Innovative selfdirected community aged care for older people










- Slides: 29

Innovative self-directed community aged care for older people with complex care needs: A capability-building approach Goetz Ottmann (UCCO/Deakin) Carmel Laragy (RMIT) Jacqui Allen (Deakin)

SDC Model Overview

Observations - Pilot and Trial Phases
Client responses - Level 2 • Some clients were reluctant to ‘rock the boat’ with their agencies • Clients asked for more information about service system • Clients voiced the need for an independent consumer advocate

Client Responses - Level 3 • Client required assistance with budgeting, hiring and firing, information regarding system & eligibility • Training Needs – Computing (email, internet, MS Excel) – Information (written & online) – Care planning & budgeting – Empowerment/Advocacy • Saw the need for a Support Group (phone, email, face-to -face)

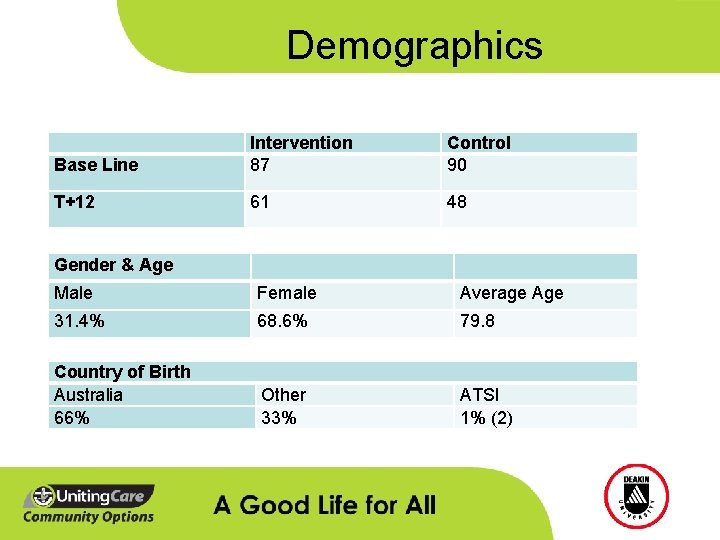
Project Outcomes - Demographics
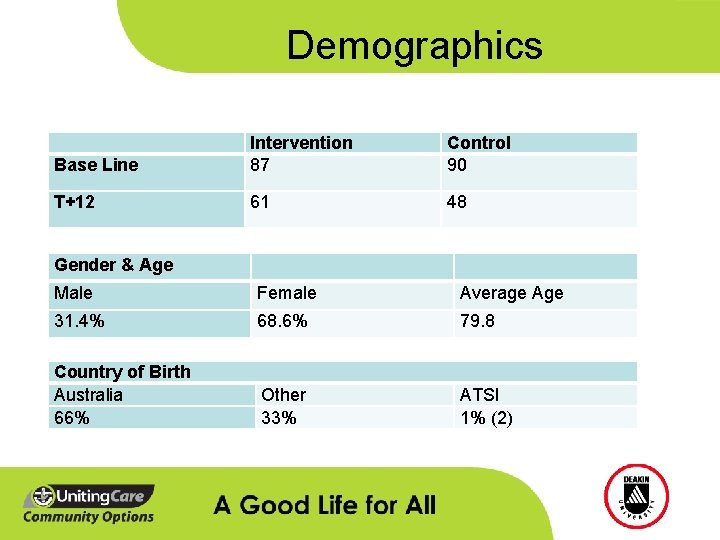
Demographics Base Line Intervention 87 Control 90 T+12 61 48 Gender & Age Male Female Average Age 31. 4% 68. 6% 79. 8 Country of Birth Australia 66% Other 33% ATSI 1% (2)
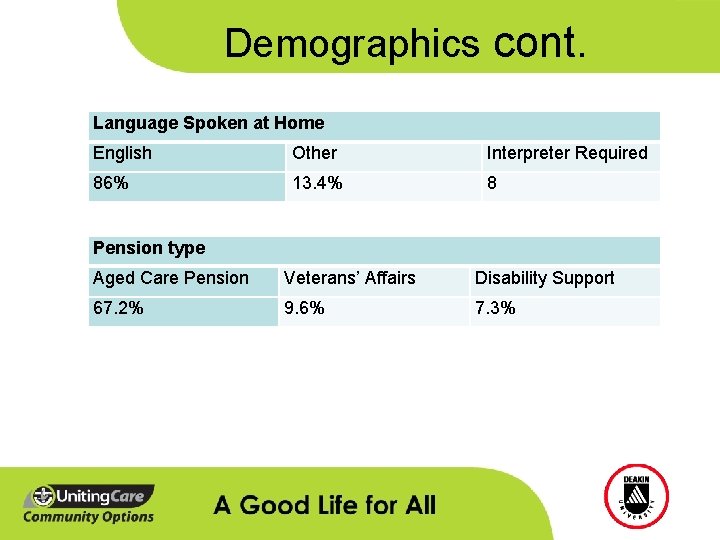
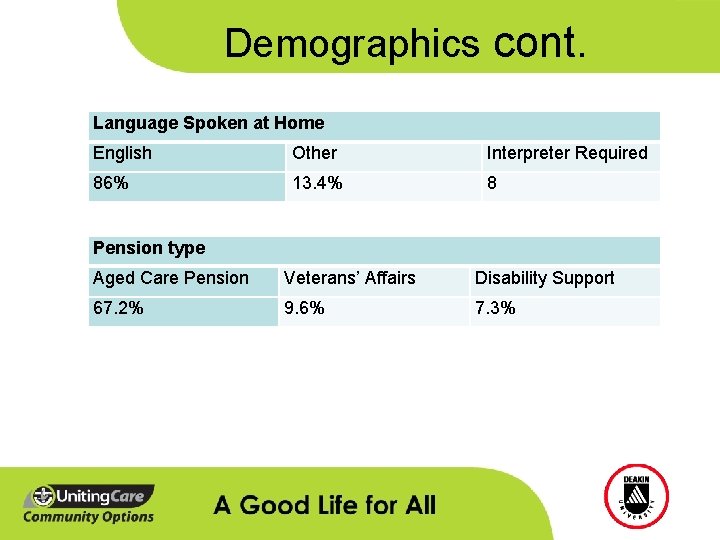
Demographics cont. Language Spoken at Home English Other Interpreter Required 86% 13. 4% 8 Pension type Aged Care Pension Veterans’ Affairs Disability Support 67. 2% 9. 6% 7. 3%
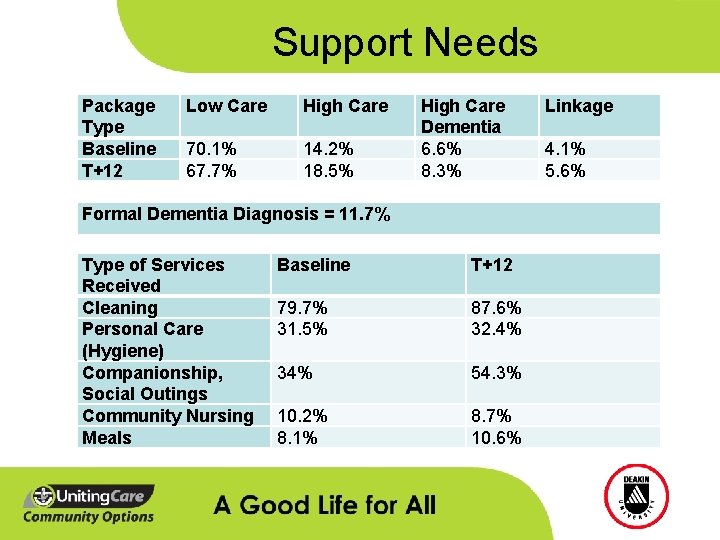
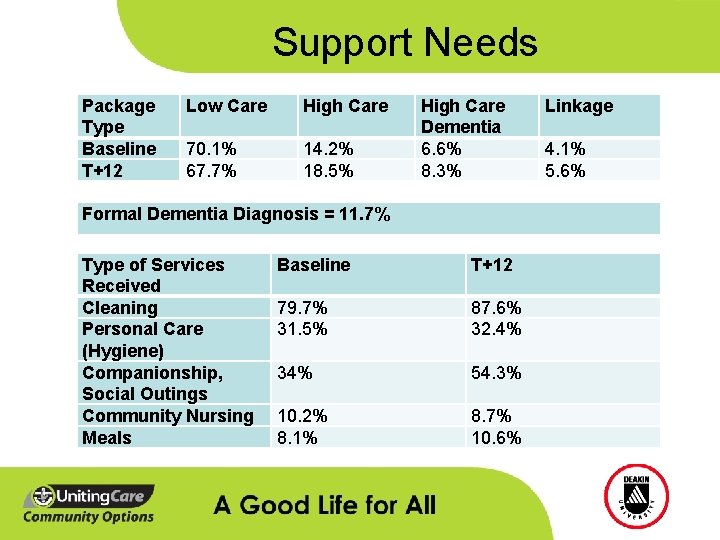
Support Needs Package Type Baseline T+12 Low Care High Care 70. 1% 67. 7% 14. 2% 18. 5% High Care Dementia 6. 6% 8. 3% Formal Dementia Diagnosis = 11. 7% Type of Services Received Cleaning Personal Care (Hygiene) Companionship, Social Outings Community Nursing Meals Baseline T+12 79. 7% 31. 5% 87. 6% 32. 4% 34% 54. 3% 10. 2% 8. 1% 8. 7% 10. 6% Linkage 4. 1% 5. 6%
Project Outcomes - Results
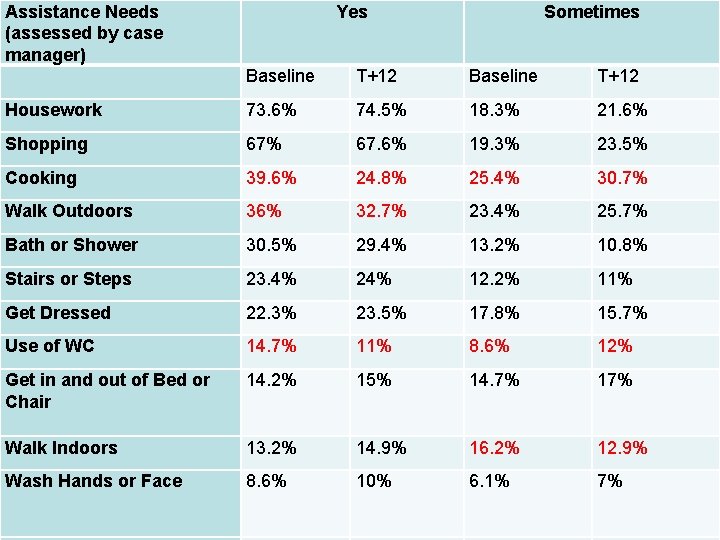
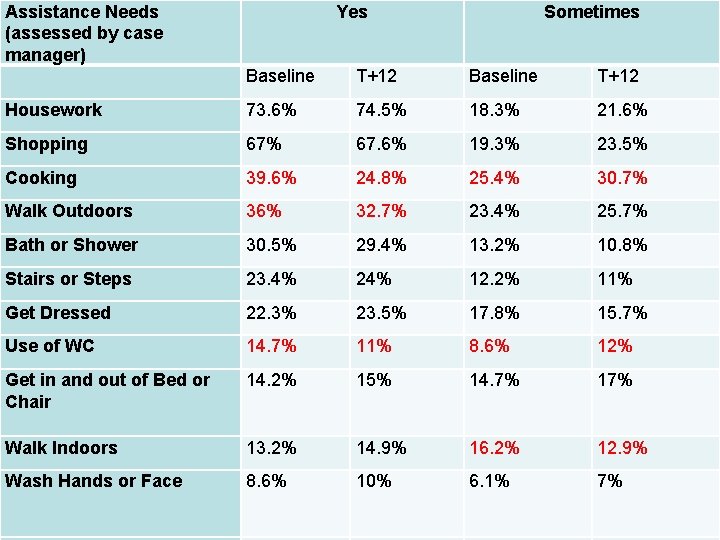
Assistance Needs (assessed by case manager) Yes Sometimes Outcomes cont. Baseline T+12 Housework 73. 6% 74. 5% 18. 3% 21. 6% Shopping 67% 67. 6% 19. 3% 23. 5% Cooking 39. 6% 24. 8% 25. 4% 30. 7% Walk Outdoors 36% 32. 7% 23. 4% 25. 7% Bath or Shower 30. 5% 29. 4% 13. 2% 10. 8% Stairs or Steps 23. 4% 24% 12. 2% 11% Get Dressed 22. 3% 23. 5% 17. 8% 15. 7% Use of WC 14. 7% 11% 8. 6% 12% Get in and out of Bed or Chair 14. 2% 15% 14. 7% 17% Walk Indoors 13. 2% 14. 9% 16. 2% 12. 9% Wash Hands or Face 8. 6% 10% 6. 1% 7%

Self-Direction Initial level of self-direction T 2 population T+12 @ Baseline Level 1 36 30 Level 2 17 21 Level 3 9 13
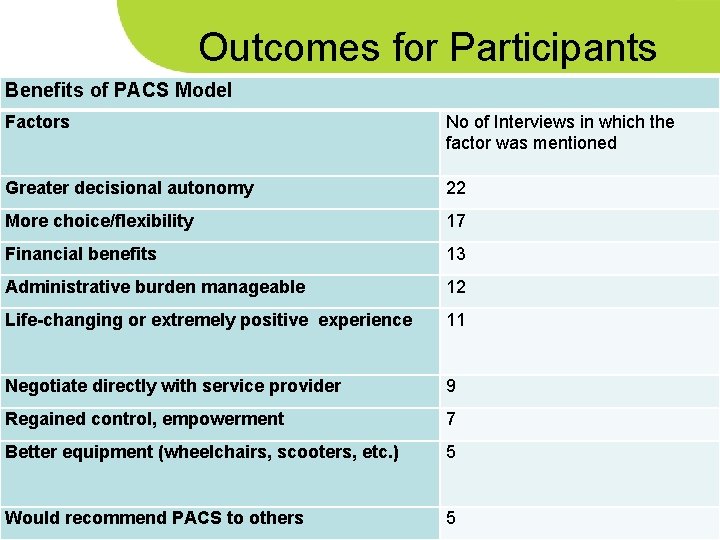
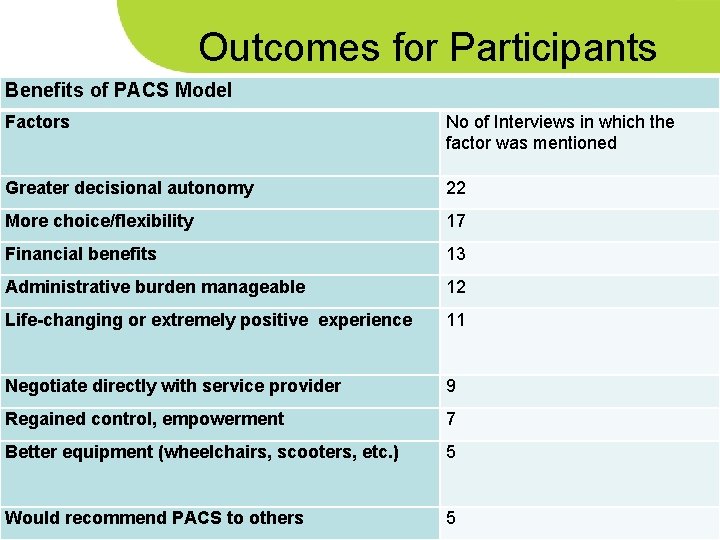
Outcomes for Participants Benefits of PACS Model Factors No of Interviews in which the factor was mentioned Greater decisional autonomy 22 More choice/flexibility 17 Financial benefits 13 Administrative burden manageable 12 Life-changing or extremely positive experience 11 Negotiate directly with service provider 9 Regained control, empowerment 7 Better equipment (wheelchairs, scooters, etc. ) 5 Would recommend PACS to others 5
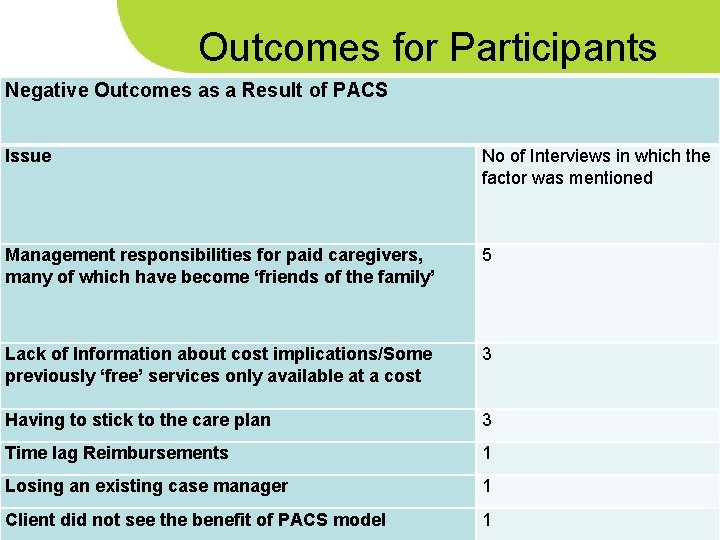
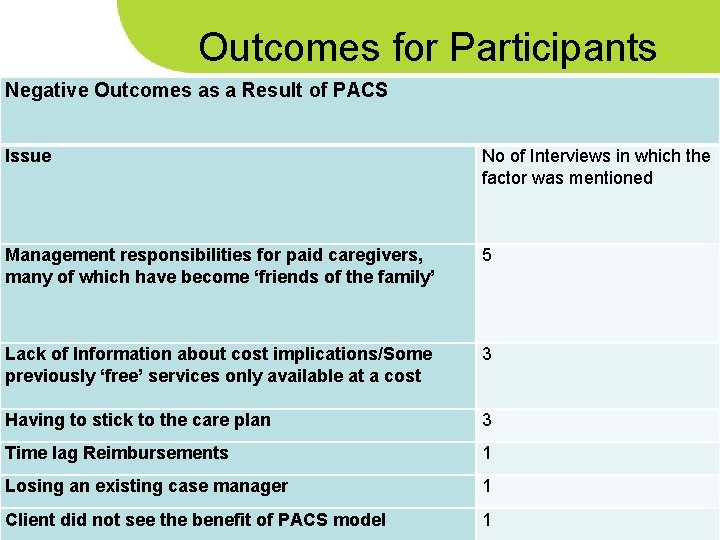
Outcomes for Participants Negative Outcomes as a Result of PACS Issue No of Interviews in which the factor was mentioned Management responsibilities for paid caregivers, many of which have become ‘friends of the family’ 5 Lack of Information about cost implications/Some previously ‘free’ services only available at a cost 3 Having to stick to the care plan 3 Time lag Reimbursements 1 Losing an existing case manager 1 Client did not see the benefit of PACS model 1

Outcomes for Participants Barriers to Self-Direction at a Higher Level (Levels 2 or 3) Factor Very little or no recollection of PACS No of Interviews in which the factor was mentioned 14 Perceived Lack of Expertise 13 Enrolment was rushed, poor communication, options not properly explained Lack of Time 14 Language Difficulties Happy the way things are Lack of Courage/Strength No Desire to handle money Settling down after crisis point Previous experience of changing care arrangements Health issues 7 (carers) 2 (participants) 3 5 2 2 1
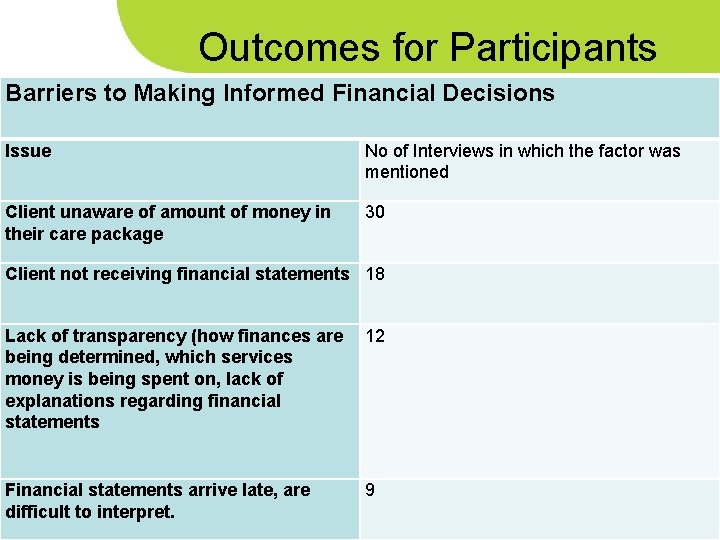
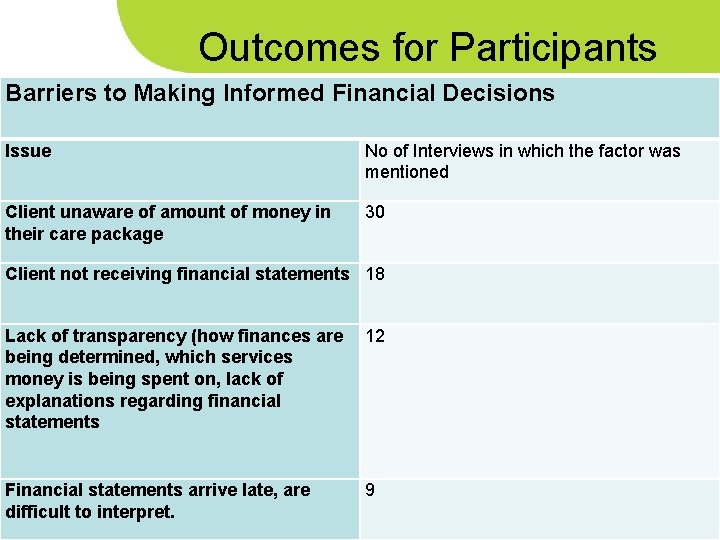
Outcomes for Participants Barriers to Making Informed Financial Decisions Issue No of Interviews in which the factor was mentioned Client unaware of amount of money in their care package 30 Client not receiving financial statements 18 Lack of transparency (how finances are being determined, which services money is being spent on, lack of explanations regarding financial statements 12 Financial statements arrive late, are difficult to interpret. 9

Outcomes for Participants Depth of Change Management Process Who made decision about the level of Self Direction? Case Manager & Client 6 13 8 Decision about what services are required Case Manager Unsure 7 6 Client 19
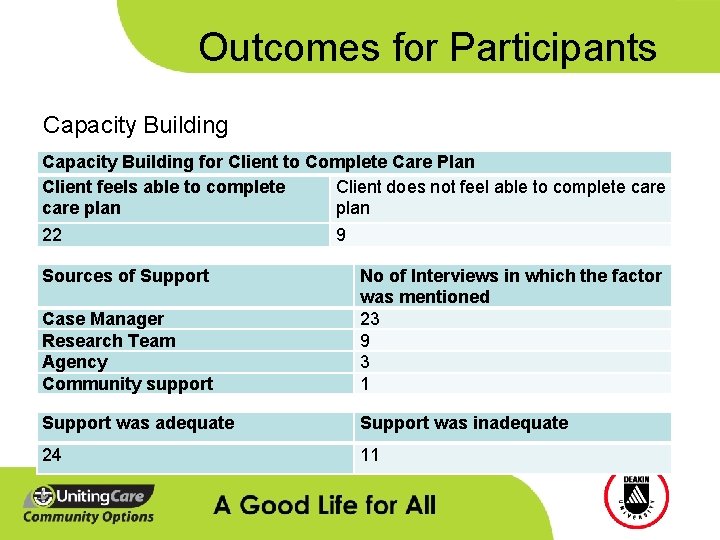
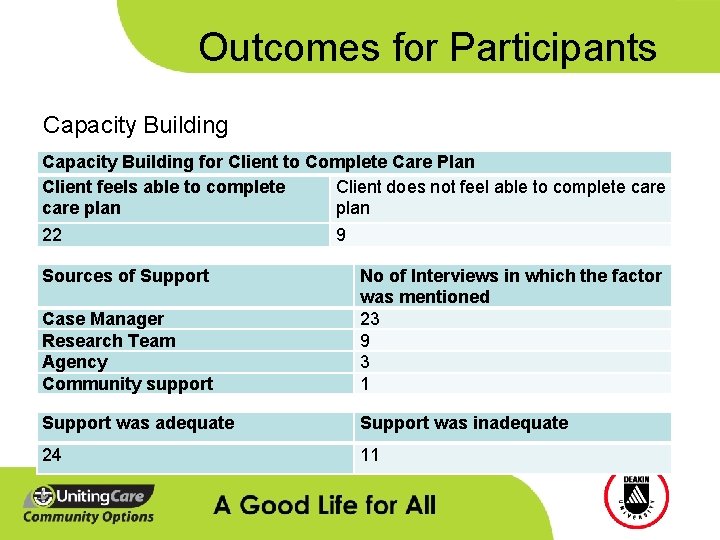
Outcomes for Participants Capacity Building for Client to Complete Care Plan Client feels able to complete Client does not feel able to complete care plan 22 9 Sources of Support Case Manager Research Team Agency Community support No of Interviews in which the factor was mentioned 23 9 3 1 Support was adequate Support was inadequate 24 11

Outcomes for Participants Comments about the Restorative Approach Factor Restorative Goal Setting Approach No of Interviews in which the factor was mentioned Positive (Good to communicate ones goals, case manager aware of goals, good to have goals/stay mentally/physically active) 22 Could not remember process, 8 No goal setting conducted with carers, goals not realistic enough, having to come up with goals without having time to think about them, couldn’t identify motivational goal, didn’t like language of ‘goals’) 5 Process not useful 3

Outcomes for Participants Comments on how to improve Case Management within a CDC context Issue No of Interviews in which the factor was mentioned Predominantly happy with the way case management is currently provided Be more thorough and responsive 29 Provide better information on what is available 11 Hand over control 6 Organise carers and accommodation 5 Should function as backup rather than as a manager 3 Ask clients about their needs – don’t assume 2 Be more transparent about funding arrangements 1 11
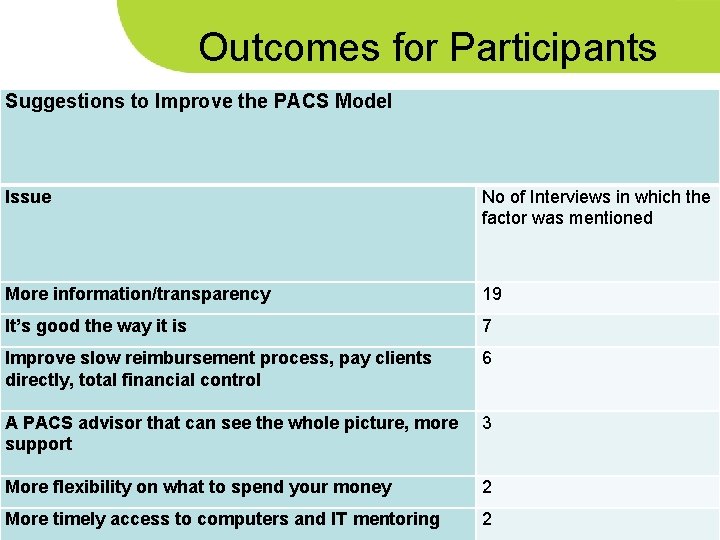
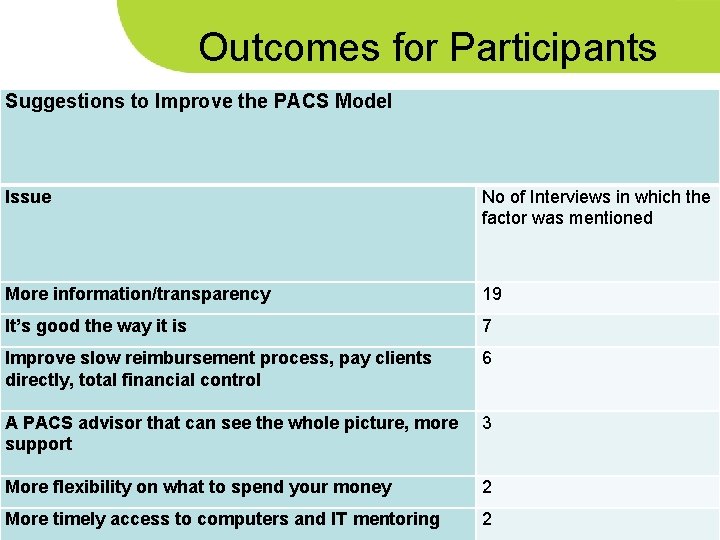
Outcomes for Participants Suggestions to Improve the PACS Model Issue No of Interviews in which the factor was mentioned More information/transparency 19 It’s good the way it is 7 Improve slow reimbursement process, pay clients directly, total financial control 6 A PACS advisor that can see the whole picture, more support 3 More flexibility on what to spend your money 2 More timely access to computers and IT mentoring 2
- Lessons Learnt
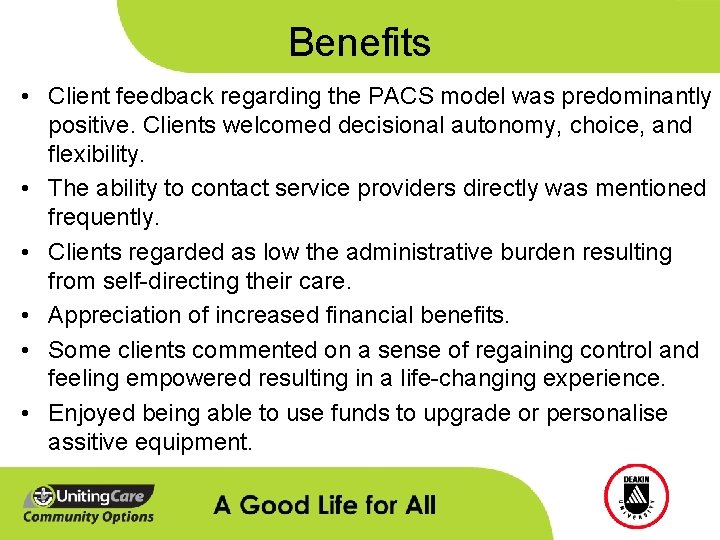
Benefits • Client feedback regarding the PACS model was predominantly positive. Clients welcomed decisional autonomy, choice, and flexibility. • The ability to contact service providers directly was mentioned frequently. • Clients regarded as low the administrative burden resulting from self-directing their care. • Appreciation of increased financial benefits. • Some clients commented on a sense of regaining control and feeling empowered resulting in a life-changing experience. • Enjoyed being able to use funds to upgrade or personalise assitive equipment.
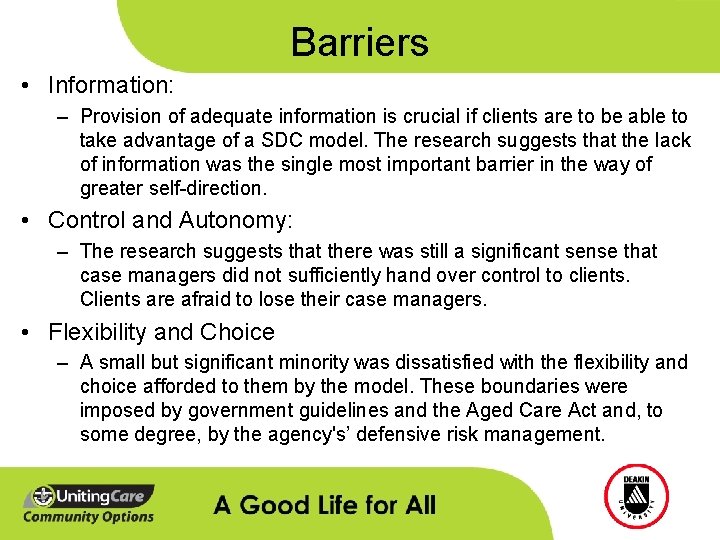
Barriers • Information: – Provision of adequate information is crucial if clients are to be able to take advantage of a SDC model. The research suggests that the lack of information was the single most important barrier in the way of greater self-direction. • Control and Autonomy: – The research suggests that there was still a significant sense that case managers did not sufficiently hand over control to clients. Clients are afraid to lose their case managers. • Flexibility and Choice – A small but significant minority was dissatisfied with the flexibility and choice afforded to them by the model. These boundaries were imposed by government guidelines and the Aged Care Act and, to some degree, by the agency's’ defensive risk management.
- Recommendations
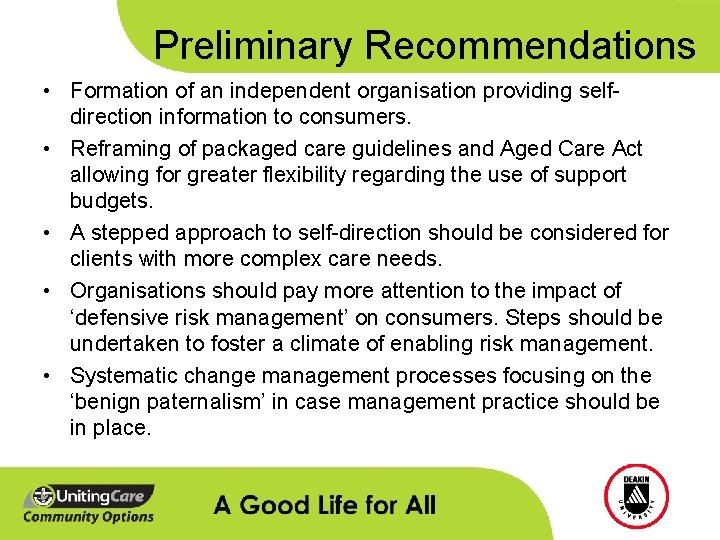
Preliminary Recommendations • Formation of an independent organisation providing selfdirection information to consumers. • Reframing of packaged care guidelines and Aged Care Act allowing for greater flexibility regarding the use of support budgets. • A stepped approach to self-direction should be considered for clients with more complex care needs. • Organisations should pay more attention to the impact of ‘defensive risk management’ on consumers. Steps should be undertaken to foster a climate of enabling risk management. • Systematic change management processes focusing on the ‘benign paternalism’ in case management practice should be in place.
Funding Support § Helen Macpherson Smith Trust § Australian Research Council § Perpetual Trustees § Percy Baxter Charitable Trust § B. B. Hutchings Bequest § John William Fleming Trust
CDC for Older People Thank you … Goetz. Ottmann@deakin. edu. au
 Life is older older than the trees
Life is older older than the trees Dignity of risk
Dignity of risk Sarah russell aged care
Sarah russell aged care 5 cultural safety principles
5 cultural safety principles My aged care
My aged care What is dignity of risk
What is dignity of risk Kimberley aged care services
Kimberley aged care services What is cultural safety in aged care
What is cultural safety in aged care Ananda aged care
Ananda aged care As people grow older
As people grow older My son aged three fell in the nettlebed
My son aged three fell in the nettlebed Nettles annotated
Nettles annotated For a moment the last sunshine fell
For a moment the last sunshine fell Levels of care primary secondary tertiary
Levels of care primary secondary tertiary Web accessibility for older users
Web accessibility for older users Shorter and older taller and younger
Shorter and older taller and younger Syncope in the older patient is
Syncope in the older patient is Which is older
Which is older Mental health and older adults
Mental health and older adults Older persons act norms and standards
Older persons act norms and standards Intellectual development in older adulthood
Intellectual development in older adulthood Older individuals who are blind program
Older individuals who are blind program Mental health and older adults
Mental health and older adults Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Older television sets had tubes
Older television sets had tubes The brother of the prodigal son
The brother of the prodigal son Nipołomice
Nipołomice Conclusion of physical examination
Conclusion of physical examination Downsizing and divesting older business
Downsizing and divesting older business Sos spelling for older students
Sos spelling for older students