JUNIORSENIOR HEALTH FIRST AID AND CPR GOOD SAMARITAN
- Slides: 21
JUNIOR/SENIOR HEALTH: FIRST AID AND CPR
GOOD SAMARITAN LAWS • Legal protections exist in the U. S. for someone who decides to act in an emergency. • Good Samaritan laws were enacted to give legal protection to people who willingly provide emergency care to ill or injured persons without expecting anything in return. • These laws are designed to encourage people to help others in an emergency situation. 2
GOOD SAMARITAN LAWS (CONTINUED) • They require that “Good Samaritans” -* Use common sense and a reasonable level of skill * Not exceed the scope of their training in emergency situations * Do their best to save a life or prevent further injury. Good Samaritan laws vary from state to state. 3
OBTAINING CONSENT • Obtaining consent is another protection for someone who responds to a first aid emergency. Obtaining consent means the victim accepts your offer to help him/her. • You must get consent before caring for a conscious victim. • To get consent – 1. 2. 3. 4. 5. State your name Tell the victim you are trained in first aid Ask the victim if you can help Explain what you think may be wrong Explain what you plan to do 4
OBTAINING CONSENT (CONTINUED) • If the victim does not give consent, do not give care. Instead, call 9 -1 -1 • A victim who is unconscious, confused, or seriously ill may not be able to grant consent. • In such cases, consent is implied. Implied consent means that victims would agree to the care if they could. 5
RECOGNIZING AN EMERGENCY UNUSUAL NOISES: • Screams, yells, moans or calls for help • Breaking glass, crashing metal or screeching tires • Changes in machinery or equipment noises • Sudden loud voices 6
RECOGNIZING AN EMERGENCY (Continued) UNUSUAL SIGHTS: 1. A stalled vehicle 2. 3. 4. 5. 6. An overturned pot A spilled medicine container Broken glass Downed electrical wires Smoke or fire 7
RECOGNIZING AN EMERGENCY (Continued) UNUSUAL ODORS: 1. Odors that are stronger than usual 2. Unrecognizable odors 3. Smell of something burning 8
RECOGNIZING AN EMERGENCY (Continued) UNUSUAL APPEARANCES OR BEHAVIORS: · · · 1. 2. 3. 4. 5. 6. Trouble breathing Clutching of the chest or throat Slurred, confused or hesitant speech Unexplainable confusion or drowsiness Sweating for no apparent reason Unusual skin color 9
EMERGENCY ACTION STEPS CHECK: 1. The scene: a. Is it safe? b. What happened? c. Are there any bystanders that can help? 2. The victim: a. Checking for consciousness * TAP and SHOUT, “Are you okay? ” 10
EMERGENCY ACTION STEPS (Continued) CALL: 1. 9 -1 -1 or the local emergency number 2. Be specific in what you tell the dispatcher a. b. c. d. Your Name Specific Location Condition of Victim What care has been given to victim 3. Never hang up until the dispatcher tells you to do so. 11
EMERGENCY ACTION STEPS (Continued) CARE: * Care for the conditions you find!! 12
Preventing Disease Transmission • What precautions could you take to protect yourself from disease transmission when giving care? ? 1. Avoid contact with a. Blood b. Body fluids 2. Use protective equipment, such as a. Disposable gloves b. Breathing barriers 3. Wash hands immediately after giving care The risk of getting a disease while giving care is extremely low, and taking basic precautions can reduce the risk even further. 13
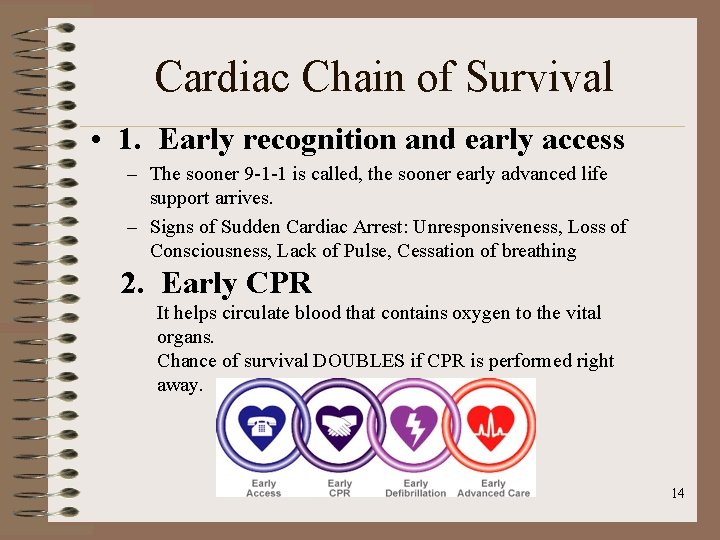
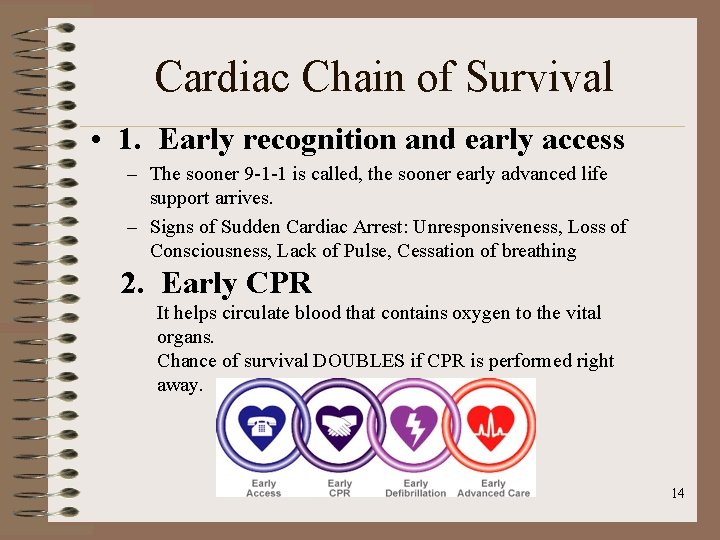
Cardiac Chain of Survival • 1. Early recognition and early access – The sooner 9 -1 -1 is called, the sooner early advanced life support arrives. – Signs of Sudden Cardiac Arrest: Unresponsiveness, Loss of Consciousness, Lack of Pulse, Cessation of breathing 2. Early CPR It helps circulate blood that contains oxygen to the vital organs. Chance of survival DOUBLES if CPR is performed right away. 14
Cardiac Chain cont… • 3. Early defibrillation (Critical Link) Most victims of sudden cardiac arrest need an electric shock called defibrillation. Each minute it is delayed = reduces chance of survival by 10% 4. Early advanced life support Given by trained medical personnel who provide further care and transport to hospital facilities. 15
Each link of the chain depends on and is connected to the other links! Very important = start CPR and continue until an AED is available or EMS arrive. 16
Preventing Heart Disease • Five Risk Factors associated with Cardiovascular Disease 1. Smoking 2. Diet 3. Exercise 4. Blood Pressure 5. Weight 17
CHECKING A VICTIM When checking a victim, you will follow the ABC’S A: Airway - Is the airway blocked? B: Breathing - Is the victim breathing? C: Circulation - Does the victim show SIGNS OF LIFE? S: Severe Bleeding - Is there any bleeding that needs immediate attention? 18
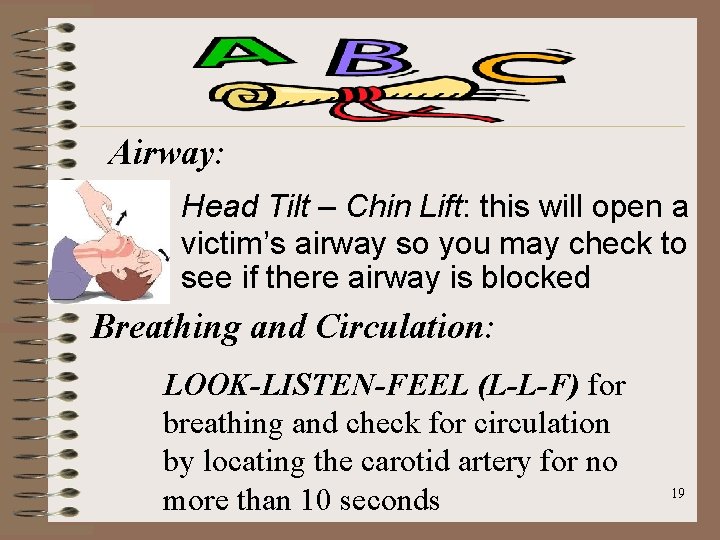
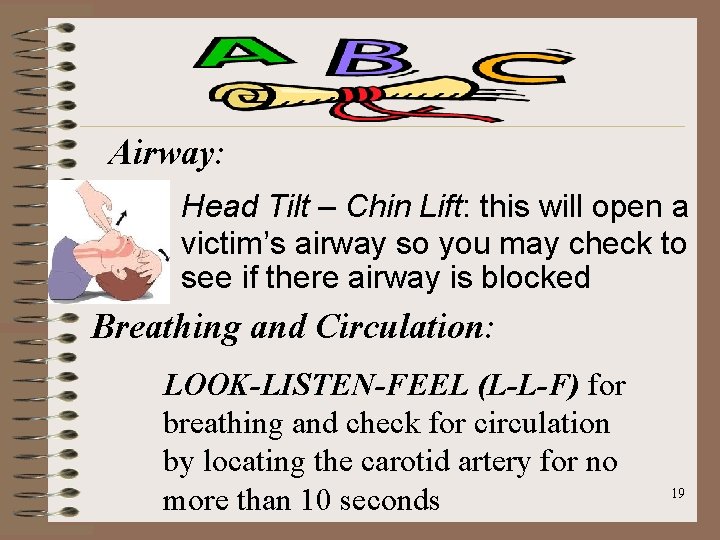
Airway: Head Tilt – Chin Lift: this will open a victim’s airway so you may check to see if there airway is blocked Breathing and Circulation: LOOK-LISTEN-FEEL (L-L-F) for breathing and check for circulation by locating the carotid artery for no more than 10 seconds 19
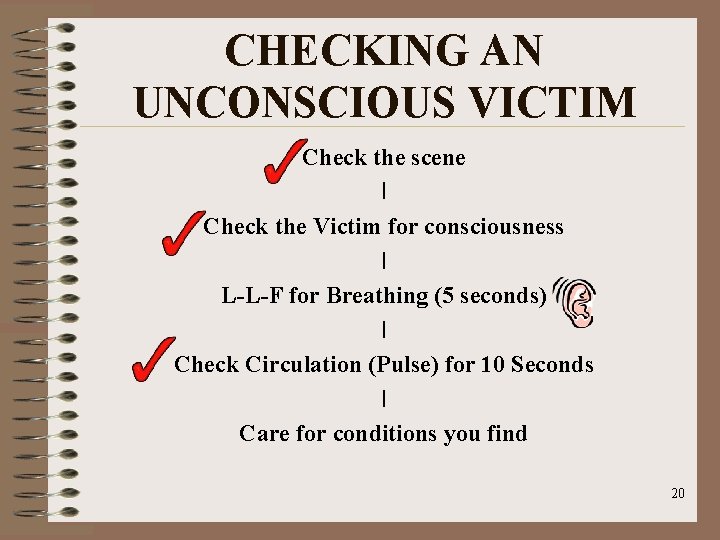
CHECKING AN UNCONSCIOUS VICTIM Check the scene I Check the Victim for consciousness I L-L-F for Breathing (5 seconds) I Check Circulation (Pulse) for 10 Seconds I Care for conditions you find 20
CONDITIONS YOU MAY BE EXPOSED TO What will you do if the victim has: 1. NO Breathing but a Pulse 2. NO Breathing and NO Pulse 3. Breathing and NO Pulse 4. Breathing and a Pulse 21