GRAMPOSITIVE COCCI 26 12 2021 1 FAMILIES n


- Slides: 20

GRAMPOSITIVE COCCI 26. 12. 2021 1
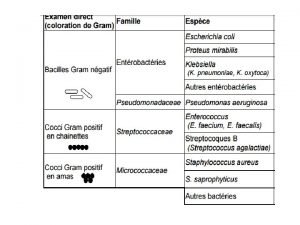
FAMILIES: n n n 26. 12. 2021 Staphylococcaceae Cluster-forming cocci, nonmotile, catalase-positive Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus saprophyticus Streptococcaceacae Chain-forming cocci and diplococci, nonmotile, catalase-negative Streptococcus pyogenes, Streptococcus pneumoniae, Streptococcus agalactiae „Enterococcaceae“ Chain-forming cocci and diplococci, a-, b-, or g-hemolysis, group antigen D, catalase-negative Enterococcus fecalis, Enterococcus faecium 2
Staphylococci n n n Can be cultured on normal nutrient media both aerobically and anaerobically. Small spherical cells (1 mm) forming grape-like clusters, nonmotile Producers of number of toxins (extracellular enzymes and exotoxins Genus Staphylococcus includes over 30 species and subspecies Human infections (hospital-acquired infections) 26. 12. 2021 3
Staphylococcus aureus n n n Coagulase-positive, facultatively anaerobic Cultures on blood agar at 37°C, hemolytic zones The cell wall consists of a thick layer of murein. Linear teichoic acids and polysaccharides are covalently coupled to the murein polysaccharide. The lipoteichoic acids permeating the entire murein are anchored in the cell membrane. Teichoic and lipoteichoic acids can trigger activation of complement by alternative pathway and stimulate macrophages to secrete cytokines. Cell wall-associated proteins are bound to the peptide components of murein. Clumping factor, fibronectin-binding protein and collagenbinding protein bind specifically to fibrinogen, fibronectin and collagen resp. And are instrumental in adhesion to tissues and foreign bodies covered with the appropriate matrix protein 26. 12. 2021 4
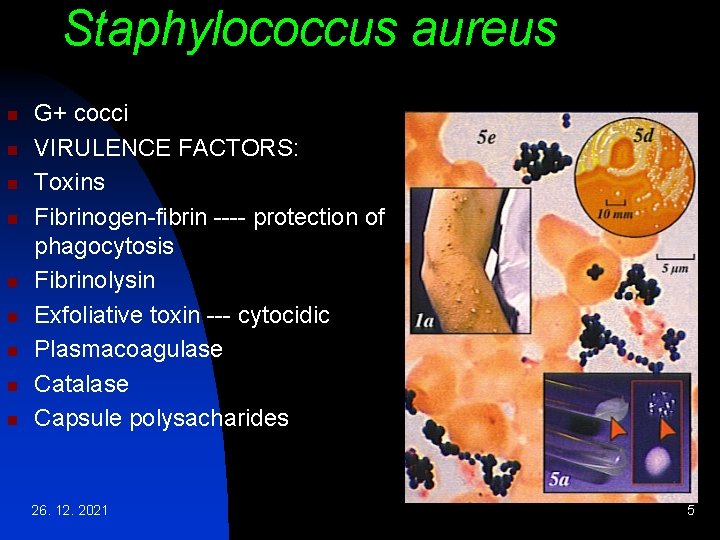
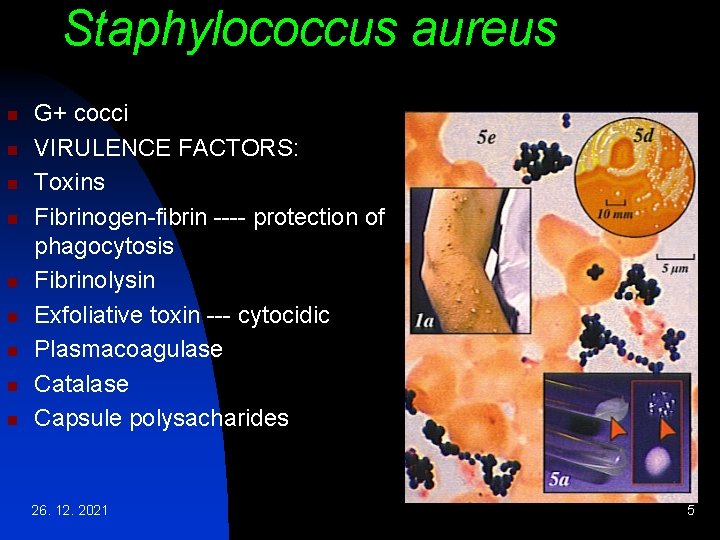
Staphylococcus aureus n n n n n G+ cocci VIRULENCE FACTORS: Toxins Fibrinogen-fibrin ---- protection of phagocytosis Fibrinolysin Exfoliative toxin --- cytocidic Plasmacoagulase Catalase Capsule polysacharides 26. 12. 2021 5
S. aureus - continued n n n Protein A binds to the Fc portion of immunoglobulins (Ig. G). It is assumed that „false“ binding of Ig. G by protein A prevents correct binding of opsonizing antibodies, thus hindering phagocytosis EXTRACELLULAR TOXINS AND ENZYMES: Plasma-coagulase – converts fibrinogen to fibrin (like thrombin) a-toxins – lethal CNS effects, membrane damage --hemolysis, dermonecrosis Leucocidin – degranulation of macrophages and microphages Exfoliatins - epidermolysis 26. 12. 2021 6
S. aureus - continued n n Enterotoxins A-E, G and I – 35 k. Da proteins are not inactivated by heating to 100°C for 15 -30 min. Superantigens. --- Food poisoning TSST-1 (Toxic Shock Syndrome Toxin) – produced by 1% of strains. Superantigen inducing clonal expansion of 10% T lymphocyte types, leading to massive production of cytokines --- rise to clinical symptoms of toxic schock PATHOGENESIS AND CLINICAL PICTURES: n Invasive infections – pathogens tend to remain in situ after penetrating through the derma and mucosa and to cause infections characterized by purulence – furuncles, carbuncles, wound infections, sinusitis, mesotitis, mastitis puerperalis 26. 12. 2021 7 n
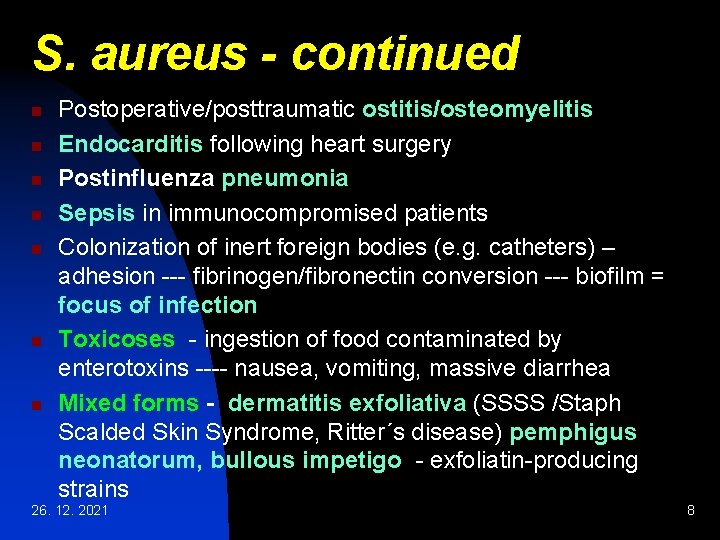
S. aureus - continued n n n n Postoperative/posttraumatic ostitis/osteomyelitis Endocarditis following heart surgery Postinfluenza pneumonia Sepsis in immunocompromised patients Colonization of inert foreign bodies (e. g. catheters) – adhesion --- fibrinogen/fibronectin conversion --- biofilm = focus of infection Toxicoses - ingestion of food contaminated by enterotoxins ---- nausea, vomiting, massive diarrhea Mixed forms - dermatitis exfoliativa (SSSS /Staph Scalded Skin Syndrome, Ritter´s disease) pemphigus neonatorum, bullous impetigo - exfoliatin-producing strains 26. 12. 2021 8
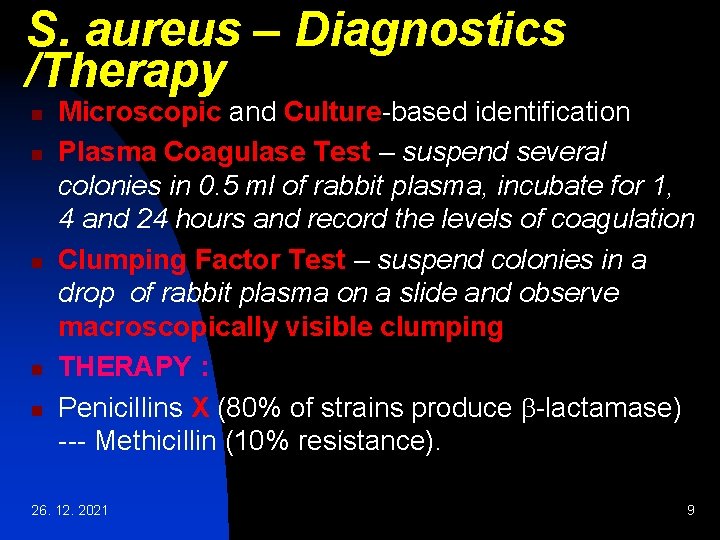
S. aureus – Diagnostics /Therapy n n n Microscopic and Culture-based identification Plasma Coagulase Test – suspend several colonies in 0. 5 ml of rabbit plasma, incubate for 1, 4 and 24 hours and record the levels of coagulation Clumping Factor Test – suspend colonies in a drop of rabbit plasma on a slide and observe macroscopically visible clumping THERAPY : Penicillins X (80% of strains produce b-lactamase) --- Methicillin (10% resistance). 26. 12. 2021 9

Coagulase-negative Staphylococci Element in the normal flora of human skin and mucosa. Classic opportunists – cause infection given a certain host disposition only. n Staphylococcus epidermidis - (70 -80% of infections) foreign body infections (intravasal catheters, continuous ambulant peritoneal dialysis catheters, endoprotheses, metal plates and screws in osteosynthesis, cardiac pacemakers, artificial heart valves, shunt valves. Coverage of foreign bodies by matrix proteins (fibrinogen/ fibronectin) supports infection. STAPHYLOCOCCI WITHIN BIOFILM ARE PROTECTED FROM ANTIBIOTICS AND THE IMMUNE SYSTEM! MAY BECOME INFECTION FOCI ---bloodstream ---- Sepsis-like illnesses Staphylococcus saprophyticus – responsible for up to 20% of acute urinary tract infections, particular dysuria of young women, small proportion of nonspecific urethritis in young men 26. 12. 2021 10
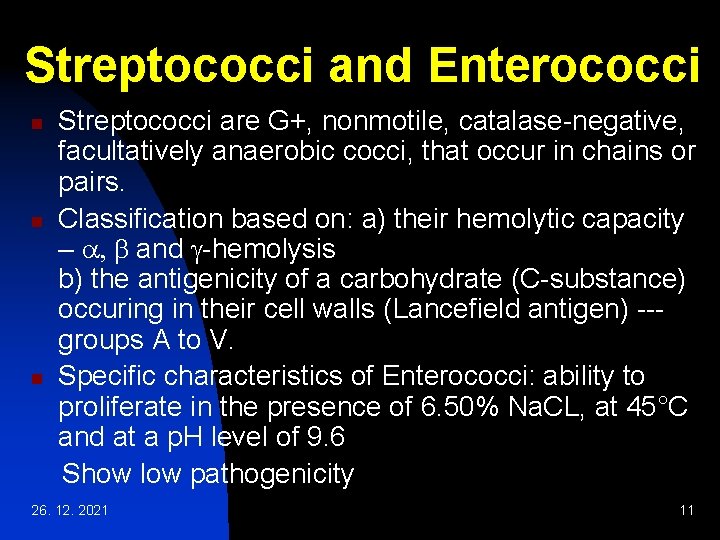
Streptococci and Enterococci n n n Streptococci are G+, nonmotile, catalase-negative, facultatively anaerobic cocci, that occur in chains or pairs. Classification based on: a) their hemolytic capacity – a, b and g-hemolysis b) the antigenicity of a carbohydrate (C-substance) occuring in their cell walls (Lancefield antigen) --groups A to V. Specific characteristics of Enterococci: ability to proliferate in the presence of 6. 50% Na. CL, at 45°C and at a p. H level of 9. 6 Show low pathogenicity 26. 12. 2021 11
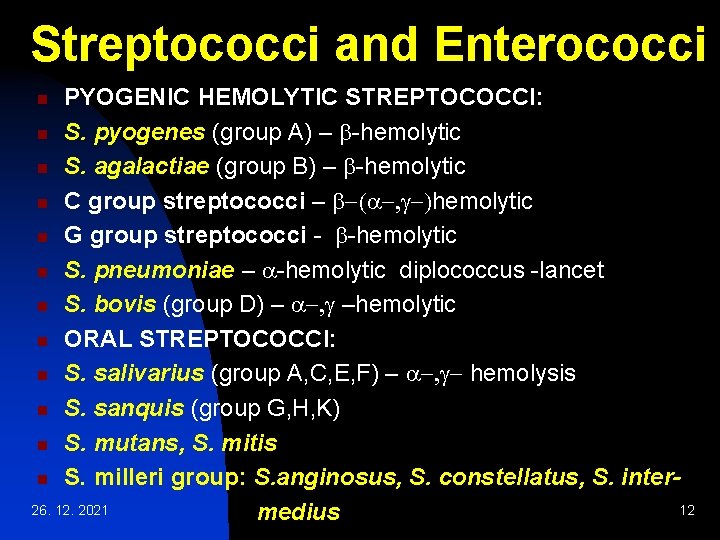
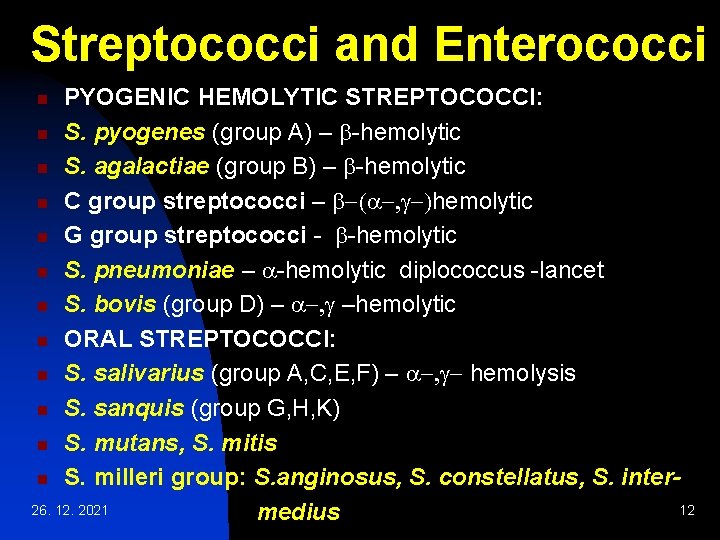
Streptococci and Enterococci PYOGENIC HEMOLYTIC STREPTOCOCCI: n S. pyogenes (group A) – b-hemolytic n S. agalactiae (group B) – b-hemolytic n C group streptococci – b-(a-, g-)hemolytic n G group streptococci - b-hemolytic n S. pneumoniae – a-hemolytic diplococcus -lancet n S. bovis (group D) – a-, g –hemolytic n ORAL STREPTOCOCCI: n S. salivarius (group A, C, E, F) – a-, g- hemolysis n S. sanquis (group G, H, K) n S. mutans, S. mitis n S. milleri group: S. anginosus, S. constellatus, S. inter 26. 12. 2021 12 medius n
Streptococci and Enterococci n n n ENTEROCOCCI: Enterococcus faecalis (group D) a-, b-, g-hemolytic Enterococcus faecium (group D) a- hemolytic a-hemolysis – colonies on blood agar are surrounded by a green zone. Greening caused by H 2 O 2, which converts hemoglobin into methemoglobin b-hemolysis - colonies on blood agar are surrounded by a large, yellowish hemolytic zone (complete) g-hemolysis – absence of macroscopically visible hemolysis 26. 12. 2021 13
S. pyogenes (group A streptococci) G+ cocci (diameter 1 mm) form chains. Colonies on blood agar show b-hemolysis caused by streptolysins The murein layer of the cell wall is followed by the serogroup A polymeric carbohydrate layer, consisting of C substance covalently bound to murein. Long, twisted protein threads that extend outward are anchored in the cell wall murein : Mprotein. Group A streptococci are classified in serovars with characteristic M-protein chemistry. Like the hyaluronic acid capsules seen in some strains, the M-protein has an antiphagocytic effect. 26. 12. 2021 14
S. pyogenes (Group A streptococci) n n n EXTRACELLULAR TOXINS AND ENZYMES: Streptolysin O, streptolysin S - destroy the membranes of erythrocytes and other cells. Streptolysin O acts as an antigen. Past infection can be detected by measuring antibodies to this toxin – ASLO PSE (Pyrogenic Streptococcal Exotoxins) A, B, C – responsible for fever, scarlet fever exanthem and enanthem, sepsis and septic shock. As superantigens induce production of large amounts of cytokines Streptokinase – dissolves fibrin: facilitates spread of streptococci in tissues Hyaluronidase – breaks down a substance that cements tissue together DNAses – breakdown of DNA producing runny pus 26. 12. 2021 15
S. pyogenes (Group A streptococci) n n PATHOGENESIS AND CLINICAL PICTURE: Invasive infections. Bacteria enter through traumas and microtraumas in skin or mucosa and cause invasive localk or generalized infections. The rare cases of severe septic infection and necrotizing fasciitis occur in persons with a high-risk MHCII-allotype: in these patients PSEA superantigens induce large amount of cytokines by binding at the same time to the MHCII-complex and the b-chain of the T-cell receptor. The excess cytokines thus produced are the cause of symptoms. 26. 12. 2021 16
S. pyogenes (Group A streptococci) n n n Sequelae – glomerulonephritis is an immune complex disease and acute rheumatic fever may be a type II immune disease. Local infections - impetigo, erysipelas, cellulitis, lymphangitis, sinusitis, tonsillitis, otitis media. If anti. PSE antibodies not present ----- scarlet fever DIAGNOSTICS AND THERAPY: Microscopy and culturing, Latex-agglutination test (direct detection of A streptococci in tonsillitis) Differentiation of A streptococci: bacitracin disk test 26. 12. 2021 17
S. pyogenes – Therapy and Epidemiology n n n Therapy: agents of choice: Penicillin G and V, resistance unknown Alternatives: oral cephalosporins or macrolides In treatment of septic shock: polyvalent immunoglobulin to inactivate PSE Epidemiology: Infection frequency varies according to geographical area, season, age. Humans are the only pathogen reservoir. Transmission: direct contact or droplets Incubation period: 1 to 3 days Incidence: 10 -20% 26. 12. 2021 18
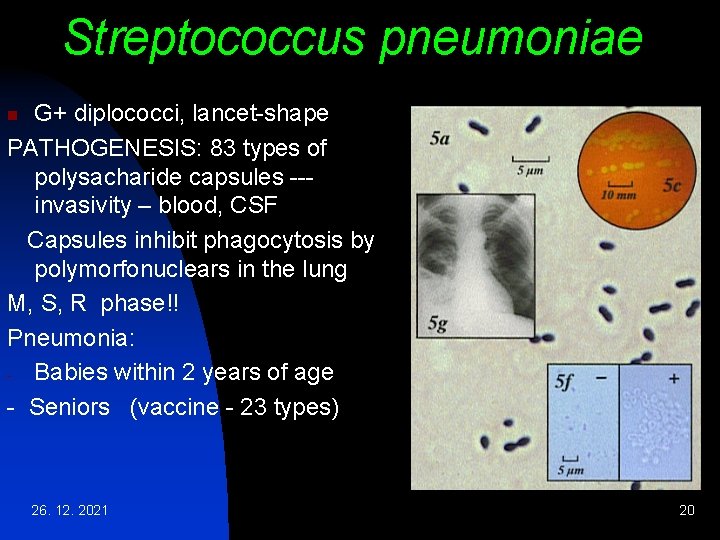
Streptococcus pneumoniae n n n G+, oval to lancet-shape cocci, usually occur in pairs (diplococcus) or short chains. The cells are surrounded by a thick capsule Cultures on blood agar: a-hemolytic colonies with mucoid ( M-form ) or smooth ( shiny) appearence ( S-form). Mutants without capsules produce colonies with a rough surface (R-form) Pneumococci are classified in 90 different serovars based on the fine chemical structure of the caspsule polysaccharides acting as antigens 26. 12. 2021 19
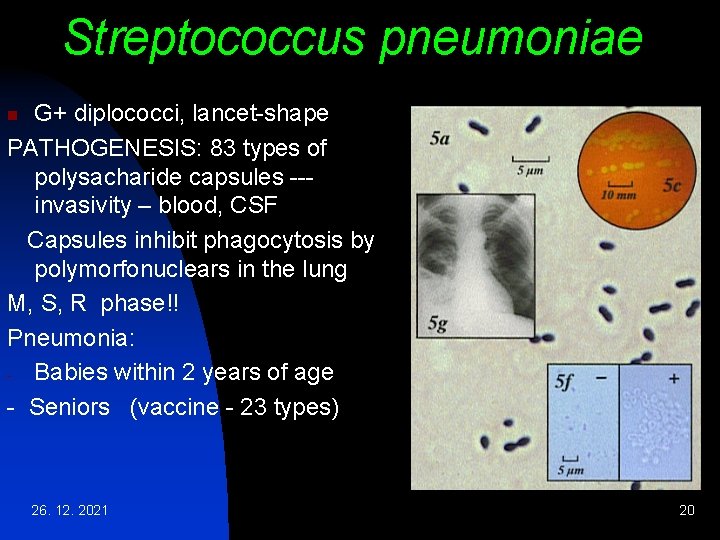
Streptococcus pneumoniae G+ diplococci, lancet-shape PATHOGENESIS: 83 types of polysacharide capsules --invasivity – blood, CSF Capsules inhibit phagocytosis by polymorfonuclears in the lung M, S, R phase!! Pneumonia: - Babies within 2 years of age - Seniors (vaccine - 23 types) n 26. 12. 2021 20
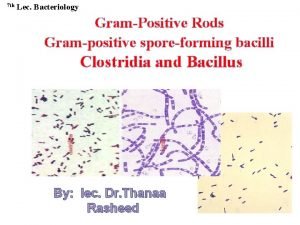
 Grampositive rods
Grampositive rods Big families vs small families
Big families vs small families Qcm cocci gram positif
Qcm cocci gram positif Gram positive grape like clusters
Gram positive grape like clusters Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli Cocci
Cocci Sarcinae
Sarcinae Cocci gram + en amas
Cocci gram + en amas Rods or cocci
Rods or cocci Biochemical test
Biochemical test Folliculitis carbuncle furuncle
Folliculitis carbuncle furuncle Coccobacilli
Coccobacilli Gram positive cocci in urethral discharge
Gram positive cocci in urethral discharge Curb-65
Curb-65 Agar
Agar Marriages and families changes choices and constraints
Marriages and families changes choices and constraints Fragrance family chart
Fragrance family chart Work and families act 2006
Work and families act 2006 Involving families in the assessment process
Involving families in the assessment process Georgia department of children and families
Georgia department of children and families Characteristics of logic
Characteristics of logic