Integrating Nutrition Assessment Counselling and Support into Health

- Slides: 32

Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery Training Course for Facility-Based Health Providers Session� 2. 4 Feeding � Children During Illness, Recovery, and Other Difficult Circumstances.
Session Objectives By the end of the session, participants will be able to: 1. Explain the importance of feeding children during illness and recovery 2. Discuss feeding practices for children during illness and recovery 3. Discuss feeding options for children in difficult circumstances Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 2
Group Discussion Why may children fail to eat during illness and recovery? Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 3
Group Discussion Why is it important to encourage children to eat during illness and recovery? Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 4
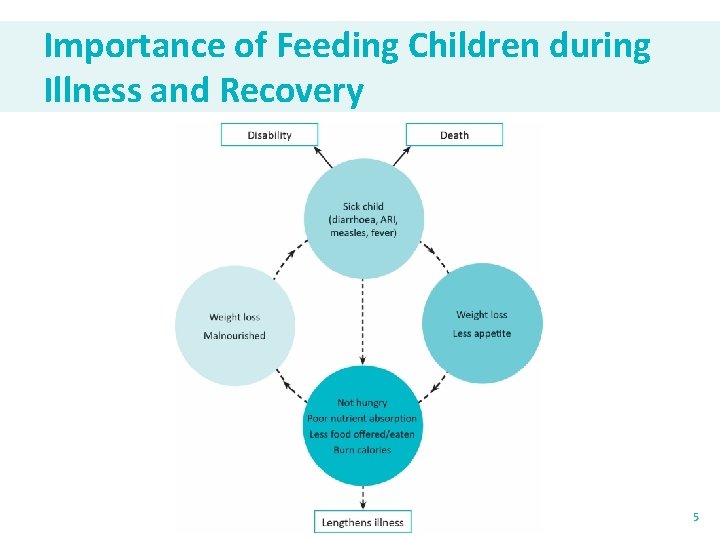
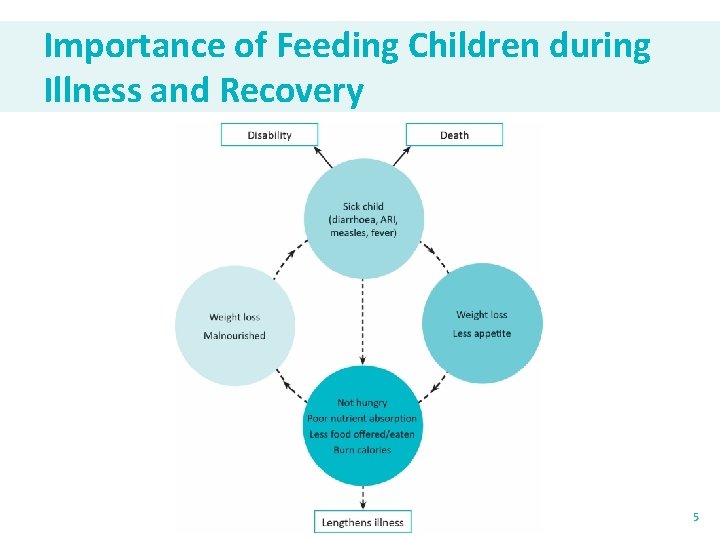
Importance of Feeding Children during Illness and Recovery 5
Brainstorm What are appropriate feeding practices during: • Illness? • Recovery? Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 6
Feeding Practices during Illness • During illness, appetite decreases and desire to breastfeed frequently increases. • Need for fluids also increases. • Goal of feeding during illness: Continue feeding (including breastfeeding) as much or more than before illness, and increase fluid intake. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 7
Feeding Practices during Illness Children under 6 months of age: �Breastfeed more frequently and longer at each feed. �For children who are not breastfed: ◦ Provide their usual breast milk substitute at least every 3 hours. ◦ Give plenty to drink every 1 -2 hours (treated water, rice water, yoghurt drinks—no soda or sweetened drinks). Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 8
Feeding Practices during Illness Children 6 -23 months of age: � Breastfeed more frequently. � Increase fluid intake. ◦ Treated water, coconut or rice water, yoghurt drinks, and other nutritious liquids should be given every 1 -2 hours; avoid sodas and sweetened juice drinks. � Feed the child more frequently with small amounts of nutritious food/drink. � Give them their favorite foods. ◦ Soft and appetizing foods may be most appealing. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 9
Feeding Practices during Illness 6 -23 Months (Cont’d) �Give the child a variety of nutrient-rich foods. �Give mashed foods to ease chewing, swallowing, and digestion. ◦ Do not dilute foods or drinks (milk). �Feed the child slowly, very patiently and in a loving way. ◦ Encourage the child to drink and/or eat, being persistent, but do not force. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 10
Feeding Practices during Illness (Cont’d) �Only use treated water. �Always wash hands with soap (or ash) and clean flowing water before preparing food or feeding the child and before and after tending to the sick child. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 11
Feeding Practices during Recovery �During recovery, appetite increases, and children need extra nutrients to ‘catch-up’ lost growth. �Goal of feeding during recovery: Provide more food than normal. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 12
Five Feeding ‘Extras’ during Recovery 1. Give the child extra breastfeeds. 2. Feed the child an extra meal (and extra snacks). 3. Give the child an extra amount of food. 4. Use extra nutrient-rich foods. 5. Feed the child with extra patience and love. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 13
Feeding Children in Difficult Circumstances Includes: �Low-birth-weight (LBW) infants (< 2, 500 g) ◦ Can suckle effectively ◦ Cannot suckle effectively �HIV-exposed infants/children �HIV-positive children �Orphaned/abandoned children and children in emergencies Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 14
Feeding Children in Difficult Circumstances Feeding LBW infants: �Term LBW (37 weeks or more gestation) ◦ Usually able to suckle effectively immediately after birth �Preterm LBW (< 37 weeks) ◦ May not be able to suckle effectively ◦ Depending on gestational age, may need to be fed expressed breast milk by cup/spoon or nasogastric tube Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 15
Feeding Children in Difficult Circumstances Term LBW (can suckle): � Assist the mother in placing infant in skin-to-skin contact and let the baby try to suckle as soon as possible after delivery. ◦ Ensure correct positioning and attachment i. e. , under arm and cross cradle may be easier for small babies. � LBW babies tend to pause while breastfeeding and may take a long time to nurse. ◦ Do not remove them from the breast immediately when they stop feeding. � Allow baby to suckle every three hours or on demand more frequently. ◦ LBW babies may want to feed more frequently, though they may tire more easily. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 16
Feeding Children in Difficult Circumstances Preterm LBW (32 -36 weeks gestation) (cannot suckle): �May need to be partially/fully fed expressed breast milk by cup or spoon until full breastfeeding can be established. �Feeds can be started when infant is clinically stable, if possible within the first hour of life. ◦ On demand, and at least every 3 hours ◦ Smaller the infant = more frequent feeds �Mother should continue putting the baby at the breast to allow the baby to lick and suckle to stimulate breastfeeding. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 17
Feeding Children in Difficult Circumstances Preterm LBW (32 -36 weeks gestation) (cannot suckle) (cont’d): �Rest of the feed provided by cup. �Gradually reduce amount of breast milk by cup as baby starts to suckle well. �Ensure skin-to-skin contact between mother and baby. �Ensure good hygiene, monitor for infections, and provide early treatment. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 18
Feeding Children in Difficult Circumstances Preterm LBW (< 32 weeks gestation) (cannot suckle): � Usually need to be fed by gastric tube in a health facility at first. � Give the baby expressed breast milk (if possible from the baby’s mother), starting with 60 ml/kg body weight per day divided into 8 -12 feeds per day, given every 2 -3 hours. � Increase the daily feed volume by 10 to 20 ml/kg per day over 7 days up to 160 ml/kg/day. � After 7 days, if the infant is still receiving breast milk by gastric tube or cup, increase the quantity given by 20 ml/kg each day until the infant is receiving 180 ml/kg/day. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 19
Feeding Children in Difficult Circumstances Preterm LBW (< 32 weeks gestation) (cannot suckle): � Mother should put the baby at the breast as soon as baby is well enough, to allow the baby to lick and suckle to stimulate breastfeeding. � Encourage skin-to-skin contact. � Amount of expressed breast milk given by gastric tube or cup may be gradually reduced as breastfeeding is established. � Important to record and check the baby’s 24 -hour intake and weigh infant regularly. � Ensure good hygiene, monitor for infection, and provide early treatment. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 20
Feeding Children in Difficult Circumstances Feeding HIV-exposed infants: � Need to balance risk of HIV transmission during breastfeeding with risk of death from malnutrition, diarrhoea, pneumonia from not breastfeeding. � Current evidence indicates that exclusive breastfeeding and the use of antiretroviral drugs greatly reduce motherto-child transmission (MTCT). � Health workers should counsel women during pregnancy on benefits and management of breastfeeding, MTCT, and the importance of adhering to antiretroviral (ARV) regimen. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 21
Feeding Children in Difficult Circumstances Feeding HIV-exposed infants/children: �Start ARV treatment during pregnancy. �Start the baby on Nevirapine (NVP) prophylaxis from birth; test the infant for HIV infection by 6 weeks of age. �Start breastfeeding within 1 hour of birth for all infants. �Exclusively breastfeed all infants from 0– 6 months. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 22
Feeding Children in Difficult Circumstances Feeding HIV-exposed infants/children (cont’d) � Give complementary foods to all children starting at 6 months of age. � For HIV-positive infants: ◦ Continue breastfeeding for 2 years or beyond. � For HIV-negative infants: ◦ Continue breastfeeding until the infant is 12 months. ◦ After 12 months, breastfeeding should be stopped only if nutritionally adequate and safe diet which includes source of milk can be provided. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 23
Feeding Children in Difficult Circumstances Feeding HIV-positive children �More vulnerable to malnutrition, growth failure and progression of HIV infection if not appropriately fed �Energy needs of HIV-positive children are greater than needs of noninfected children of their age ◦ Asymptomatic: 10% more ◦ Symptomatic: 20 -30% more ◦ Symptomatic and losing weight: 50 -100% more Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 24
Feeding Children in Difficult Circumstances Feeding HIV-positive children (cont’d) At the health facility, health workers should: � Counsel the caregiver on appropriate feeding practices, including the amount and variety of foods � Ensure the caregiver receives education on good hygiene and food preparation � Encourage the caregiver to use essential child services (immunization, vitamin A supplementation, deworming, use of insecticide-treated nets) � Identify community support services for nutrition and refer caregivers to them � Regularly monitor the child’s growth by taking and plotting weight and MUAC � Ensure early referral of children with growth faltering to appropriate counseling, or nutrition care and support Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 25
Feeding Children in Difficult Circumstances Feeding children who are orphaned, abandoned, or children in emergencies: � Orphaned/abandoned children: ◦ Infants under 6 months usually need to be on replacement feeding, using infant formula. Caregivers should be instructed and follow appropriate and hygienic preparation and use of breast milk substitutes. ◦ At 6 months, these children should receive complementary foods in addition to either infant formula or animal milk. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 26
Feeding Children in Difficult Circumstances Children who are orphaned, abandoned, or in emergencies (cont’d) � Children in emergencies: ◦ Greater risk of malnutrition and disease ◦ Recommendations for optimal infant and young child feeding remain the same � Children who are with their mothers should be exclusively breastfed for the first 6 months and then started on complementary feeding using locally-available ingredients as much as possible. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 27
Feeding Children in Difficult Circumstances Children in emergencies (cont’d) � For children who are not able to breastfeed: breast milk substitutes should be procured and distributed as part of the regular inventory of foods and medicines, in quantities only as needed. ◦ Caregivers should be instructed on appropriate and hygienic use and preparation of breast milk substitutes. ◦ Care should be taken to avoid ‘spillover’ of breast milk substitute use among the general population. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 28
Summary �Ill children should continue feeding as much as or more than before illness and increase fluid intake. �ARVs and exclusive breastfeeding greatly reduce MTCT while improving overall chance of infant survival. Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 29
Summary �Counsel caregivers of HIV-exposed children on feeding practices, hygiene, essential health services, and available community services �Monitor child growth and refer for counseling or care as needed �In emergencies, protect and promote breastfeeding and ensure safe and timely complementary feeding �Orphans and children under 6 months in emergencies who are unable to breastfeed under 6 months may need breast milk substitutes; care should be taken to avoid ‘spillover’ Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 30
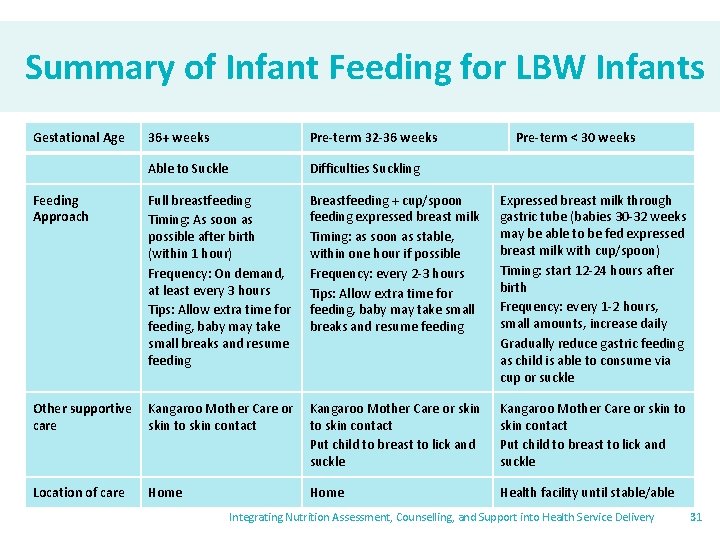
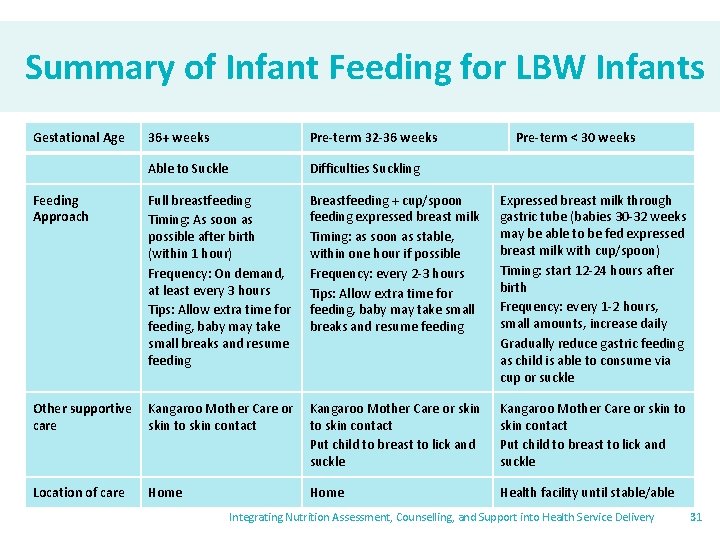
Summary of Infant Feeding for LBW Infants Gestational Age 36+ weeks Pre-term 32 -36 weeks Pre-term < 30 weeks Able to Suckle Difficulties Suckling Feeding Approach Full breastfeeding Timing: As soon as possible after birth (within 1 hour) Frequency: On demand, at least every 3 hours Tips: Allow extra time for feeding, baby may take small breaks and resume feeding Breastfeeding + cup/spoon feeding expressed breast milk Timing: as soon as stable, within one hour if possible Frequency: every 2 -3 hours Tips: Allow extra time for feeding, baby may take small breaks and resume feeding Expressed breast milk through gastric tube (babies 30 -32 weeks may be able to be fed expressed breast milk with cup/spoon) Timing: start 12 -24 hours after birth Frequency: every 1 -2 hours, small amounts, increase daily Gradually reduce gastric feeding as child is able to consume via cup or suckle Other supportive care Kangaroo Mother Care or skin to skin contact Put child to breast to lick and suckle Location of care Home Health facility until stable/able Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 31
Thank you! Questions, additions, and clarifications? Integrating Nutrition Assessment, Counselling, and Support into Health Service Delivery 32
 A firm's strengths that cannot be easily matched
A firm's strengths that cannot be easily matched Strategic management internal assessment
Strategic management internal assessment Tactical communication skills
Tactical communication skills Integrating public health and primary care
Integrating public health and primary care Integrating quotes into an essay
Integrating quotes into an essay Integrating sources into your writing
Integrating sources into your writing Difference between health education and promotion
Difference between health education and promotion Difference between counseling and advice
Difference between counseling and advice Health education and propaganda
Health education and propaganda Enteral parenteral beslenme
Enteral parenteral beslenme Signal words example
Signal words example Chapter 5 lesson 1 health
Chapter 5 lesson 1 health Project title for health and nutrition
Project title for health and nutrition Chapter 55 nutrition and health
Chapter 55 nutrition and health Integrating classification and association rule mining
Integrating classification and association rule mining Integrating factor non exact equations
Integrating factor non exact equations Integrating science and social studies
Integrating science and social studies Integrating qualitative and quantitative methods
Integrating qualitative and quantitative methods Integrating sel and pbis
Integrating sel and pbis Nutrition program planning
Nutrition program planning Abcd in nutrition assessment
Abcd in nutrition assessment How to assess edema
How to assess edema Nutrition focused physical examination
Nutrition focused physical examination Early assessment and support alliance
Early assessment and support alliance Socio-ecological model of nutrition & health
Socio-ecological model of nutrition & health Chapter 10 nutrition for health lesson 2 answer key
Chapter 10 nutrition for health lesson 2 answer key Chapter 10 nutrition for health vocabulary practice
Chapter 10 nutrition for health vocabulary practice Nutrition in primary health care
Nutrition in primary health care Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Positive food
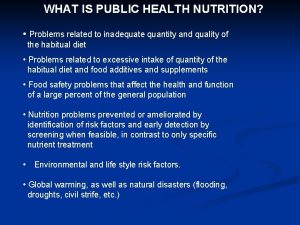
Positive food Public health nutrition problems
Public health nutrition problems Introduction to public health nutrition
Introduction to public health nutrition Chapter 10 lesson 1 the importance of nutrition
Chapter 10 lesson 1 the importance of nutrition