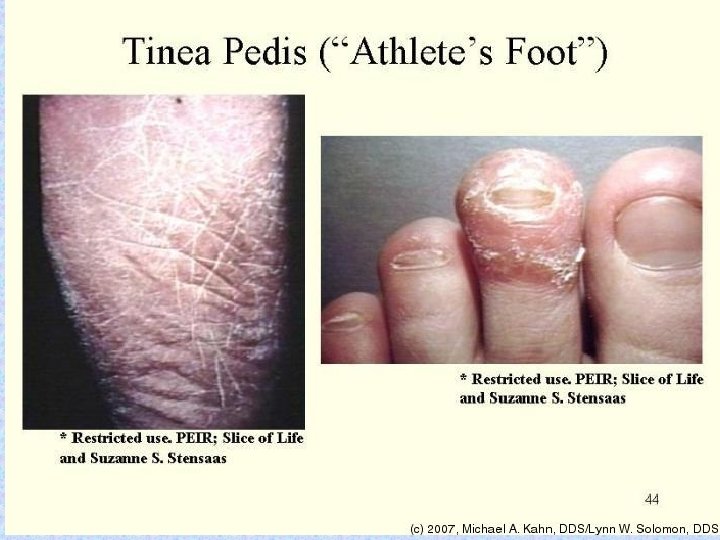
Fungal Infections of the Skin – 2 types 1 -Fungi that are truly pathogenic to humans 2 -Opportunistic infections can cause infection to a patient with an altered immune system Tinea pedis (athlete’s foot or dermatophytosis), tinea cruris (jock itch), tinea of the scalp (ringworm), and tinea barbae (barber’s itch) Copyright © 2017, Elsevier Inc. All rights reserved. 42

ringworm 43
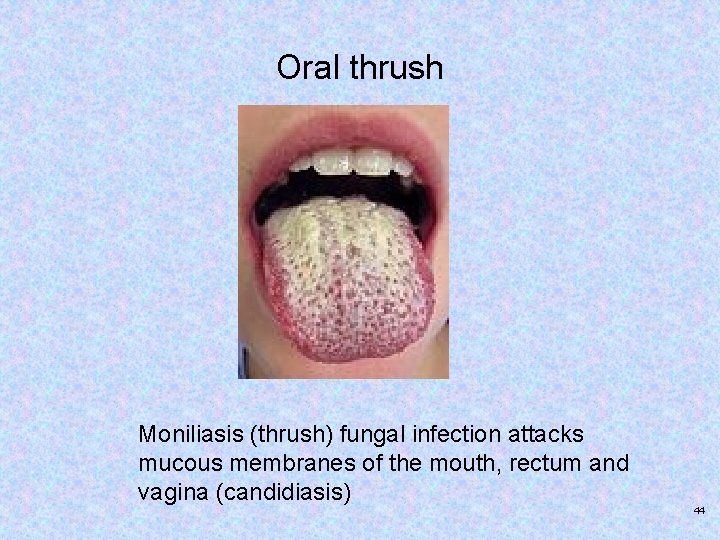
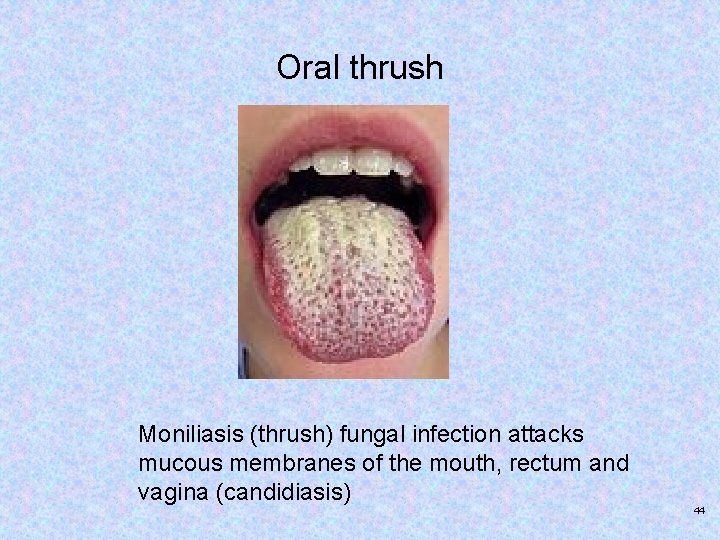
Oral thrush Moniliasis (thrush) fungal infection attacks mucous membranes of the mouth, rectum and vagina (candidiasis) 44
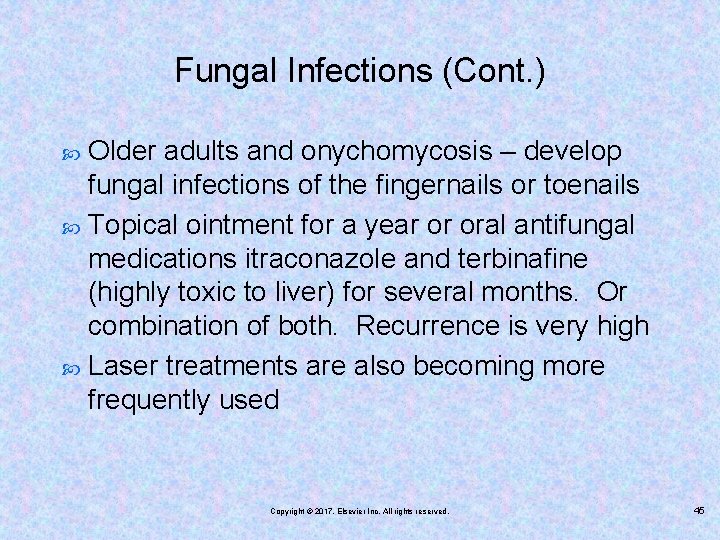
Fungal Infections (Cont. ) Older adults and onychomycosis – develop fungal infections of the fingernails or toenails Topical ointment for a year or oral antifungal medications itraconazole and terbinafine (highly toxic to liver) for several months. Or combination of both. Recurrence is very high Laser treatments are also becoming more frequently used Copyright © 2017, Elsevier Inc. All rights reserved. 45
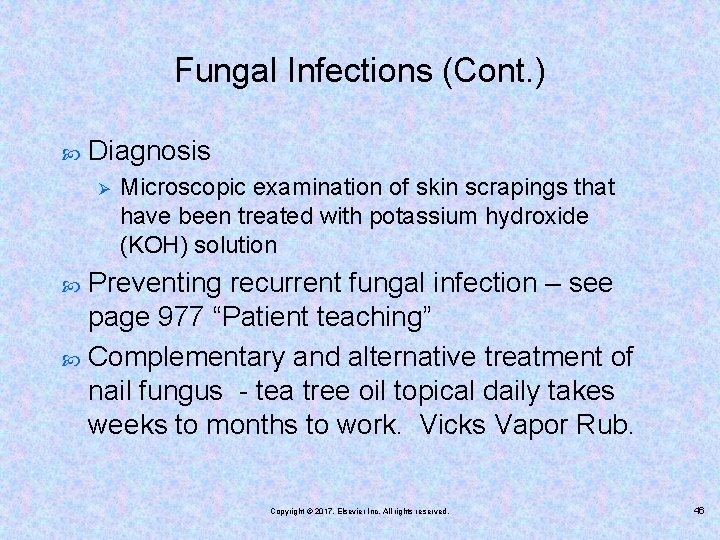
Fungal Infections (Cont. ) Diagnosis Ø Microscopic examination of skin scrapings that have been treated with potassium hydroxide (KOH) solution Preventing recurrent fungal infection – see page 977 “Patient teaching” Complementary and alternative treatment of nail fungus - tea tree oil topical daily takes weeks to months to work. Vicks Vapor Rub. Copyright © 2017, Elsevier Inc. All rights reserved. 46

Onychomycosis (Nail Fungus) Copyright © 2017, Elsevier Inc. All rights reserved. 47
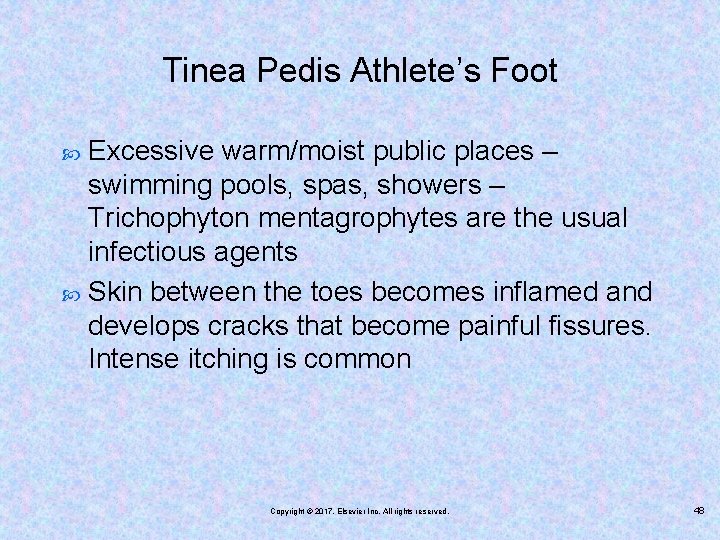
Tinea Pedis Athlete’s Foot Excessive warm/moist public places – swimming pools, spas, showers – Trichophyton mentagrophytes are the usual infectious agents Skin between the toes becomes inflamed and develops cracks that become painful fissures. Intense itching is common Copyright © 2017, Elsevier Inc. All rights reserved. 48
49

Tinea Pedis Dx: physical exam Tx: keep area dry, clean, exposed to air and sunlight. Burow solution soaks. Topical antifungals: ketoconazole (Nizoral), econazole (Spectazole) Naftifine (Naftin) plus oral medications itraconzole (Sporanox) terbinafine (Lamisil) Nursing mgt: daily regular application of ointment, use own towel, clean shower area to prevent transmission 50

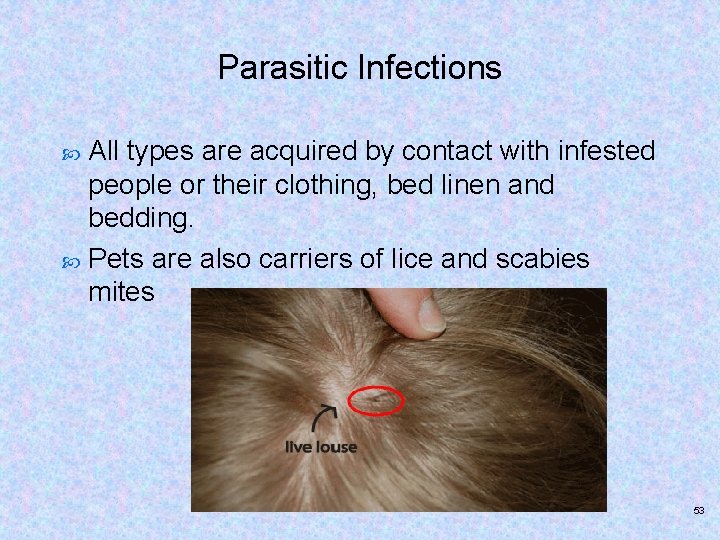
Parasitic Infections of the Skin Pediculosis and Scabies Etiology and pathophysiology Ø Ø Ø The head louse, Pediculus humanus capitis The body louse, Pediculus humanus corporis The pubic or crab louse, Phthirus pubis Schools, nursing homes, dormitories – parasites can infest anyone Signs and symptoms Ø Severe itching leading to excoriation Diagnosis Ø Body inspection and examination of skin scraping Copyright © 2017, Elsevier Inc. All rights reserved. 51
lice 52
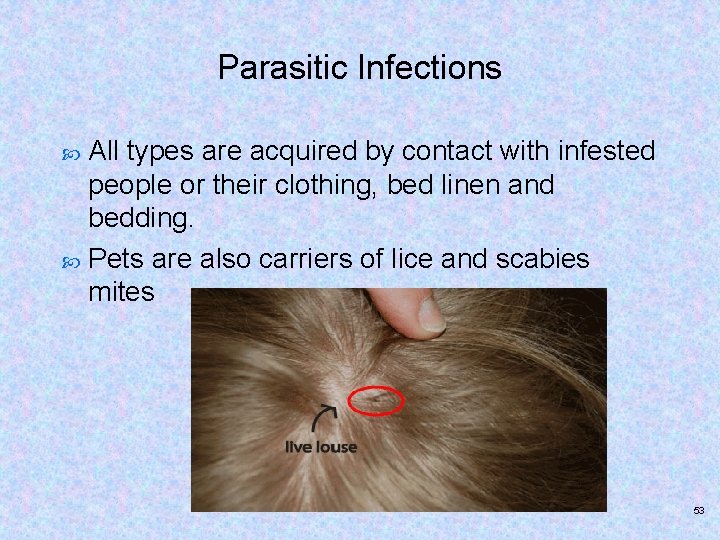
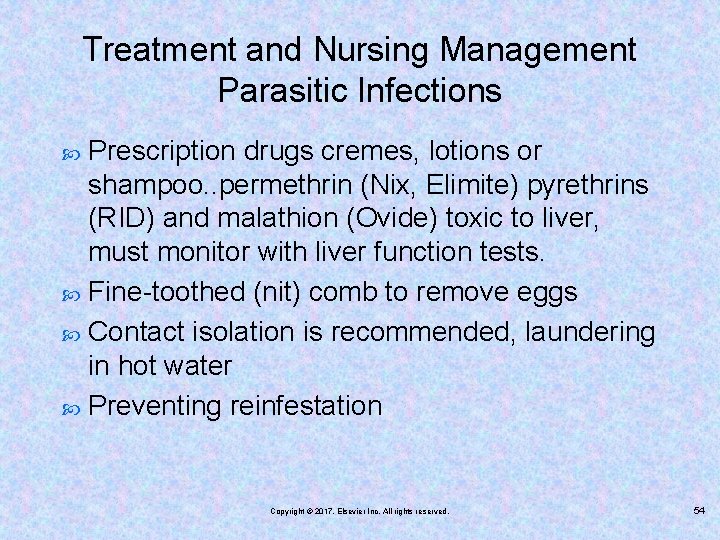
Parasitic Infections All types are acquired by contact with infested people or their clothing, bed linen and bedding. Pets are also carriers of lice and scabies mites 53
Treatment and Nursing Management Parasitic Infections Prescription drugs cremes, lotions or shampoo. . permethrin (Nix, Elimite) pyrethrins (RID) and malathion (Ovide) toxic to liver, must monitor with liver function tests. Fine-toothed (nit) comb to remove eggs Contact isolation is recommended, laundering in hot water Preventing reinfestation Copyright © 2017, Elsevier Inc. All rights reserved. 54
Audience Response Question 3 The nurse who observes evidence of severe itching on the scalp of a school-aged girl with pediculosis should give which important instruction(s)? (Select all that apply. ) 1. 2. 3. 4. 5. “Machine wash clothes and bedding using the coldest cycle. ” “Share combs and hair brushes. ” “Soak all combs and brushes in very hot water for more than 5 minutes. ” “Seal items that cannot be washed in air-expelled plastic bags for 14 days. ” “Instruct all family members about the infestation and ways to prevent reinfestation. ” Copyright © 2017, Elsevier Inc. All rights reserved. 55
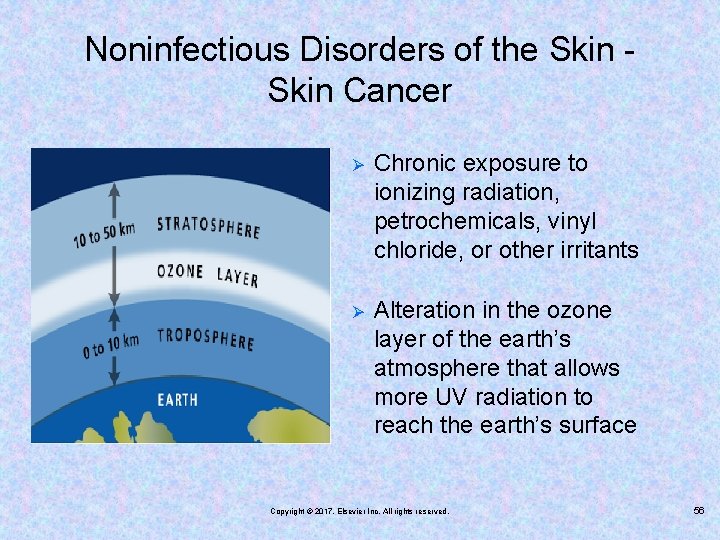
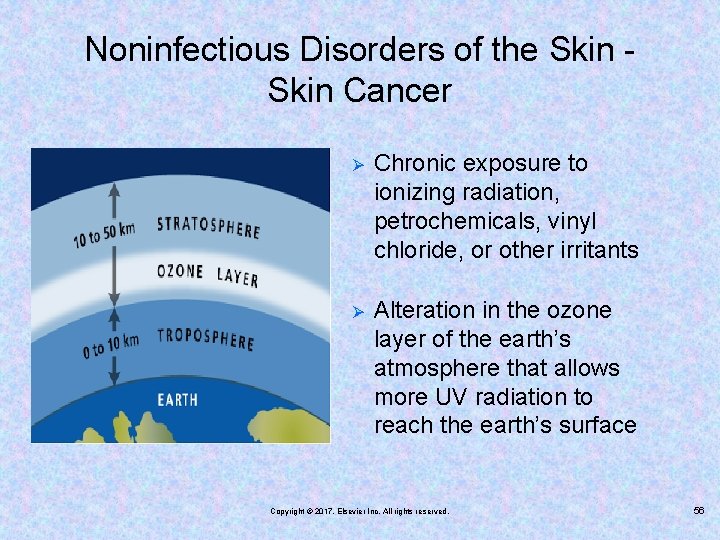
Noninfectious Disorders of the Skin Cancer Ø Chronic exposure to ionizing radiation, petrochemicals, vinyl chloride, or other irritants Ø Alteration in the ozone layer of the earth’s atmosphere that allows more UV radiation to reach the earth’s surface Copyright © 2017, Elsevier Inc. All rights reserved. 56

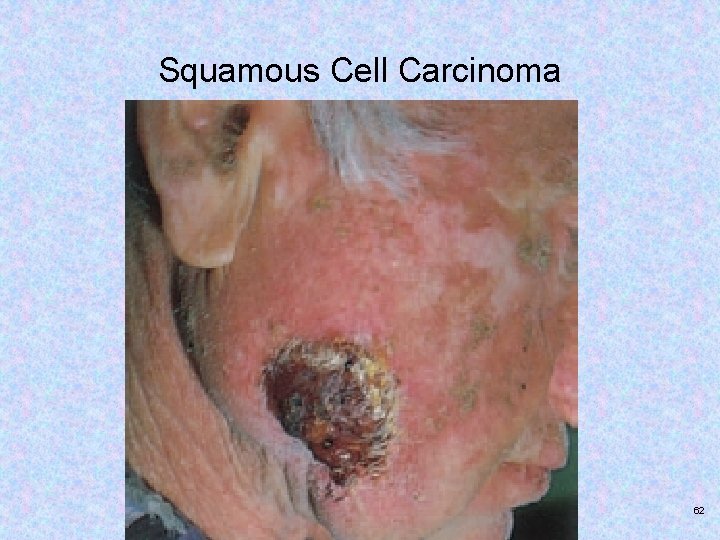
Three Major Types of Skin Cancer – page 980 Table 42 -1 Basal cell carcinoma Squamous cell carcinoma Superficial spreading melanoma (SSM) Nodular malignant melanoma (NMM) Lentigo maligna melanoma (LMM) Copyright © 2017, Elsevier Inc. All rights reserved. 57
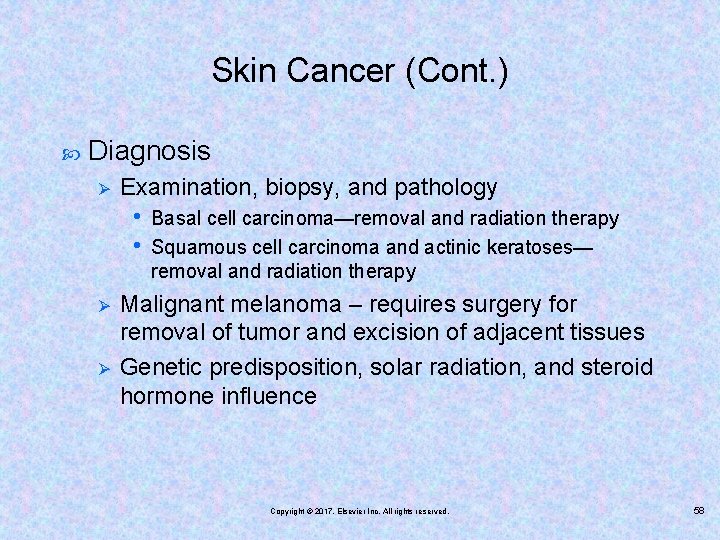
Skin Cancer (Cont. ) Diagnosis Ø Examination, biopsy, and pathology • • Ø Ø Basal cell carcinoma—removal and radiation therapy Squamous cell carcinoma and actinic keratoses— removal and radiation therapy Malignant melanoma – requires surgery for removal of tumor and excision of adjacent tissues Genetic predisposition, solar radiation, and steroid hormone influence Copyright © 2017, Elsevier Inc. All rights reserved. 58
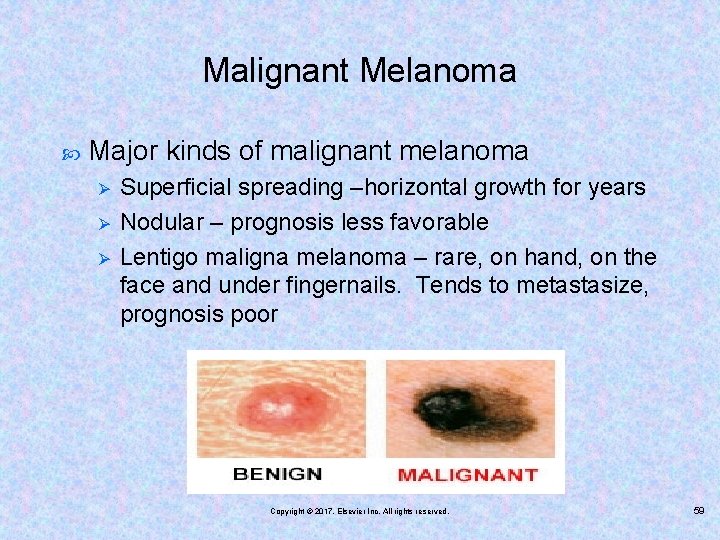
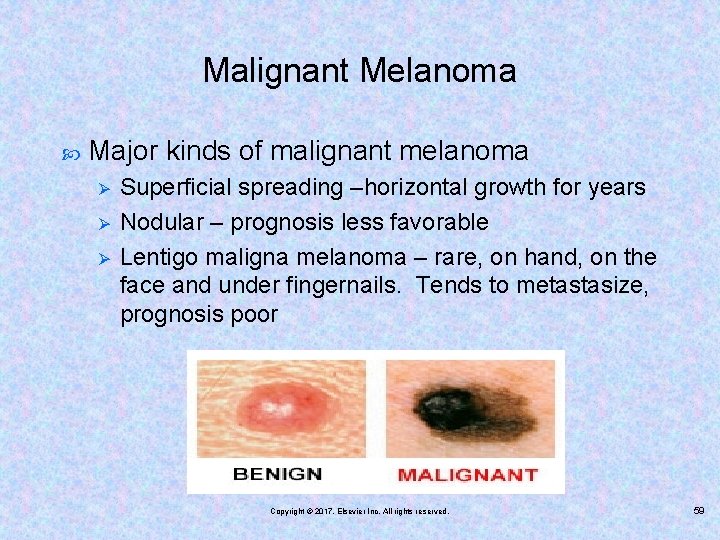
Malignant Melanoma Major kinds of malignant melanoma Ø Ø Ø Superficial spreading –horizontal growth for years Nodular – prognosis less favorable Lentigo maligna melanoma – rare, on hand, on the face and under fingernails. Tends to metastasize, prognosis poor Copyright © 2017, Elsevier Inc. All rights reserved. 59
Treatment Surgical removal of the tumor and excision of adjacent tissues and nearby lymphatic structures Chemotherapy – for migrating tumor cells Radiation therapy – not indicated for malignant melanoma unless there is extensive metastasis Early detection and removal of cancerous tissue is key Copyright © 2017, Elsevier Inc. All rights reserved. 60

Basal Cell Carcinoma Copyright © 2017, Elsevier Inc. All rights reserved. 61
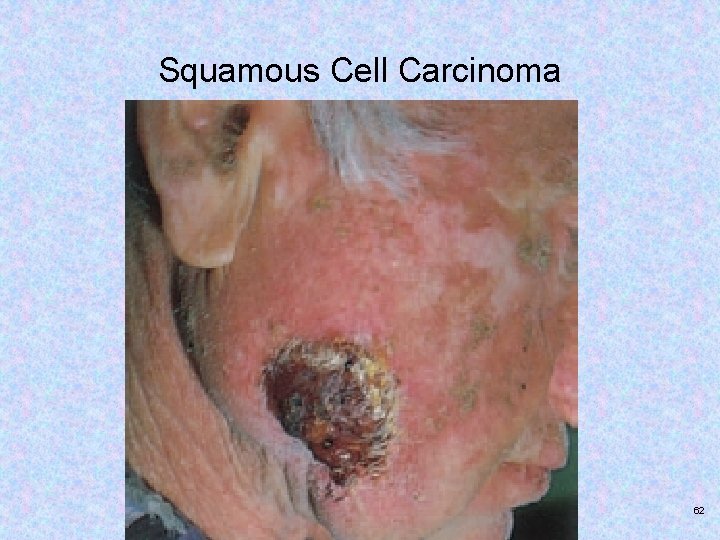
Squamous Cell Carcinoma Copyright © 2017, Elsevier Inc. All rights reserved. 62
Nursing Management Report different skin lesions and prompt medical attention Patient education and reassurance – if treated in early stages cure is successful. Those with skin cancer history should be checked at least once a year Local community resources, support groups Copyright © 2017, Elsevier Inc. All rights reserved. 63

Melanoma Copyright © 2017, Elsevier Inc. All rights reserved. 64
Malignant Melanoma Drug Therapy Interferon alfa-2 b Ipilimunab (Yervoy) Vemurafenib (Zelboraf) Boosts the immune system to help fight cancer. These treatments are made of substances produced by the body or similar substances produced in a laboratory. Side effects of these treatments are similar to those of the flu, including chills, fatigue, fever, headache and muscle aches. 65

Non-Infectious Disorders of the Skin Pressure Ulcers Risk factors Ø Confinement, immobility, incontinence, malnutrition, decreased level of consciousness or confusion, obesity, diabetes mellitus, dehydration, edema, excessive sweating, and extreme age Prevention Ø Pressure relief, positioning, padding, use of pressure relief devices, adequate nutrition, and excellent skin care Copyright © 2017, Elsevier Inc. All rights reserved. 66
Non-Infectious Disorders of the Skin Pressure Ulcers Cells die very quickly without adequate blood supply. 67
Pressure Ulcers (Cont. ) page 983 Braden scale system or the Norton system National Pressure Ulcer Advisory Panel (NPUAP) staging system for classification Ø Ø Ø Suspected deep tissue injury Stage III Unstageable Copyright © 2017, Elsevier Inc. All rights reserved. 68
Pressure ulcers 69
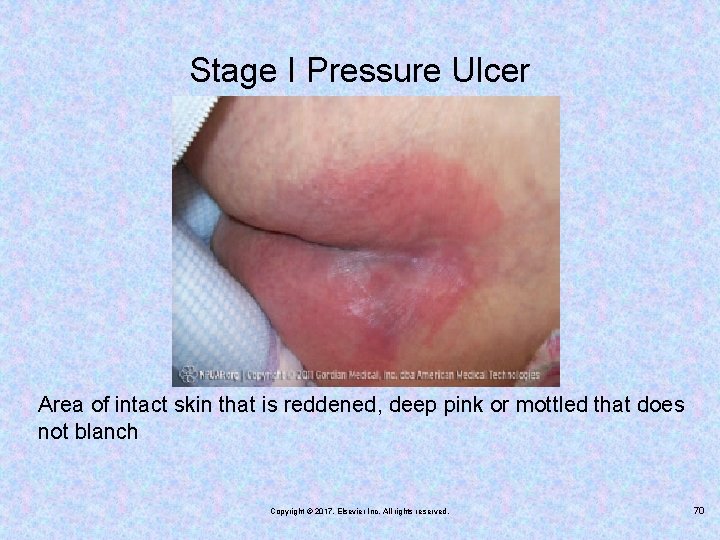
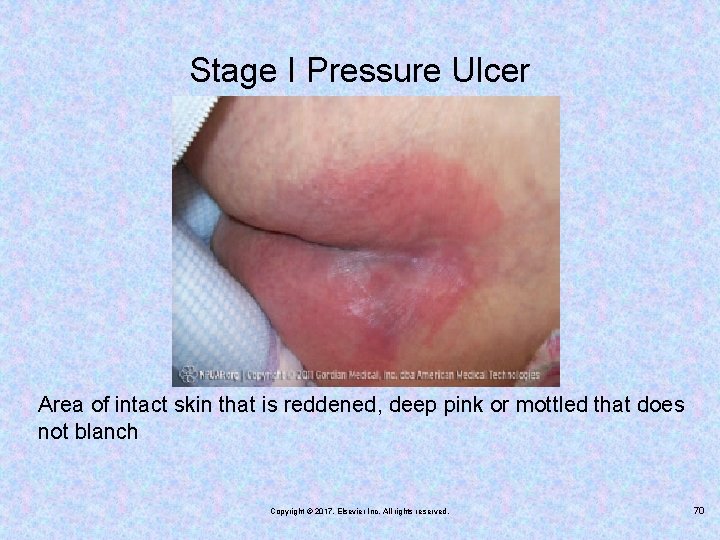
Stage I Pressure Ulcer Area of intact skin that is reddened, deep pink or mottled that does not blanch Copyright © 2017, Elsevier Inc. All rights reserved. 70
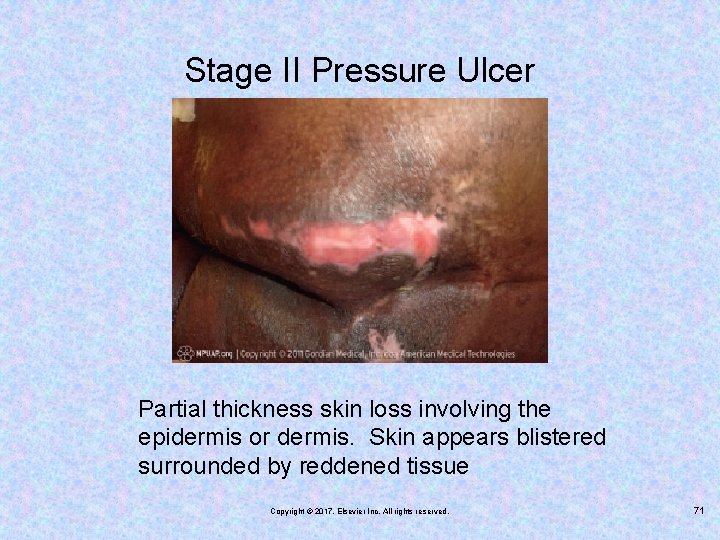
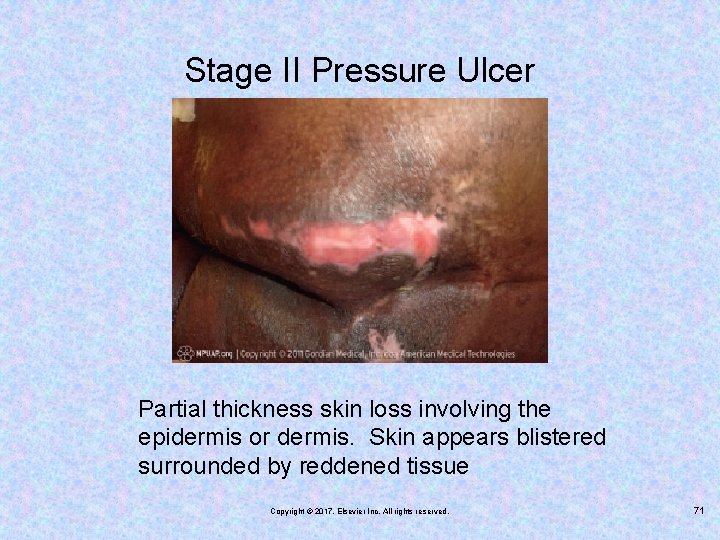
Stage II Pressure Ulcer Partial thickness skin loss involving the epidermis or dermis. Skin appears blistered surrounded by reddened tissue Copyright © 2017, Elsevier Inc. All rights reserved. 71
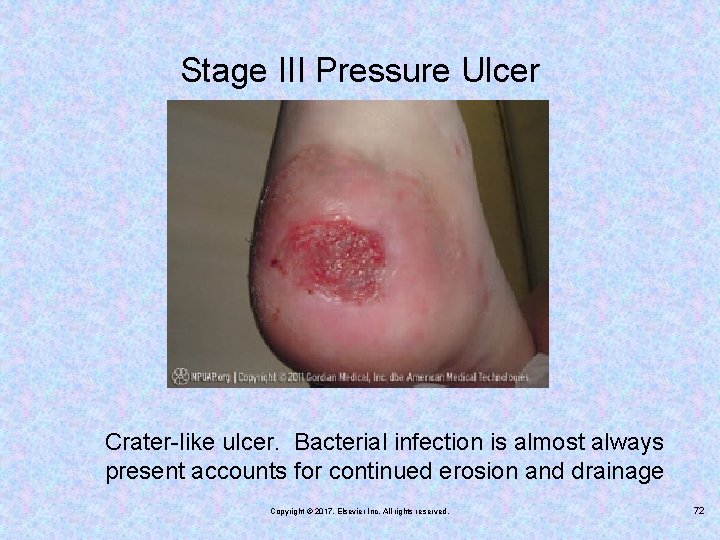
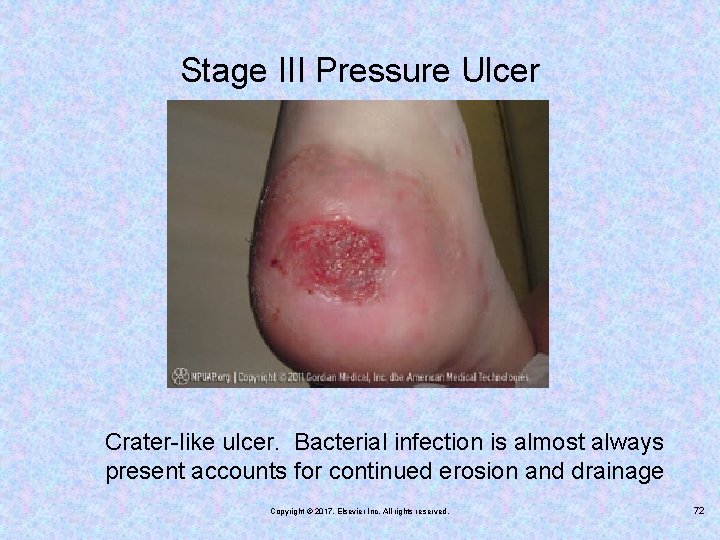
Stage III Pressure Ulcer Crater-like ulcer. Bacterial infection is almost always present accounts for continued erosion and drainage Copyright © 2017, Elsevier Inc. All rights reserved. 72
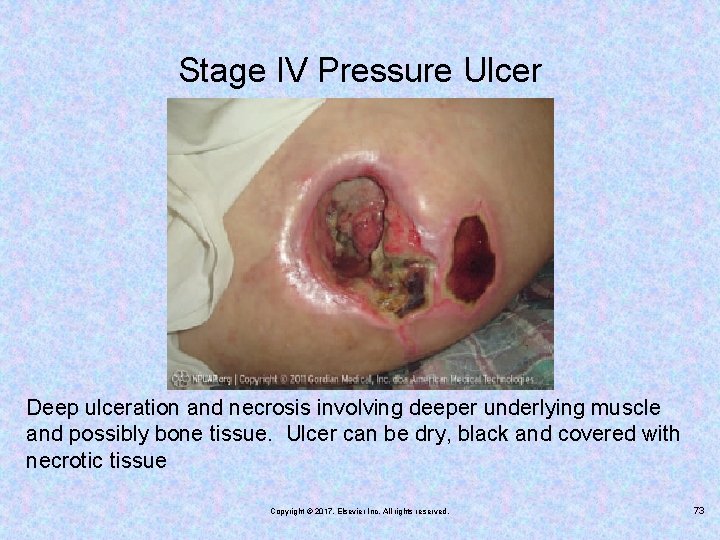
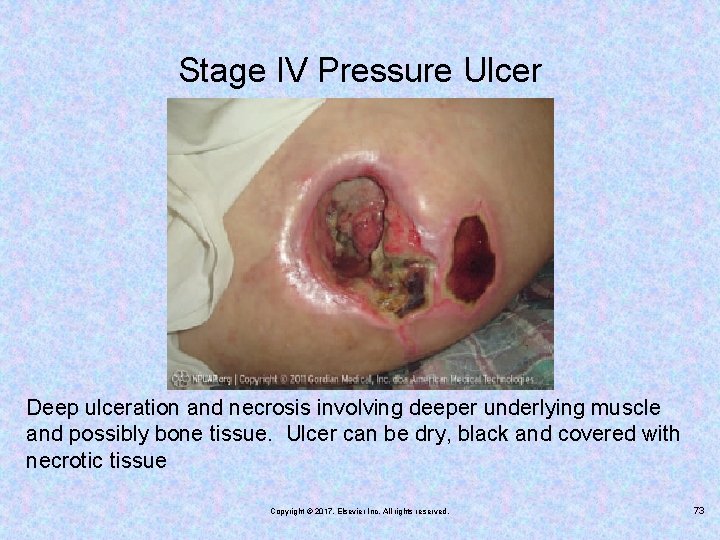
Stage IV Pressure Ulcer Deep ulceration and necrosis involving deeper underlying muscle and possibly bone tissue. Ulcer can be dry, black and covered with necrotic tissue Copyright © 2017, Elsevier Inc. All rights reserved. 73
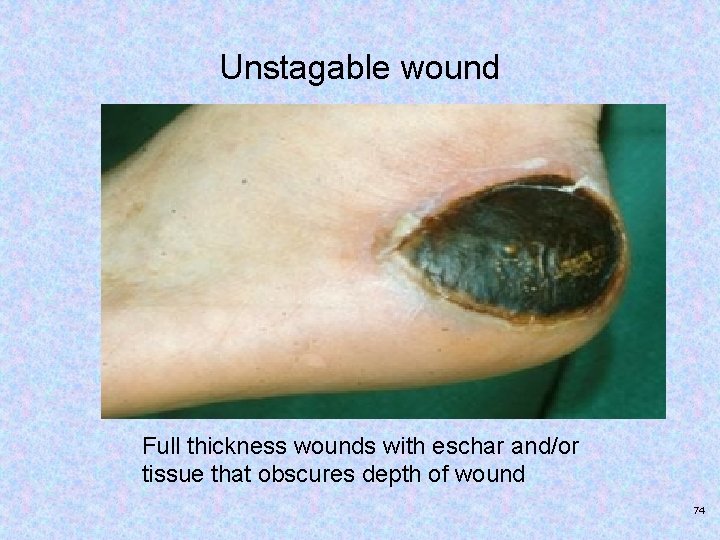
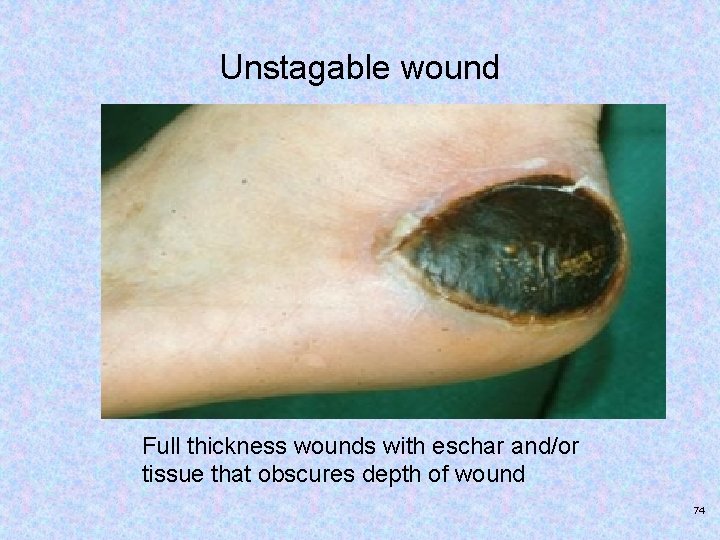
Unstagable wound Full thickness wounds with eschar and/or tissue that obscures depth of wound 74
Treatment and Nursing Interventions for Pressure Ulcers Débridement Dead tissue is removed so that the underlying tissue may heal. Surgical – forceps and scissors, mechanically - whirpool baths, wet-to-dry sale dressings and chemically with dextranomer beads sprinkled over the wound or other chemical products. Sufficient analgesia must be provided to the patient process can be painful Copyright © 2017, Elsevier Inc. All rights reserved. 75

Treatment and Nursing Interventions for Pressure Ulcers Cleansing and dressing – irrigated with normal saline to reach undermined areas and tunnels. Dressing include hydrogel, alginates, biologics, etc. Pressure must be kept off the wound for it to heal Other treatment methods – wound vac for chronic ulcers, hyperbaric oxygen therapy Documentation – measured once a week, note exudate from wound, methods of treatment noted in chart 76
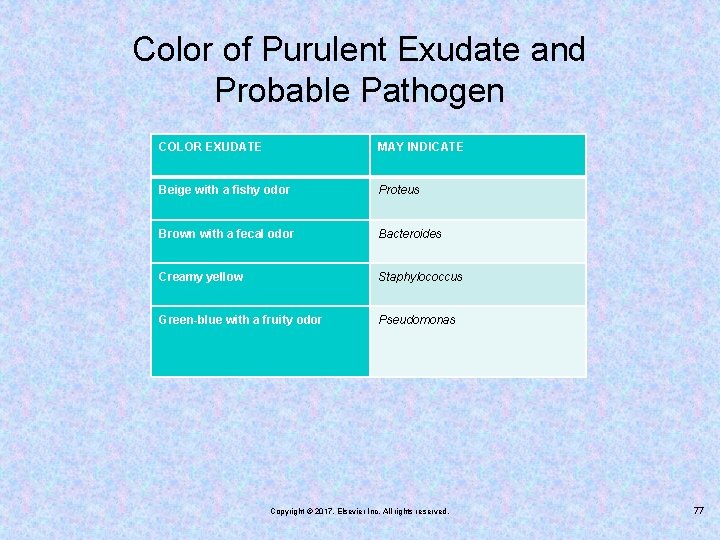
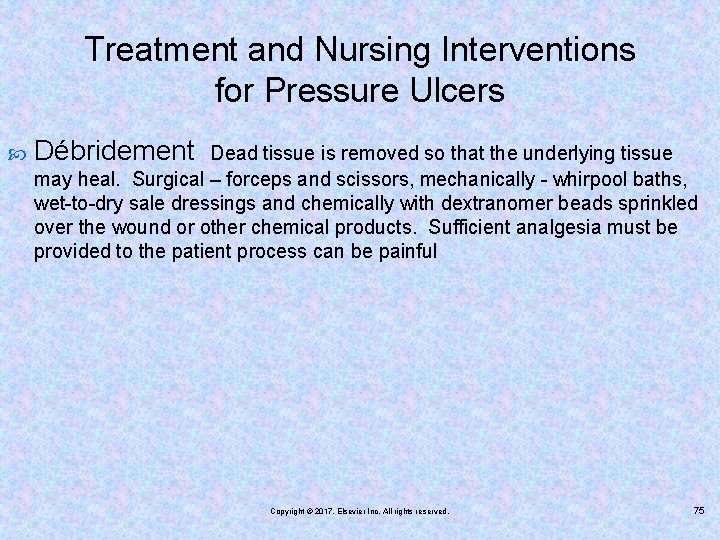
Color of Purulent Exudate and Probable Pathogen COLOR EXUDATE MAY INDICATE Beige with a fishy odor Proteus Brown with a fecal odor Bacteroides Creamy yellow Staphylococcus Green-blue with a fruity odor Pseudomonas Copyright © 2017, Elsevier Inc. All rights reserved. 77

Documentation and Pressure Ulcer Scale for Healing (PUSH) tool 78
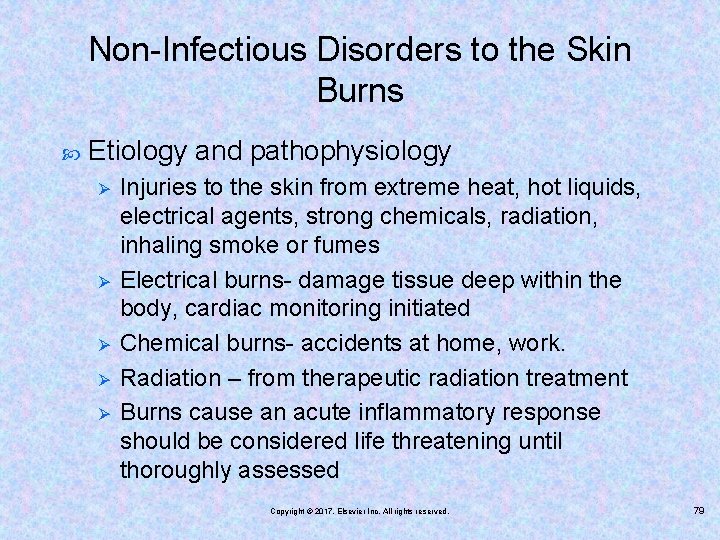
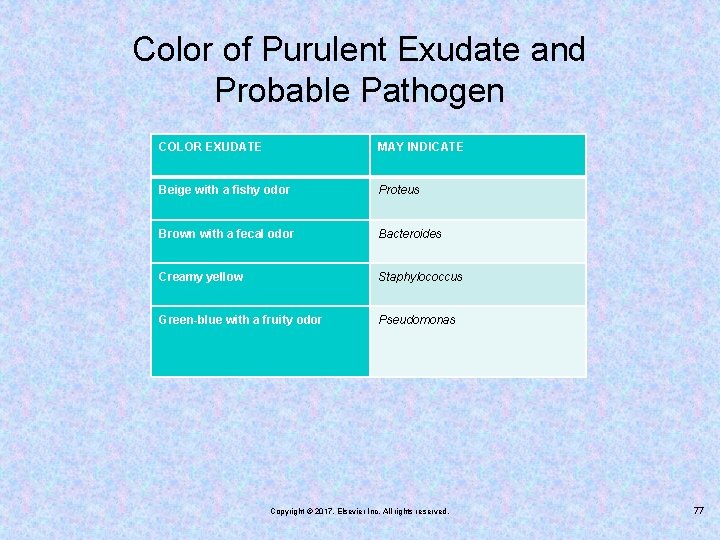
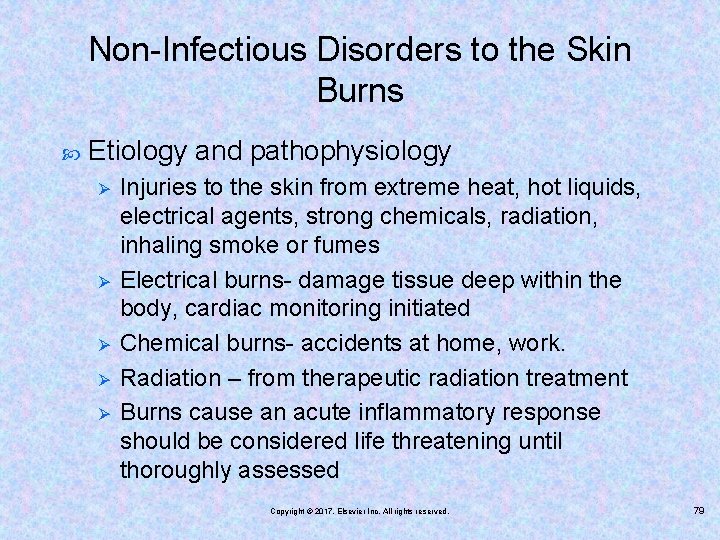
Non-Infectious Disorders to the Skin Burns Etiology and pathophysiology Ø Ø Ø Injuries to the skin from extreme heat, hot liquids, electrical agents, strong chemicals, radiation, inhaling smoke or fumes Electrical burns- damage tissue deep within the body, cardiac monitoring initiated Chemical burns- accidents at home, work. Radiation – from therapeutic radiation treatment Burns cause an acute inflammatory response should be considered life threatening until thoroughly assessed Copyright © 2017, Elsevier Inc. All rights reserved. 79

Non-Infectious Disorders to the Skin Burns Dangers Hyperkalemia- potassium is released from damaged cells Hyponatremia – potassium shifts leads to metabolic acidosis. Hypovolemia – low blood pressure and possible hypovolemic shock Increased viscosity of the blood –blood flow slows causing tissue hypoxia Curling ulcer – decreased perfusion affects gastric mucosa – this ulcer may develop within 24 hours 80
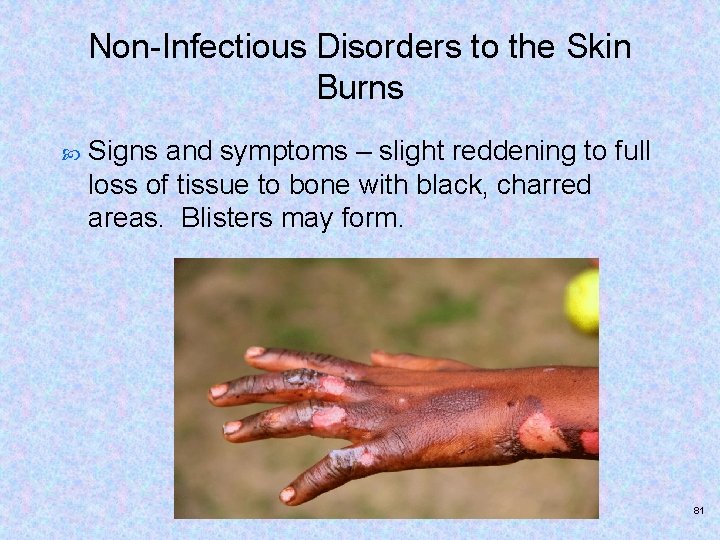
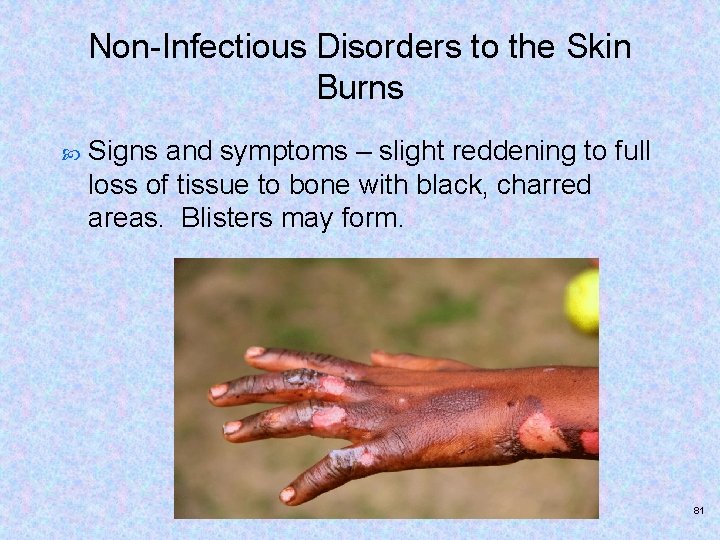
Non-Infectious Disorders to the Skin Burns Signs and symptoms – slight reddening to full loss of tissue to bone with black, charred areas. Blisters may form. 81
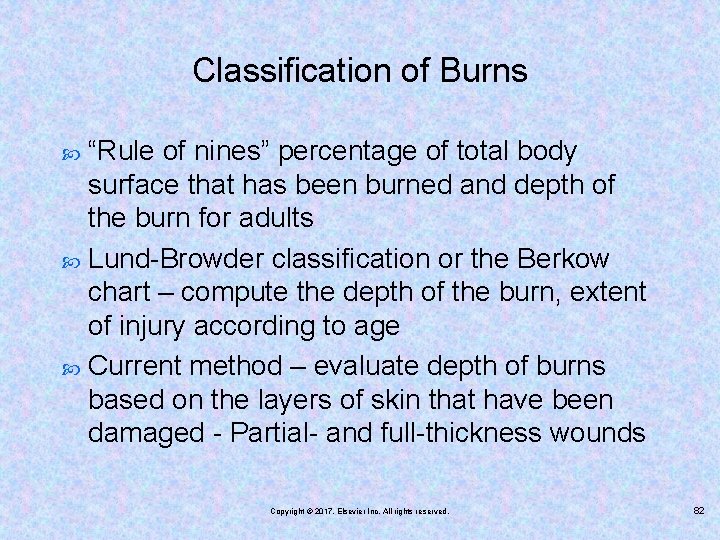
Classification of Burns “Rule of nines” percentage of total body surface that has been burned and depth of the burn for adults Lund-Browder classification or the Berkow chart – compute the depth of the burn, extent of injury according to age Current method – evaluate depth of burns based on the layers of skin that have been damaged - Partial- and full-thickness wounds Copyright © 2017, Elsevier Inc. All rights reserved. 82
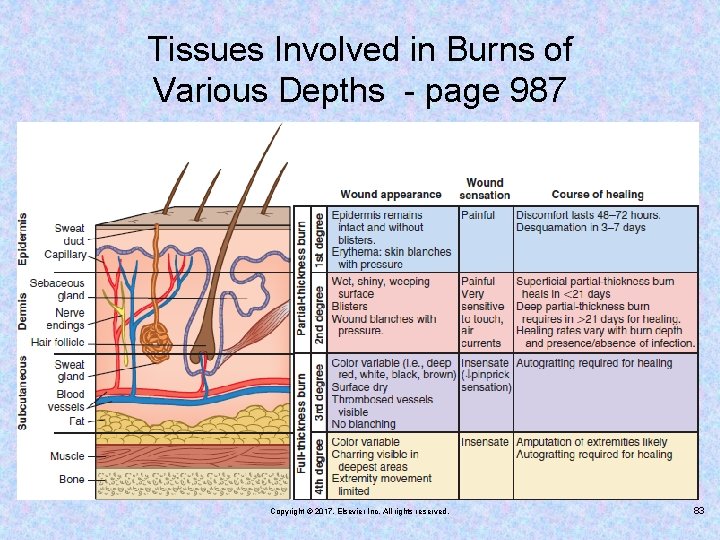
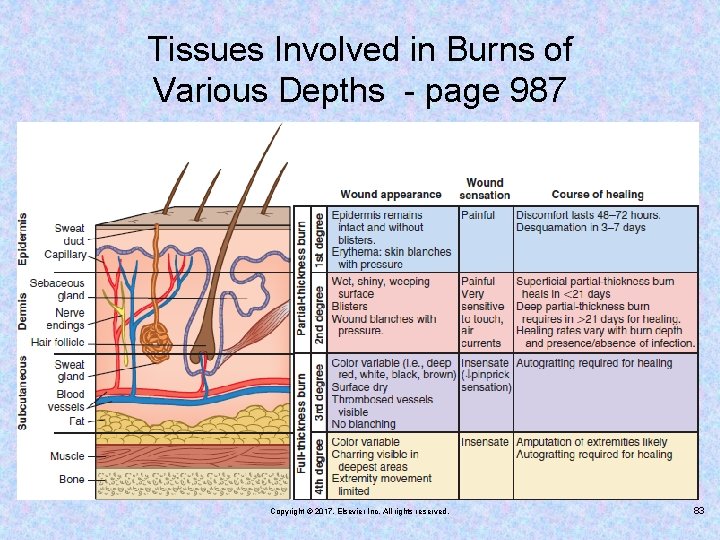
Tissues Involved in Burns of Various Depths - page 987 Copyright © 2017, Elsevier Inc. All rights reserved. 83

Partial-Thickness Burn Injury Epidermal appendages are not destroyed and wound will heal by itself. Copyright © 2017, Elsevier Inc. All rights reserved. 84
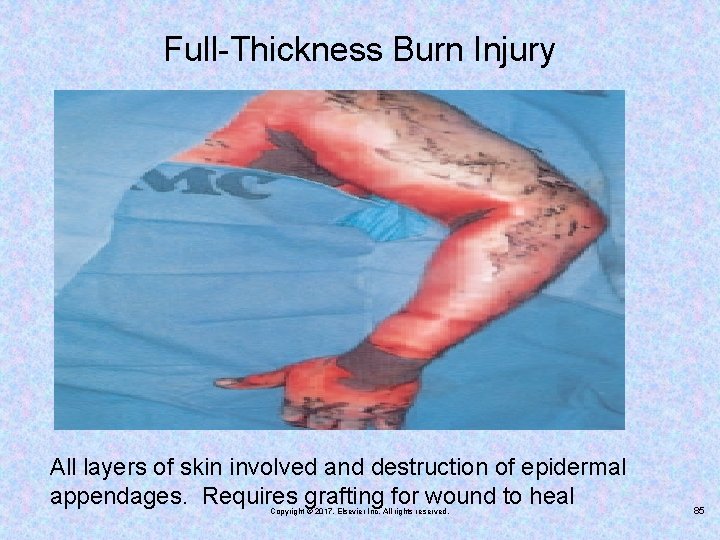
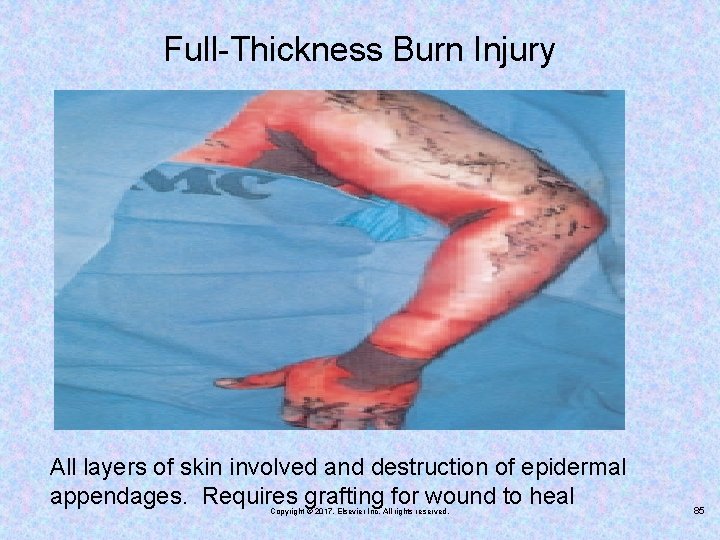
Full-Thickness Burn Injury All layers of skin involved and destruction of epidermal appendages. Requires grafting for wound to heal Copyright © 2017, Elsevier Inc. All rights reserved. 85
Classification of Burn Depth – see table 42 -3 page 968 Color Edema Pain Blisters Eschar Healing time Grafts required Copyright © 2017, Elsevier Inc. All rights reserved. 86
First Aid for Minor Burns Run cool water over the burn continuously for 10 to 15 minutes. Apply cool compresses if continuous water flow is not available. Do not apply ice, ice water, butter, or ointments. Do not pop blisters. Cover loosely with a sterile gauze bandage. Take ibuprofen or acetaminophen for pain. Copyright © 2017, Elsevier Inc. All rights reserved. 87
Emergency Treatment of Burns All burn patients are treated as trauma patients Establish and maintain airway 1 st priority Oxygen and pulse oximetry Assessment for carbon monoxide inhalation – check for mucous membranes for cherry red color Intravenous fluid therapy and more extensive medical treatment. Transfer to burn center according to guidelines Copyright © 2017, Elsevier Inc. All rights reserved. 88

Emergent Phase of Burns – 24 to 48 hours (may last 3 days) Tetanus toxoid IM injection Respiratory support – upper airways may be burned, swelling may occur. s/s respiratory distress – increased RR, use of accessory muscles, nasal flaring, restlessness and confusion. Burn patients observed for respiratory problems: burns on face/neck, dark/black sputum, burning sensation in throat or chest and hx of burned in an enclosed space. Copyright © 2017, Elsevier Inc. All rights reserved. 89

Emergent Phase of Burns – 24 to 48 hours (may last 3 days) Fluid resuscitation and prevention of shock – circulatory collapse. Replacement of lost fluids and electrolytes and enhancement of tissue perfusion. Parkland formula used see page 989. Unless fluids are replaced – cardiac output will drop and shock may be fatal. Extreme fluid deficit will cause acute renal failure. Lab data checked frequently for status of electrolytes Pain management 90
Fluid Resuscitation and Prevention of Shock 4 m. L of Ringer’s lactate % Burn Weight in kilograms Ø Ø Half of the required fluid should be given within 8 hours of the time of the burn. The second half is given over the next 16 hours. Fluids are based on specific volume and electrolyte imbalances and response to treatment. Calculated from the time of injury, not from the time of arrival at the medical facility Copyright © 2017, Elsevier Inc. All rights reserved. 91

Emergent Phase of Burns – 24 to 48 hours (may last 3 days) Pain management – IV morphine or hydromorphone hydrochloride (Dilaudid) at high levels – 2 to 4 mg every 5 to 10 minutes. Fentanyl with benzodiazepine prior to wound care procedures NSAIDs not used with grafting due to possibly of stress ulcers Gabapentin and methadone for chronic pain 92
Acute Phase of Burns Acute phase – from time that fluids mobilize and burned area is covered by grafts or healed. Management of pain and anxiety, promote nutrition and rehabilitation Prevention of infection – any signs of infection should be reported immediately, IV antibiotics specific to bacteria in the wound are given with topical ABT applied to wound. Copyright © 2017, Elsevier Inc. All rights reserved. 93

Acute Phase of Burns Wound treatment – six principles see page 990. Cleansed using sterile technique. Remove excess exudate, topical ointment like Bacitracin usually applied every 8 hours. Silver sulfadiazine used for burns, does not penetrate eschar. 94
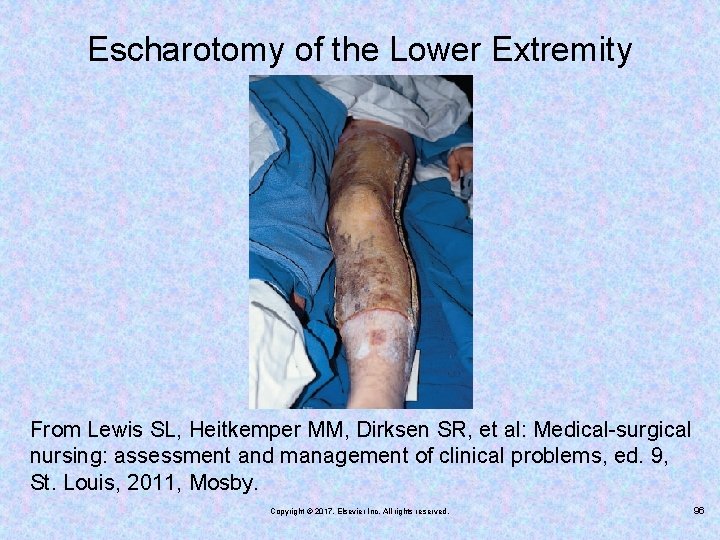
Burn Wound treatment Ø Ø Ø Escharotomy – eschar impairs healing and is a source of infection. 1 week after burn eschar is removal with skin grafting. Eschar can also constrict tissue perfusion – escharotomy performed with incision into subq tissue. Débridement – removal of eschar done in the OR Grafting Complications Rehabilitation phase 95
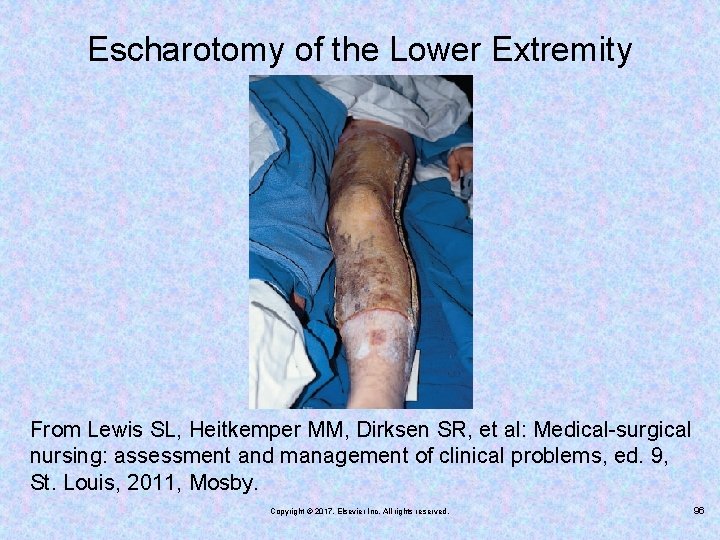
Escharotomy of the Lower Extremity From Lewis SL, Heitkemper MM, Dirksen SR, et al: Medical-surgical nursing: assessment and management of clinical problems, ed. 9, St. Louis, 2011, Mosby. Copyright © 2017, Elsevier Inc. All rights reserved. 96
Signs of Infection Strong odor Color change to dark red or brown Redness around edges extending to nonburned skin Texture change Exudate and purulent drainage Sloughing of graft Copyright © 2017, Elsevier Inc. All rights reserved. 97

Nursing Care of Burns Manage pain. Prevent infection. Manage itch. Nutritional support Psychosocial support Patient-family education Community care Copyright © 2017, Elsevier Inc. All rights reserved. 98