Improving Family Planning Training for Family Medicine Residents

- Slides: 18
Improving Family Planning Training for Family Medicine Residents *Data included may not be published without authors’ permission Marji Gold, MD Crystal Query, MD Jessica Dalby, MD Cara Herbitter, MPH, CPH Megan Greenberg STFM National 2009
Objectives Participants will be able to: 1. 2. 3. Describe the gaps in reproductive health education in family medicine residency programs Identify possible causes for the gaps Describe strategies for improving reproductive health training in your own residencies
Discussion Outline l l l Introductions: Reproductive health (RH) training at your residency program Research Findings: Gaps in current practice and training Group Discussion: obstacles and strategies to improving RH residency training
Introductions What is reproductive health training like at your residency program/med school?
Q: Why Does Family Planning Matter to Family Physicians?
A: Most people need family planning! l l l 98% of ever sexually active women ages 15 -44 have used contraception Half of pregnancies in the US every year are unintended and 1/3 of those end in abortion 21% of women seeking private sector reproductive health care see family physicians

Research Findings l Gaps in current practice l Gaps in current training
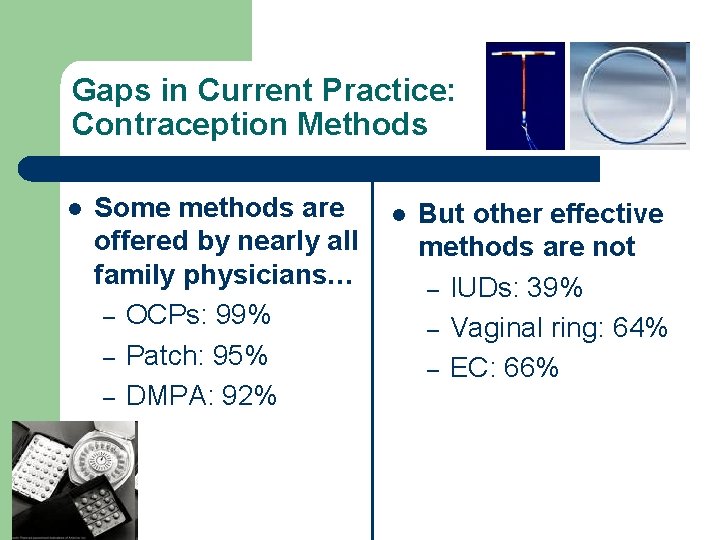
Gaps in Current Practice: Contraception Methods l Some methods are offered by nearly all family physicians… – OCPs: 99% – Patch: 95% – DMPA: 92% l But other effective methods are not – IUDs: 39% – Vaginal ring: 64% – EC: 66%
Gaps in Current Practice: Contraception Protocols l Evidence-based contraceptive protocols are not yet established in family medicine l Of family physicians surveyed, only: – – – 56% allow new hormonal contraception users to delay the pelvic exam 13% offer quick-start pill initiation 25% provide EC in advance
Gaps in Current Training: Contraception Methods l Nearly all chief residents report clinical training in some methods… – – OCPs: 100% DMPA: 92% Condoms: 89% Patch: 80% l But not in others – Hormonal IUD: 78% – EC: 75% – Copper IUD: 71% – Vaginal ring: 67%
Gaps in Current Training: Abortion and Options Counseling l Majority of residents (60%) report receiving no clinical abortion training (medication, MVA, or EVA) l Options counseling: 20% of chief residents report no clinical experience and 38% report no didactic instruction
Conclusion Residency training in the full range of contraception options and abortion should be increased to prepare family doctors to meet patients’ reproductive health needs.
Group Discussion: Obstacles What are obstacles to teaching residents the full range of contraceptive methods, pregnancy options counseling, and abortion?
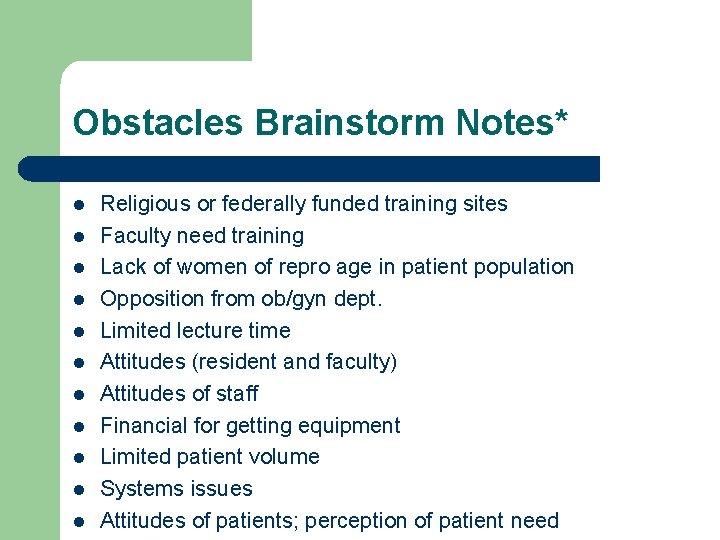
Obstacles Brainstorm Notes* l l l Religious or federally funded training sites Faculty need training Lack of women of repro age in patient population Opposition from ob/gyn dept. Limited lecture time Attitudes (resident and faculty) Attitudes of staff Financial for getting equipment Limited patient volume Systems issues Attitudes of patients; perception of patient need
Group Discussion: Strategies How can we improve training for the next generation of family doctors?
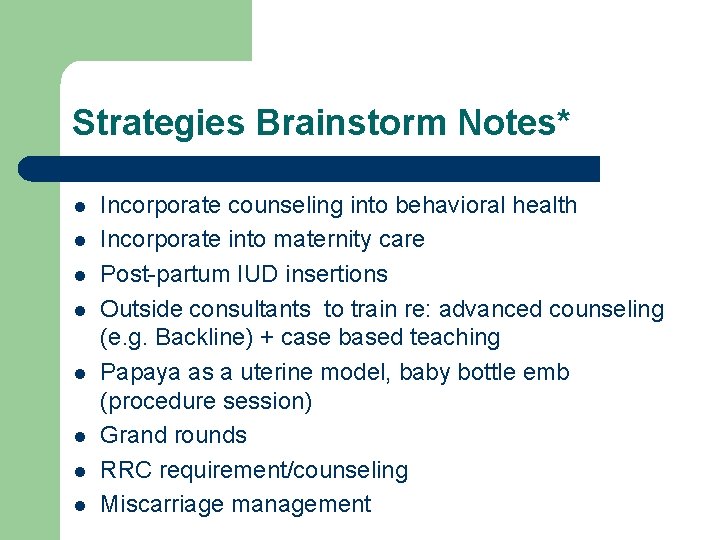
Strategies Brainstorm Notes* l l l l Incorporate counseling into behavioral health Incorporate into maternity care Post-partum IUD insertions Outside consultants to train re: advanced counseling (e. g. Backline) + case based teaching Papaya as a uterine model, baby bottle emb (procedure session) Grand rounds RRC requirement/counseling Miscarriage management
References 1. Landry DJ et al. Public and private providers’ involvement in improving their patients’ contraceptive use. Contraception 2008; 78: 42 -51. 2. Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health 2006; 38: 90 -96. 3. Mosher WD et al. , Use of contraception and use of family planning services in the United States: 1982– 2002, Advance Data from Vital and Health Statistics 2004 No. 350. 4. Steinauer JE, Depineres T, Robert AM, Westfall J, Darbey P. Training Family Practice Residents in Abortion and other Reproductive Health Care: A Nationwide Survey. Fam Plann Perspect 1997; 29: 222 -7.
 Uihc internal medicine residency
Uihc internal medicine residency Unm emergency medicine residents
Unm emergency medicine residents Uthscsa internal medicine residents
Uthscsa internal medicine residents Uw neurosurgery residents
Uw neurosurgery residents Umass memorial medical center pharmacy residency
Umass memorial medical center pharmacy residency Dr kirk kleinfeld
Dr kirk kleinfeld Https://ncc-efm.org/game/efmgame.cfm
Https://ncc-efm.org/game/efmgame.cfm Tufts neurology residency
Tufts neurology residency Unmc oasis
Unmc oasis Dr julia creider
Dr julia creider Informed delivery campaigns
Informed delivery campaigns Karl suure tähtsaim residents
Karl suure tähtsaim residents Tourism involving non-residents of the given area.
Tourism involving non-residents of the given area. How can an na best help residents with eating?
How can an na best help residents with eating? 13 personal care skills
13 personal care skills Famous people from yonkers
Famous people from yonkers St louis family medicine residency
St louis family medicine residency Uf neurology residents
Uf neurology residents Herodicus of megara
Herodicus of megara