Glomus tumor DR MADHU PRIYA 2 nd Most

- Slides: 13
Glomus tumor DR MADHU PRIYA
• 2 nd Most common benign neoplasm of middle ear • Also known as chemodectomas/ paragangliomas • Origin from glomus bodies/derived from paraganglionic cells derived from neural crest • Found in the dome of jugular bulb or promontory or along the course of tympanic branch of IX cranial nerve or the auricular branch of vagus, their position in the temporal bone is highly variable. • Two types: GLOMUS TYMPANICUM GLOMUS JUGULARE
Aetiopathogenesis • Histologically, they resemble carotid body. It contains epitheloid cells interspaced in a highly vascular stroma of capillary and precapillary vessels. • Non or thinly encapsulated, extremely vascular neoplasm • Abundance of thin blood sinusoids with no contractile muscle coat • BIOPSY CONTRAINDICATED
• Incidence: Glomus jugulare occurs in about 1 in 100000 patients, female preponderance-6 times Hereditary pattern: It shows autosomal dominant inheritance Endocrine activity: Even though these tumors are considered non chromaffin paragangliomas with no endocrine activity, some cases with endocrine activity by these tumors have been reported. It is hence important to look for evidence of endocrine activity by urine estimation of VMA (Vanillylmandelic acid).
• Locally invasive tumour • Along the path of least resistance tumour may initially fill the middle ear and later • perforate through the tympanic membrane to present as a vascular polyp. • It may invade labyrinth, petrous pyramid and the mastoid. • By spread through eustachian tube, it may present in the nasopharynx. • It may invade jugular foramen and the base of skull, causing IXth to Xllth cranial nerve palsies. • It may spread intracranially to the posterior and middle cranial fossae. • Metastatic spread to lungs and bones is rare, but seen in 4% of cases.
Clinical features • Depends upon the type • Glomus tympanicum – pertaining to ear (90%) • Glomus jugulare – neurological signs
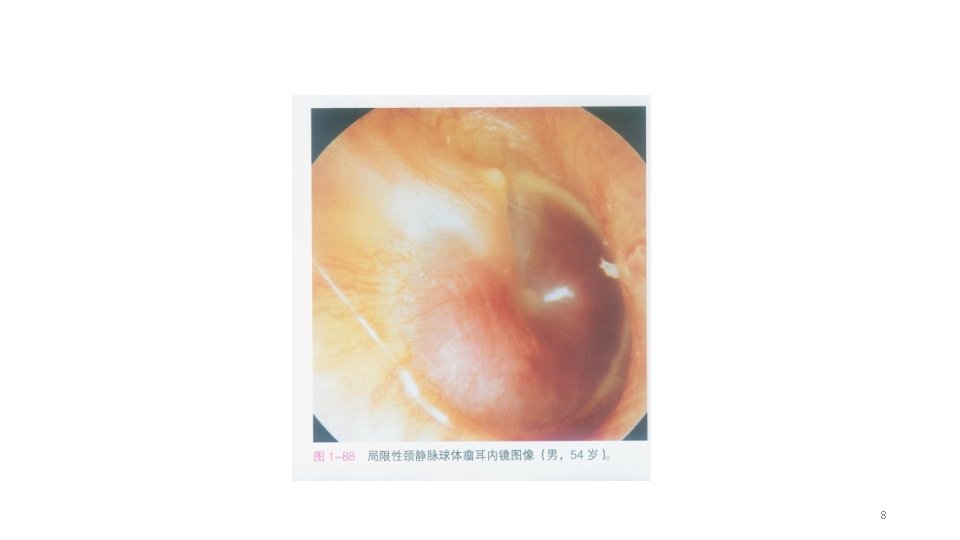
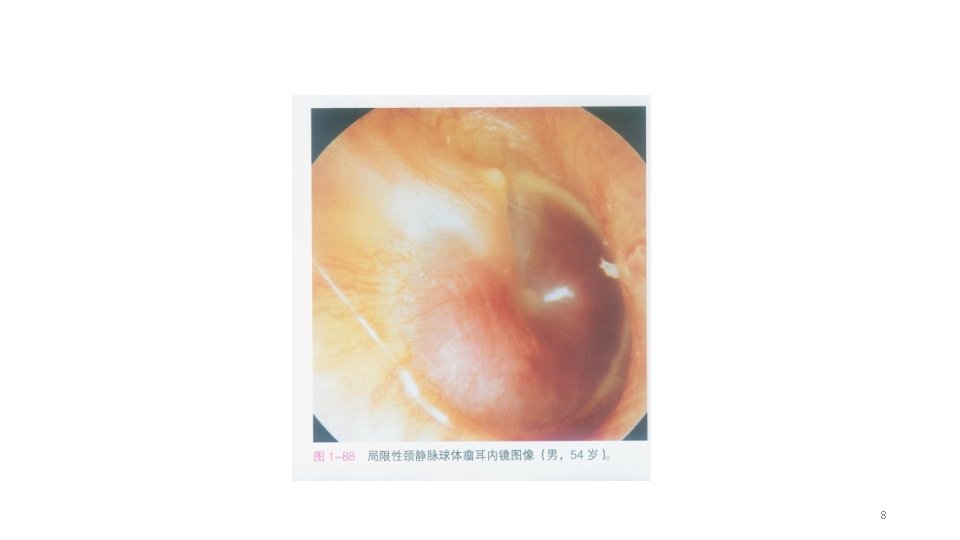
CLINICAL PRESENTATION • SYMPTOMS & SIGNS : • • Presenting symptoms, in order of decreasing frequency, were: pulsatile tinnitus hearing loss aural pressure/fullness vertigo/dizziness otalgia and bloody otorrhea The Brown sign, which consists of a pulsatile purple-red middle ear mass that blanches with positive pneumatic otoscopy, was seen in less than 10% of patients.
8
9

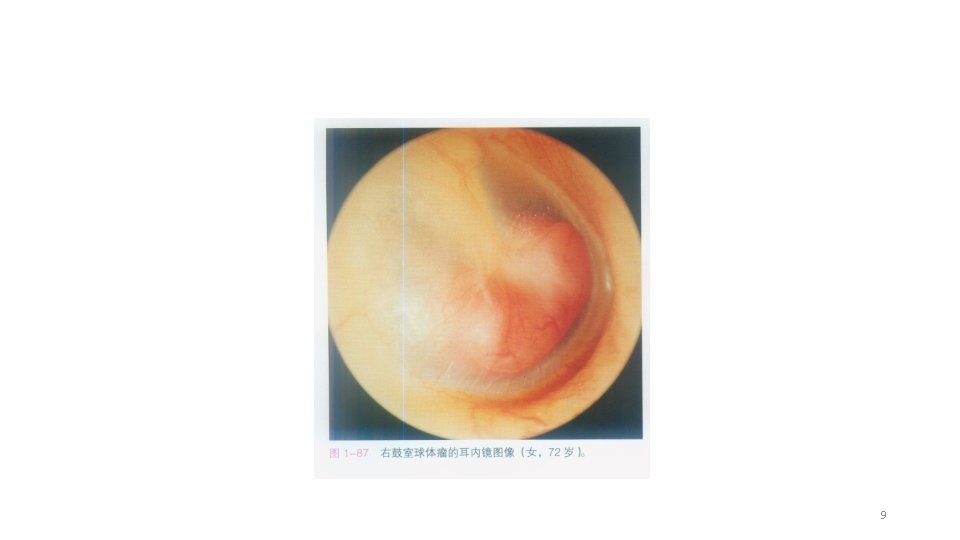
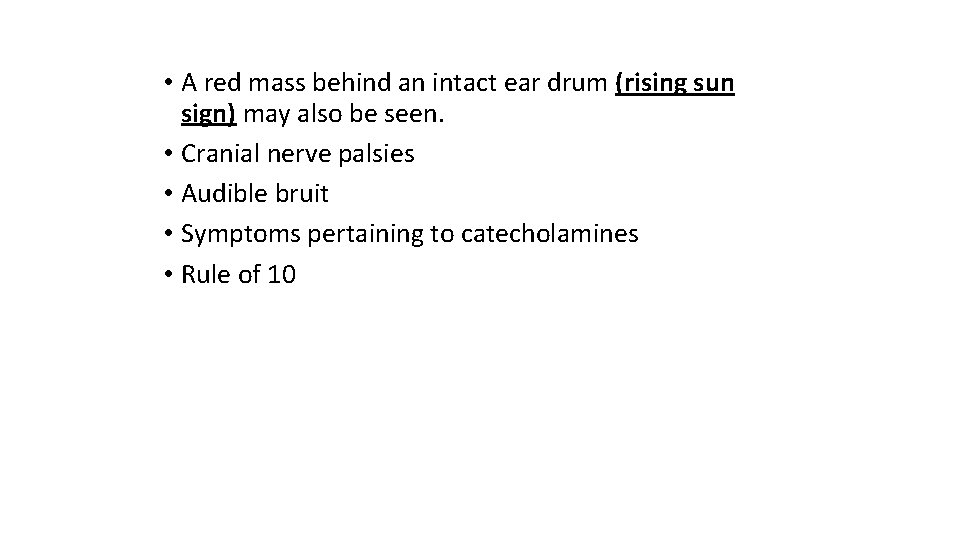
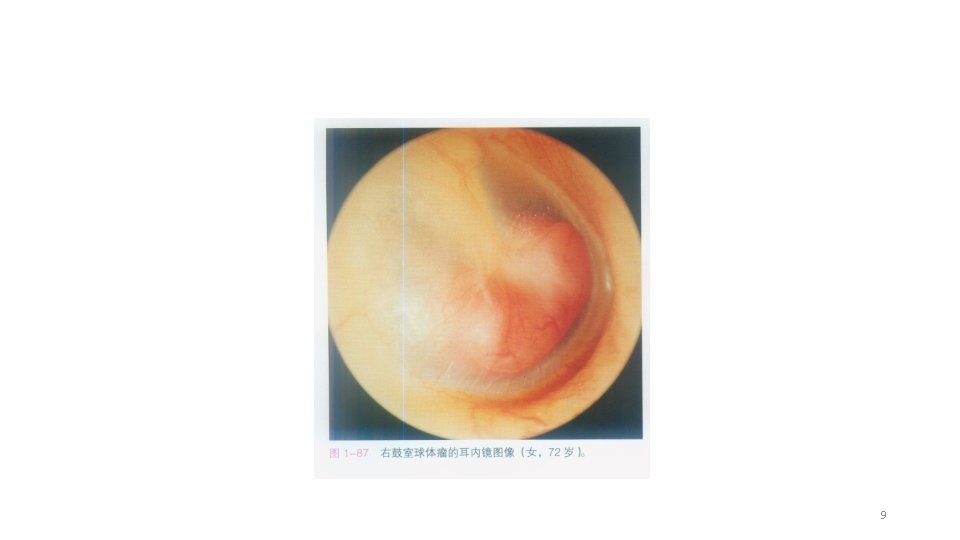
• A red mass behind an intact ear drum (rising sun sign) may also be seen. • Cranial nerve palsies • Audible bruit • Symptoms pertaining to catecholamines • Rule of 10
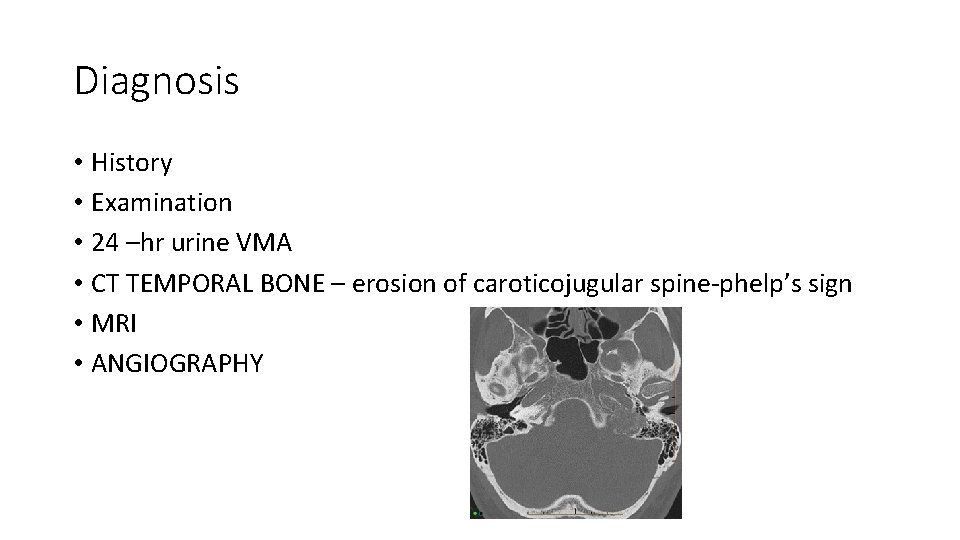
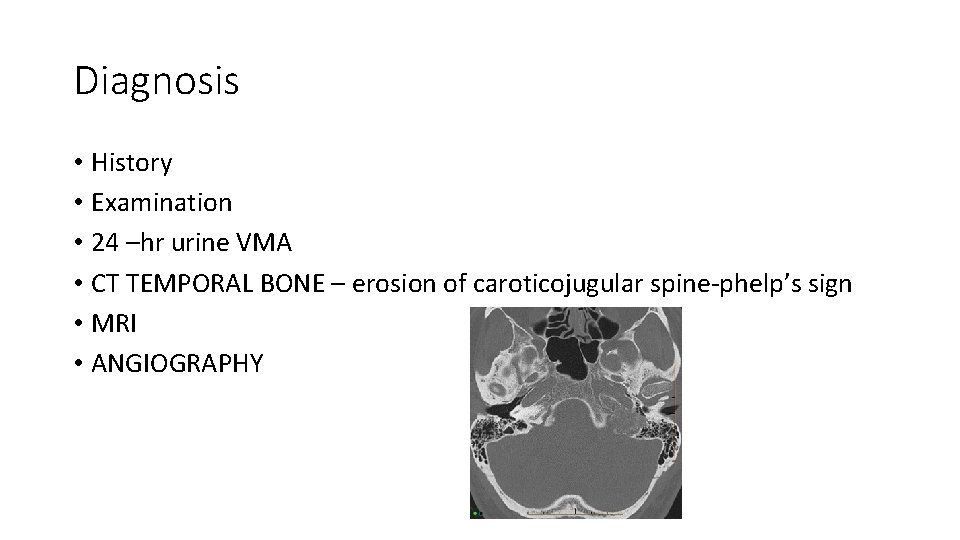
Diagnosis • History • Examination • 24 –hr urine VMA • CT TEMPORAL BONE – erosion of caroticojugular spine-phelp’s sign • MRI • ANGIOGRAPHY
TREATMENT • It consists of: • 1. Surgical removal. • 2. Radiation. • 3. Embolisation. • 4. Combination of the above techniques. • Depending on the extent of tumour, surgical removal • may be done through transmeatal, transmastoid or skull base approach.