I Dont Care Depression Anxiety and Apathy in















- Slides: 26
I Don’t Care! Depression, Anxiety, and Apathy in Parkinson’s Disease Rebecca Radue, MD with Art Walaszek, MD

Introductions – Raised in Stevens Point, WI – Graduated from UW School of Medicine and Public Health in 2014 – PGY-3 in Psychiatry – American Association of Geriatric Psychiatry Honor Scholar – Former Certified Nursing Assistant in Long Term Care – Granddaughter and caregiver to my grandma with Parkinson’s Disease

What will we cover? – Apathy –Depression –Anxiety

Apathy A lack of interest, enthusiasm, or concern - Apathy will affect - 40% of people without cognitive impairment and PD - 60% of people with cognitive impairment and PD
Who is at risk for apathy? – Older Men – Cognitive Impairment – More severe PD symptoms

What does apathy look like? – Lack of motivation to do things – Feeling that usually enjoyable or routine activities will take too much effort – Not wanting to go anywhere – Requiring constant prompting to get things done – If left to their own devices and without prompting, people may just sit on the couch or watch TV – People may not eat or drink without prompting

Depression – Low mood, sadness, irritability – Trouble with sleep – Trouble with appetite – Feelings of guilt or worthlessness – Poor concentration – Lack of enjoyment in things that the person used to enjoy – Low energy – Thoughts of suicide
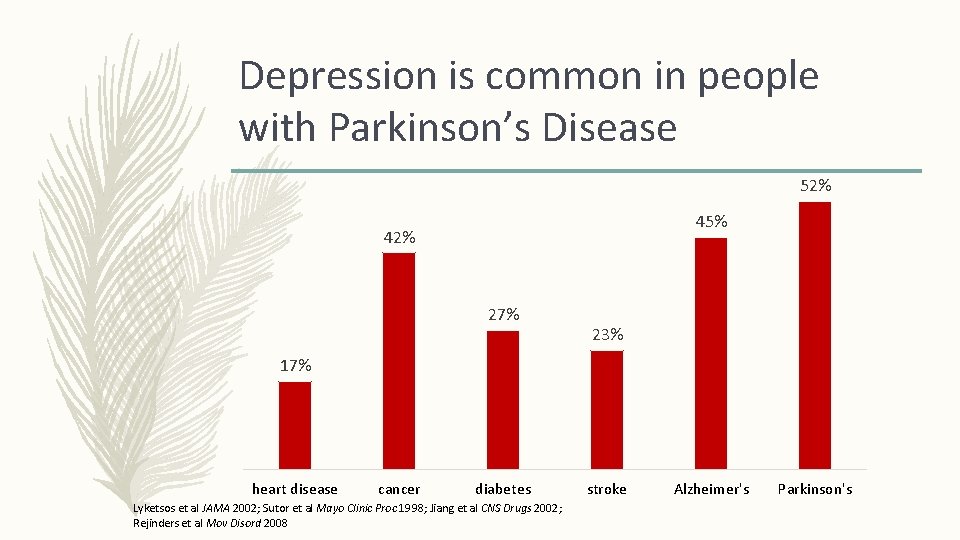
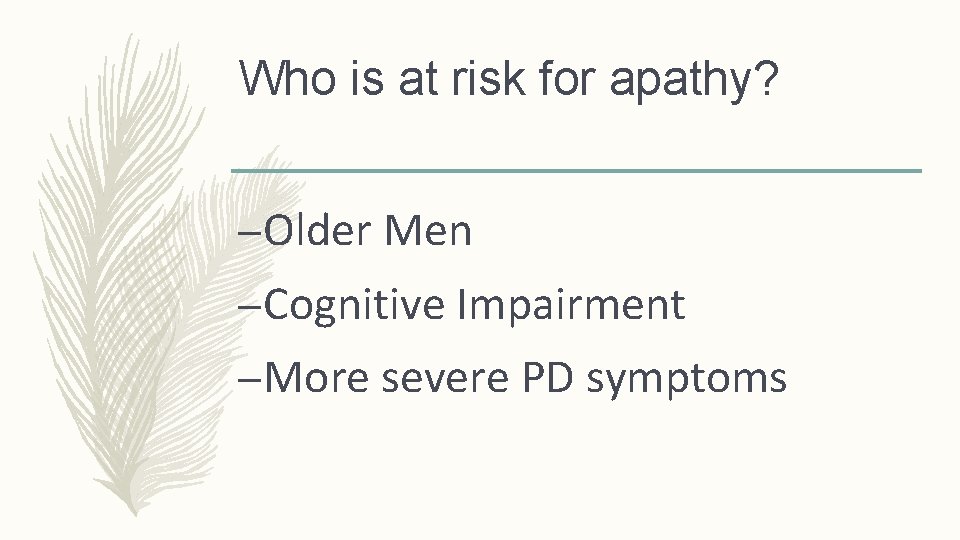
Depression is common in people with Parkinson’s Disease 52% 45% 42% 27% 23% 17% heart disease cancer diabetes Lyketsos et al JAMA 2002; Sutor et al Mayo Clinic Proc 1998; Jiang et al CNS Drugs 2002; Rejinders et al Mov Disord 2008 stroke Alzheimer's Parkinson's
Who is at risk for PD Depression? – Women > Men – Family history of depression – Early onset of PD

PD Depression versus non-PD Depression – more anxiety, pessimism, and suicidal ideation (without suicidal behavior) – less guilt and self-reproach – most common symptoms: low energy, difficulty with concentration or making decisions, feeling blue, feeling hopeless, poor sleep – depression may be prodromal to (coming before) PD

Depression versus Apathy – Only Depression will have associated low mood, and may come with feelings of worthlessness or sadness – Apathy and Depression both can lead to people not enjoying things they used to enjoy doing
Parkinson’s Dementia versus Lewy Body Dementia – In Lewy Body Dementia: – cognitive and motor symptoms begin within one year of each other – cognitive impairment usually comes first – tremor does not occur early on, rather, rigidity and trouble walking do – Thinking and memory ability tends to fluctuate – In Parkinson’s Disease Dementia – Some minor cognitive impairment is common in all people living with PD – Major cognitive issues don’t usually become a problem for 10 -15 years after motor symptoms start

Anxiety – Constant feelings of anxiety, nervousness, or worry – Anxiety about “wearing off” of PD medications – Panic Attacks – Can make PD motor symptoms worse – Can be a side effect of some PD medications
Anxiety in Parkinson’s Disease An estimated 25 -45% of people living with PD will experience bothersome anxiety

How do we manage these issues?

Apathy: Tips for people living with PD and their caregivers – Try not to get frustrated – Maintain social relationships – Create a daily schedule – Set weekly goals – Increase enjoyable activities – dance, garden, fish…

Treatment Options for Apathy – Optimize PD medication regimen – Optimize sleep – Stimulant medications – Less evidence for cholinesterase inhibitors, antidepressants

Depression: Tips for people living with PD and their caregivers – Keep in mind that depression is common, frequently associated with PD, and is treatable – Work with your doctor to find the right treatment for you – Keep close with your social supports – Try to do as many activities as you enjoy – “fake it till you make it”

Non-Medication Treatments for Depression – light therapy – electroconvulsive therapy – repetitive transcranial magnetic stimulation – Exercise – Psychotherapy
Medication Options for Depression – Optimize medication treatment of PD – Antidepressant Medications – TCAs (nortriptyline) – SSRIs (sertraline/Zoloft, escitalopram/Lexapro, citalopram/Celexa) – SNRIs (venlafaxine/Effexor, duloxetine/Cymbalta) – Mirtazapine/Remeron – Augmentation Strategies with Other Meds
Anxiety: Tips for People Living with PD and their Caregivers – Keep a diary of your anxiety and PD symptoms – Try to determine what your triggers are – Work with your doctor to find the best treatment for you – Keep close with social supports

Treatment Options for Anxiety – Optimize treatment for PD, especially if “wearing off” makes anxiety worse – Antidepressants – Exercise – Psychotherapy
Psychotherapy: A safe and effective treatment for anxiety and depression – Cognitive Behavioral Therapy is the most evidence-based approach – Mindfulness – Otherapies may also be effective

Other Medical Issues that can lead to Anxiety or Depression – Thyroid problems – Cardiac or other vascular problems – Certain medication side effects – Be sure to see your doctor if you or your loved one has a sudden change in behavior
Take Home Points – Anxiety, Depression, and Apathy are common in PD – Anxiety, Depression, and Apathy are treatable – Work with your doctors to find the best treatments for your loved one
Thank you! rradue@uwhealth. org
 Dont ask dont tell political cartoon
Dont ask dont tell political cartoon Dont laugh at me dont call me names
Dont laugh at me dont call me names Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Stress anxiety depression
Stress anxiety depression Anxiety in the heart of man causes depression
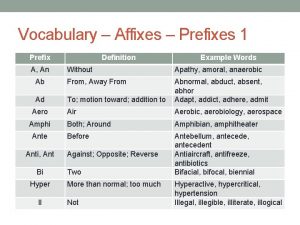
Anxiety in the heart of man causes depression Contrasting prefixes medical terminology
Contrasting prefixes medical terminology Zeal etymology
Zeal etymology Apathy
Apathy Employee apathy
Employee apathy An definition
An definition Apathy is the solution
Apathy is the solution Apathy word origin
Apathy word origin Apathy in a sentence
Apathy in a sentence Apathy etymology
Apathy etymology Verilog dont care
Verilog dont care I dont care ascii
I dont care ascii I dont care ascii
I dont care ascii Words for dont care
Words for dont care People dont care
People dont care Nursing interventions for grieving
Nursing interventions for grieving Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Clip clop and you don't stop
Clip clop and you don't stop Why dont water and oil mix
Why dont water and oil mix Chapter 8 managing stress and anxiety
Chapter 8 managing stress and anxiety Frustration anxiety and tension
Frustration anxiety and tension Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders