Longitudinal Study of NC EHDI Program A joint













- Slides: 35
Longitudinal Study of NC EHDI Program A joint study by the Office of Education Services of the NC Dept. of Health and Human Services And BEGINNINGS For Parents of Children Who Are Deaf or Hard of Hearing, Inc. Presented by Joni Alberg, Ph. D. and Christene Tashjian, MPA BEGINNINGS--Raleigh, NC
Faculty Disclosure Information In the past 12 months, we have not had a significant financial interest or other relationship with the manufacturer(s), the product(s) or provider(s) of the service(s) that will be discussed in our presentation. This presentation will not include discussion of pharmaceuticals or devices that have not been approved by the FDA, nor will we discuss any unapproved or “off – label” uses of pharmaceuticals or devices.

Study Design Team Joni Alberg, Ph. D. --Executive Director—BEGINNINGS Cyndie Bennett, MA—Superintendent—Office of Education Services, NC Dept. of Health & Human Services Jack Roush, Ph. D. , CCC/A, Chair--Director--Division of Speech and Hearing Sciences, UNC-CH School of Medicine Member, Joint Committee on Infant Hearing Christene Tashjian, MPA—Assistant Executive Director of Research & Development, BEGINNINGS Kathryn Wilson, MA, CCC-SLP, Cert-AVT—Director—Resource Support Program, Office of Education Services, NC Dept. of Health & Human Services
Goals of the NC EHDI Program v All infants are screened for hearing loss prior to discharge from birthing/neonatal facilities, or within one month of birth.
v. All infants referred from the screening process complete diagnostic audiological evaluation by three months of age. v. All infants with diagnosed hearing loss receive appropriate interventions by six months of age, including amplification selection (if appropriate) and early intervention.
Early Intervention Program for Children Who Are Deaf or Hard of Hearing Provide comprehensive, developmental and educational services to children who are deaf, hard of hearing, or deaf/blind, ages birth to 3, and their families with a concentration on language and communication skill development.
Purpose of the Study Ø Examine efforts to achieve 1 -3 -6 goals for newborn hearing screening/diagnosis/intervention. ØExamine language outcomes of children transitioning from EI to Preschool. Ø Follow the language development progress of children who have exited EI.
Questions We Set Out to Answer 1. Are we meeting our goals for newborn screening and diagnosis? 2. Are we achieving desired goals for language and communication development in children enrolled in EI? 3. Do children continue to make gains in preschool so that they are “on par” with hearing peers when they enter Kindergarten?
Study Design • • Longitudinal Statewide in scope Representative Pilot Phase

Study Subjects • • • BEGINNINGS’ database Received EI services Born since newborn screening implemented Turning three years old during Pilot Phase Parents agree to participate

BEGINNINGS For Parents of Children Who Are Deaf or Hard of Hearing, Inc. Location of Longitudinal Study Children As of December 2005 ORANGE YADKIN FORSYTHGUILFORD NVI LLE VANC E DURHA M GRA WILKES ALAMANCE A BERTIE MD 2 EN 1 CK UG CA CA ITU IT M AV STOKES ROCKINGHAM NORTHGATE WARREN AMPTON HERT- S FORD HALIFAX RR TA SURRY L EL SW PERSON CHOW WA ALLEGHANY CU ASHE COUNTIES 1 PASQUOTANK 2 PERQUIMANS ER LL RE TY L EL CH Y AN FRANKLIN CALDWELL ALEXNASH EDGEDAVIE WASHCOMBE ANDER MADISON DAVIDINGTON MARTIN IREDELL WAKE BURKE SON RANDOLPH WILSON CHATHAM HAYBUN- Mc. DOWELL CATAWBA PITT ROWAN WOOD COMBE BEAUFORT HYDE JOHNSTON RUTHERLINCOL GREENE LEE R E CABARRUS D FORD N WAYNE N GASTON HARNETT MONTAN IAHE LENOIR STANLY MOORE TR VAN SON POLK GOMERY CRAVEN L PAMLIC SY O CUMBER- SAMPSON JONES RICHHOKE DUPLIN LAND UNION ANSON MOND SCOT CARTERET ONSLOW LANDROBESON BLADEN PENDER YA CE NY SWAIN LEN CK ME URG B A EL EV CL ND CHEROKEE MACON CLAY N SO CK JA GRAHAM COLUMBUS BRUNSWICK As of of 12/31/05 As 12/31/03 NEW HANOVE R DARE

Methodology • Design Team developed data collection forms • BEGINNINGS created parent release forms, FAQs, abstract; translated into Spanish • BEGINNINGS’ staff, EI staff, CHAC were trained to use the forms
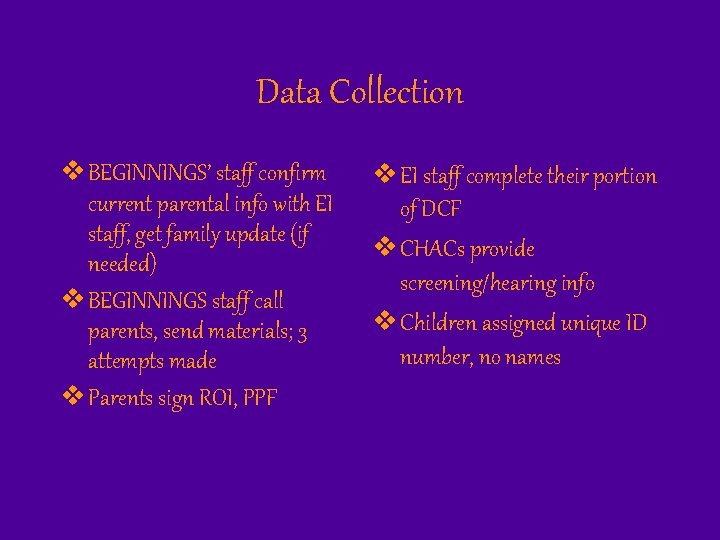
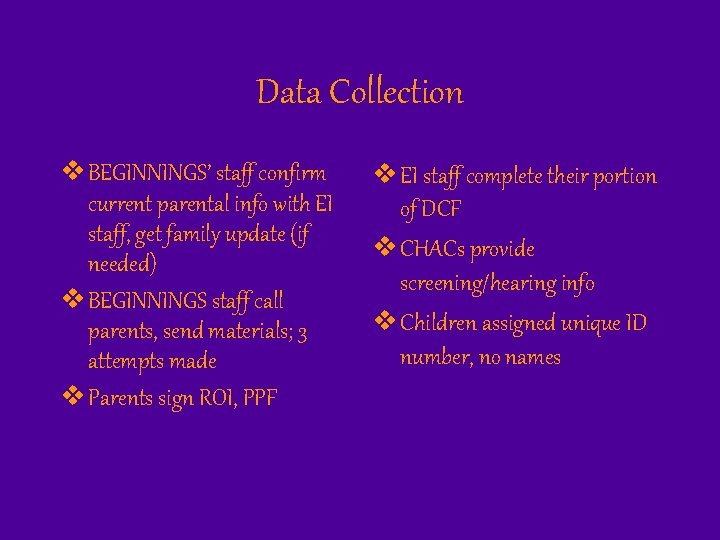
Data Collection v BEGINNINGS’ staff confirm current parental info with EI staff, get family update (if needed) v BEGINNINGS staff call parents, send materials; 3 attempts made v Parents sign ROI, PPF v EI staff complete their portion of DCF v CHACs provide screening/hearing info v Children assigned unique ID number, no names
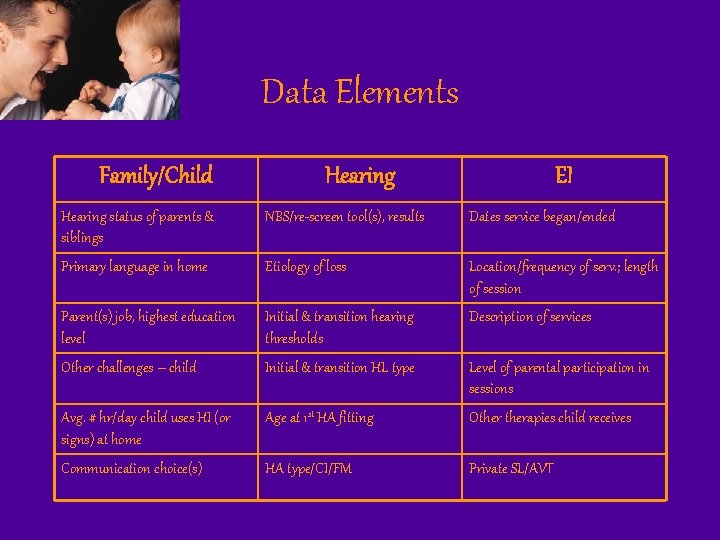
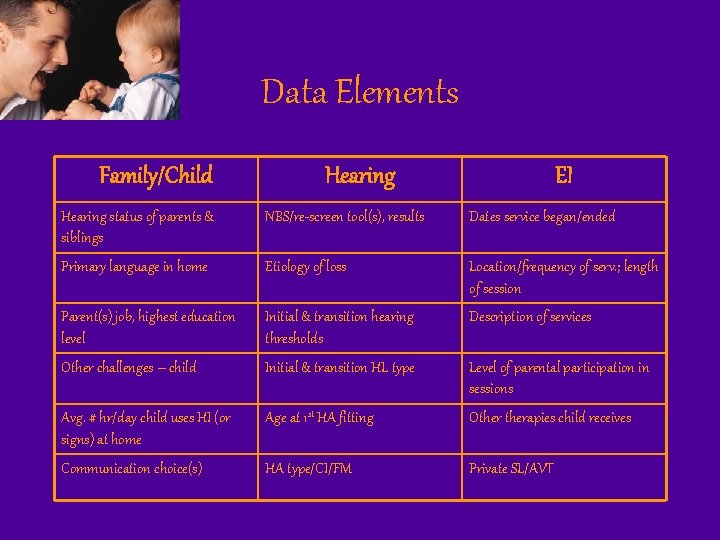
Data Elements Family/Child Hearing EI Hearing status of parents & siblings NBS/re-screen tool(s), results Dates service began/ended Primary language in home Etiology of loss Location/frequency of serv. ; length of session Parent(s) job, highest education level Initial & transition hearing thresholds Description of services Other challenges – child Initial & transition HL type Level of parental participation in sessions Avg. # hr/day child uses HI (or signs) at home Age at 1 st HA fitting Otherapies child receives Communication choice(s) HA type/CI/FM Private SL/AVT

EI File Review v EI transition language assessment scores v Rosetti, DOCs, PLS-4 v Subset of 30 -40 children to be given PLS-4 by EI SLPs
PLS - 4 v To be administered to all subjects at ages 4, 5, 6 v Test results compared with previous year(s) to assess progress v Share results with parents & preschool

Preliminary Findings 45 subjects Located in 29/100 counties Gender 27 female 18 male Other Challenges 20 None 3 Unknown 8 One Challenge 3 Two Challenges 10 Three or More Challenges
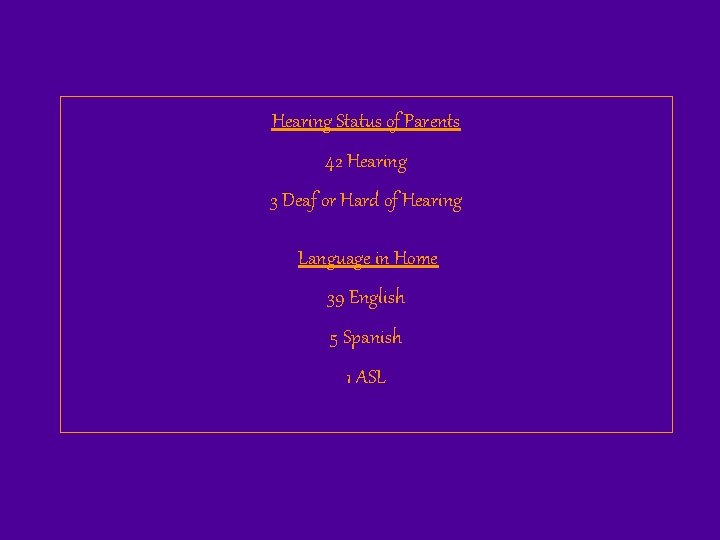
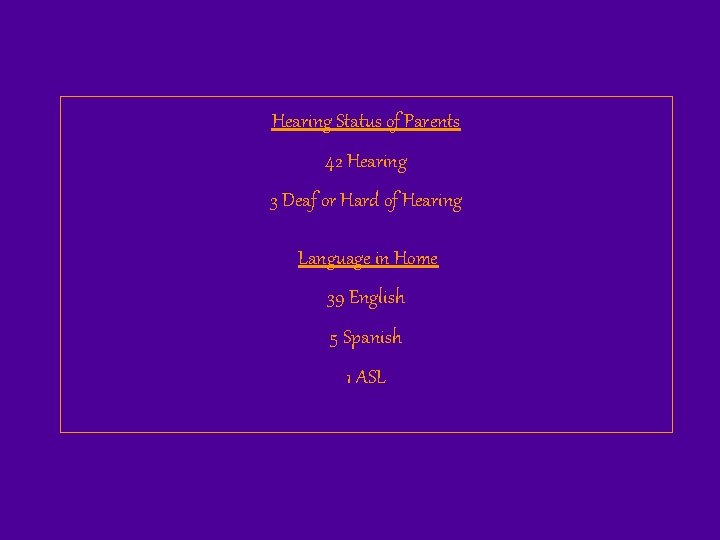
Hearing Status of Parents 42 Hearing 3 Deaf or Hard of Hearing Language in Home 39 English 5 Spanish 1 ASL
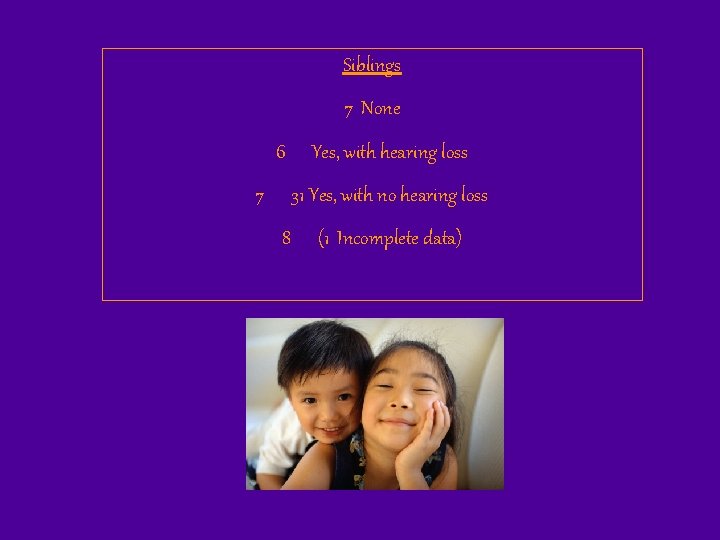
Siblings 7 None 6 7 Yes, with hearing loss 31 Yes, with no hearing loss 8 (1 Incomplete data)

Other Therapies 23 None 22 One or more 9 One only 5 Two therapies 4 Three therapies 2 Four therapies 3 1 Six therapies 4 1 Seven therapies

Screening Tools Location Results AABR 18 NICU 11 Refer-both 21 OAE 4 WBN 17 Pass-both 3 2 – Step 4 Other/Unknown 3 Refer-one 5 Unknown 5 Direct Refer 2
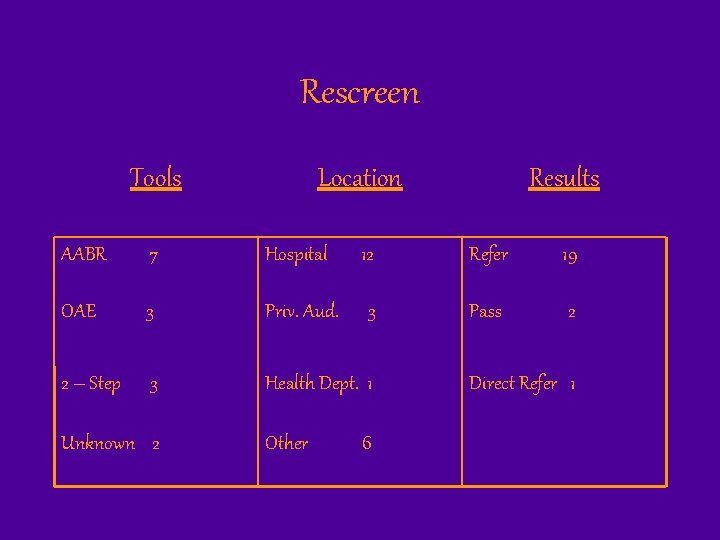
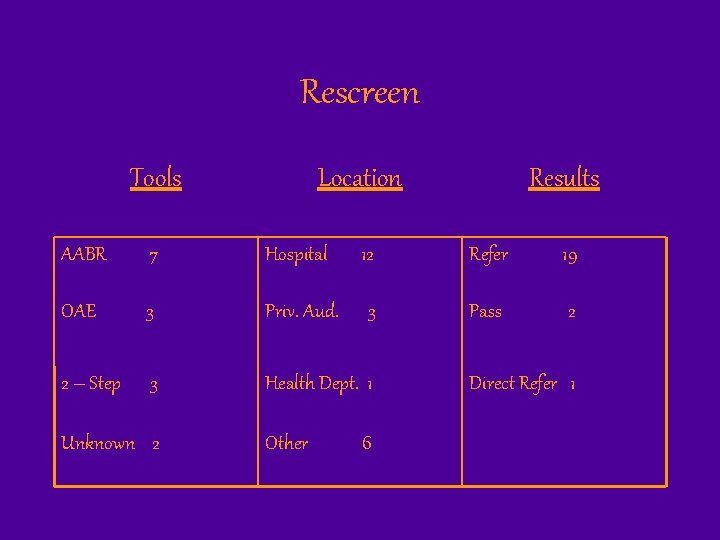
Rescreen Tools Location Results AABR 7 Hospital 12 Refer 19 OAE 3 Priv. Aud. 3 Pass 2 2 – Step 3 Health Dept. 1 Unknown 2 Other 6 Direct Refer 1
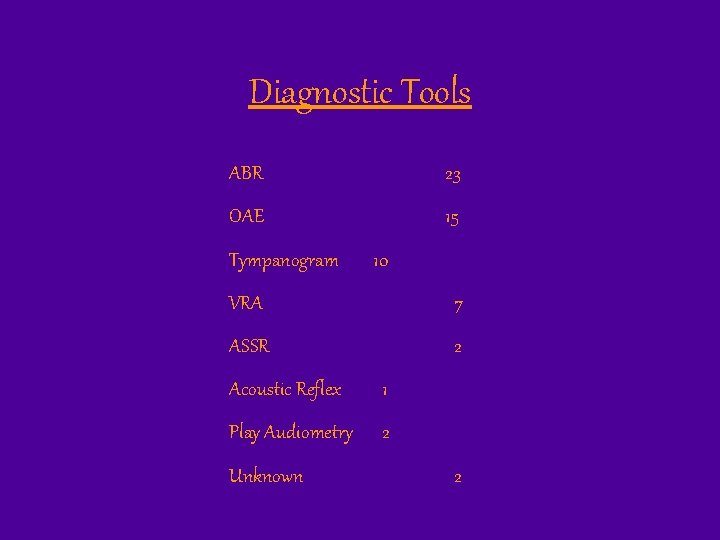
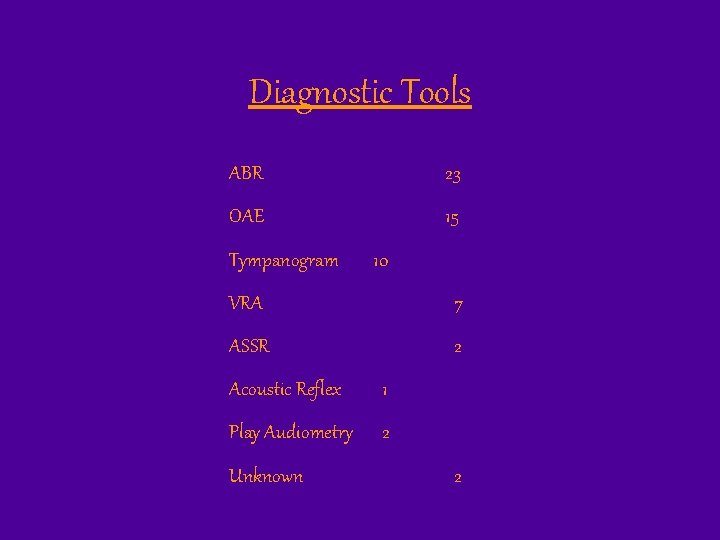
Diagnostic Tools ABR 23 OAE 15 Tympanogram 10 VRA 7 ASSR 2 Acoustic Reflex 1 Play Audiometry 2 Unknown 2

Type of Hearing Loss At Diagnosis Bilateral 27 Unilateral 3 Unknown 3 Right Ear Sensorineural 20 Conductive AN/AD Left Ear 3 4 Sensorineural 21 Conductive AN/AD 3 4 None 1 None 0 Unknown 5

Type of Hearing Loss At Transition Bilateral 23 Unilateral 2 Unknown 8 Right Ear Sensorineural Left Ear 16 Sensorineural 17 Conductive 4 Conductive 3 Mixed 1 AN/AD Unknown 3 AN/AD 9 Unknown 3 9
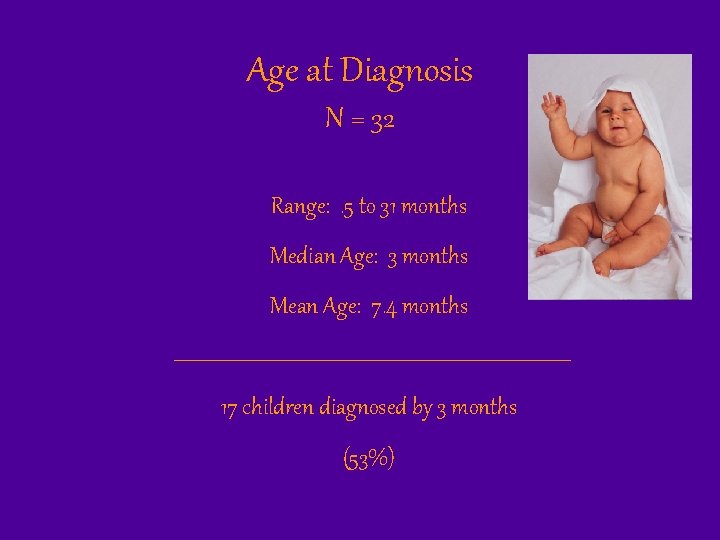
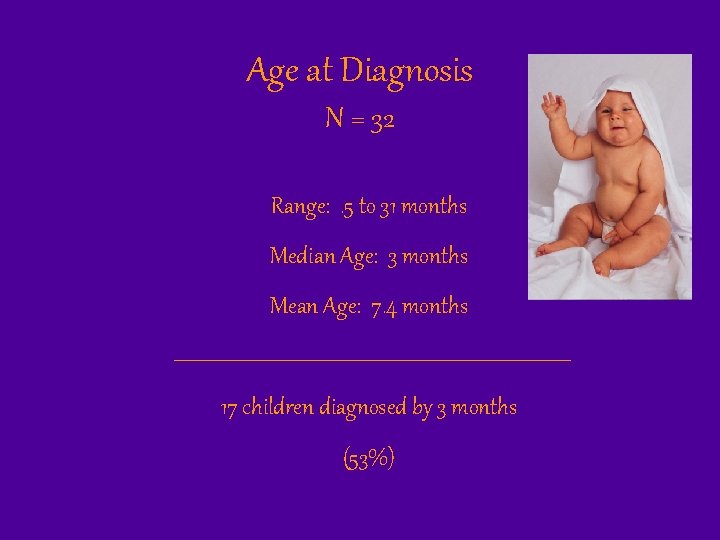
Age at Diagnosis N = 32 Range: . 5 to 31 months Median Age: 3 months Mean Age: 7. 4 months 17 children diagnosed by 3 months (53%)

Age at EI Initiation (N=45) Range: 2 to 34 months Median: 11 months Mean: 12. 6 months 14 children (31%) were enrolled in EI by 6 months
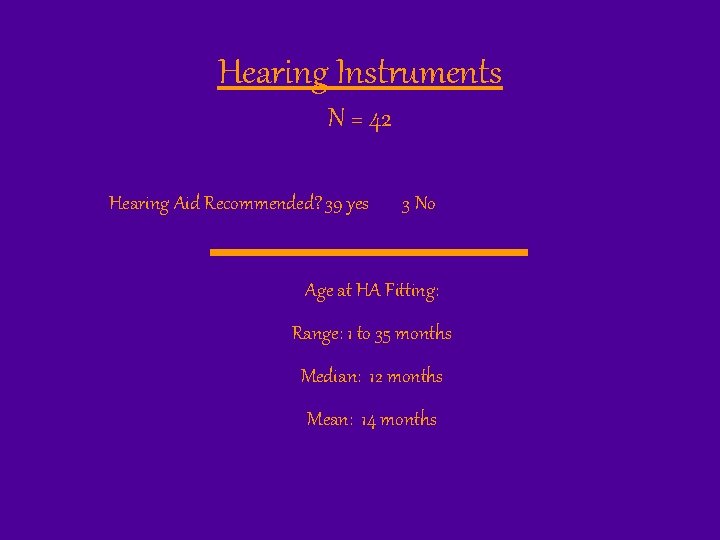
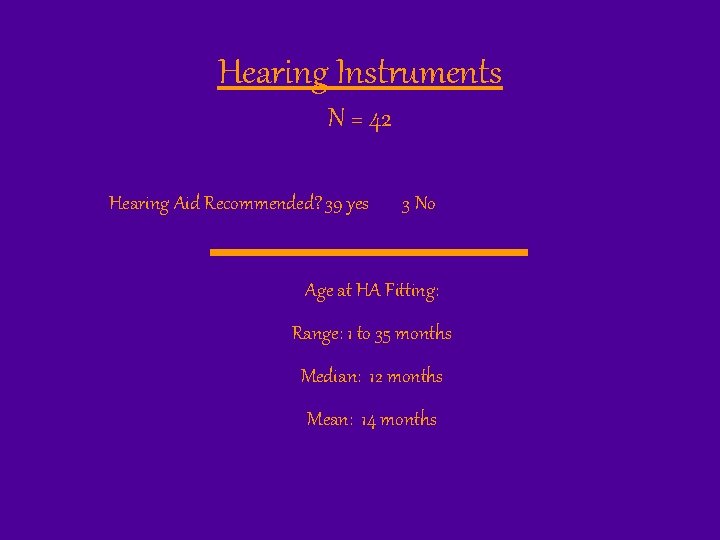
Hearing Instruments N = 42 Hearing Aid Recommended? 39 yes 3 No Age at HA Fitting: Range: 1 to 35 months Median: 12 months Mean: 14 months
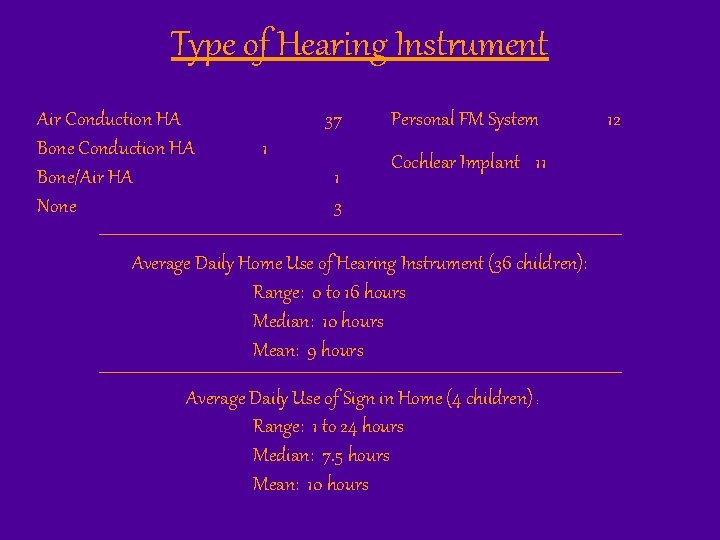
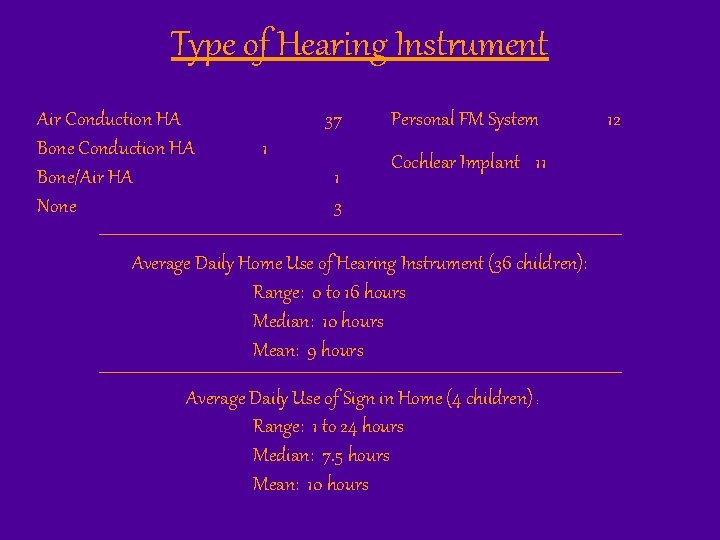
Type of Hearing Instrument Air Conduction HA Bone/Air HA None 37 1 1 3 Personal FM System Cochlear Implant 11 Average Daily Home Use of Hearing Instrument (36 children): Range: 0 to 16 hours Median: 10 hours Mean: 9 hours Average Daily Use of Sign in Home (4 children) : Range: 1 to 24 hours Median: 7. 5 hours Mean: 10 hours 12
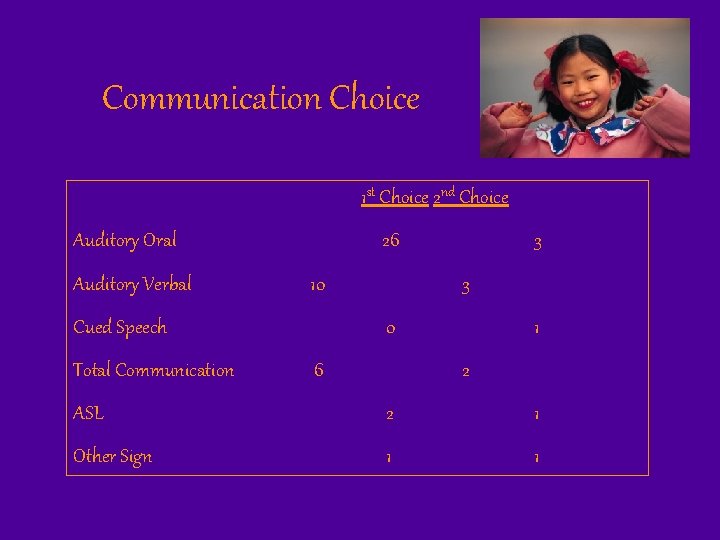
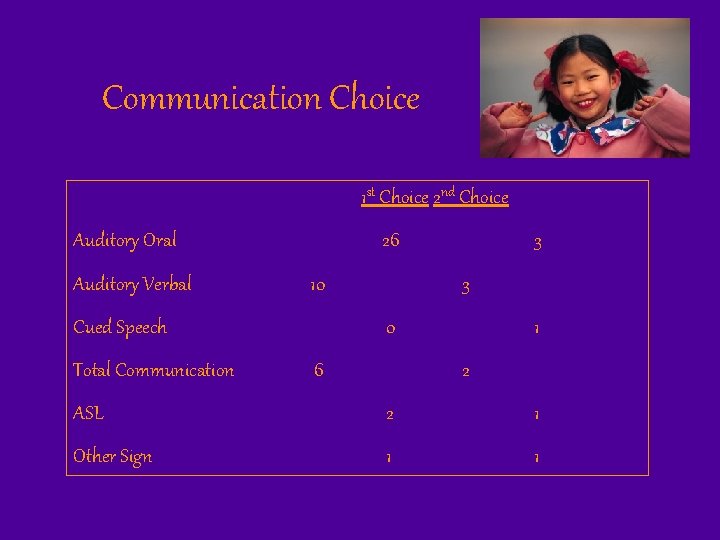
Communication Choice 1 st Choice 2 nd Choice Auditory Oral Auditory Verbal 26 10 Cued Speech Total Communication 3 3 0 6 1 2 ASL 2 1 Other Sign 1 1
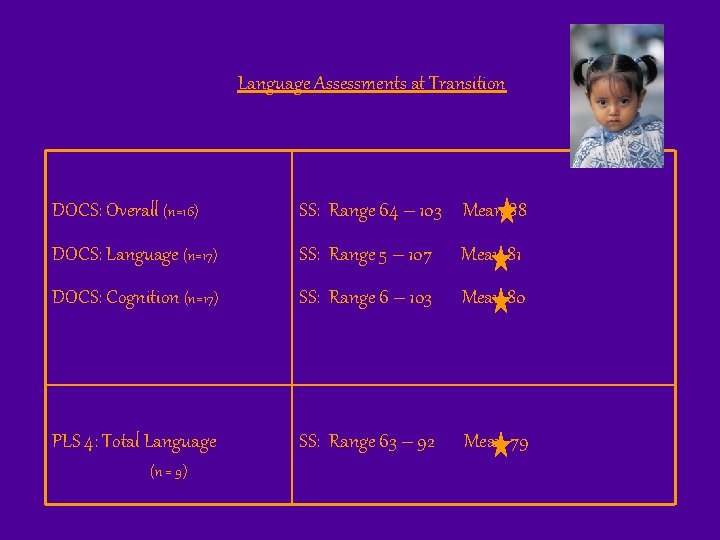
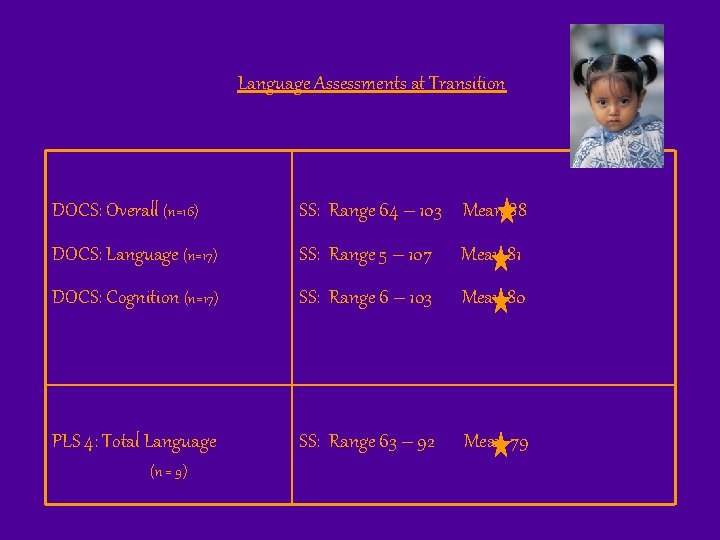
Language Assessments at Transition DOCS: Overall (n=16) SS: Range 64 – 103 Mean 88 DOCS: Language (n=17) SS: Range 5 – 107 Mean 81 DOCS: Cognition (n=17) SS: Range 6 – 103 Mean 80 PLS 4: Total Language SS: Range 63 – 92 Mean 79 (n = 9)
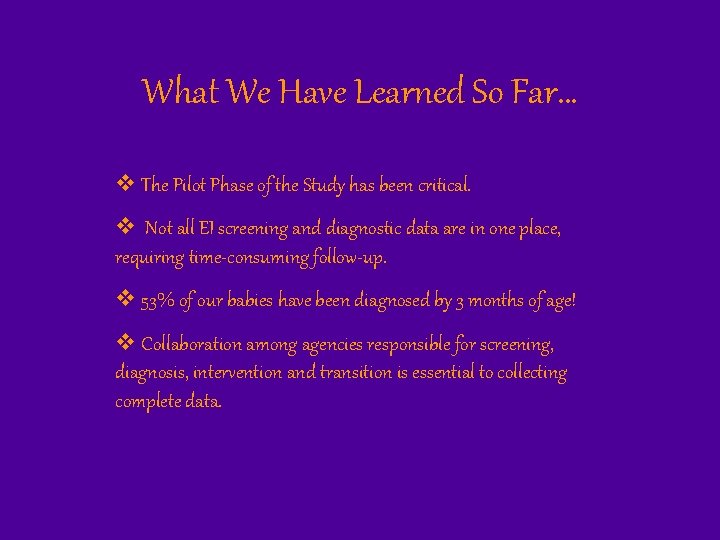
What We Have Learned So Far… v The Pilot Phase of the Study has been critical. v Not all EI screening and diagnostic data are in one place, requiring time-consuming follow-up. v 53% of our babies have been diagnosed by 3 months of age! v Collaboration among agencies responsible for screening, diagnosis, intervention and transition is essential to collecting complete data.
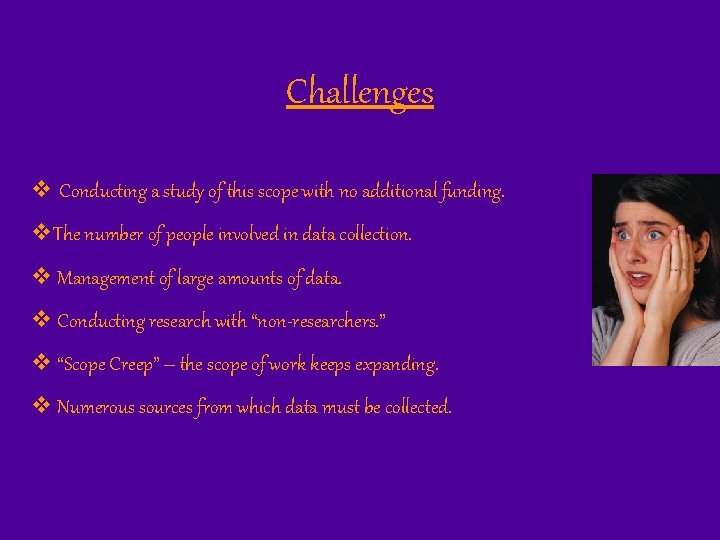
Challenges v Conducting a study of this scope with no additional funding. v. The number of people involved in data collection. v Management of large amounts of data. v Conducting research with “non-researchers. ” v “Scope Creep” – the scope of work keeps expanding. v Numerous sources from which data must be collected.

Next Steps… v Continue Pilot Study until we have 100 children. v Seek additional funding. v Begin testing 4 year olds using the PLS-4.

Thank you!!