Linking Sexual Reproductive Health and HIV PMTCT Simple
- Slides: 13
Linking Sexual & Reproductive Health and HIV PMTCT: Simple and Complex ICW, Baylor, IPPF New members IATT - 2007 Satellite Session, International AIDS Conference, Mexico City, 5 August 2008 Lynn Collins, Technical Advisor, UNFPA 1
Comprehensive PMTCT 1) Primary prevention of HIV among women of childbearing age 2) Preventing unintended pregnancies among women living with HIV 3) Preventing HIV transmission from a woman living with HIV to her infant 4) Providing treatment, care and support to mothers living with HIV, their children and families 2
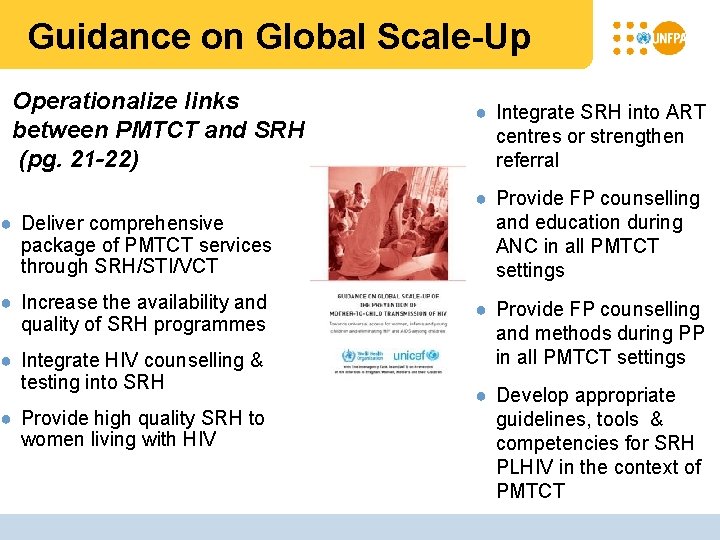
Guidance on Global Scale-Up Operationalize links between PMTCT and SRH (pg. 21 -22) ● Deliver comprehensive package of PMTCT services through SRH/STI/VCT ● Increase the availability and quality of SRH programmes ● Integrate HIV counselling & testing into SRH ● Provide high quality SRH to women living with HIV ● Integrate SRH into ART centres or strengthen referral ● Provide FP counselling and education during ANC in all PMTCT settings ● Provide FP counselling and methods during PP in all PMTCT settings ● Develop appropriate guidelines, tools & competencies for SRH PLHIV in the context of PMTCT
Primary prevention of HIV among women of childbearing age – Simple! • Increase awareness of PMTCT & pregnancy/BF as time of risk/vulnerability • STI management (e. g. ANC syphilis) • Safer sex counselling • Condoms with negotiation skills • Treatment of anemia • Viral load/ ‘+ prevention’ • Engagement of men (MNC/FP) • Empowerment of women • Blood safety/universal precautions 4
Primary prevention of HIV among women of childbearing age – Complex! • Delineating the scope/accountability • Weak couples involvement • Insufficient post-test counselling • Low risk/vulnerability perception • Difficulties with behaviour change • PP/ANC/FP not advocating dual protection from condoms • Failure to do ‘positive prevention’ • Gender inequality, GBV stigma and discrimination 5
Preventing unintended pregnancies among women living with HIV – Simple! • Awareness of rights • Counselling (rights, fertility intentions, preventing vertical transmission, etc. ) • Provision of contraceptives (if desired) • Infertility services 6
Preventing unintended pregnancies among women living with HIV – Complex! If it is not measured it doesn’t happen! • Acceptance of FP indicator in PMCT • Linking FP with other services (e. g. ANC, PP, ARV delivery, VCT, etc. ) • Health providers’/others’ attitudes and knowledge of rights and SRH of PLHIV • Package of rights-based FP for PLHIV not widely available 7
Providing treatment, care and support to mothers living with HIV, their children and families – Joint Responsibility! Rights and sexual and reproductive health (SRH) of people living with HIV is a joint responsibility of SRH and HIV programmes • ‘Verticalization’ has created lack of accountability to support the rights and address the SRH/HIV concerns of PLHIV • Multiple entry points but poorly linked • Experience with bi-directional linkages exists 8
Key Messages ● HIV prevention is doable in the context of current PMTCT programmes but not given sufficient priority ● Supporting a rights-based family planning indicator in the context of PMTCT will increase recognition of its importance in PMTCT ● The rights and sexual and reproductive health of people living with HIV is a backbone of PMTCT and must be the joint coordinated responsibility of HIV and SRH programmes, including linking family planning with other services
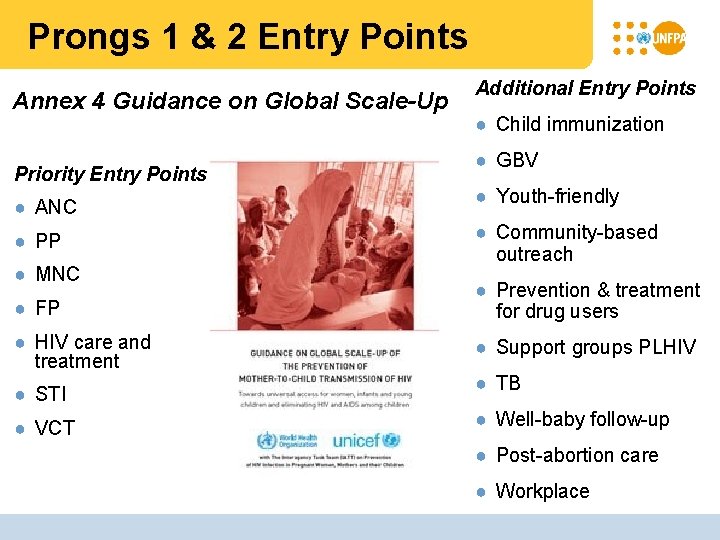
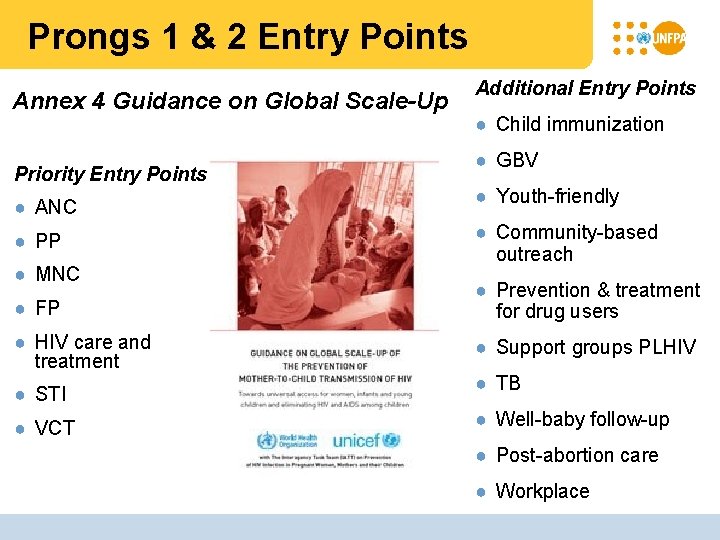
Prongs 1 & 2 Entry Points Annex 4 Guidance on Global Scale-Up Priority Entry Points ● ANC ● PP ● MNC Additional Entry Points ● Child immunization ● GBV ● Youth-friendly ● Community-based outreach ● FP ● Prevention & treatment for drug users ● HIV care and treatment ● Support groups PLHIV ● STI ● VCT ● TB ● Well-baby follow-up ● Post-abortion care ● Workplace
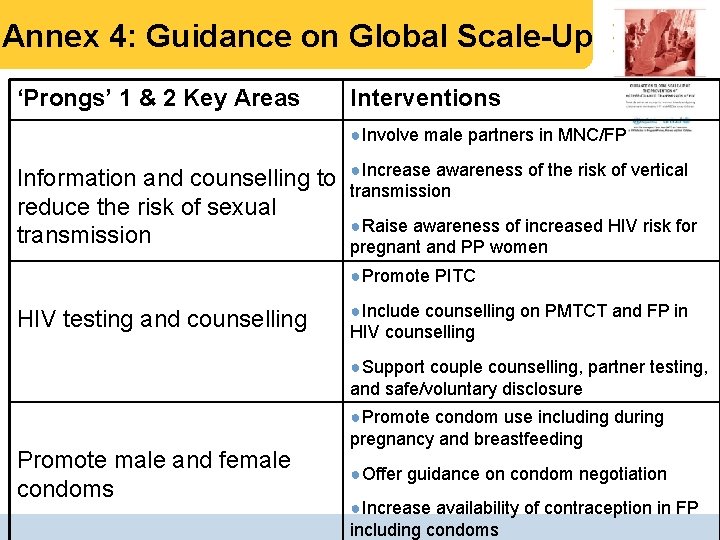
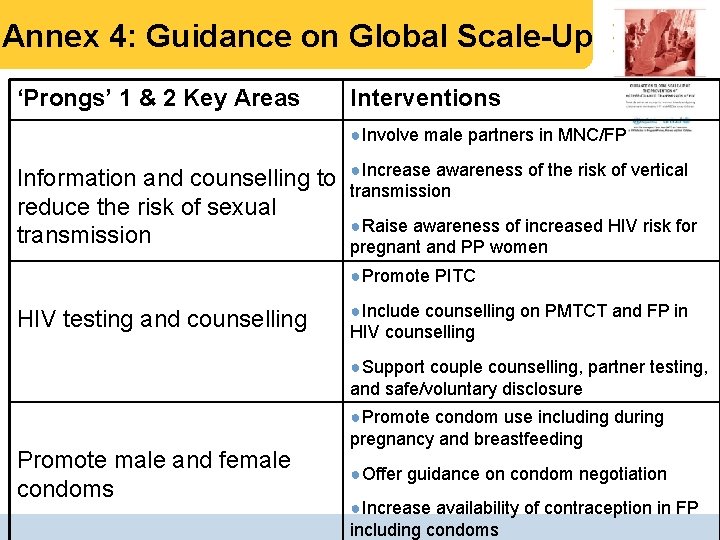
Annex 4: Guidance on Global Scale-Up ‘Prongs’ 1 & 2 Key Areas Interventions ●Involve male partners in MNC/FP Information and counselling to reduce the risk of sexual transmission ●Increase awareness of the risk of vertical transmission ●Raise awareness of increased HIV risk for pregnant and PP women ●Promote PITC HIV testing and counselling ●Include counselling on PMTCT and FP in HIV counselling ●Support couple counselling, partner testing, and safe/voluntary disclosure Promote male and female condoms ●Promote condom use including during pregnancy and breastfeeding ●Offer guidance on condom negotiation ●Increase availability of contraception in FP including condoms
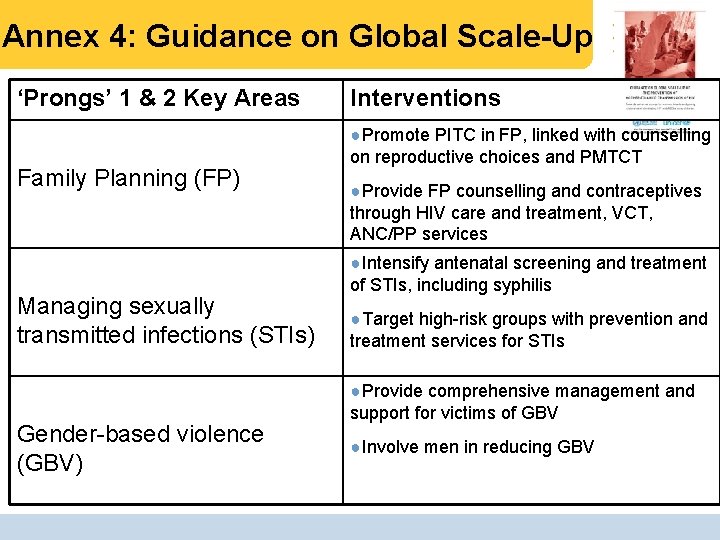
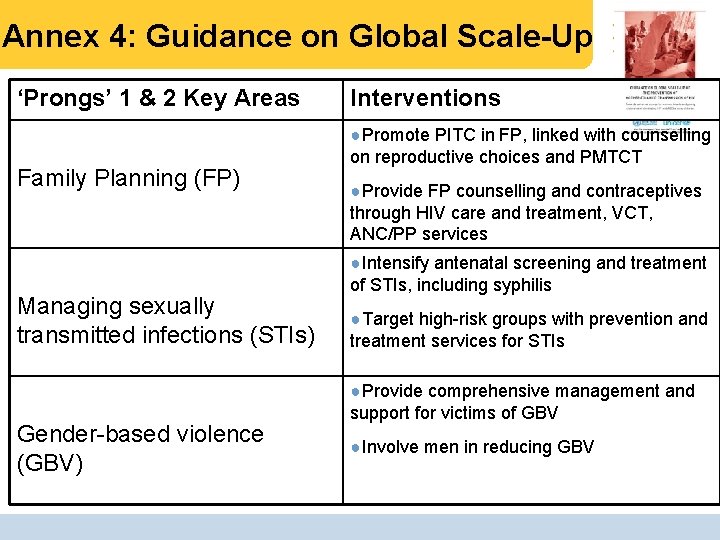
Annex 4: Guidance on Global Scale-Up ‘Prongs’ 1 & 2 Key Areas Family Planning (FP) Managing sexually transmitted infections (STIs) Gender-based violence (GBV) Interventions ●Promote PITC in FP, linked with counselling on reproductive choices and PMTCT ●Provide FP counselling and contraceptives through HIV care and treatment, VCT, ANC/PP services ●Intensify antenatal screening and treatment of STIs, including syphilis ●Target high-risk groups with prevention and treatment services for STIs ●Provide comprehensive management and support for victims of GBV ●Involve men in reducing GBV
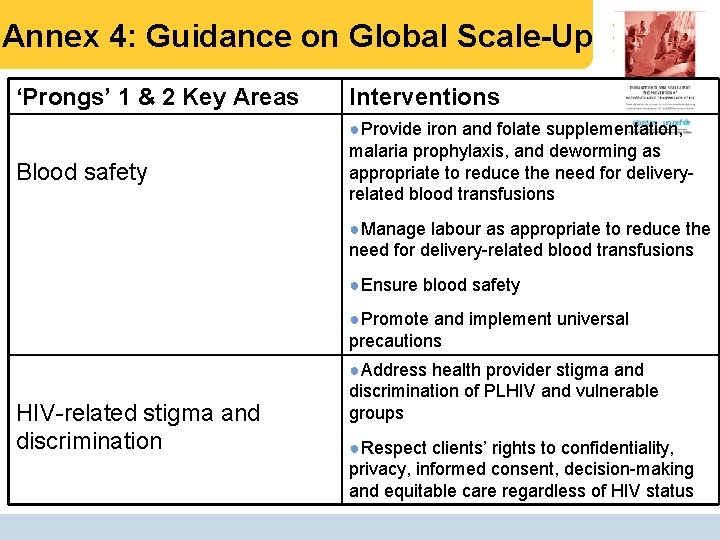
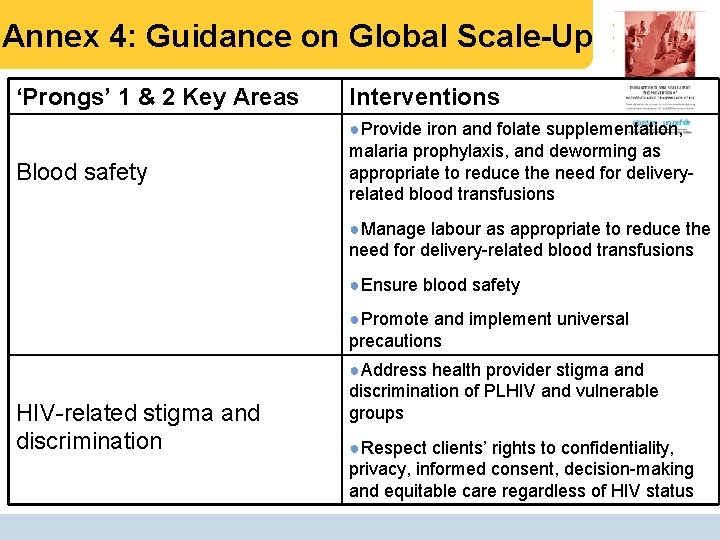
Annex 4: Guidance on Global Scale-Up ‘Prongs’ 1 & 2 Key Areas Blood safety Interventions ●Provide iron and folate supplementation, malaria prophylaxis, and deworming as appropriate to reduce the need for deliveryrelated blood transfusions ●Manage labour as appropriate to reduce the need for delivery-related blood transfusions ●Ensure blood safety ●Promote and implement universal precautions HIV-related stigma and discrimination ●Address health provider stigma and discrimination of PLHIV and vulnerable groups ●Respect clients’ rights to confidentiality, privacy, informed consent, decision-making and equitable care regardless of HIV status
 Who pmtct guidelines 2019
Who pmtct guidelines 2019 Dynamic linking vs static linking
Dynamic linking vs static linking Zygomycota characteristics
Zygomycota characteristics Fungi domain
Fungi domain Sexual health and relationships education scotland
Sexual health and relationships education scotland Mention any two different goals of rch programme
Mention any two different goals of rch programme Role of nurse in rch phase 2
Role of nurse in rch phase 2 Sti clinic st albans
Sti clinic st albans Redhill gum clinic
Redhill gum clinic What is sexual health
What is sexual health Sexual health
Sexual health Amsa sexual health leadership course
Amsa sexual health leadership course Society of sexual health advisers
Society of sexual health advisers Inguinal
Inguinal