Hot Topics in Healthcare Emerging Trends and What


- Slides: 26
Hot Topics in Healthcare Emerging Trends and What is Changing American Association of Healthcare Administrative Management November 7, 2017
Agenda • State Legislative Issues • Medicaid Reform • Payor Update • Regulatory Update 2
State Legislative Issues

State Legislative Issues • Certificate of Need • Taxes • Graduate Medical Education • Behavioral Health 4
Medicaid Reform
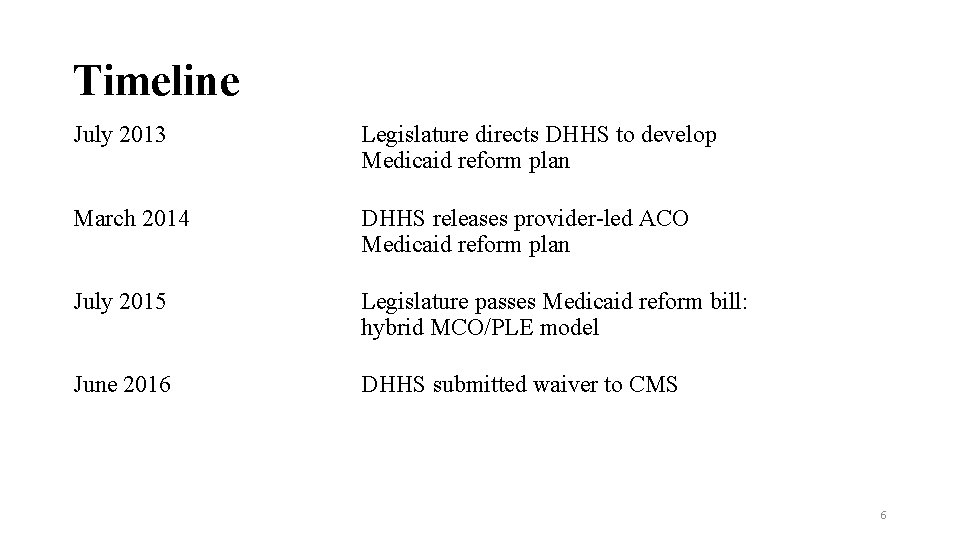
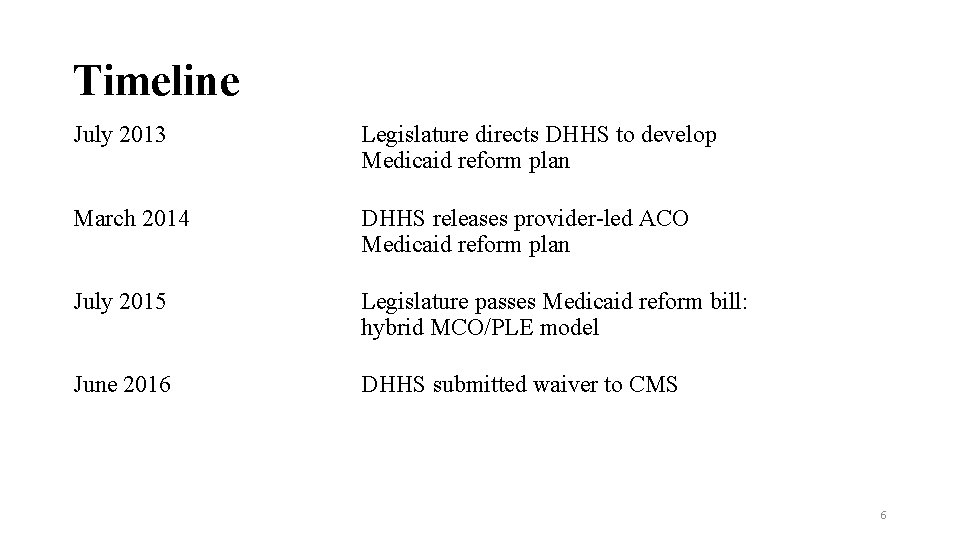
Timeline July 2013 Legislature directs DHHS to develop Medicaid reform plan March 2014 DHHS releases provider-led ACO Medicaid reform plan July 2015 Legislature passes Medicaid reform bill: hybrid MCO/PLE model June 2016 DHHS submitted waiver to CMS 6
Timeline (Cont’d) May 2017 DHHS solicits feedback on pending waiver Sept 2017 DHHS solicits feedback on its revised reform proposal July 2019 Projected start date of Medicaid managed care (but actual start is contingent on when CMS approves the waiver) Mid 2023 Projected start date of behavioral health integration (unless changed by legislature) 7
The 1115 Waiver Process States can implement a managed care delivery system using three basic types of federal authorities: • State plan authority [Section 1932(a)] • Waiver authority [Section 1915 (a) and (b)] • Waiver authority [Section 1115] NC is pursuing the 1115 waiver (as ”directed” by the legislature) 8
Major Aspects of Waiver (and Legislation) • 3 Statewide MCOs; up to 12 regional PLEs - Last week, DHHS released two requests for information • Statement of Interest from prepaid health plains due November 22, 2017 • Financial aspects, including capitation rate setting, due December 1, 2017 - Request of Proposal for potential prepaid health plans expected in Spring 2018 • 6 PLE regions • Licensed by DOI; regulated by DHHS - DOI looks at solvency - NCHA pushing for ”Chapter 58” (insurance law) and other protections, such as prompt pay requirements 9
Two types of plans DHHS envisions 2 types of plans: • Standard plan (most of the population) • Tailored plans (to be phased in): - Special Needs population - Dual eligible beneficiaries - Foster children - Long stay nursing home patients 10
Waiver Aspects DHHS and NCHA support expediting integration of physical and behavioral health - Will require a legislative change (currently projected to integrate in 2023) DHHS foresees advanced medical homes (including payments for care management) - Not clear how CCNC may evolve or be involved 11
Other Aspects of the Waiver Medical loss ratio (85% under federal rules) Network adequacy standards Beneficiary protections • 30 days to choose a plan; switch PCPs at certain times Provider relations: MCOs must • Have provider call center • Provide manuals and policies • Provide appeals process if provider terminated over quality; contract breach 12
Medicaid Managed Care: Safety Net • Supplemental payments are not permissible in a managed care environment. • CMS Medicaid Managed Care Rule issued in 2015. • Doesn’t align with DHHS’ policy direction. • Preservation of safety net extremely important 13
Medicaid Managed Care Contracting Challenges • Assess capabilities to move toward value-based and/or alternative payment methodologies • Negotiate payment methodologies that meet the following standards • Must have the tools to evaluate and monitor financial impact of payment methodology • Payment methodology must result in proper sharing of risks between the parties • Costs to administer and monitor must be reasonable • Never focus exclusively on price during managed care contract negotiations, since numerous contract terms can affect the degree of legal, strategic, and financial risk • Negotiate all contract terms and rates as part of a comprehensive arrangement 14
Medicaid Managed Care - Revenue Cycle Challenges • Challenges posed by the increase in Managed Medicaid plans, while not outside of the usual set of problems, will have a dramatically increased impact on the stability of the revenue cycle • System Enhancements • Establish Plan Codes • Update claim scrubber • Update Contract Management System • Provider Enrollment/Credentialing • Eligibility requirements • Detailed insurance verification is critical • Selecting correct Plan Code is a must • Staff Education extremely important 15
Medicaid Managed Care - Revenue Cycle Challenges • Authorization Requirement • More restrictive authorizations rules • Frequent changes to policies • Build authorization matrix to assist staff • Staff education extremely important • Denial Management • Working with Third Party Administrators (TPAs) • Many payers are outsourcing to reduce administrative costs • Processes become more complex with the increased number of players • Variation from standard CMS claims editing • New Reimbursement methodologies 16
Payor Update
Payor Update • Medicare Provider Workgroup • Medicaid Technical Advisory Workgroup • Managed Care Committee 18
Payor Update • CY 2018 ACA Market Update • Medicaid Payment Shortfalls – I/P Rehabilitation Services • Medicaid Secondary Claims Payment Issues 19
Medicaid Secondary Claim Payment Issues • On September 25, 2017, DMA announced that it would be suspending the new Medicaid secondary claims edits related to Claim Adjustment Reason Code (CARC) 97 for 90 days. • During this 90 -day period, NCTracks will allow the claim or claim line billed with primary payer CARC 97 to process and adjudicate without denying the claim or claim line. DMA will provide further instructions before the 90 -day period expires. • During this 90 -day period, hospitals should work with their vendors to ensure that they can submit claims with CARC information, at the header and detail line level, exactly as it appears on the primary payer’s EOB/Remittance. • Mismatches created by payor’s different billing requirements 20

Regulatory Update
CMS Releases Final OPPS Rule for 2018 • Finalized proposal that cuts Medicare Part B drug reimbursement to hospitals in the 340 B drug discount program for separately payable drugs by nearly 30 percent, from average sales price (ASP) plus 6 percent to ASP minus 22. 5 percent. The reduction takes effect January 1, 2018. • Payment reduction does not affect critical access hospitals, which are not paid under the OPPS, rural sole community hospitals, children’s hospitals, and PPSexempt cancer hospitals. • Payment reduction applies to hospitals enrolled in 340 B as disproportionate share (DSH) hospitals and rural referral centers (RRC). 22
CMS Releases Final OPPS Rule for 2018 • CMS estimates that the final rule will reduce hospital’s Medicare Part B drug reimbursement by $1. 6 billion, higher than the $900 million estimate in the proposed rule. • CMS stated that it will redistribute the “savings” to payment under the OPPS for non-drug items and services to all hospitals, including non-340 B hospitals. • The final rule also establishes two modifiers to identify 340 B drugs billed under OPPS that hospitals must begin using effective January 1, 2018 • One for 340 B hospitals that are subject to the payment reduction (JB) • Separate informational modifier for 340 B hospitals not subject to the payment reduction (TB) 23
CMS Releases Final OPPS Rule for 2018 • The America Hospital Association (AHA), the Association of American Medical Colleges (AAMC), and America’s Essential Hospitals (AEH) said they will challenge the 340 B payment change in court, arguing that the new policy subverts Congress’ intent for the program. 24
CMS Releases Final 2018 Physician Payment Rule • Makes changes to policies implementing the site-neutral provisions of Section 603 of the Bipartisan Budget Act of 2015. • Section 603 requires that, except for dedicated emergency department services, services furnished in off-campus provider-based departments that began billing under the OPPS on or after Nov. 2, 2015, or that could not meet the 21 st Century Cures "mid-build" exception, will no longer be paid under the outpatient prospective payment system, but under another applicable Part B payment system. • Confirms policy to pay hospitals at 40%, rather than 50%, of the OPPS rate for non-excepted services in 2018. 25
Questions/Discussion Ronnie Cook rcook@ncha. org 919 -677 -4225 26
 Emerging trends in community development
Emerging trends in community development Emerging trends in business intelligence
Emerging trends in business intelligence Emerging trends in software engineering ppt
Emerging trends in software engineering ppt Emerging trends in business intelligence implementation
Emerging trends in business intelligence implementation Strategic management trends
Strategic management trends Emerging trends in society
Emerging trends in society Challenges of emerging trends in operating systems
Challenges of emerging trends in operating systems Emerging trends in disaster management
Emerging trends in disaster management Mis trends
Mis trends Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine meaning
Sports medicine meaning Chapter 1 history and trends of health care
Chapter 1 history and trends of health care Chapter 1 history and trends of health care
Chapter 1 history and trends of health care Emily edison nutrition
Emily edison nutrition Hot topics in patent law
Hot topics in patent law Hot topics in networking
Hot topics in networking Hot topics in leadership
Hot topics in leadership Histology resume
Histology resume Hot topics in networking
Hot topics in networking White hot vs red hot temperature
White hot vs red hot temperature Advantages of cold working
Advantages of cold working Perbedaan hot lava dan hot lava volcano
Perbedaan hot lava dan hot lava volcano Hot nor
Hot nor Deca prepares emerging leaders and entrepreneurs
Deca prepares emerging leaders and entrepreneurs It infrastructure and emerging technologies
It infrastructure and emerging technologies The byzantine empire and emerging europe
The byzantine empire and emerging europe It infrastructure and emerging technologies
It infrastructure and emerging technologies