Implementing Quality Improvement and P 4 P in
- Slides: 14
Implementing Quality Improvement and P 4 P in Ambulatory Academic Group Practice Neil Goldfarb Associate Dean for Research, JSPH Co-Director, College for Value-based Purchasing of Health Benefits Director of Ambulatory Care Performance Improvement, Jefferson University Physicians Disclosure: No identified conflicts of interest.
Jefferson University Physicians – 500+ physicians – Clinical Care Subcommittee • History • Staffing • Approach to projects – Departmental initiatives – JUP-wide initiatives – Value-based purchasing initiatives
Smoking Cessation Program Department of Otolaryngology • 85% of head & neck cancers are associated with tobacco use and account for 3% of all cancers in the U. S. • In 2006, the Department of Otolaryngology conducted a study of head & neck cancer patients – Baseline finding: 60% documentation of smoking hx – Redesigned charting tool, educated providers – Follow-up finding: 100% documentation
JUP-wide smoking cessation initiative • Charts reviewed • Feedback provided • Education and CME provided – Includes information on billing for counseling • Tools and resources provided • Six-month follow-up charts reviewed
Physician Practice Patient Safety Assessment (PPPSA) • Developed and tested in 2006 by: – Health Research Education Trust (HRET) – Institute for Safe Medication Practices (ISMP) – Medical Group Management Association (MGMA) – National expert panel and advisory committee • Self-assessment tool covers 79 safety-related ambulatory processes and practices • Self-administered by a multidisciplinary team of administrators, physicians, pharmacists, nurses and technicians • Comparative national benchmarks established by MGMA pilot test
Implementation • Fall 2006 – Based on a review of patient safety assessment tools, the PPPSA tool was selected for a pilot implementation throughout JUP • Spring 2007 – Pilot study performed in the Division of Internal Medicine • 2007 -2008: Survey expanded to other JUP practices • January 2009, JUP Management Committee: – Completion of the survey mandated across JUP practices and tied to financial incentive for practice administrators – Selection of one departmental/divisional priority areas for improvement based on baseline measurement – Development and implementation of an action plan – Completion of a timeline for implementation of performance improvement actions and re-measurement
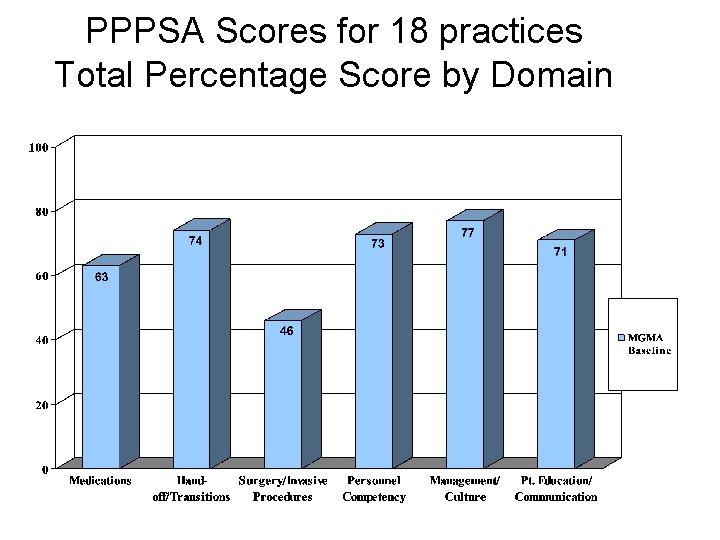
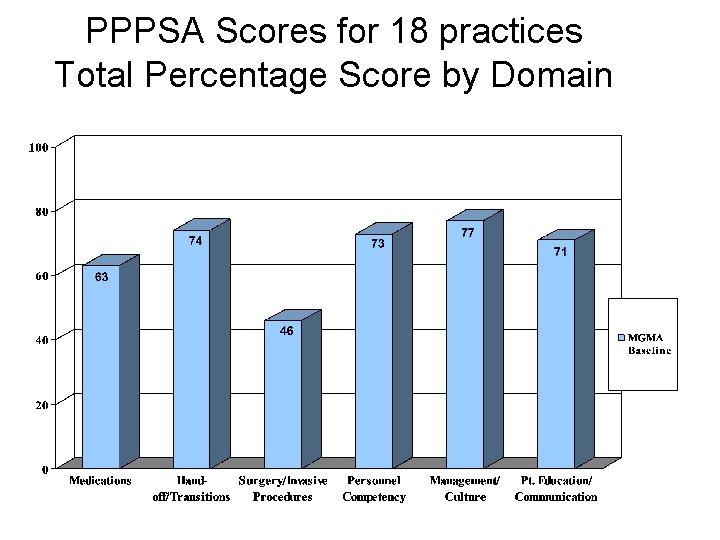
PPPSA Scores for 18 practices Total Percentage Score by Domain
Recommendations Department Level • Identify one safety metric for improvement • Develop and submit action plan for selected safety metric JUP Level • Interdisciplinary patient safety task force • Medication safety educational initiatives • Develop/improve patient education materials, including literacy and language • Develop staff education and competency programs and standards • Examine systems for patient notification of test results • Develop a system for error and near-miss reporting
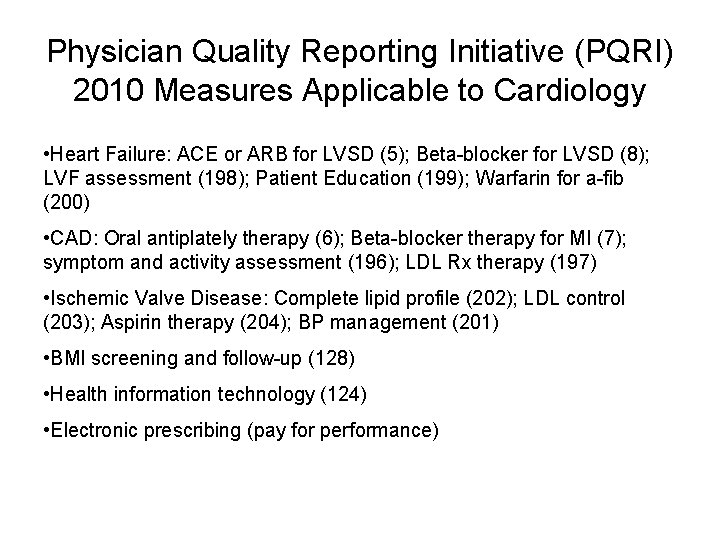
Physician Quality Reporting Initiative (PQRI) 2010 Measures Applicable to Cardiology • Heart Failure: ACE or ARB for LVSD (5); Beta-blocker for LVSD (8); LVF assessment (198); Patient Education (199); Warfarin for a-fib (200) • CAD: Oral antiplately therapy (6); Beta-blocker therapy for MI (7); symptom and activity assessment (196); LDL Rx therapy (197) • Ischemic Valve Disease: Complete lipid profile (202); LDL control (203); Aspirin therapy (204); BP management (201) • BMI screening and follow-up (128) • Health information technology (124) • Electronic prescribing (pay for performance)
Requirements for Successful PQRI Implementation • Leadership and faculty interest and buy-in • Infrastructure support • Priority within the organization
JUP Approach to PQRI Implementation • Team of administrator and clinical quality nurse meet with practices to provide education on PQRI measures • Selection and specifications of measures • Identification of process changes required for successful PQRI reporting • Development of tools and worksheets • Testing of claims submission using CMS test code • Follow-up with practices • Members of the JUP quality team and JUP administration function as a resource for all practices • Larger PQRI team, consisting of compliance officer, statistician and quality analysts meet to discuss PQRI progress across JUP practices
Barriers and Lessons Learned • Difficult to get buy-in from providers and office staff – Bonus size may be too small – Increased cost of measure submission – Belief that PQRI reporting will not improve patient care • Measures are based on new billing codes and processes • Complexity of measure specifications • Constantly changing measurement set and specifications • Multidisciplinary approach is crucial • Essential to provide ongoing education to practices • Staff must be available to practices as a resource for clarification of measure specifications
Other Initiatives • Support for EMR implementation and achieving “meaningful use” • P 4 P program support: chart reviews, registry development, measurement development, VBP task force
Summary: Challenges from the provider perspective • Need clarity and agreement on measurement parameters (and recognition of issues such as sample size, attribution) • Need frequent, timely feedback • Need recognition of sicker, under-served, nonadherent populations • Need educational tools for providers and patients • Need resources to implement IT and QI • Hospital and physician incentives need to be aligned