Vaginitis Cases From the common to the challenging












- Slides: 46
Vaginitis Cases: From the common to the challenging Caroline Mitchell, MD, MPH Vincent Center for Reproductive Biology, MGH Assistant Professor, Harvard Medical School
Caroline Mitchell, MD, MPH Dr. Mitchell is a consultant for Scynexis, Inc and receives research funding from Merck Additional disclosure: Some of the treatment regimens discussed are not FDA approved for the specific indication for which they are mentioned. 2

Learning Objectives At the end of this presentation, the participant will be able to: • Describe the differential diagnosis for vaginal discharge and the clinical signs and symptoms associated with each of the major causes. • Outline the tests needed to confirm diagnosis and appropriate treatments. • Explain the challenges of recurrent and resistant infections.
Case 1 SC is a 27 -year-old G 1 P 1 woman who presents with 3 day history of worsening vulvovaginal pruritis, thick vaginal discharge and some dysuria. She has had one sexual partner for the past 3 years. She reports a history of gestational diabetes in her pregnancy a year ago. She relies on birth control pills for contraception. She tried to douche to relieve her symptoms, but to no avail. Her BMI is 26 kg/m 2. On exam, her vulva is erythematous, edematous and somewhat excoriated. Speculum exam reveals thick adherent white clumpy discharge. Cervix has no mucopurulent discharge and there is no CMT.
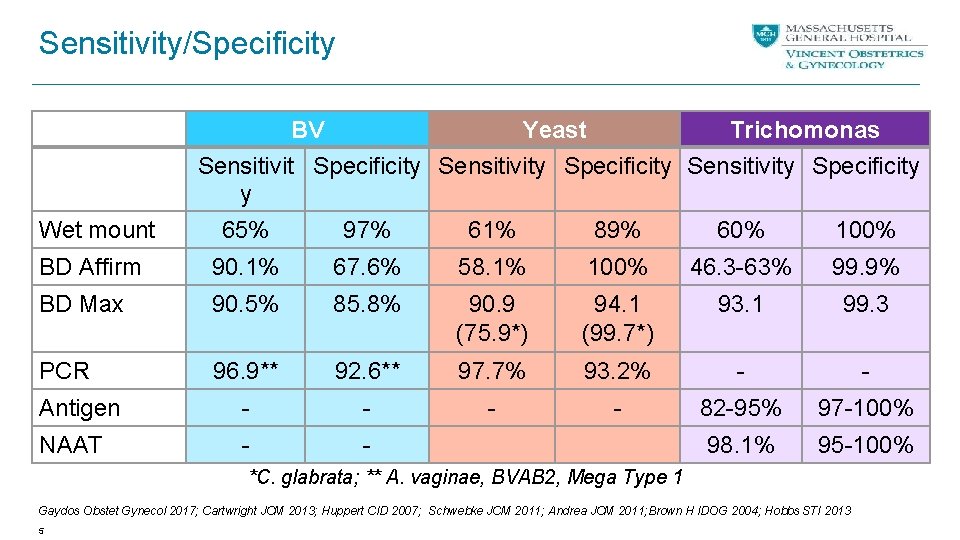
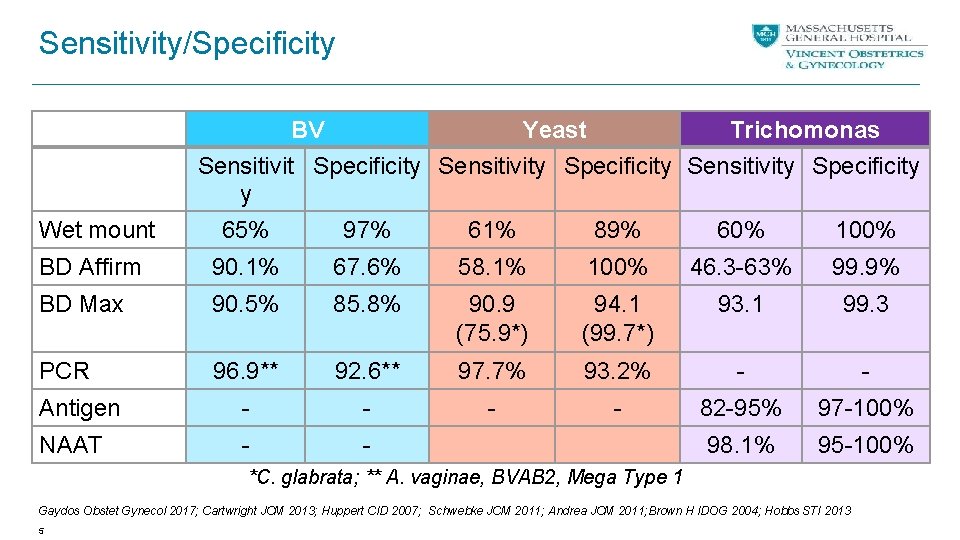
Sensitivity/Specificity Wet mount BV Yeast Trichomonas Sensitivit Specificity Sensitivity Specificity y 65% 97% 61% 89% 60% 100% BD Affirm 90. 1% 67. 6% 58. 1% 100% 46. 3 -63% 99. 9% BD Max 90. 5% 85. 8% 90. 9 (75. 9*) 94. 1 (99. 7*) 93. 1 99. 3 PCR 96. 9** 92. 6** 97. 7% 93. 2% - - Antigen - - 82 -95% 97 -100% NAAT - - 98. 1% 95 -100% *C. glabrata; ** A. vaginae, BVAB 2, Mega Type 1 Gaydos Obstet Gynecol 2017; Cartwright JCM 2013; Huppert CID 2007; Schwebke JCM 2011; Andrea JCM 2011; Brown H IDOG 2004; Hobbs STI 2013 5

6

Yeast Clinical p. H WBC Bacteria Other Discharge, Itching Normal +/- Lactobacilli usually present Hyphae, buds 96% Candida albicans
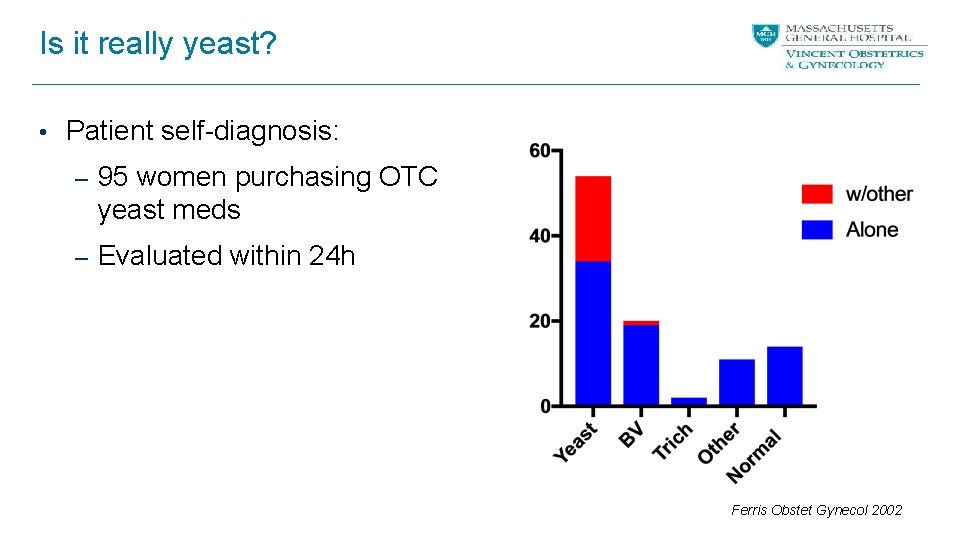
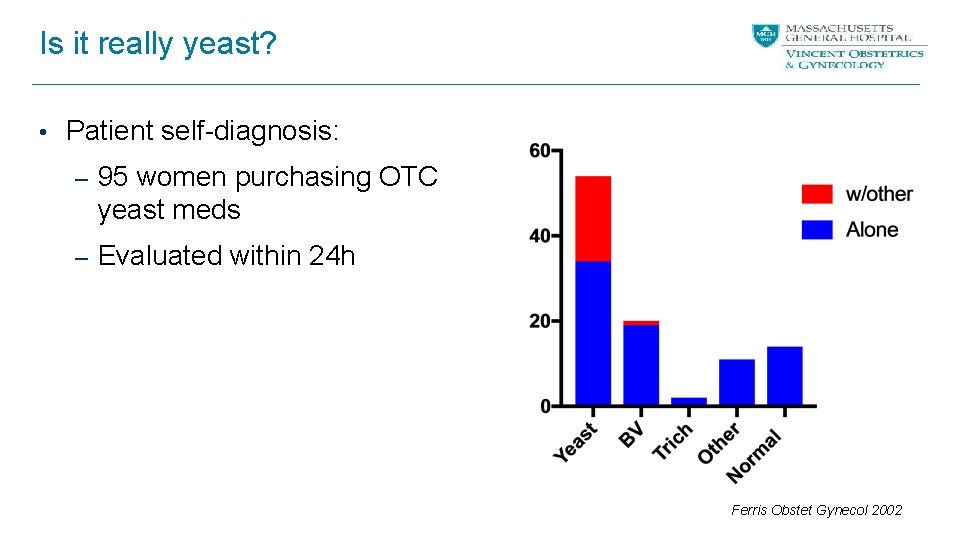
Is it really yeast? • Patient self-diagnosis: – 95 women purchasing OTC yeast meds – Evaluated within 24 h Ferris Obstet Gynecol 2002
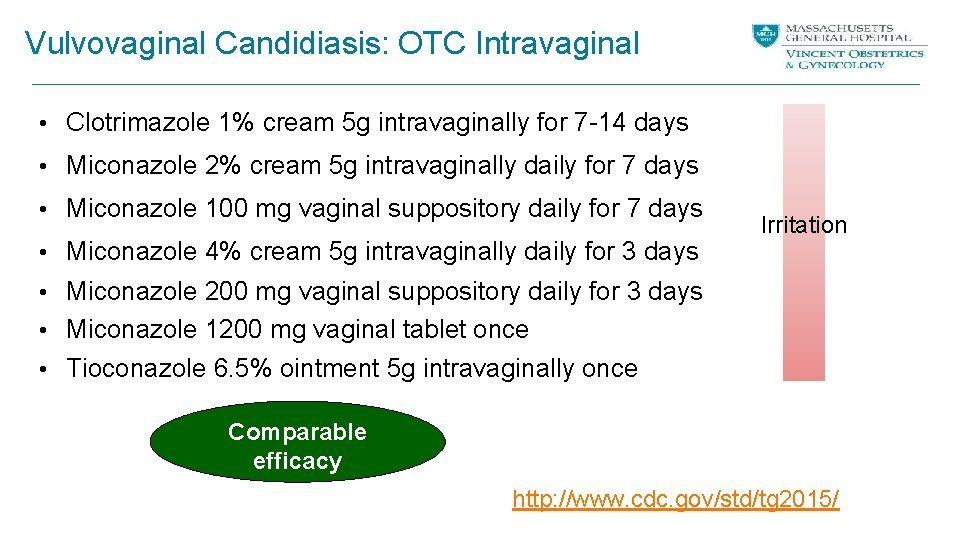
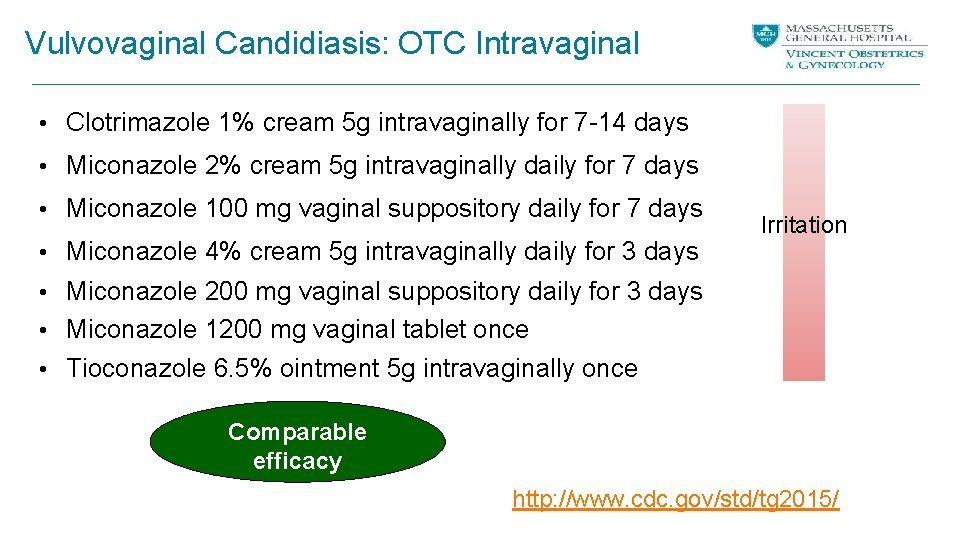
Vulvovaginal Candidiasis: OTC Intravaginal • Clotrimazole 1% cream 5 g intravaginally for 7 -14 days • Miconazole 2% cream 5 g intravaginally daily for 7 days • Miconazole 100 mg vaginal suppository daily for 7 days • Miconazole 4% cream 5 g intravaginally daily for 3 days Irritation • Miconazole 200 mg vaginal suppository daily for 3 days • Miconazole 1200 mg vaginal tablet once • Tioconazole 6. 5% ointment 5 g intravaginally once Comparable efficacy http: //www. cdc. gov/std/tg 2015/

Vulvovaginal Candidiasis: Rx Intravaginal • Butoconazole 2% cream (bioadhesive product), 5 g • • intravaginally in a single application Tioconazole 6. 5% ointment 5 g intravaginally once Terconazole 0. 4% cream 5 g intravaginally nightly for 7 days Terconazole 0. 8% cream 5 g intravaginally nightly for 3 days Terconazole 80 mg suppository nightly for 3 days Comparable efficacy http: //www. cdc. gov/std/tg 2015/
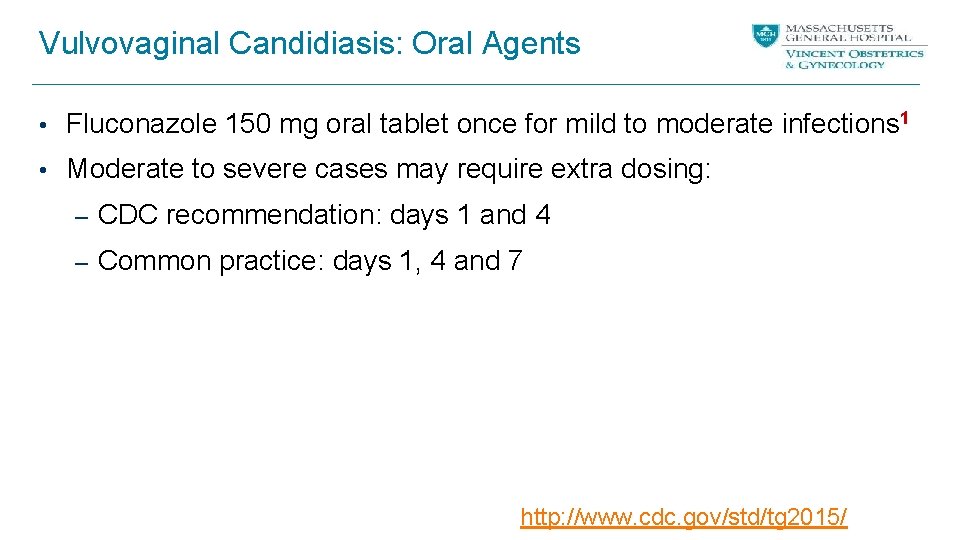
Vulvovaginal Candidiasis: Oral Agents • Fluconazole 150 mg oral tablet once for mild to moderate infections 1 • Moderate to severe cases may require extra dosing: – CDC recommendation: days 1 and 4 – Common practice: days 1, 4 and 7 http: //www. cdc. gov/std/tg 2015/
Case 1 She comes back a year later, having self-treated symptoms several times with OTC products. She went to an urgent care where they did an exam but no testing, and she was given a single dose of fluconazole, which helped. She again has symptoms of itching, vaginal discharge and pain with sex.
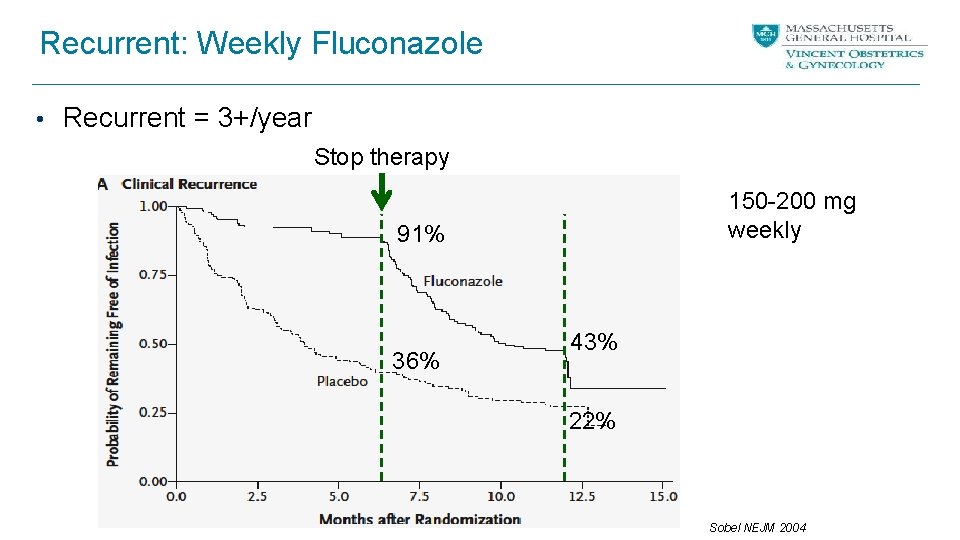
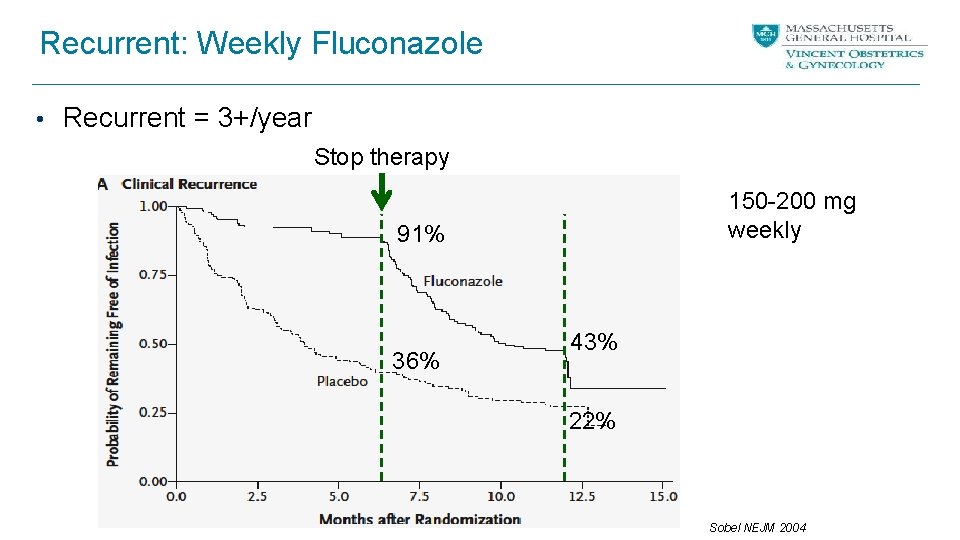
Recurrent: Weekly Fluconazole • Recurrent = 3+/year Stop therapy 150 -200 mg weekly 91% 36% 43% 22% Sobel NEJM 2004
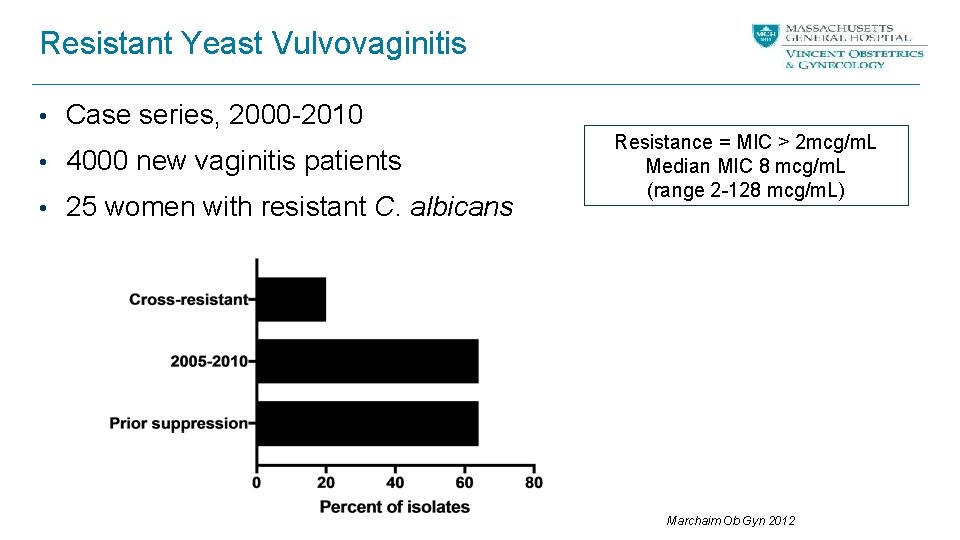
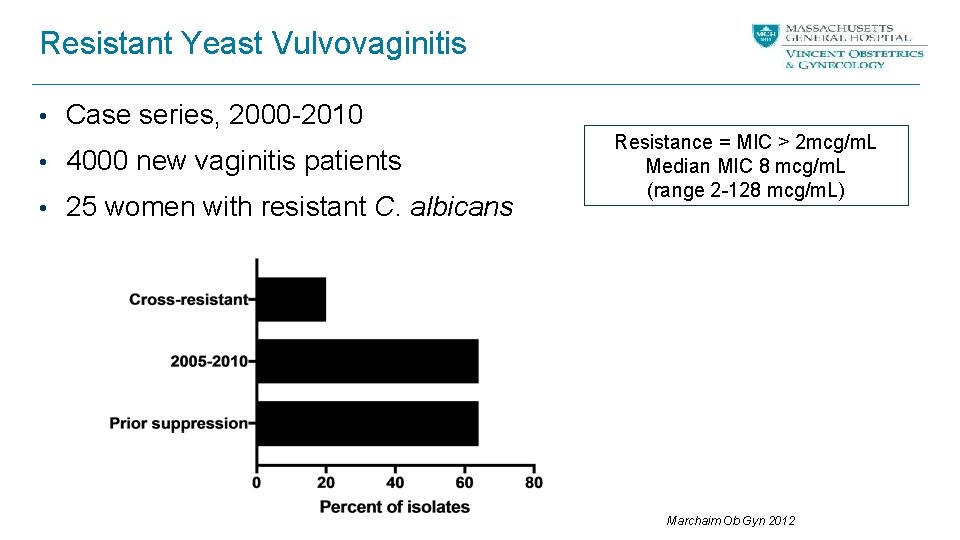
Resistant Yeast Vulvovaginitis • Case series, 2000 -2010 • 4000 new vaginitis patients • 25 women with resistant C. albicans Resistance = MIC > 2 mcg/m. L Median MIC 8 mcg/m. L (range 2 -128 mcg/m. L) Marchaim Ob Gyn 2012
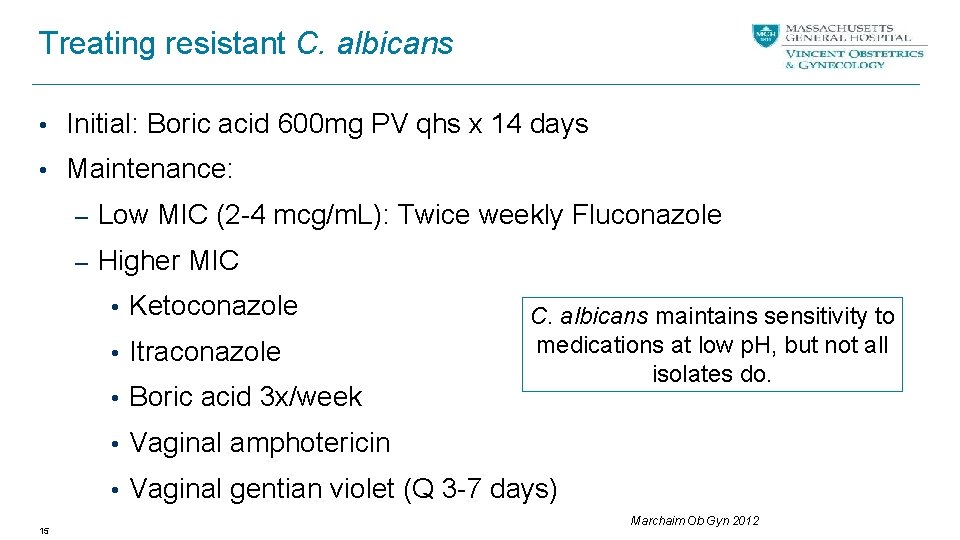
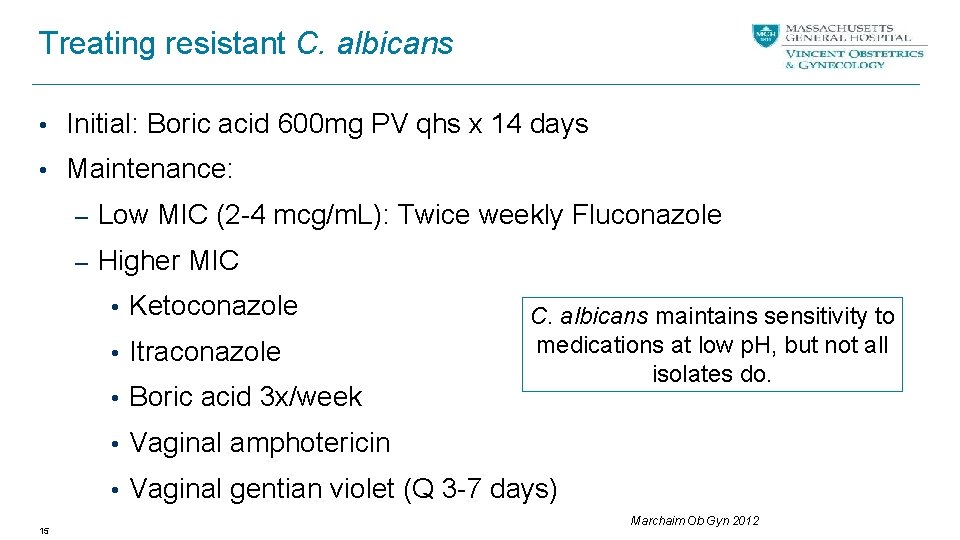
Treating resistant C. albicans • Initial: Boric acid 600 mg PV qhs x 14 days • Maintenance: – Low MIC (2 -4 mcg/m. L): Twice weekly Fluconazole – Higher MIC • Ketoconazole • Itraconazole • Boric acid 3 x/week C. albicans maintains sensitivity to medications at low p. H, but not all isolates do. • Vaginal amphotericin • Vaginal gentian violet (Q 3 -7 days) 15 Marchaim Ob Gyn 2012
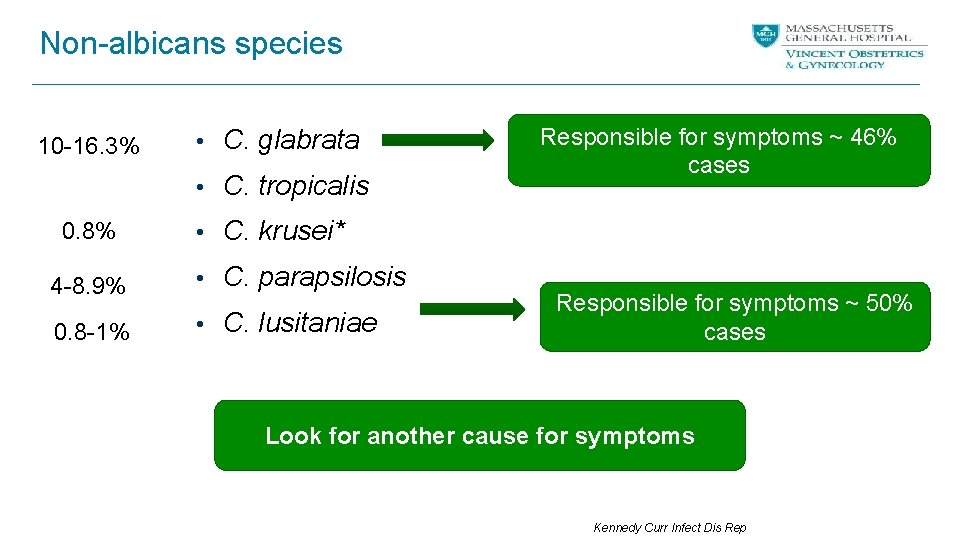
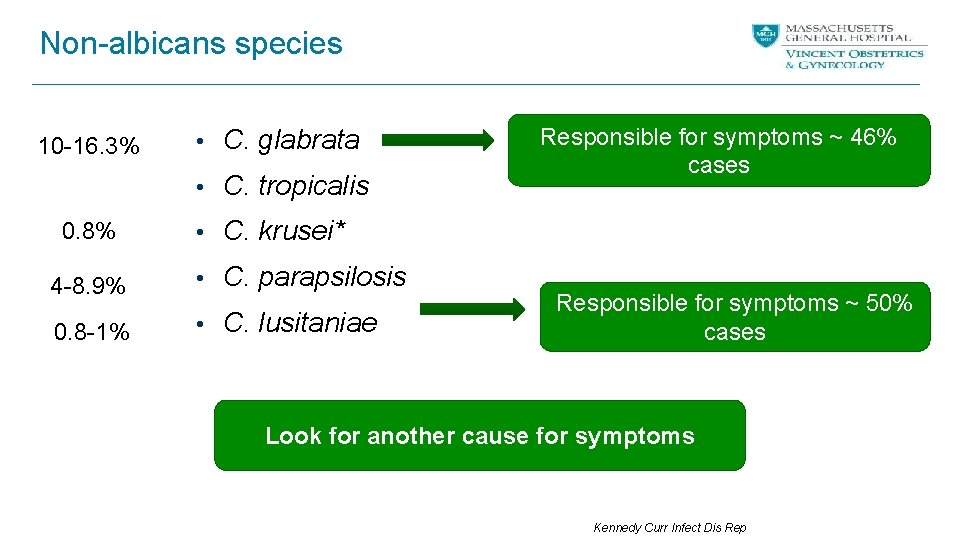
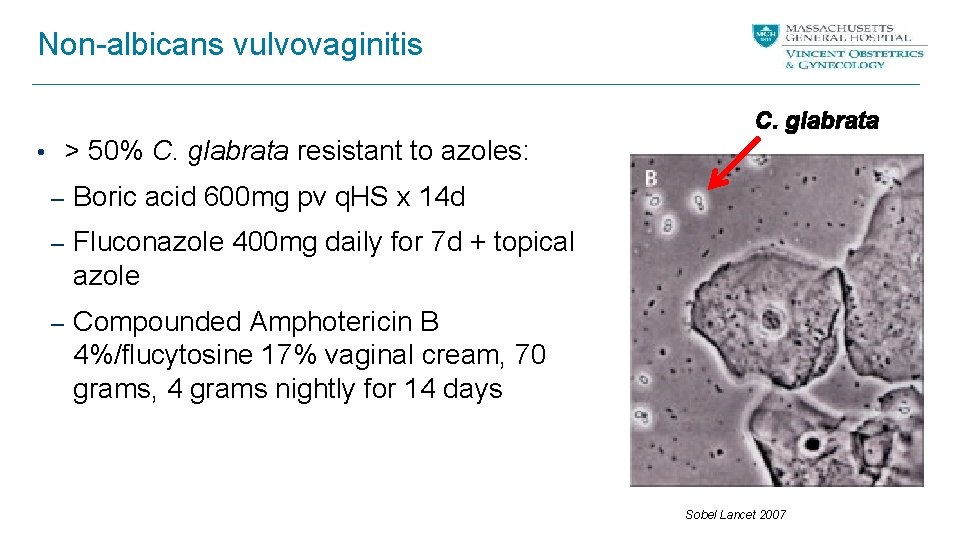
Non-albicans species 10 -16. 3% • C. glabrata • C. tropicalis 0. 8% Responsible for symptoms ~ 46% cases • C. krusei* 4 -8. 9% • C. parapsilosis 0. 8 -1% • C. lusitaniae Responsible for symptoms ~ 50% cases Look for another cause for symptoms Kennedy Curr Infect Dis Rep
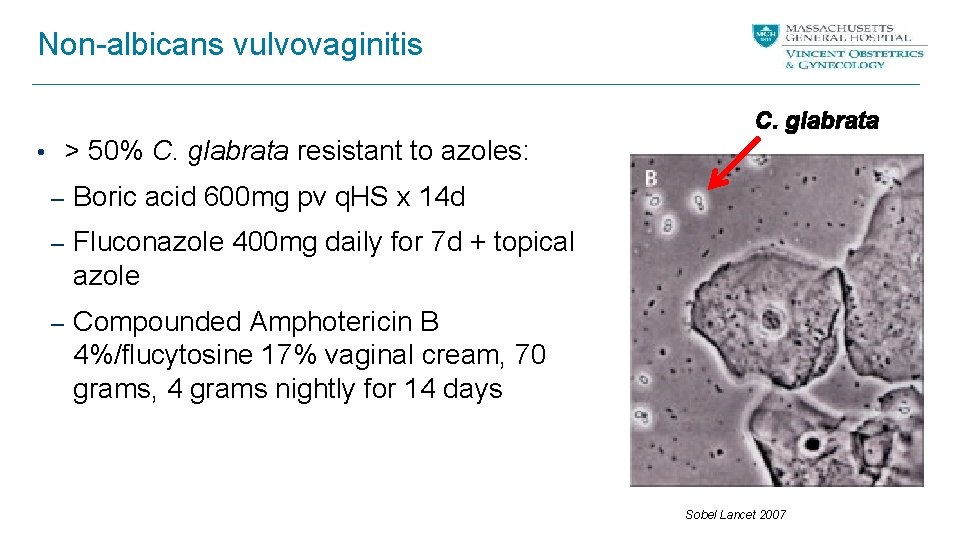
Non-albicans vulvovaginitis C. glabrata • > 50% C. glabrata resistant to azoles: – Boric acid 600 mg pv q. HS x 14 d – Fluconazole 400 mg daily for 7 d + topical azole – Compounded Amphotericin B 4%/flucytosine 17% vaginal cream, 70 grams, 4 grams nightly for 14 days Sobel Lancet 2007
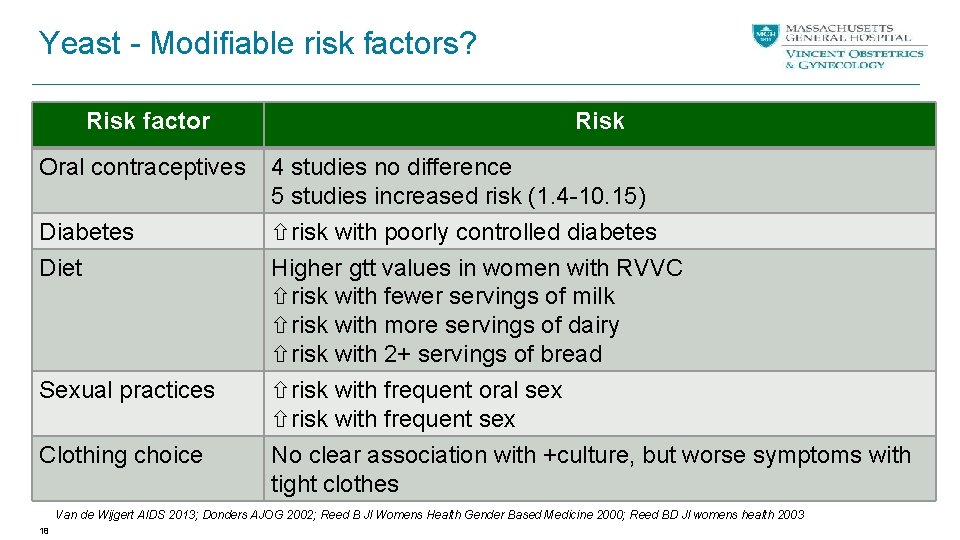
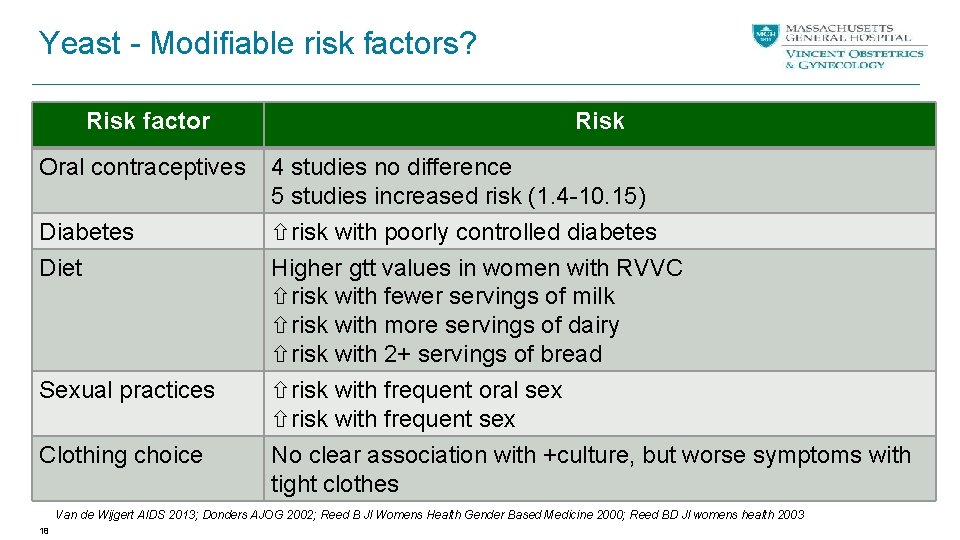
Yeast - Modifiable risk factors? Risk factor Oral contraceptives Diabetes Risk 4 studies no difference 5 studies increased risk (1. 4 -10. 15) risk with poorly controlled diabetes Diet Higher gtt values in women with RVVC risk with fewer servings of milk risk with more servings of dairy risk with 2+ servings of bread Sexual practices risk with frequent oral sex risk with frequent sex Clothing choice No clear association with +culture, but worse symptoms with tight clothes Van de Wijgert AIDS 2013; Donders AJOG 2002; Reed B Jl Womens Health Gender Based Medicine 2000; Reed BD Jl womens health 2003 18
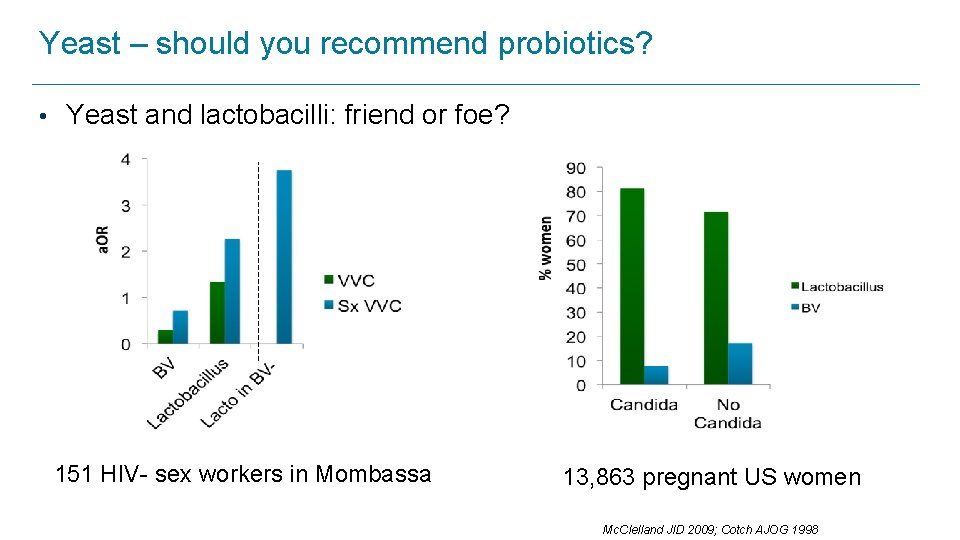
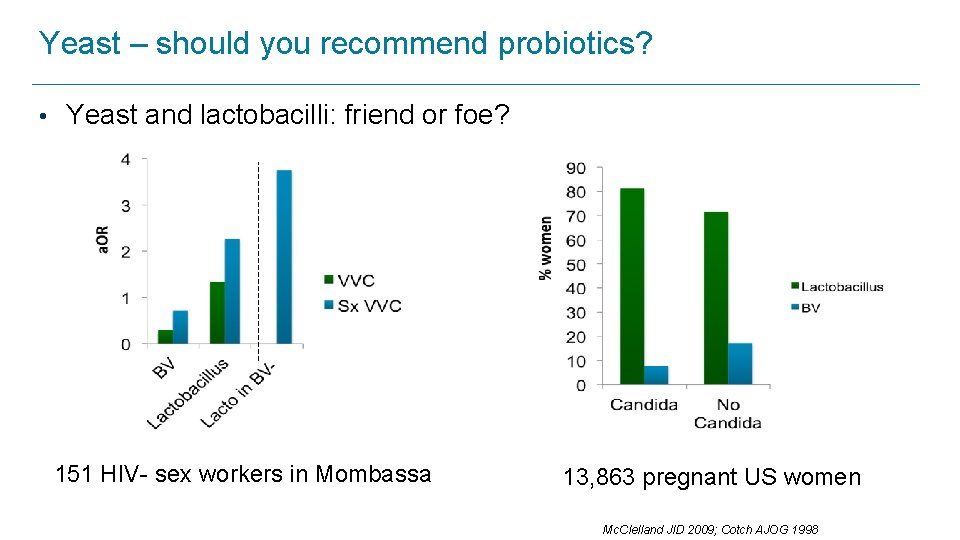
Yeast – should you recommend probiotics? • Yeast and lactobacilli: friend or foe? 151 HIV- sex workers in Mombassa 13, 863 pregnant US women Mc. Clelland JID 2009; Cotch AJOG 1998
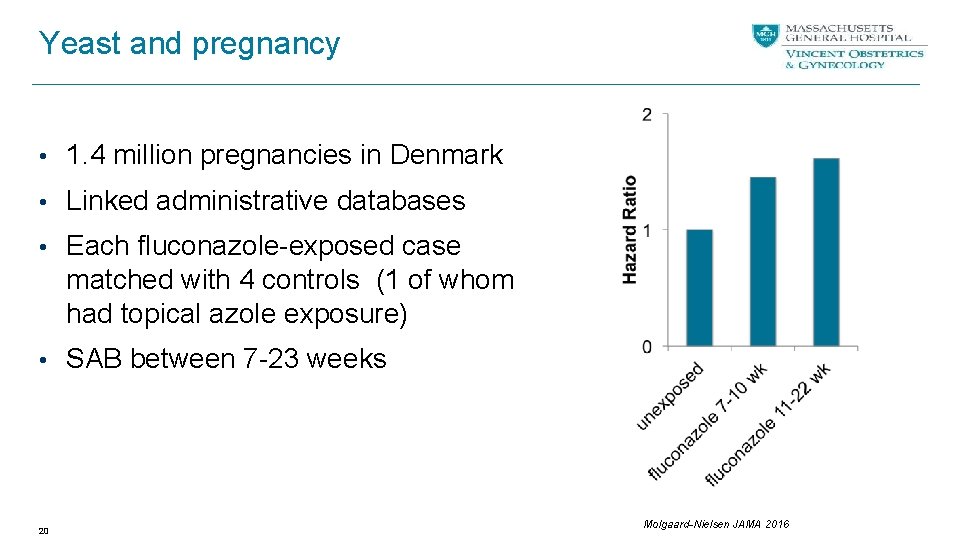
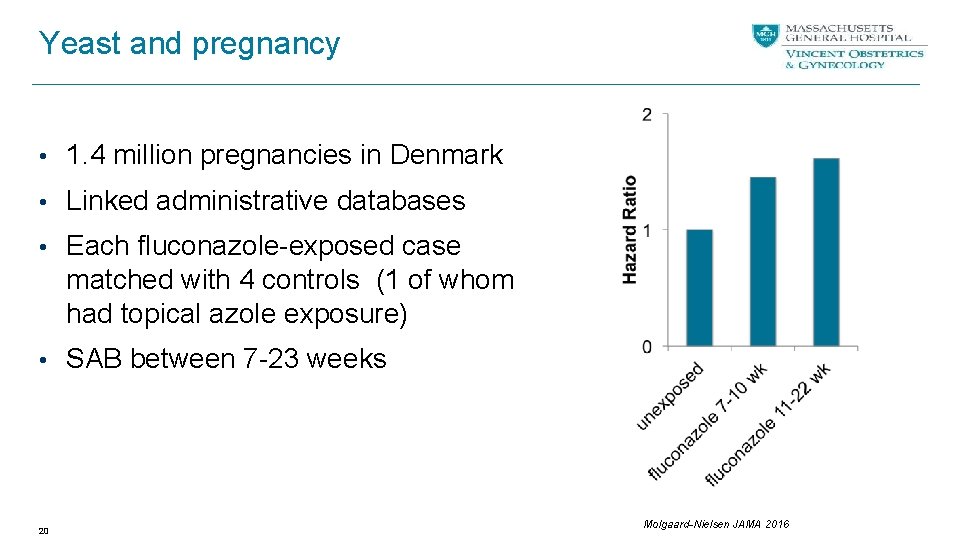
Yeast and pregnancy • 1. 4 million pregnancies in Denmark • Linked administrative databases • Each fluconazole-exposed case matched with 4 controls (1 of whom had topical azole exposure) • SAB between 7 -23 weeks 20 Molgaard-Nielsen JAMA 2016
What if. . . Her history was slightly different. What would you think of if all she had ever complained of was intense pruritis and post scratching burning without discharge and this is what you saw on your exam?

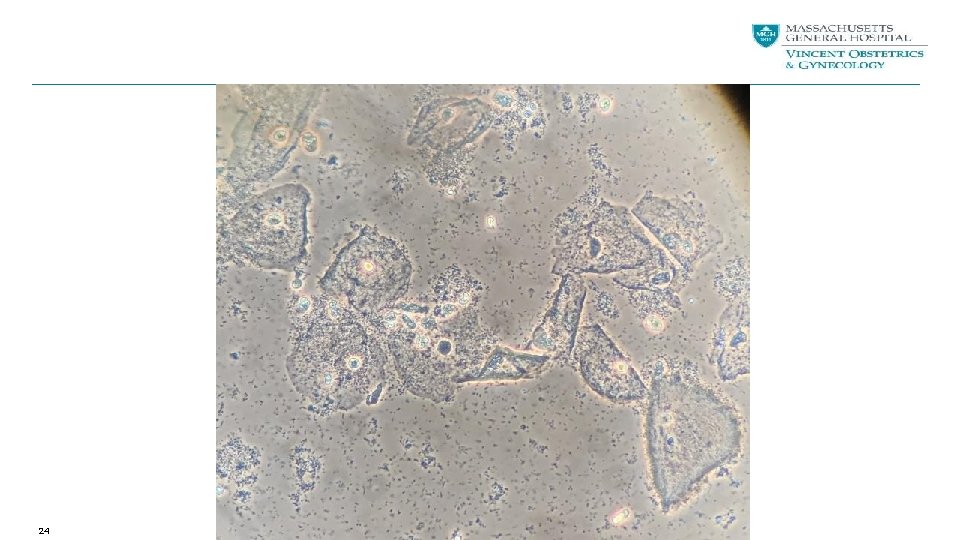
Case 2 A 23 -year-old heterosexual woman presents with classic symptoms of foul smelling vaginal discharge for about a week. Douching did not resolve symptoms for long. She denies any new sexual partners or any unprotected sex. She and her partner use external condoms fairly regularly. Vaginal p. H is 6. 0. On microscopy this is what you see. . .
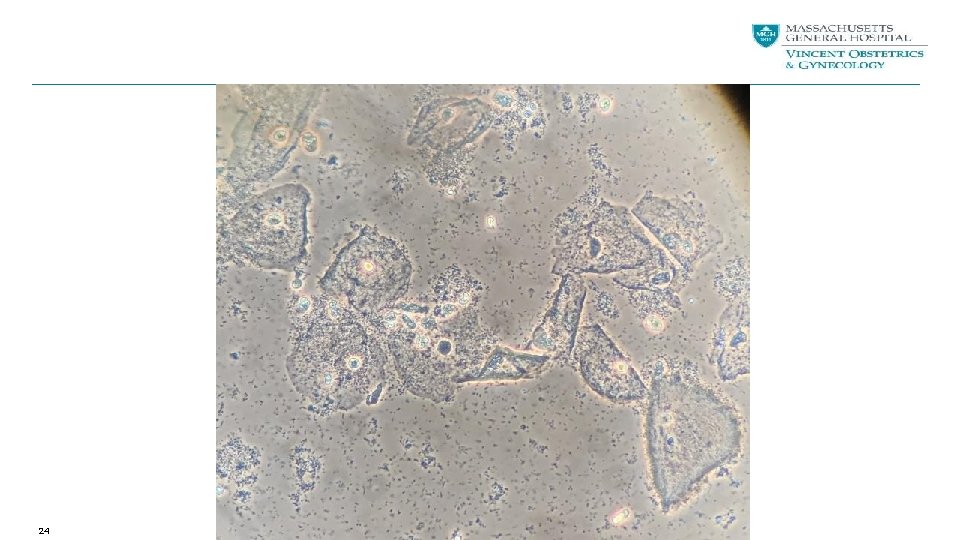
24
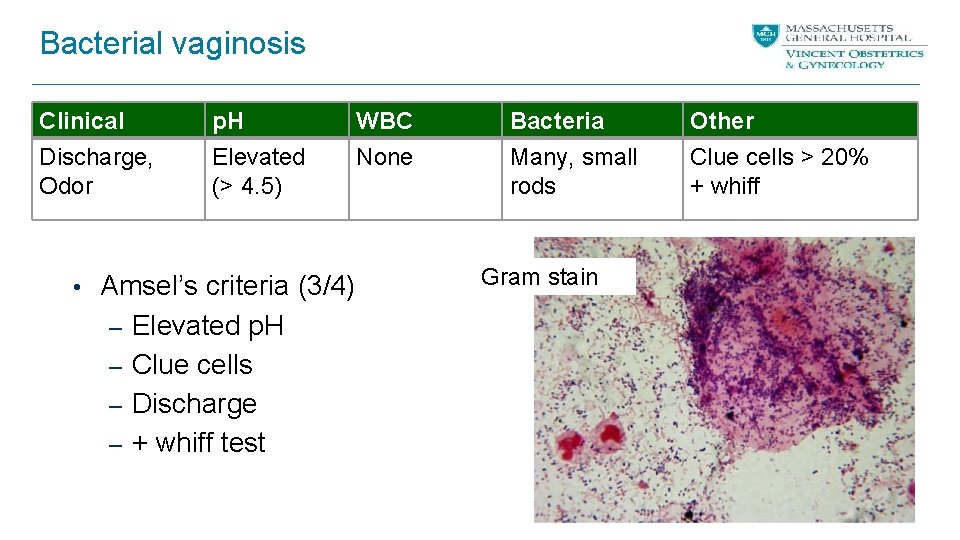
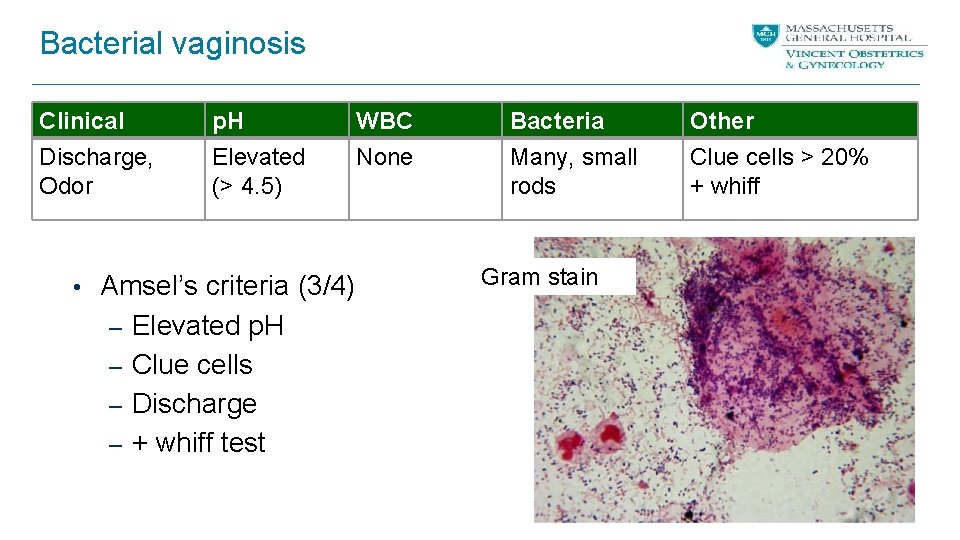
Bacterial vaginosis Clinical Discharge, Odor p. H Elevated (> 4. 5) • Amsel’s criteria (3/4) – Elevated p. H – Clue cells – Discharge – + whiff test WBC None Bacteria Many, small rods Gram stain Other Clue cells > 20% + whiff
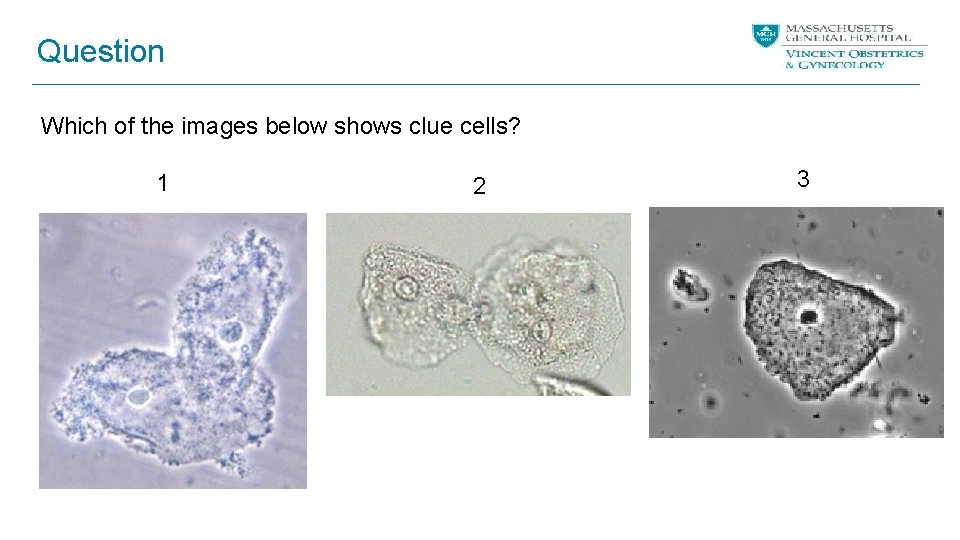
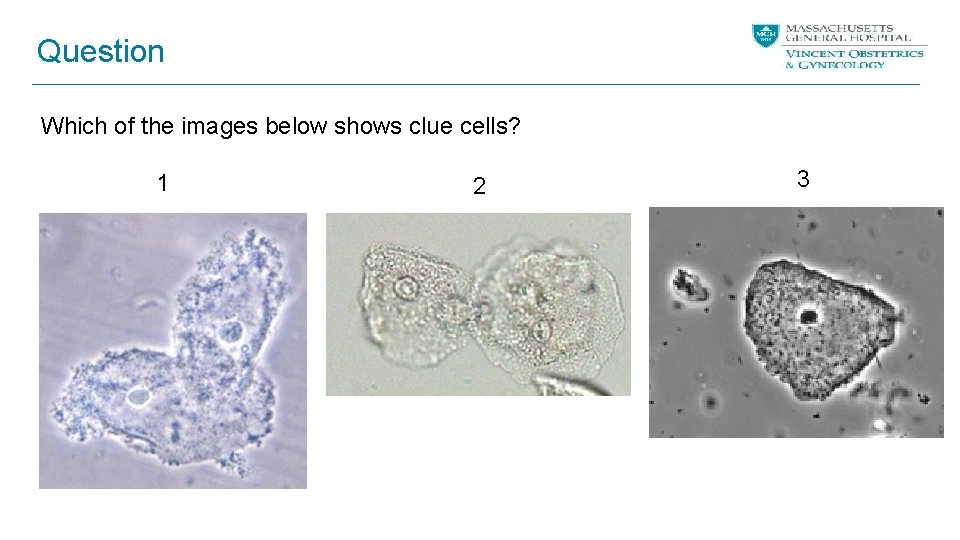
Question Which of the images below shows clue cells? 1 2 3

Question Which of the images below shows clue cells? 1 2 3
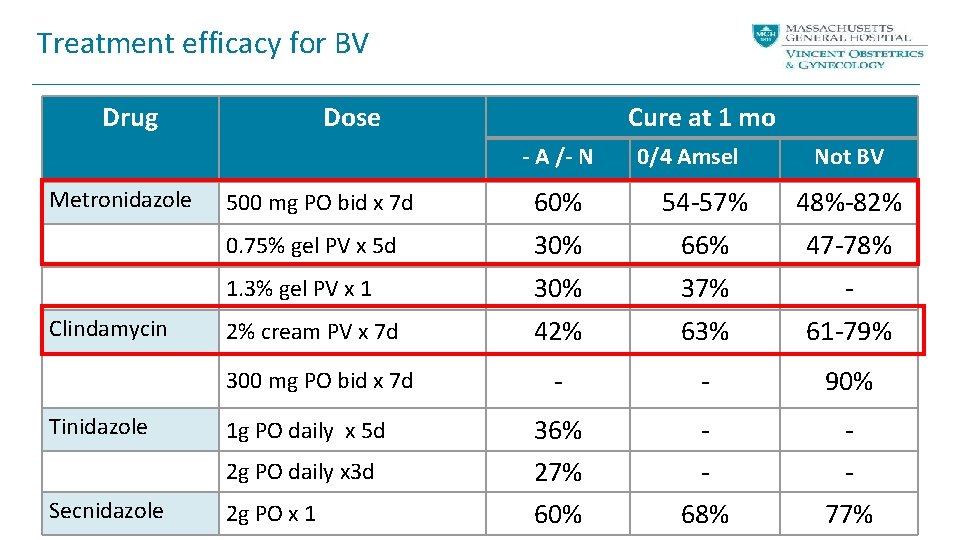
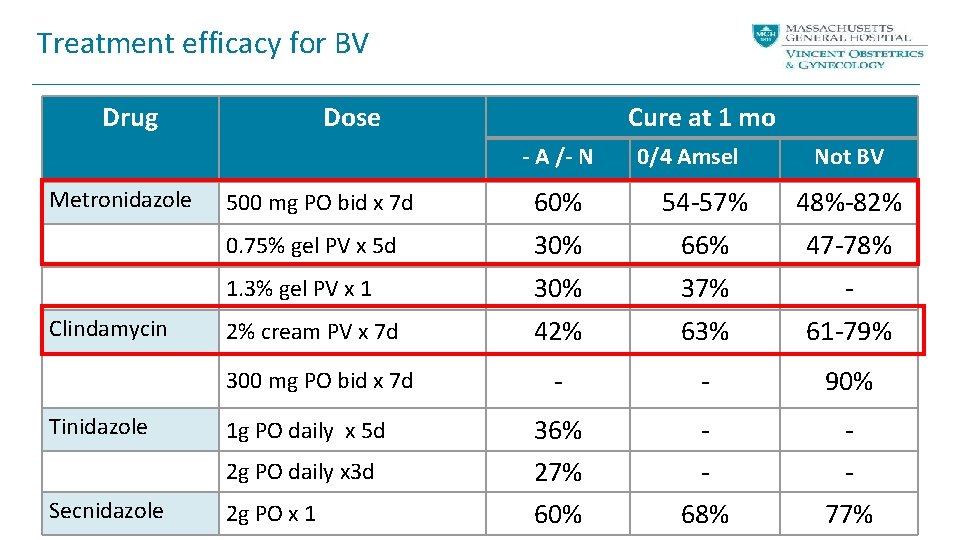
Treatment efficacy for BV Drug Dose Cure at 1 mo - A /- N Metronidazole Clindamycin 60% 54 -57% 48%-82% 0. 75% gel PV x 5 d 30% 66% 47 -78% 1. 3% gel PV x 1 30% 37% - 2% cream PV x 7 d 42% 63% 61 -79% - - 90% 36% 27% 60% 68% 77% 1 g PO daily x 5 d 2 g PO daily x 3 d Secnidazole Not BV 500 mg PO bid x 7 d 300 mg PO bid x 7 d Tinidazole 0/4 Amsel 2 g PO x 1
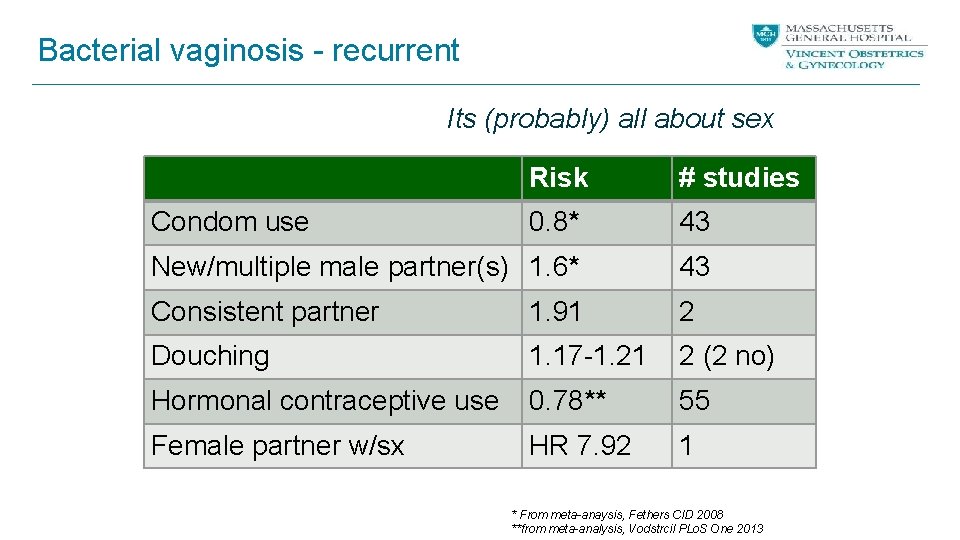
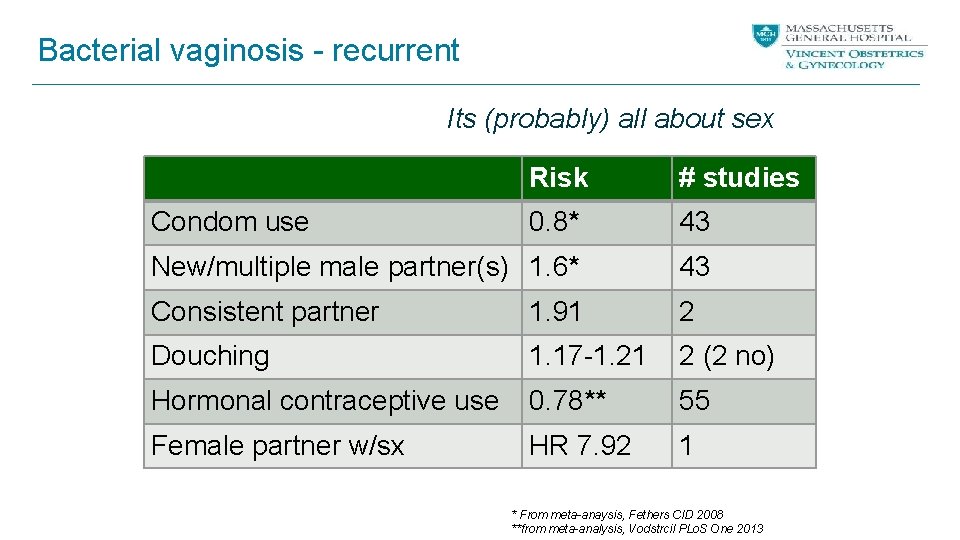
Bacterial vaginosis - recurrent Its (probably) all about sex Risk # studies 0. 8* 43 New/multiple male partner(s) 1. 6* 43 Consistent partner 1. 91 2 Douching 1. 17 -1. 21 2 (2 no) Hormonal contraceptive use 0. 78** 55 Female partner w/sx HR 7. 92 1 Condom use * From meta-anaysis, Fethers CID 2008 **from meta-analysis, Vodstrcil PLo. S One 2013
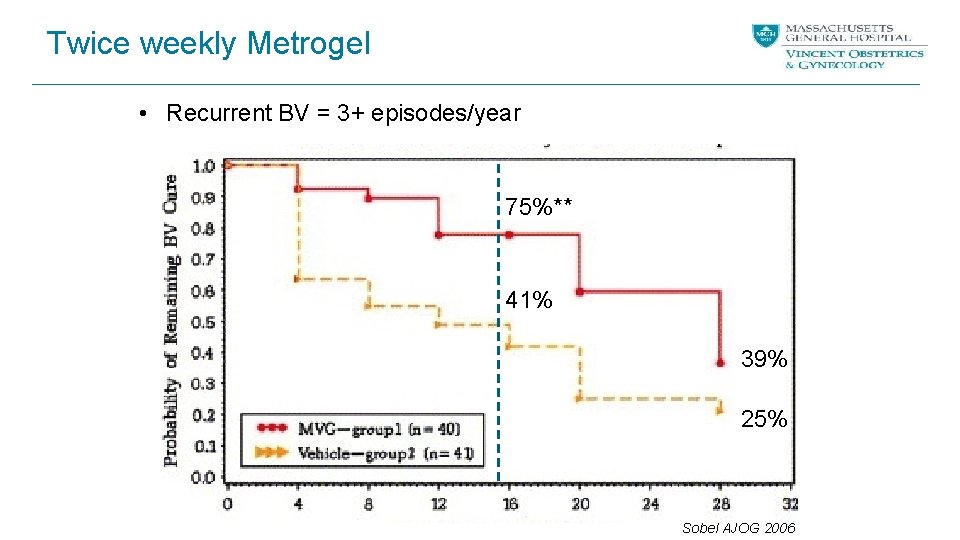
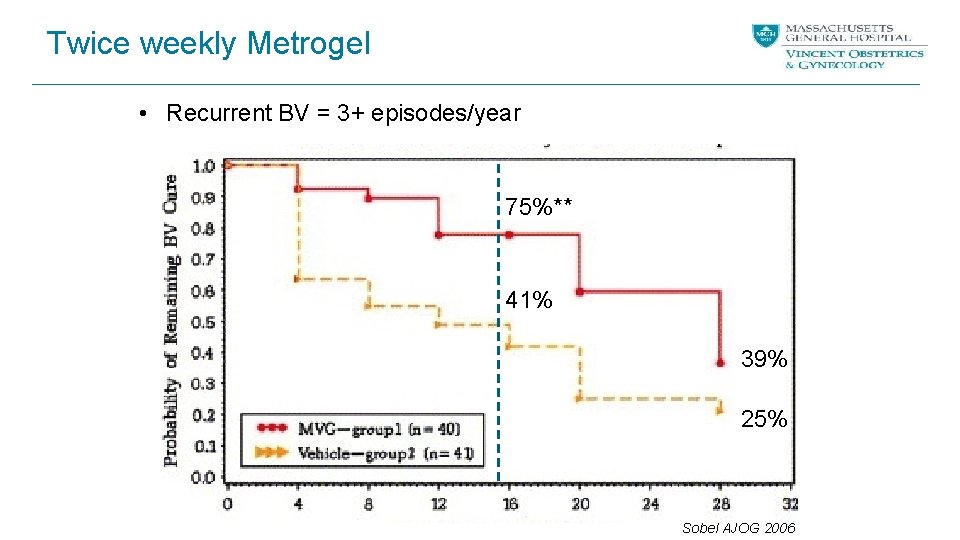
Twice weekly Metrogel • Recurrent BV = 3+ episodes/year 75%** 41% 39% 25% Sobel AJOG 2006
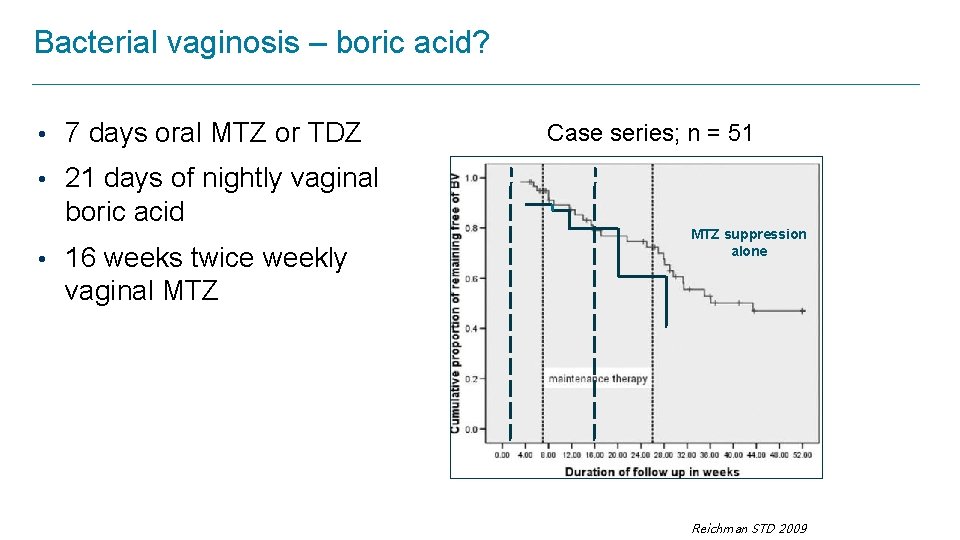
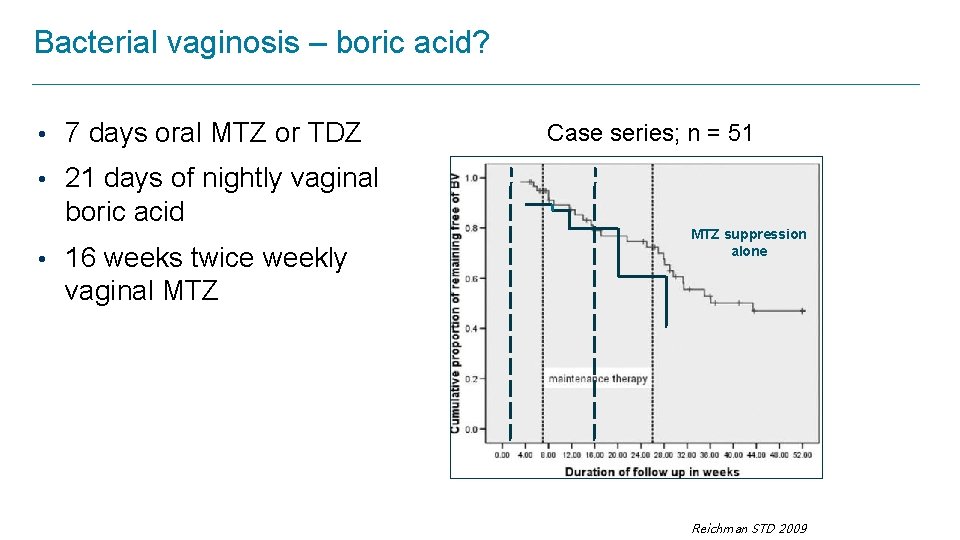
Bacterial vaginosis – boric acid? • 7 days oral MTZ or TDZ Case series; n = 51 • 21 days of nightly vaginal boric acid • 16 weeks twice weekly MTZ suppression alone vaginal MTZ Reichman STD 2009
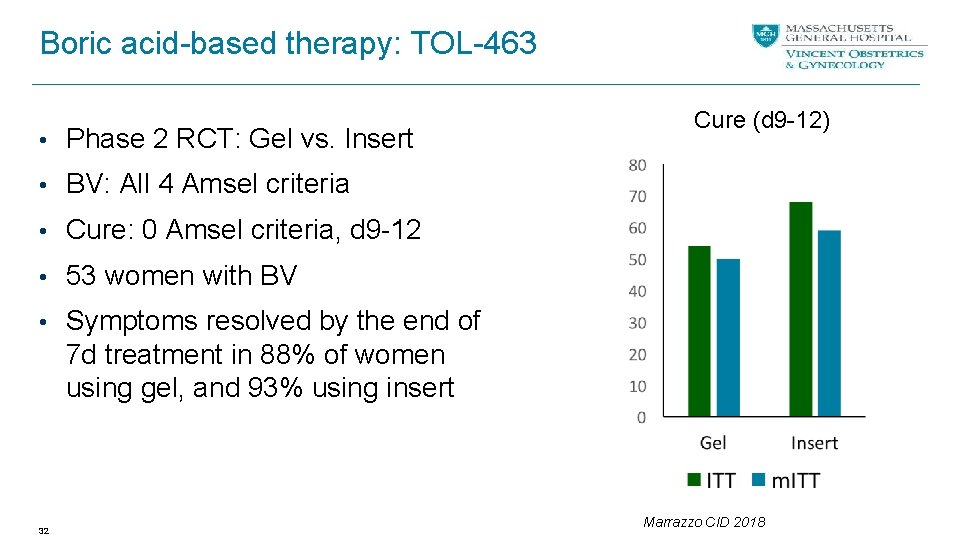
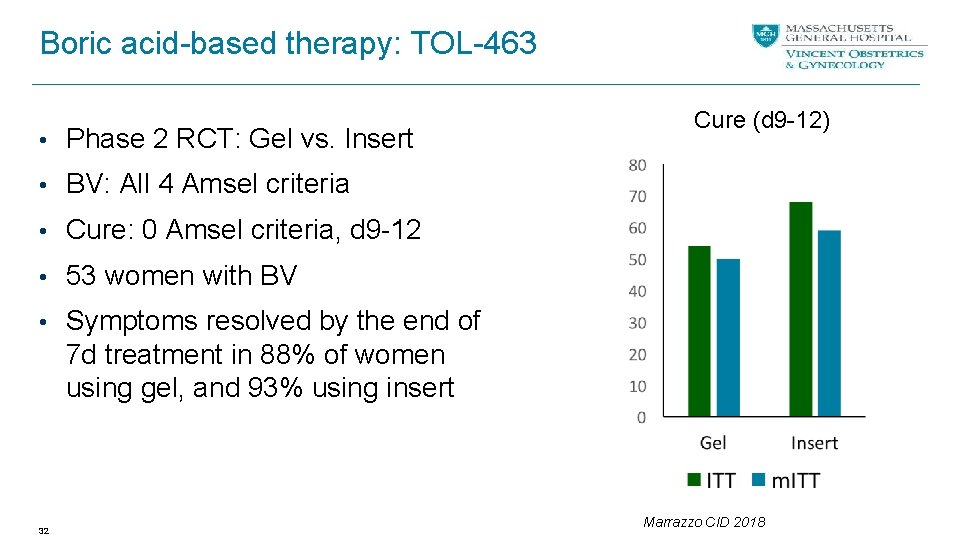
Boric acid-based therapy: TOL-463 • Phase 2 RCT: Gel vs. Insert Cure (d 9 -12) • BV: All 4 Amsel criteria • Cure: 0 Amsel criteria, d 9 -12 • 53 women with BV • Symptoms resolved by the end of 7 d treatment in 88% of women using gel, and 93% using insert 32 Marrazzo CID 2018

Probiotics - Prevention L. crispatus L. Rhamnosus GR N 125 450 95 215 65 100 49 64 190 250 120 98 Tx 30 d 12 d 5 d var 6 d 10 d+ 6 m 28 d 7 d 7 m 14 dm F/u 30 d 30 d 60 d 14 d 30 d 28 d 60 d 120 d Route PO V V V PO V
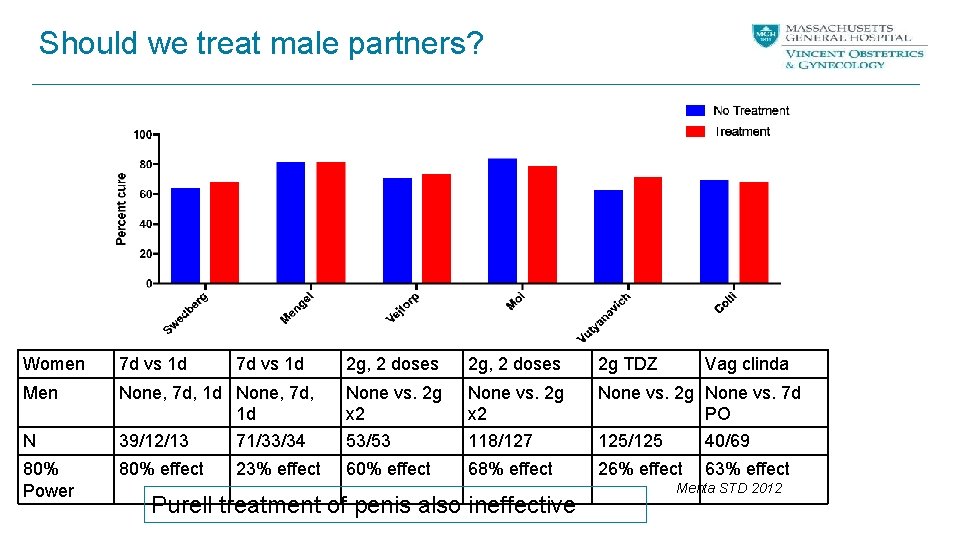
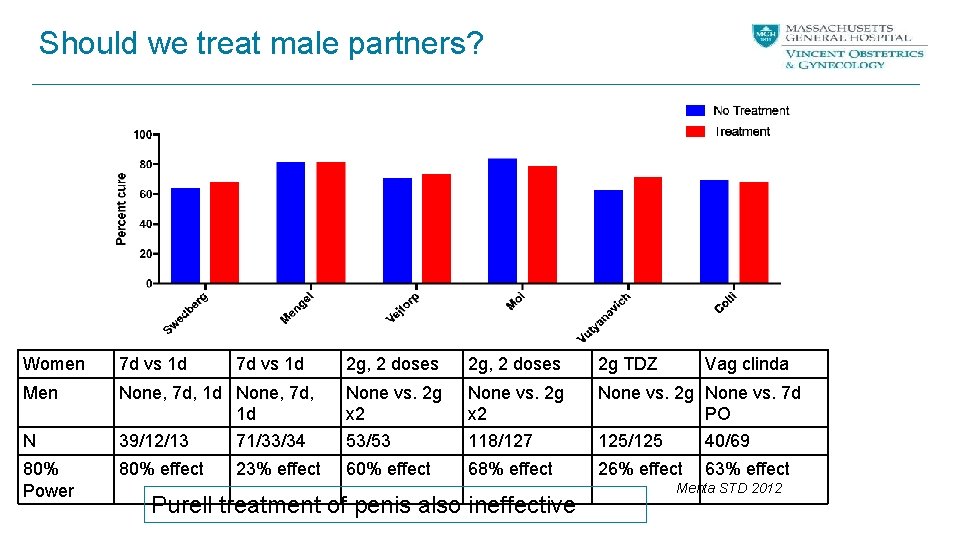
Should we treat male partners? Women 7 d vs 1 d Men N 80% Power 7 d vs 1 d 2 g, 2 doses 2 g TDZ None, 7 d, 1 d 39/12/13 71/33/34 None vs. 2 g x 2 53/53 None vs. 2 g x 2 118/127 None vs. 2 g None vs. 7 d PO 125/125 40/69 80% effect 68% effect 26% effect 23% effect Purell treatment of penis also ineffective Vag clinda 63% effect Mehta STD 2012
Case 3 CC is a 42 -year-old woman presents with complaints of large amounts of vaginal discharge; some vulvar irritation and some post coital bleeding. She has had two sex partners in the past six months. She uses an IUD for contraception. On exam, she has copious amounts of discharge around introitus, erythema of vaginal walls, petechiae on cervix and bubbles in the nonadherent discharge pooled in posterior vault. No cervical motion tenderness.


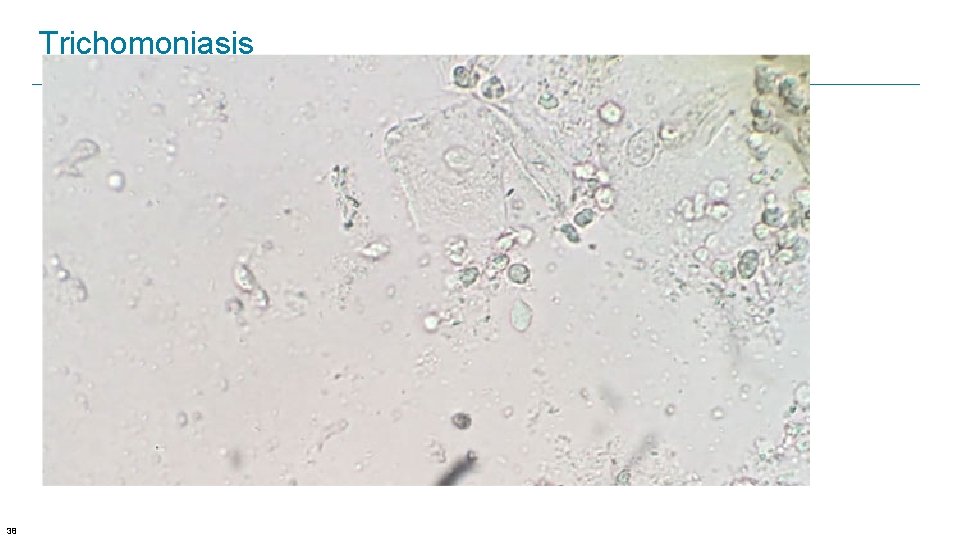
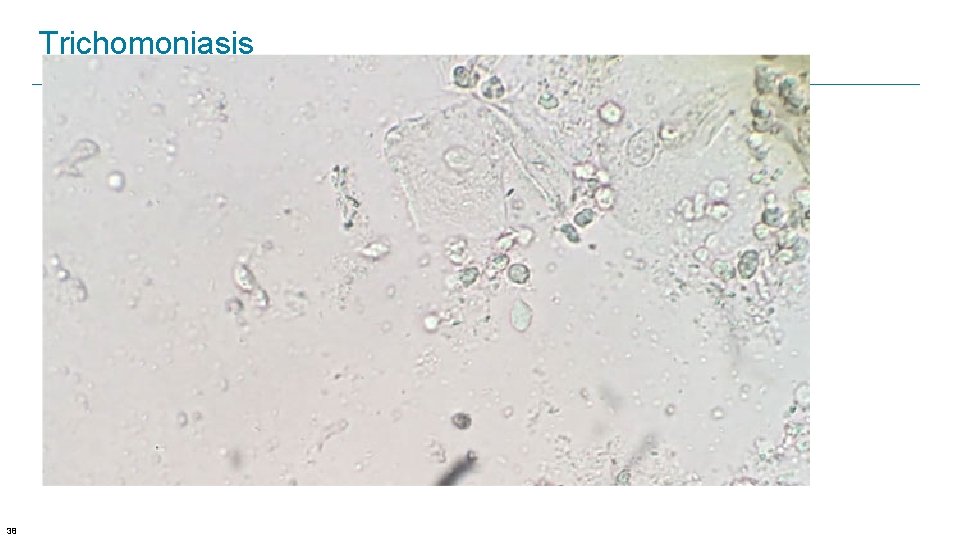
Trichomoniasis 38
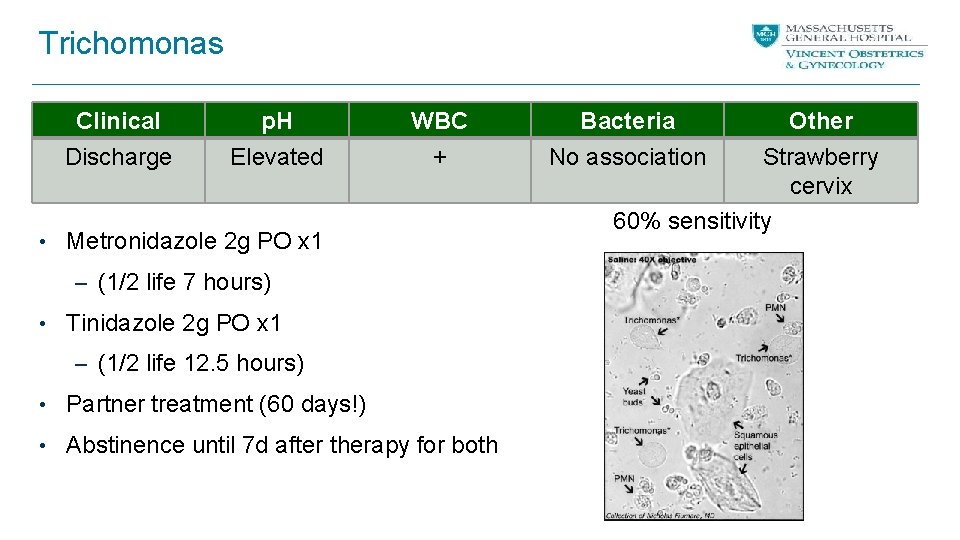
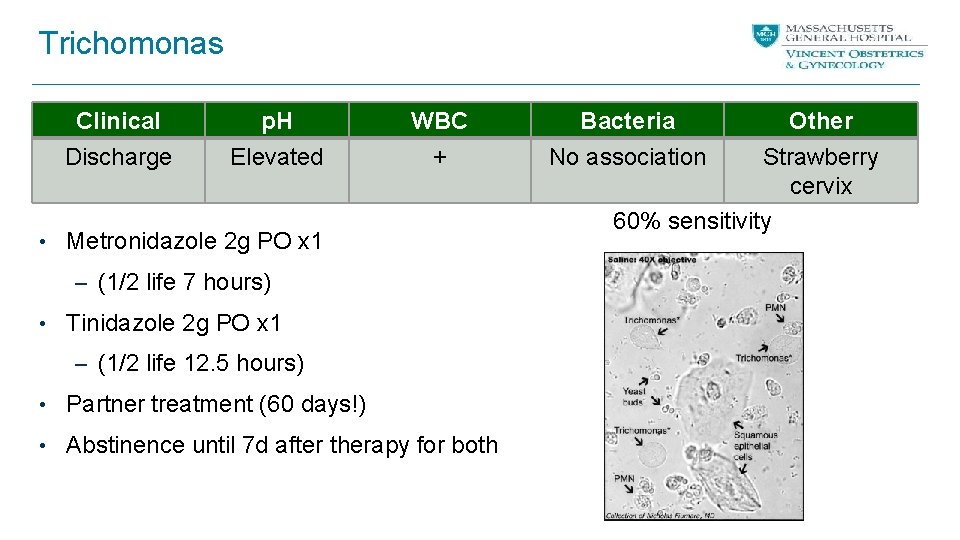
Trichomonas Clinical p. H WBC Bacteria Discharge Elevated + No association • Metronidazole 2 g PO x 1 – (1/2 life 7 hours) • Tinidazole 2 g PO x 1 – (1/2 life 12. 5 hours) • Partner treatment (60 days!) • Abstinence until 7 d after therapy for both Other Strawberry cervix 60% sensitivity

Trichomoniasis in HIV+ women • RCT of HIV+ women with trichomoniasis – 2833 screened: 16. 9% + for trich – 270 randomized to either 2 g x 1 or 500 mg BID x 7 d – 92% African American Treatment Failure or Recurrence Single dose 7 day RR TOC (8 -12 d) 21/125 (16. 8%) 11/130 (8. 5%) 0. 5 (0. 25, 1. 0) 3 month f/u 19/79 (24. 1%) 8/73 (11%) 0. 46 (0. 21, 0. 98) Kissinger et al JAIDS 2010
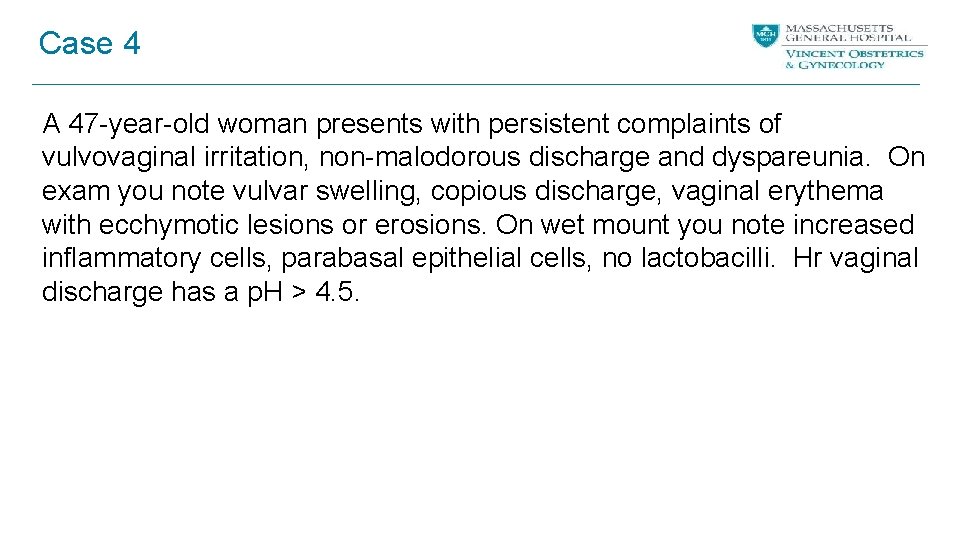
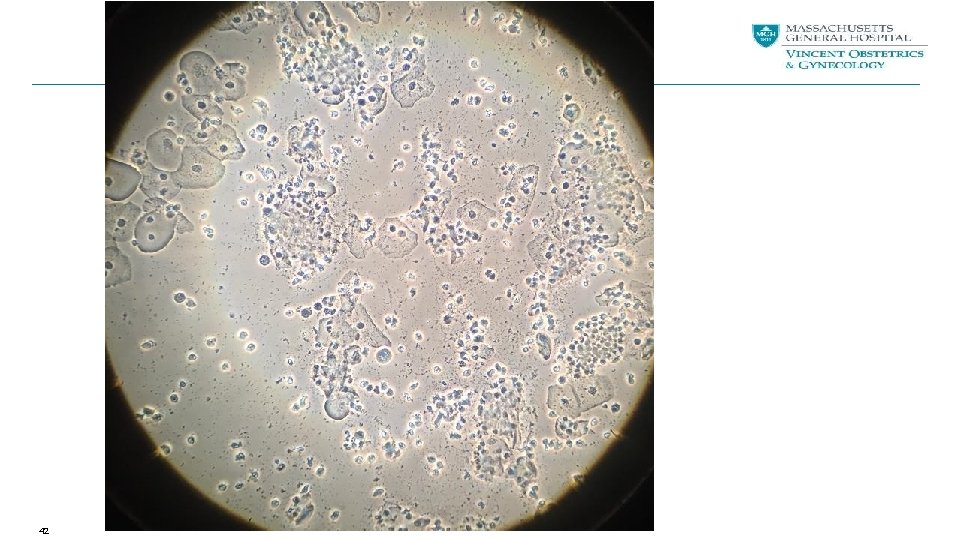
Case 4 A 47 -year-old woman presents with persistent complaints of vulvovaginal irritation, non-malodorous discharge and dyspareunia. On exam you note vulvar swelling, copious discharge, vaginal erythema with ecchymotic lesions or erosions. On wet mount you note increased inflammatory cells, parabasal epithelial cells, no lactobacilli. Hr vaginal discharge has a p. H > 4. 5.
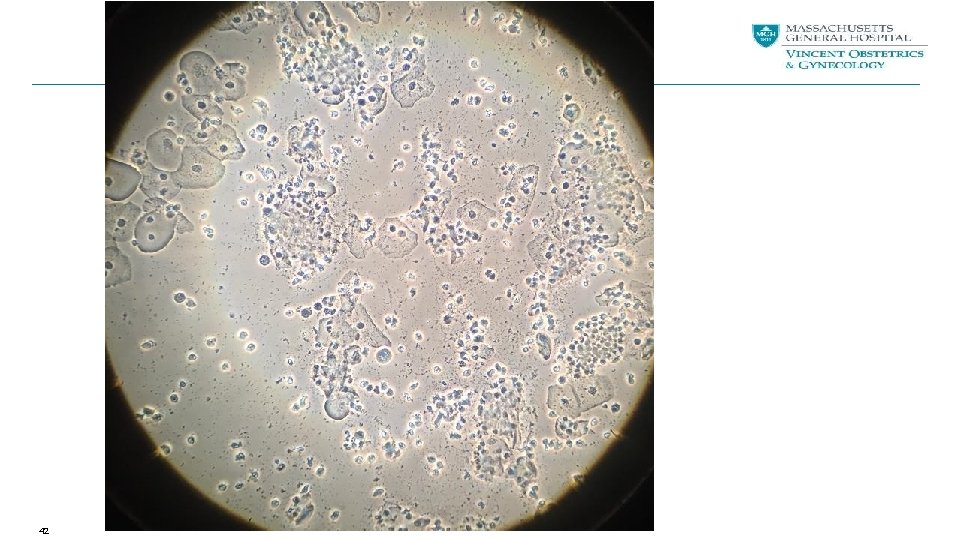
42
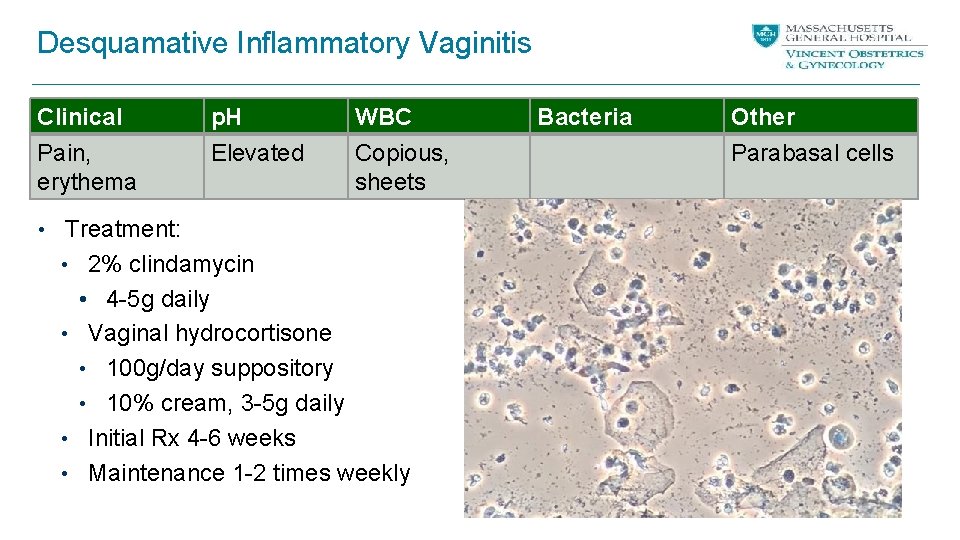
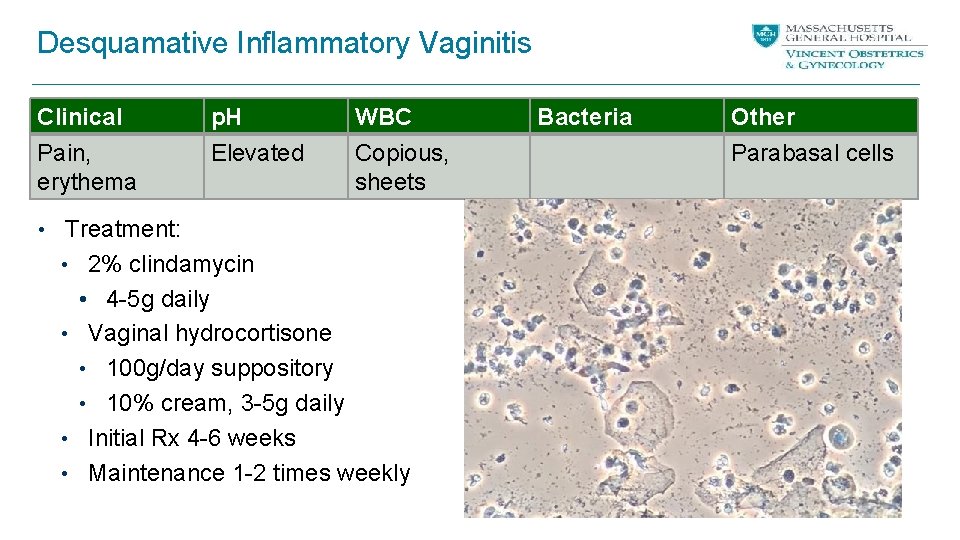
Desquamative Inflammatory Vaginitis Clinical Pain, erythema p. H Elevated WBC Copious, sheets • Treatment: • 2% clindamycin • 4 -5 g daily • Vaginal hydrocortisone • 100 g/day suppository • 10% cream, 3 -5 g daily • Initial Rx 4 -6 weeks • Maintenance 1 -2 times weekly Bacteria Other Parabasal cells

Vaginal discomfort NOS • • • Discharge Irritation Burning Itching Pain with sex Vulvodynia

Thank you • Vincent Center for Reproductive Biology • David Eschenbach • Jeanne Marrazzo • Lisa Manhart • Ina Park • Katherine Hsu • Rochelle Walensky