HEALTH AND P E CPR and First Aid

- Slides: 26
HEALTH AND P. E. CPR and First Aid
FIRST AID Why is First Aid important? It is important because a delay of just a few minutes when a person’s heart stops can mean the difference between life or death. What is First Aid? It is the immediate care to an injured or suddenly ill person. It consists of providing temporary medical assistance until qualified medical care arrives. Good Samartian Laws provide protection against lawsuits. As in when a rescuer is acting during an emergency, in good faith, without compensation, and not guilty of malicious misconduct. Duty to act can be required by employment or if the rescuer is a caretaker. A verbal nod is consent to perform first aid. If the victim is unresponsive, then verbal consent is implied. Abandonment is when the rescuer leaves the victim without help. Negligence is when the victim suffers further injury because the care given did not meet standards expected from a person of similar training. Items in a First Aid Kit should be bandages, gloves, tape, scissors, etc.
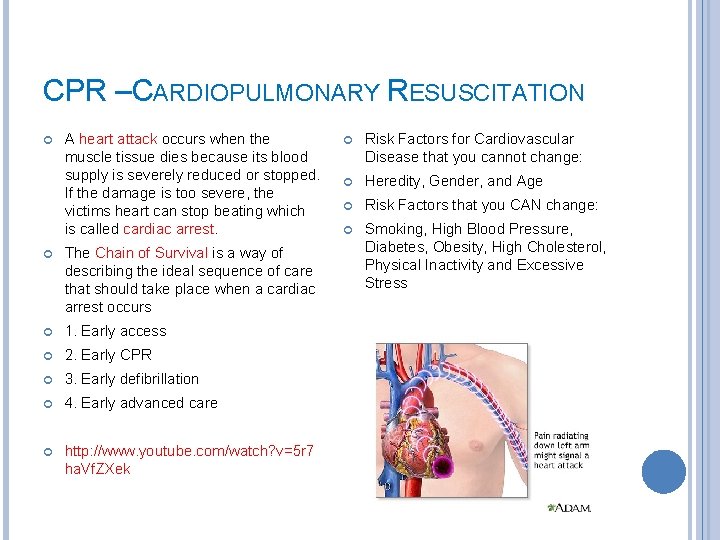
CPR –CARDIOPULMONARY RESUSCITATION A heart attack occurs when the muscle tissue dies because its blood supply is severely reduced or stopped. If the damage is too severe, the victims heart can stop beating which is called cardiac arrest. The Chain of Survival is a way of describing the ideal sequence of care that should take place when a cardiac arrest occurs 1. Early access 2. Early CPR 3. Early defibrillation 4. Early advanced care http: //www. youtube. com/watch? v=5 r 7 ha. Vf. ZXek Risk Factors for Cardiovascular Disease that you cannot change: Heredity, Gender, and Age Risk Factors that you CAN change: Smoking, High Blood Pressure, Diabetes, Obesity, High Cholesterol, Physical Inactivity and Excessive Stress
PERFORMING CPR When a person’s heart stops beating, they need CPR consists of breathing oxygen into a victim’s lungs and moving blood to the heart and brain by giving chest compressions. CPR Steps 1. Check for responsiveness. Tap the victims shoulder and ask if they are OK. If the victim does not respond, ask a bystander to call 911. 2. Chest compressions. This moves a minimal amount of blood to the heart and brain. Place one hand over the other in the center of the chest and give 30 compressions ranging from 1. 5 to 2 inches on an adult. 3. Open airway and check for breathing. Place the victim on a hard surface and open airway by doing the head tilt, chin lift. Place your ear by their mouth and listen for breathing while you watch to see if the chest rises and falls. 4. Rescue breaths. Pinch the nose and put your mouth over victim’s and give 2 rescue breaths.
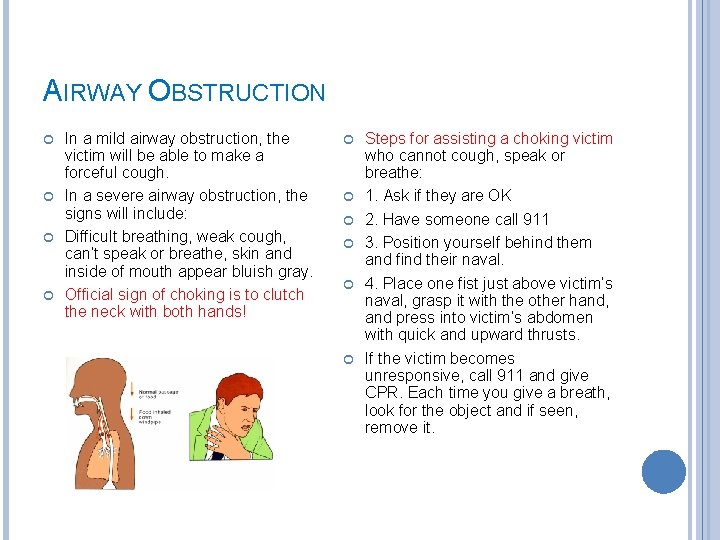
AIRWAY OBSTRUCTION In a mild airway obstruction, the victim will be able to make a forceful cough. In a severe airway obstruction, the signs will include: Difficult breathing, weak cough, can’t speak or breathe, skin and inside of mouth appear bluish gray. Official sign of choking is to clutch the neck with both hands! Steps for assisting a choking victim who cannot cough, speak or breathe: 1. Ask if they are OK 2. Have someone call 911 3. Position yourself behind them and find their naval. 4. Place one fist just above victim’s naval, grasp it with the other hand, and press into victim’s abdomen with quick and upward thrusts. If the victim becomes unresponsive, call 911 and give CPR. Each time you give a breath, look for the object and if seen, remove it.
GRAPHIC ORGANIZER 4 Steps of CPR Explain in detail what occurs in each step What is First Aid? Why is it important? Explain all vocabulary associated with First Aid.
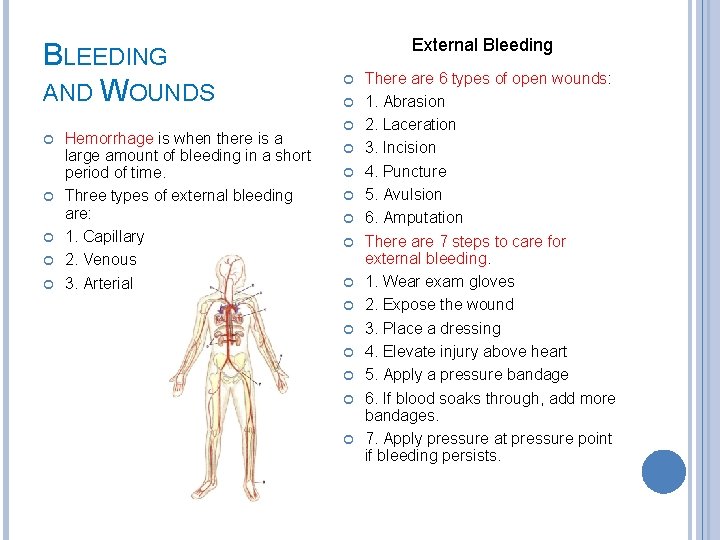
BLEEDING AND WOUNDS Hemorrhage is when there is a large amount of bleeding in a short period of time. Three types of external bleeding are: 1. Capillary 2. Venous 3. Arterial External Bleeding There are 6 types of open wounds: 1. Abrasion 2. Laceration 3. Incision 4. Puncture 5. Avulsion 6. Amputation There are 7 steps to care for external bleeding. 1. Wear exam gloves 2. Expose the wound 3. Place a dressing 4. Elevate injury above heart 5. Apply a pressure bandage 6. If blood soaks through, add more bandages. 7. Apply pressure at pressure point if bleeding persists.
BLEEDING AND WOUNDS Internal Bleeding Wound Care Signs of internal bleeding include: Care for a minor wound: Bruising, painful tender areas, vomiting or coughing up blood, and stool that black or contains blood. Care for minor internal bleeding: R. I. C. E – Rest, ice, compression, elevation Wash with soap and water, flush wound, remove small objects, apply direct pressure, apply antibiotic ointment, cover the area with dressing, and seek medical attention for a wound with a high risk of infection. Care for serious internal bleeding: Signs of wound infection: Call 911, care for shock by raising legs 6 -12 inches, roll victim onto side if they are vomiting, monitor breathing. Swelling and redness, sensation of warmth, throbbing pain, pus discharge, fever, swollen lymph nodes, red streaks from wound to heart.
BLEEDING AND WOUNDS Special Wounds that require medical care Caring for amputations: Wounds that will not stop bleeding Call 911, control bleeding, care for shock, recover amputated part, wrap it in sterile gauze and in a waterproof container and keep it cool – do not freeze it. Long or deep cuts that need stitches Cuts over a joint Cuts that impair function Cuts that remove all layers of skin Care for impaled objects: Cuts from an animal or human bite Expose the area, do NOT remove the object, control bleeding with pressure, stabilize object, shorten the object of necessary. Damaged nerves, tendons, or joints Cuts over broken bones Cuts caused by crushing injuries Cuts caused by embedded objects Cuts caused by metal Puncture wounds
SHOCK –WHEN THE BODY’S TISSUE DOES NOT RECEIVE ENOUGH OXYGENATED BLOOD Signs of shock Altered mental status Agitation Anxiety Restlessness Confusion Cold, pale, clammy skin, nails, lips Nausea and vomiting Unresponsiveness Care Includes: Place victim on back Raise legs 6 -12 inches Place blankets under and over victim Anaphylaxis A severe allergic reaction caused by: Medications, food, insect stings or plants Signs of anaphylaxis include: Breathing difficulty, skin reaction, swelling of the tongue/mouth/throat, sneezing, coughing, tightness in chest, blueness around lips and mouth, dizziness, nausea and vomiting Care Includes: Call 911 Determine if victim has medication for their allergy Keep victim sitting up to promote breathing
ANY QUESTIONS? ?
BURNS –THERE ARE THREE CLASSIFICATIONS OF BURNS: THERMAL, CHEMICAL AND ELECTRICAL Thermal Burns First Degree Burn affects the skin’s outer layer and includes redness, mild swelling, tenderness and pain. Second Degree Burn extends to the inner layers of skin and includes blisters, swelling, weeping fluid and pain. Third Degree Burns penetrate all layers including fat and muscle.
BURNS Seek Care for Thermal Burns when the victim: Is younger than 5 or older than 55 Has difficulty breathing Other injuries exist Electrical injuries exist Face, hands, feet or genital are burned Child abuse is suspected Second degree larger than 20% of body Burn is third degree
BURNS Care for First Degree Burns: Cool burn with cold water Apply aloe vera or moisturizer Give ibuprofen Care for Second Degree Burns <20% body Remove clothing and jewelry Cool burn with cold water Apply antibiotic ointment Cover burn with dry, nonstick dressing Give ibuprofen Care for Second Degree Burns >20% body Monitor breathing Remove clothing or jewelry that is not stuck Cover burn with dry, non stick dressing Care for shock Seek medical care.
BURNS Chemical Burns – when a caustic or corrosive substance touches the skin Examples – battery acid, harsh cleaning supplies Care for a chemical burn Flush area with water Remove clothing and jewelry Cover affected area with dry dressing Seek medical care Electrical Burns – types and cause are thermal burns (flame), arc burn (flash), and true electrical injury (contact) Care for Electrical Burns Unplug or turn off power Monitor breathing Check for possible spinal injury Care for shock Call 911 for medical care

HEAD AND SPINAL INJURIES Scalp wounds – result in heavy bleeding Care for scalp wounds Apply a sterile dressing and direct pressure Head and shoulders need to be slightly elevated Seek medical care Skull fracture – results from a significant force to the skull Signs of skull fracture Pain at the point of injury Deformity of the skull Drainage of fluids from nose or ears Bruising under the eyes or behind the ear Changes in pupils Heavy scalp bleeding Penetrating wound Care for Skull Fracture Monitor breathing Control bleeding Stabilize head and neck Seek medical care
CONCUSSION – A TEMPORARY DISTURBANCE OF BRAIN ACTIVITY, CAN BE CAUSE BY A BLOW TO THE HEAD Signs of brain injury include: Care for brain injury: Befuddled facial expression Slowness in answering questions Monitor breathing and provide care if necessary Unaware of where they are Stabilize head and neck Slurred speech Control any scalp bleeding Crying for no reason If vomiting turn victim on their side Inability to recite months of the year in reverse Seek medical care Unresponsiveness Complaints of headache, dizziness and nausea
EYE INJURIES Care for eye injuries: Lift the upper lid over the lower lid, so the lashes can brush object out Hold eyelid open and wash with warm water Examine the lower lid by pulling it down gently Examine the underside of the upper lid. If you can see the object, remove it gently. Care for penetrating eye injury: Stabilize embedded object with bulky dressing Have victim keep eye closed Call 911 Care for a blow to the eye: Apply ice for 15 min (NOT directly on eyeball Seek medical care if there is pain, double vision or reduced vision
EYE CARE Care for cuts of the eye: Do not apply direct pressure Keep victim’s eye closed Seek medical care Care for chemicals in the eye: Flush with warm water for 20 minutes Loosely bandage eyes with wet dressings Seek medical care Care for burns of the eye from light: Cover both eyes with wet dressings and cold packs Seek medical care
NOSE INJURIES – TWO TYPES ARE ANTERIOR AND POSTERIOR Care for a nosebleed: Tilt victim’s head slightly FORWARD Pinch soft parts with steady pressure Seek medical care Recognize a broken nose: Pain, swelling and crooked nose Bleeding and breathing difficulty Black eyes appear 1 -2 days after injury Care for a broken nose: Provide care as a nosebleed Apply icepack Seek medical care
SPINAL INJURIES Common signs of spinal injuries: Inability to move arms or legs Numbness, tingling, weakness or burning sensation Deformity Neck or back pain Care for spinal injuries: Stabilize head and neck to prevent movement (Do NOT MOVE VICTIM to do this!) Open airway, check for breathing Call 911
CHEST INJURIES Closed chest injury: when the victims skin is not broken Open Chest Injury: When the skin is broken and the chest wall is penetrated. Flail Chest: When several ribs in the same area are broken in more than one place. Signs of rib fracture: Sharp pain Shallow breathing Victim holds injured area Care for rib fractures: Help victim find comfortable position Stabilize the ribs Seek medical care Care for embedded object in chest: Do NOT remove object Use bulky dressings to stabilize object Call 911
ABDOMINAL INJURIES Closed Abdominal Injury: When there is a direct blow from a blunt object. Care: Place victim in comfortable position, care for shock and seek medical care Open Abdominal Injury: Penetrating wounds, embedded objects and protruding organs. Care: Comfortable position with legs upward, Cover loosely with dressings, care for shock, call 911 Pelvic Injuries Usually caused by a motor vehicle crash or fall from a height Signs: pain that increases with movement, inability to walk or stand, signs of shock Care: Keep victim still, care for shock, call 911
PELVIC INJURIES Usually caused by a motor vehicle crash or fall from a height Signs: pain that increases with movement, inability to walk or stand, signs of shock Care: Keep victim still, care for shock, call 911
REVIEW
ROLE PLAY – TEAMS OF 6 You will be assigned a scenario from any of the subjects that we have covered. You must create a First Aid plan of action to help your victim(s). You will be doing a 10 minute presentation after the break. Everyone has a role and must participate. Work with each other and with your notes to figure out the best First Aid care to give. 6 people on a team Director (in command of the presentation) Author (write down the plan of action) Narrator (tell us what is going on and what First Aid care is happening to fix the problem. 2 First Aid Responders (must be the ones giving the first aid correctly. ) 1 Victim (has all the injuries) BE CREATIVE and HAVE FUN!