LECTURE TOPIC VAGINITIS Vaginitis is a common presenting
- Slides: 27
LECTURE TOPIC: VAGINITIS Vaginitis is a common presenting symptom seen in the STD, Family Planning and Gynaecology clinics. It is often characterised by vaginal discharge with or without itching. Vaginal discharge may be physiological or pathological in origin. 1
Physiological causes • Vaginal discharge is a continuum. • Some patients do have copious discharge and others may have little or no discharge. • Thus, it is the patient who can determine what is the normal amount of discharge for herself. 2
• But normal vaginal discharge may increase pre-menstrually, at ovulation time, when on contraceptive pills or during pregnancy. • The use of douches, deodorant or perfumed soap may cause inflammation that may result in vaginal discharge 3
Pathological causes: The common causative agents of pathological vaginal discharge are: Candida albicans Trichomonas vaginalis Gardnerella vaginalis Mobiluncus and anaerobes 4
These agents colonise the genital tract or are usually sexually transmitted. A woman coming to the clinic with a complaint of vaginitis/vaginal discharge should be thoroughly investigated, followed up and counseled where necessary. 5
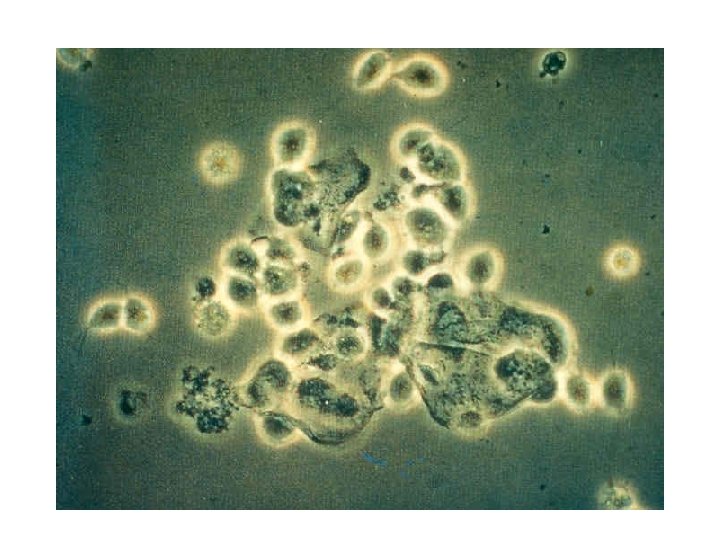
Candida albicans: By far the commonest cause of vaginal discharge is the Candida albicans ( 90 – 95% ). The condition is also known as candidiasis, moniliasis or thrush. Other species of Candida and other yeasts e. g. Torulosis glabrata, may also be involved. Contraction may be by sexual or non-sexual contact Infection limited to labia, vulva and vaginal mucosa 6
Signs and symptoms Causes intense vaginal itching ( pruritis ) and cordlike (cheesy) discharge Also associated with pregnancy, diabetes mellitus, antibiotic use, oral contraceptive, and immunosuppression. Causes soreness, redness and irritation of the penis in men especially in the uncircumcised ones. 7
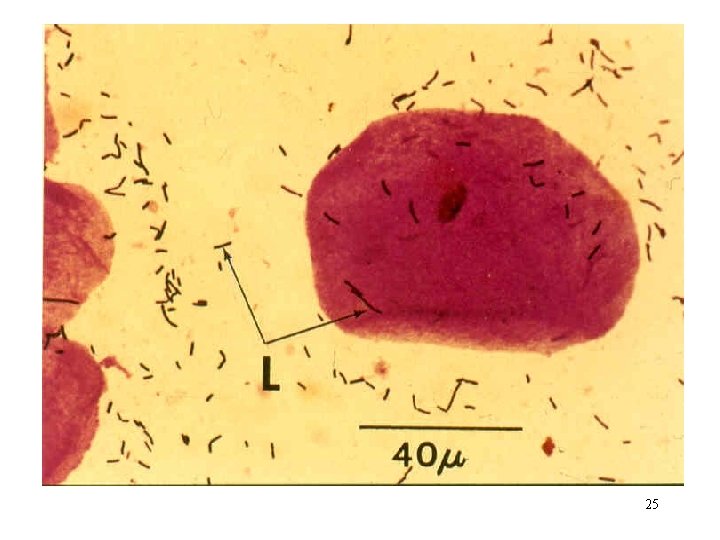
Laboratory diagnosis Specimen High vaginal swab (HVS): Microscopy: Wet Prep – Budding yeast cells in the presence or absence of pus cells Gram stain – Gram positive yeast cells Culture: Onto SAB agar at 370 C for 48 hrs. 8
Identification: Germ tube test: Pseudo hyphae API Aux Sensitivity test: Very sensitive to nystatin, fluconazole, etc. The antifungal drugs are poorly absorbed, so treatment is usually topical with creams and pessaries. 9
Trichomonas vaginalis T. vaginalis infection is also known as trichomoniasis. It presents with severe symptoms in women. The infection is nearly always sexually transmitted 10
• Signs and symptoms Copious, frothy greenish foul smelling discharge Moderate to severe vulval itching May present with acute pelvic pain Causes mild urethritis with occasional pin-prick pain in the urethra in men. 11
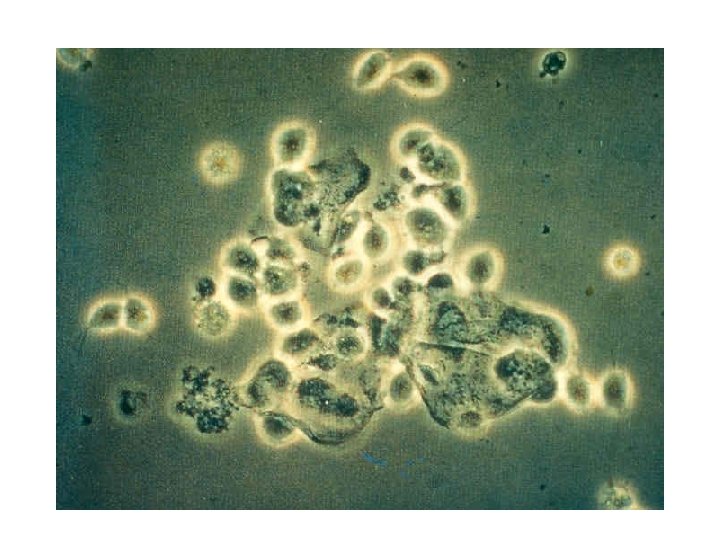
Laboratory diagnosis Specimen High vaginal swab (HVS) Microscopy i) Wet Prep – Motile T. vaginalis and pus cells. ii) Pap stain – Good morphology of T. vaginalis iii) Acridine orange stain- Stains yellow iv) Gram stain- Stains red 12
Culture - Can be done but not a routine test. • Urine Microscopy: Centrifuged urine – look for motile T. vaginalis Treatment: Usually with flagyl ( metronidazole ) and related drugs. . 13
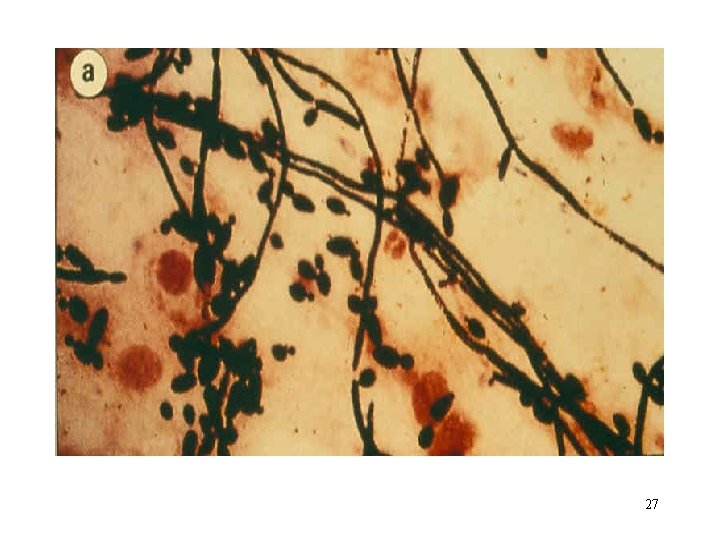
Gardnerella vaginalis G. vaginalis causes a mild form of vaginitis. It is characterized by light greenish vaginal discharge with little or no itching. It is believed to be a sexually transmitted disease. Symptoms are absent in men. 14
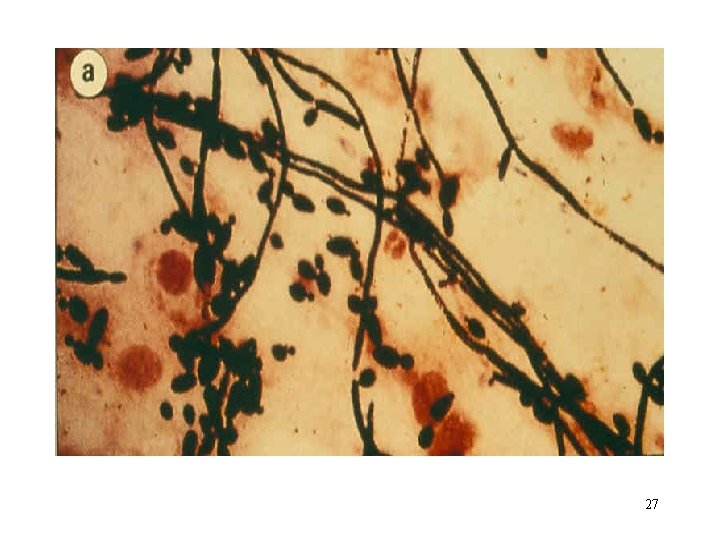
Laboratory diagnosis Specimen High vaginal swab (HVS) Microscopy – Wet Prep: “Clue” cells with few or no pus cells Gram stain: “clue” cells easier to recognize: vaginal epithelial cell covered by numerous Gram variable small rods. Acridine orange stain: “Clue” cells stain yellow 15
Culture Columbia nalidixic acid human blood agar or Chocolate agar, microaerophilic or CO 2 incubation at 370 C for 48 hours. Beta haemolytic, catalase and oxidase negative. Sensitivity – sensitive to metronidazole, amoxacyline, clindamycin etc. Necessary to treat sexual partners of patients. 16
Bacterial vaginosis • A mixed bacterial flora of G. vaginalis, Mobiluncus species and other anaerobes cause the condition known as bacterial vaginosis. • This condition used to be referred to as non-specific vaginitis and it is a common syndrome in sexually active females. • Contraction is invariably by sexual contact. • It is called vaginosis due to lack of inflammatory cells. 17
• Signs and symptoms It is mainly symptomised by thin dirty vaginal discharge with very offensive fishy odour; p. H above 5. 0. No pain or irritation. - Men are usually asymptomatic. • Laboratory diagnosis • Specimen High vaginal swab (HVS) Microscopy – Same as for G. vaginalis. 18
Culture Same as for G. vaginalis but incubate anaerobically Amine smell on addition of KOH Sensitivity Sensitive to metronidazole Treat the partner of a positive case. etc. 19
• Other less frequent aetiological agents of pathological vaginal discharge (vaginitis) include: • Streptococcus group B: • This organism colonises the vagina with little or no symptoms i. e. very scanty or no discharge. 20
It must be treated when isolated fromm a pregnant woman because the baby can be infected during delivery and so may develop neonatal meningitis or sepsis. • ·Neisseria gonorrhoeae: • This organism causes cervicitis accompanied by cervical discharge which flows into the vagina. N. gonorrhoeae does not infect the vagina per se. 21
Definitive laboratory diagnosis lies in the isolation and identification of the organism from HVS or cervical swab. · Chlamydia trachomatis: This organism causes cervical infection resulting in cervical discharge which in turn flows down into the vagina. It is diagnosed in the laboratory by tissue culture or microscopy. 22
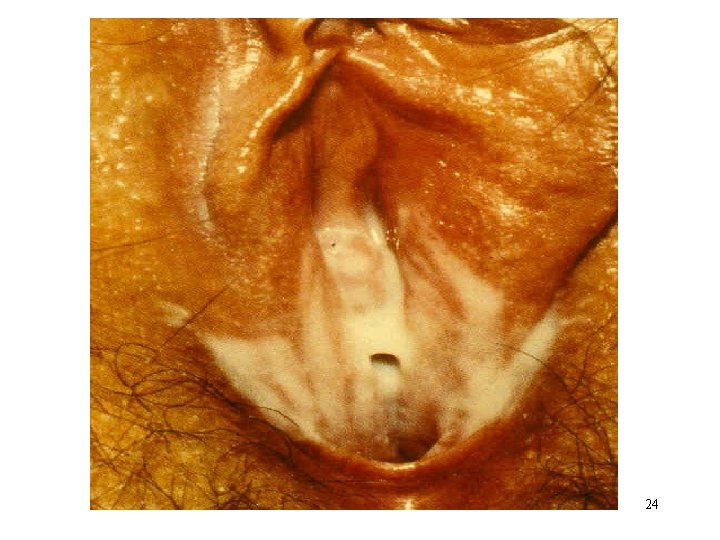
Cervical lesions due to i) Herpes (HSV), ii) Genital warts(HPV) iii) Syphilitic sores (T. pallidum) may all result in the production of cervical and vaginal discharge. 23
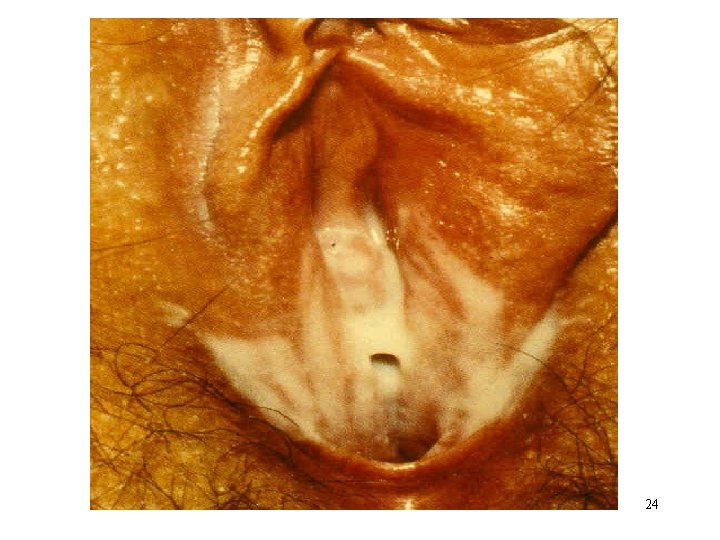
24
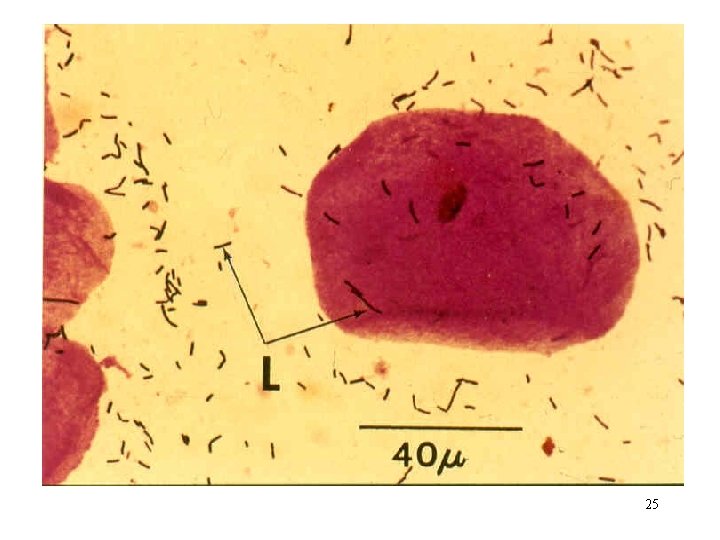
25
26
27