Introduction and Approach to Transplantation Pathology Disclosures Omnyx


- Slides: 20
Introduction and Approach to Transplantation Pathology
Disclosures • Omnyx – Clinical development team and potential for eventual equity shares • Wyeth - Consultant • Bristol-Myers Squibb - Consultant • DCL/Novartis - Consultant
Transplant Pathology General Considerations • Allograft pathology (and reporting) is the same as native organ pathology, except for syndromes unique to the allograft: – – – Preservation/reperfusion injury Rejection Opportunistic viruses Malignancies GVHD • Final diagnosis is based on extensive clinicopathologic diagnosis • More than one insult can contribute to the injury and diagnostic hierarchy should be assigned, if possible. • Pathophysiologic approach usually trumps morphological approach, but combination is best
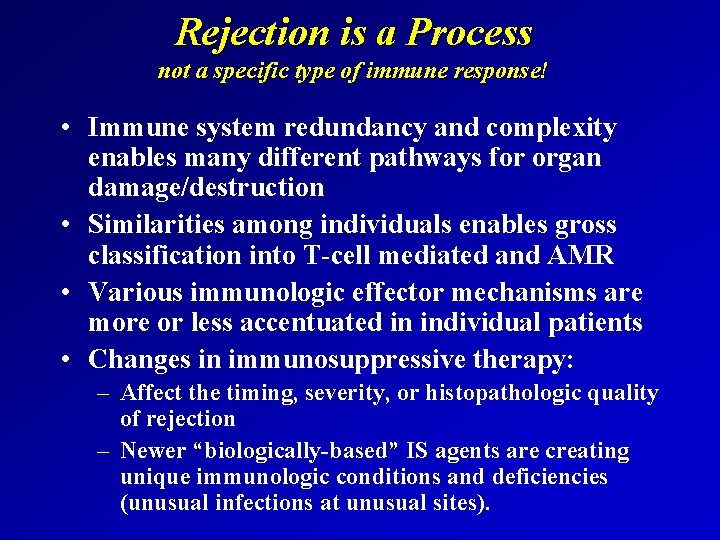
Rejection is a Process not a specific type of immune response! • Immune system redundancy and complexity enables many different pathways for organ damage/destruction • Similarities among individuals enables gross classification into T-cell mediated and AMR • Various immunologic effector mechanisms are more or less accentuated in individual patients • Changes in immunosuppressive therapy: – Affect the timing, severity, or histopathologic quality of rejection – Newer “biologically-based” IS agents are creating unique immunologic conditions and deficiencies (unusual infections at unusual sites).
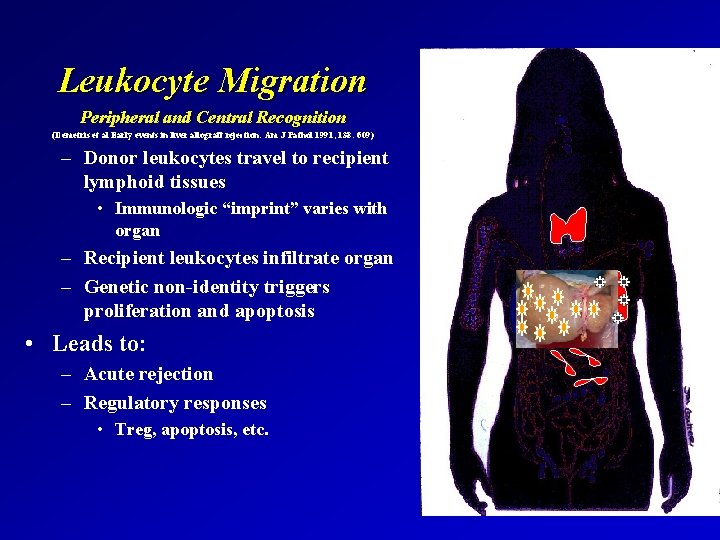
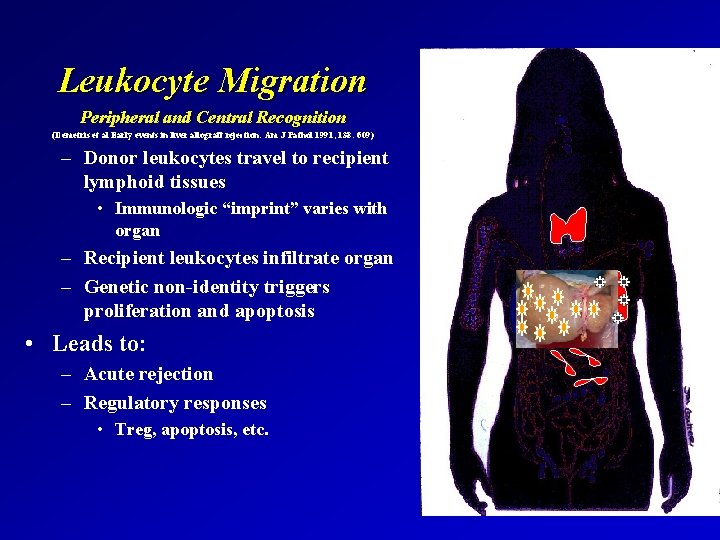
Leukocyte Migration Peripheral and Central Recognition (Demetris et al Early events in liver allograft rejection: Am J Pathol 1991; 138: 609) – Donor leukocytes travel to recipient lymphoid tissues • Immunologic “imprint” varies with organ – Recipient leukocytes infiltrate organ – Genetic non-identity triggers proliferation and apoptosis • Leads to: – Acute rejection – Regulatory responses • Treg, apoptosis, etc.
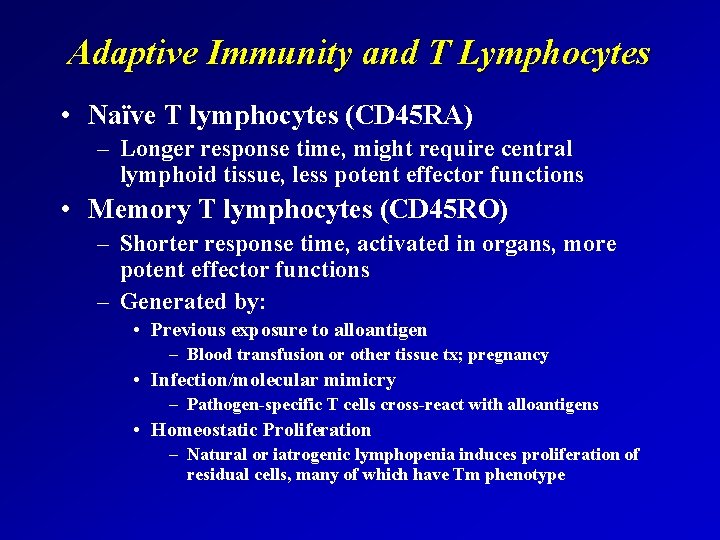
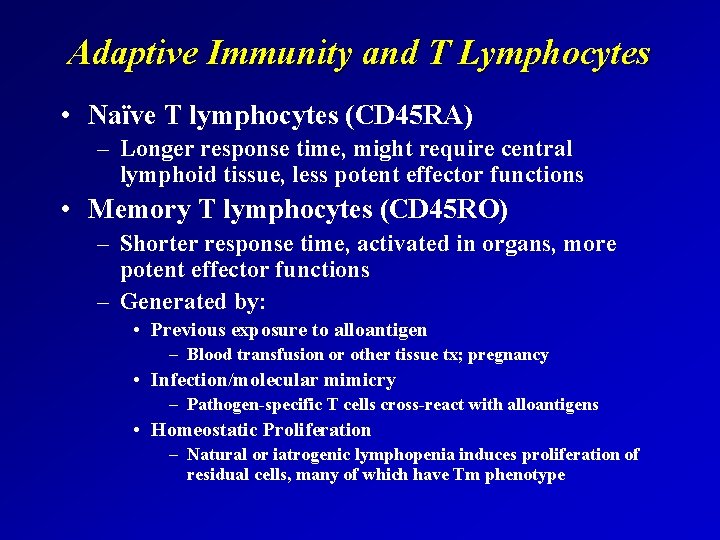
Adaptive Immunity and T Lymphocytes • Naïve T lymphocytes (CD 45 RA) – Longer response time, might require central lymphoid tissue, less potent effector functions • Memory T lymphocytes (CD 45 RO) – Shorter response time, activated in organs, more potent effector functions – Generated by: • Previous exposure to alloantigen – Blood transfusion or other tissue tx; pregnancy • Infection/molecular mimicry – Pathogen-specific T cells cross-react with alloantigens • Homeostatic Proliferation – Natural or iatrogenic lymphopenia induces proliferation of residual cells, many of which have Tm phenotype

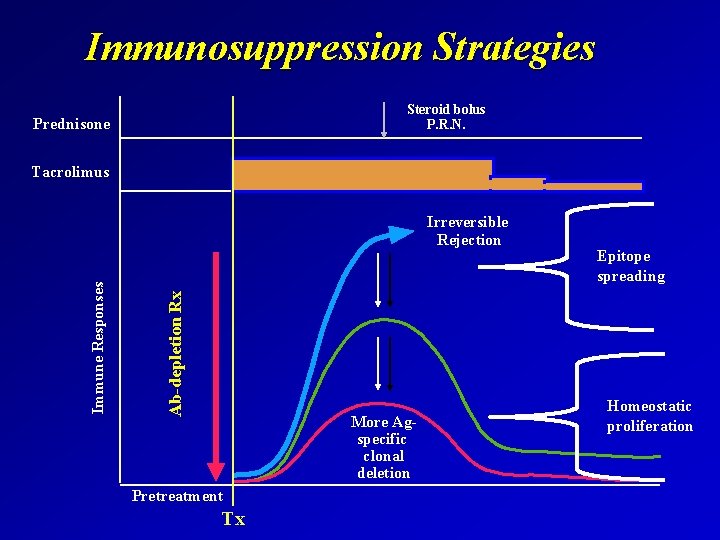
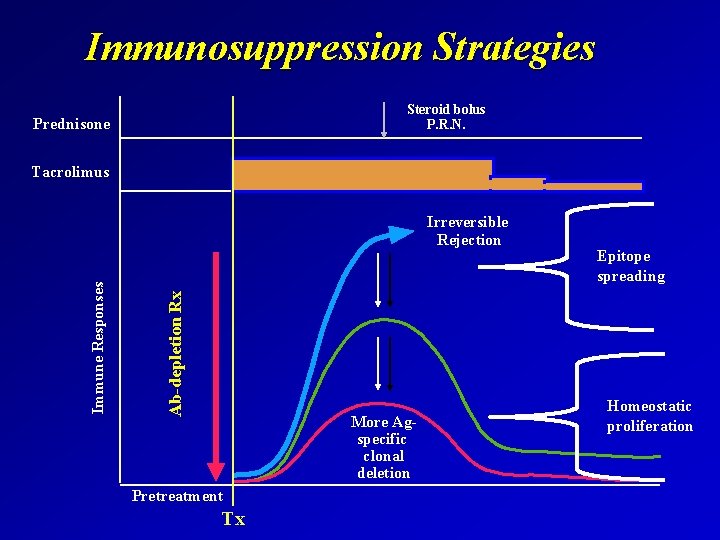
Immunosuppression Strategies Steroid bolus P. R. N. Prednisone Tacrolimus Ab-depletion Rx Immune Responses Irreversible Rejection More Agspecific clonal deletion Pretreatment Tx Epitope spreading Homeostatic proliferation
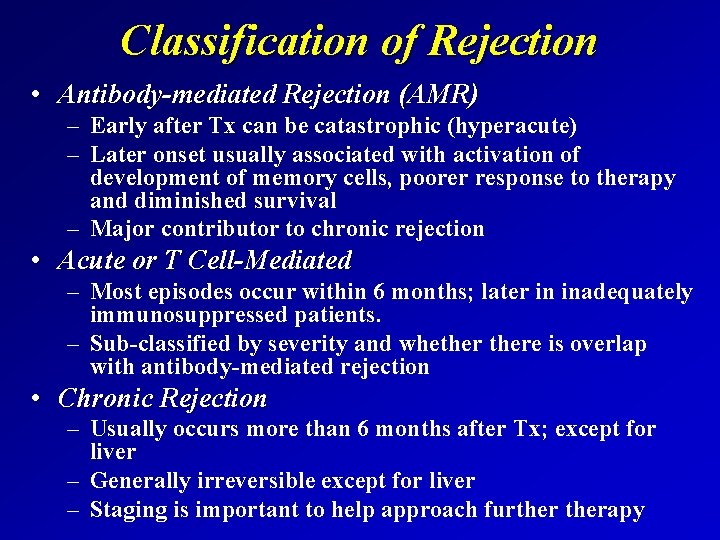
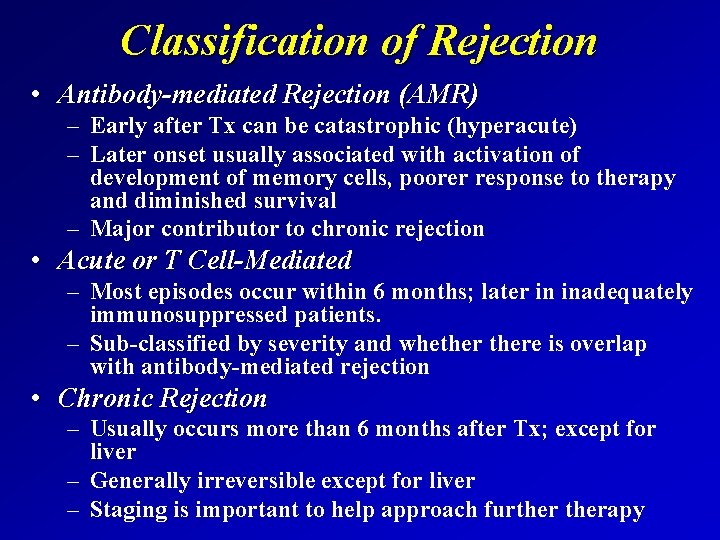
Classification of Rejection • Antibody-mediated Rejection (AMR) – Early after Tx can be catastrophic (hyperacute) – Later onset usually associated with activation of development of memory cells, poorer response to therapy and diminished survival – Major contributor to chronic rejection • Acute or T Cell-Mediated – Most episodes occur within 6 months; later in inadequately immunosuppressed patients. – Sub-classified by severity and whethere is overlap with antibody-mediated rejection • Chronic Rejection – Usually occurs more than 6 months after Tx; except for liver – Generally irreversible except for liver – Staging is important to help approach furtherapy

Antibody-Mediated Rejection • Antibodies may be preformed or develop after transplantation – Anti-endothelial cells most deleterious (ABO, lymphocytotoxic) – Susceptibility = kidney > heart > intestine > lung > liver – Increased risk in multiparous women, previous blood, or tissue exposure • Recognized histopathologically as microvascular endothelial “activation”, leukocyte margination, injury and congestion, lymphocytic and necrotizing arteritis • Definitive diagnosis usually requires clinical dysfunction, typical histopathologic changes and evidence of antibody-mediate injury and circulating anti-donor antibodies.
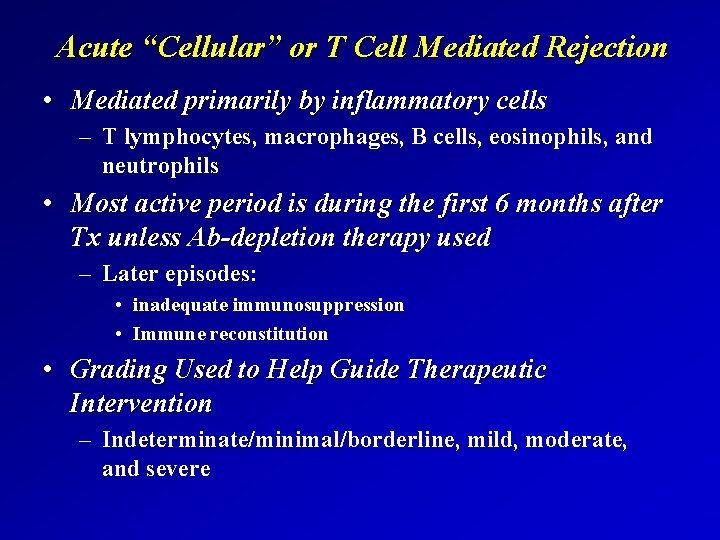
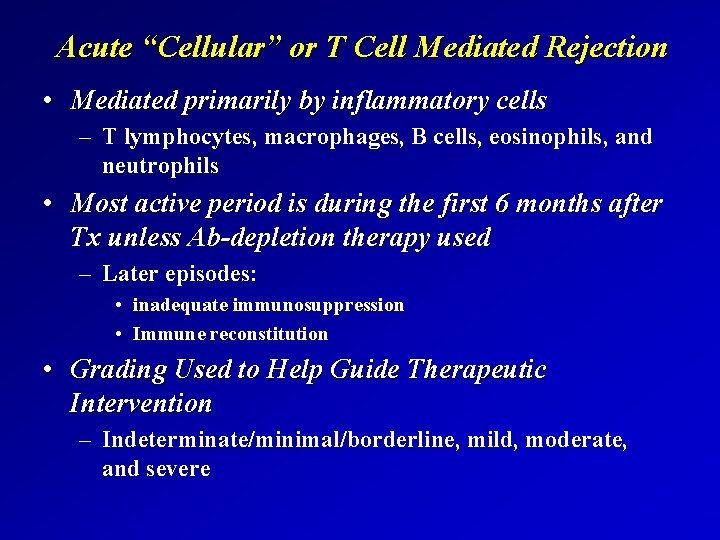
Acute “Cellular” or T Cell Mediated Rejection • Mediated primarily by inflammatory cells – T lymphocytes, macrophages, B cells, eosinophils, and neutrophils • Most active period is during the first 6 months after Tx unless Ab-depletion therapy used – Later episodes: • inadequate immunosuppression • Immune reconstitution • Grading Used to Help Guide Therapeutic Intervention – Indeterminate/minimal/borderline, mild, moderate, and severe
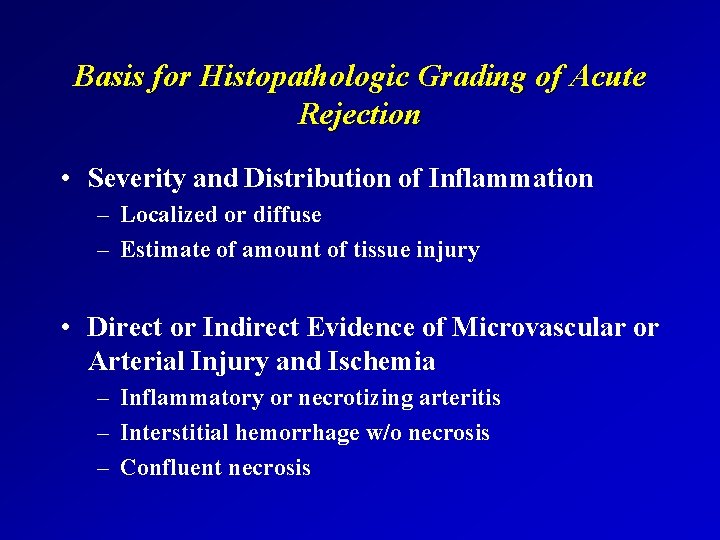
Basis for Histopathologic Grading of Acute Rejection • Severity and Distribution of Inflammation – Localized or diffuse – Estimate of amount of tissue injury • Direct or Indirect Evidence of Microvascular or Arterial Injury and Ischemia – Inflammatory or necrotizing arteritis – Interstitial hemorrhage w/o necrosis – Confluent necrosis
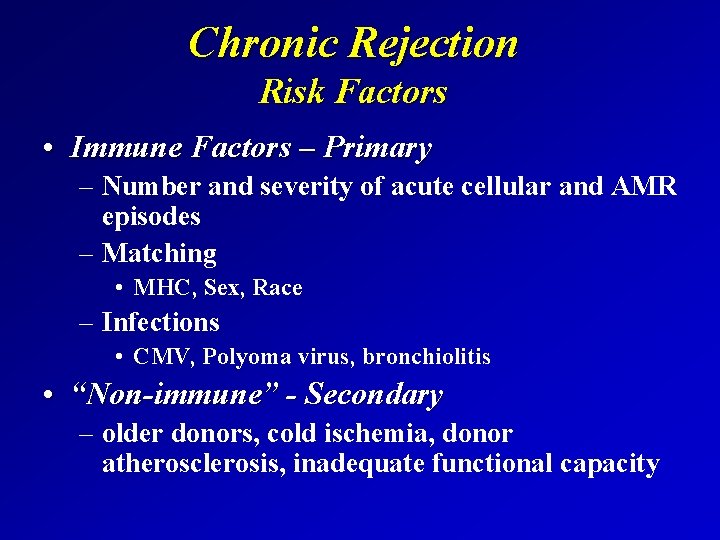
Chronic Rejection Risk Factors • Immune Factors – Primary – Number and severity of acute cellular and AMR episodes – Matching • MHC, Sex, Race – Infections • CMV, Polyoma virus, bronchiolitis • “Non-immune” - Secondary – older donors, cold ischemia, donor atherosclerosis, inadequate functional capacity
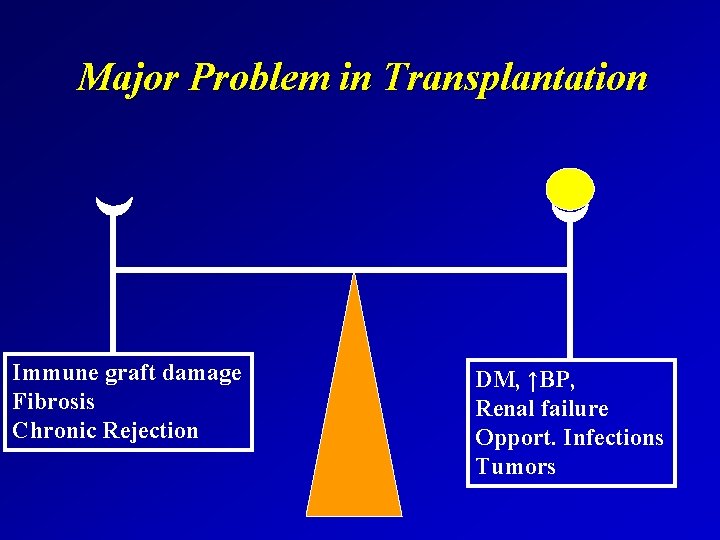
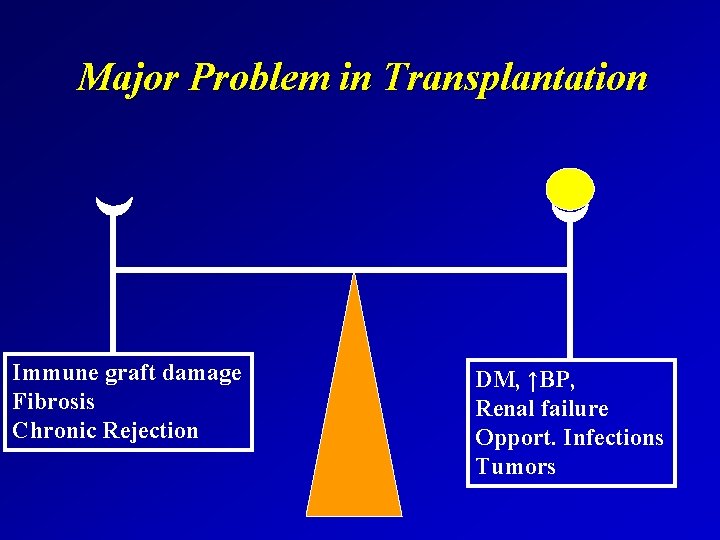
Major Problem in Transplantation Immune graft damage Fibrosis Chronic Rejection DM, ↑BP, Renal failure Opport. Infections Tumors
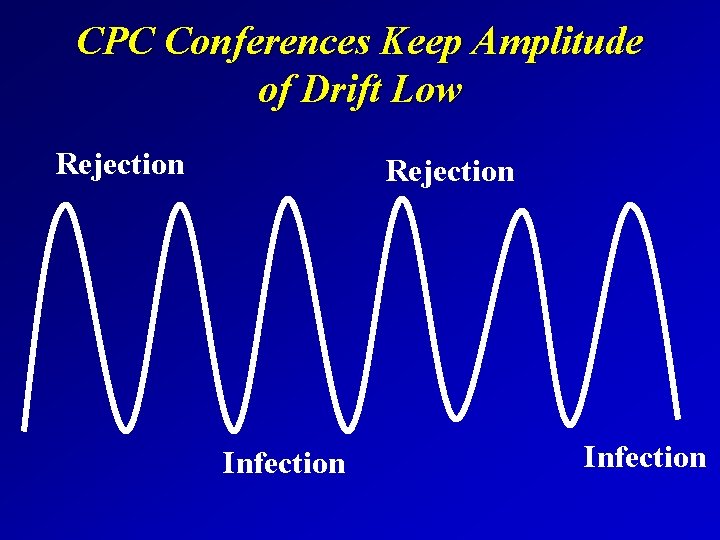
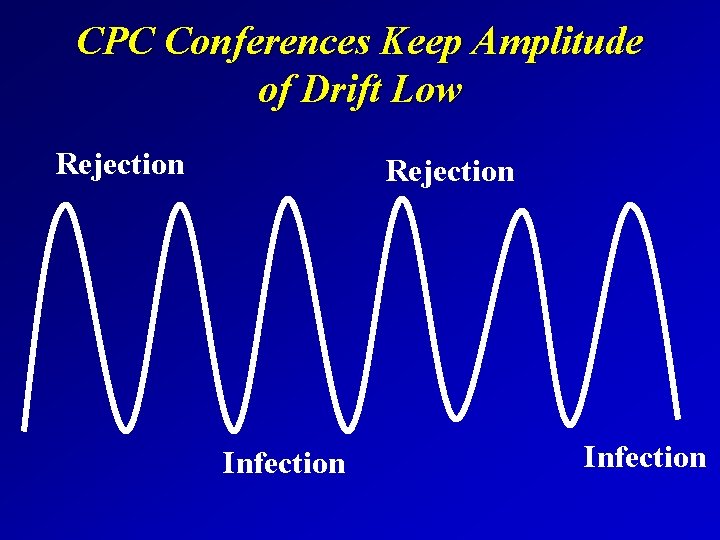
CPC Conferences Keep Amplitude of Drift Low Rejection Infection
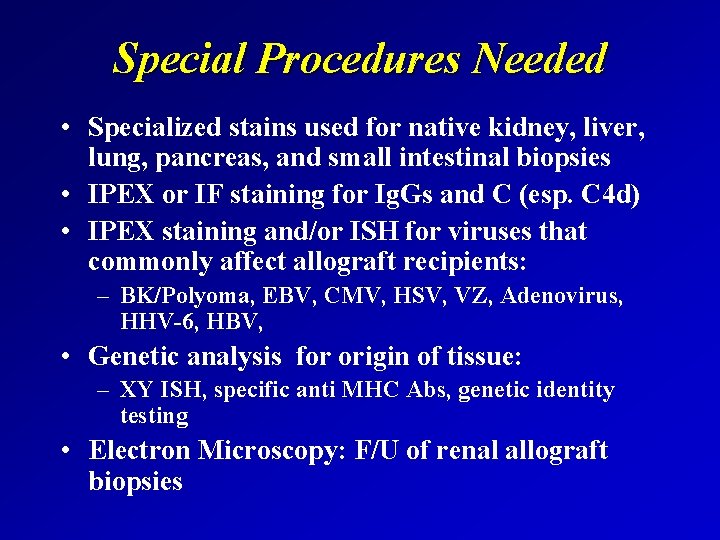
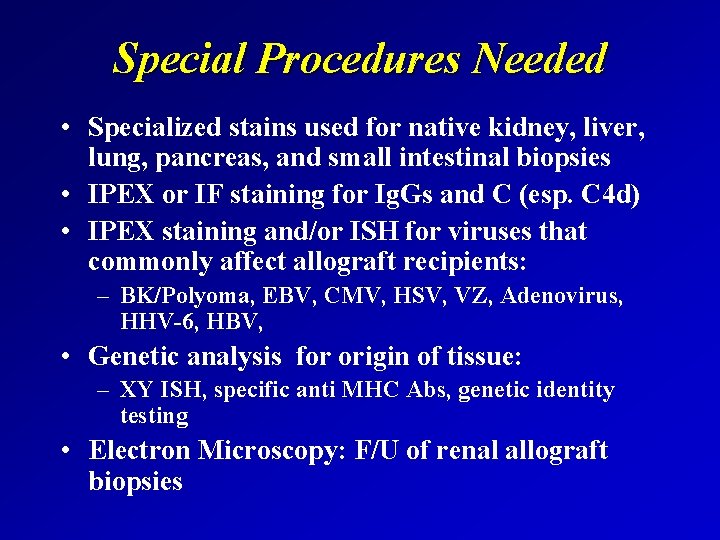
Special Procedures Needed • Specialized stains used for native kidney, liver, lung, pancreas, and small intestinal biopsies • IPEX or IF staining for Ig. Gs and C (esp. C 4 d) • IPEX staining and/or ISH for viruses that commonly affect allograft recipients: – BK/Polyoma, EBV, CMV, HSV, VZ, Adenovirus, HHV-6, HBV, • Genetic analysis for origin of tissue: – XY ISH, specific anti MHC Abs, genetic identity testing • Electron Microscopy: F/U of renal allograft biopsies
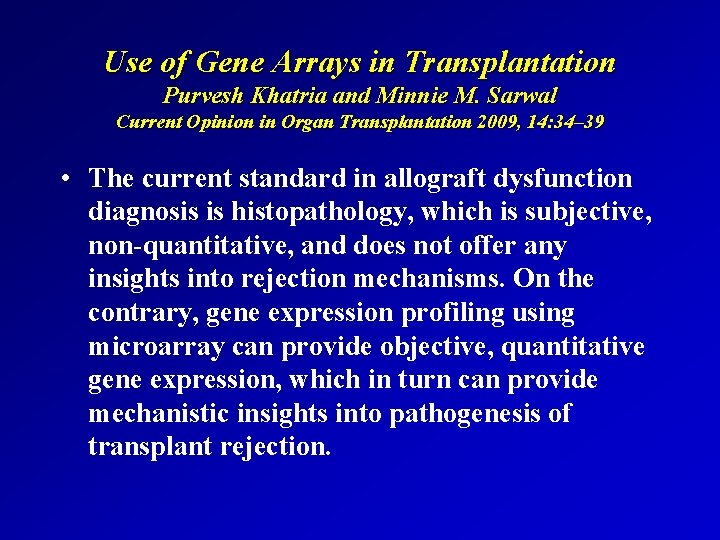
Use of Gene Arrays in Transplantation Purvesh Khatria and Minnie M. Sarwal Current Opinion in Organ Transplantation 2009, 14: 34– 39 • The current standard in allograft dysfunction diagnosis is histopathology, which is subjective, non-quantitative, and does not offer any insights into rejection mechanisms. On the contrary, gene expression profiling using microarray can provide objective, quantitative gene expression, which in turn can provide mechanistic insights into pathogenesis of transplant rejection.
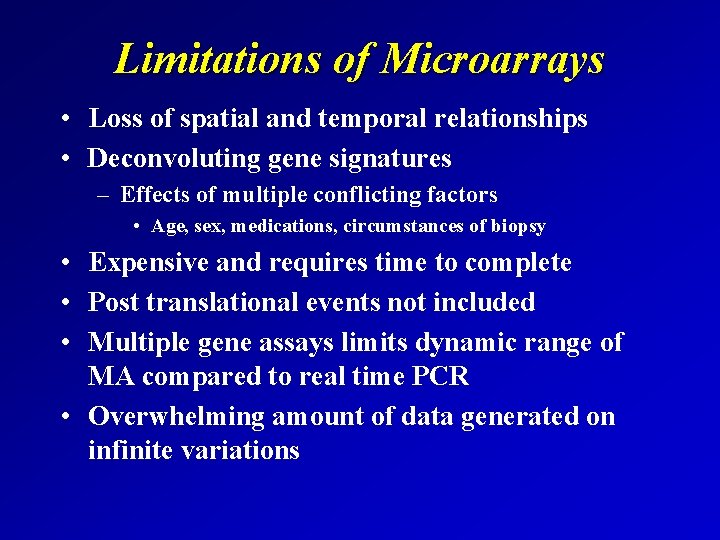
Limitations of Microarrays • Loss of spatial and temporal relationships • Deconvoluting gene signatures – Effects of multiple conflicting factors • Age, sex, medications, circumstances of biopsy • Expensive and requires time to complete • Post translational events not included • Multiple gene assays limits dynamic range of MA compared to real time PCR • Overwhelming amount of data generated on infinite variations
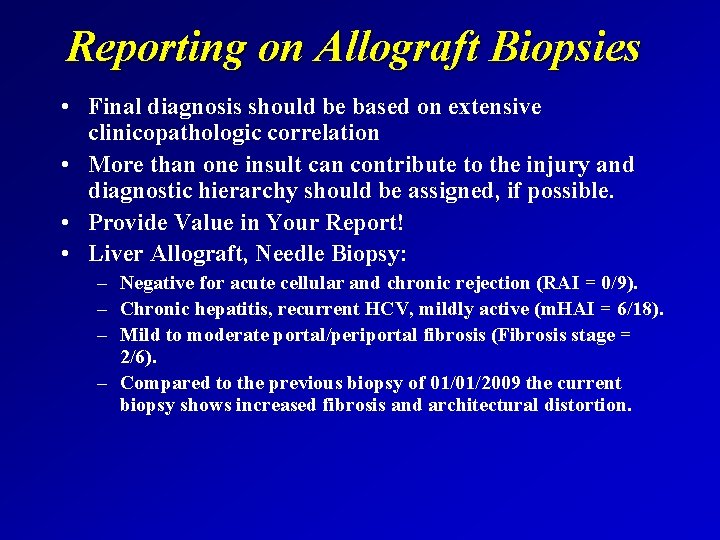
Reporting on Allograft Biopsies • Final diagnosis should be based on extensive clinicopathologic correlation • More than one insult can contribute to the injury and diagnostic hierarchy should be assigned, if possible. • Provide Value in Your Report! • Liver Allograft, Needle Biopsy: – Negative for acute cellular and chronic rejection (RAI = 0/9). – Chronic hepatitis, recurrent HCV, mildly active (m. HAI = 6/18). – Mild to moderate portal/periportal fibrosis (Fibrosis stage = 2/6). – Compared to the previous biopsy of 01/01/2009 the current biopsy shows increased fibrosis and architectural distortion.
Conclusions • Antigen migration/lymphoid trafficking early after transplantation important concept • Working knowledge of immunologic events and mechanisms greatly assists clinical practice and research • Final interpretation should be based on complete clinicopathologic correlation • Specialized staining procedures needed for complete specimen evaluation • Reporting should be complete, hierarchical, if needed, and answer clinical questions/concerns
 Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard transplantation
Patrick evrard transplantation Calque examples
Calque examples Types of transplantation
Types of transplantation Stem cell or bone marrow transplantation thailand
Stem cell or bone marrow transplantation thailand Disclosure slide
Disclosure slide Voluntary disclosures meaning
Voluntary disclosures meaning No disclosures slide
No disclosures slide Website disclosures under companies act 2013
Website disclosures under companies act 2013 When becomes weakness
When becomes weakness Introduction and importance of seed pathology
Introduction and importance of seed pathology Difference between datagram and virtual circuit approach
Difference between datagram and virtual circuit approach Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Waterfall approach marketing example
Waterfall approach marketing example Multiple conflict
Multiple conflict Bandura's reciprocal determinism
Bandura's reciprocal determinism Research approach definition
Research approach definition Diagram for traditional approach
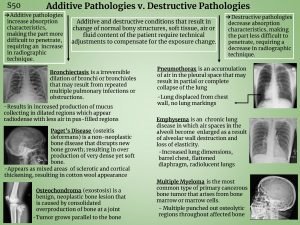
Diagram for traditional approach Additive pathology in radiography examples
Additive pathology in radiography examples