Tumor immunology Tumor antigens a Tumor specific antigens


- Slides: 45
Tumor immunology
Tumor antigens a) Tumor – specific antigens (TSA) complexes of MHCgp I with abnormal fragments of cellular proteins (chemically induced tumors, leukemia with chromosomal translocation) complexes of MHC gp with fragments of oncogenic viruses proteins (tumors caused by viruses: EBV, SV 40, polyomavirus…) abnormal forms of glycoproteins (sialylation of surface proteins of tumor cells) idiotypes of myeloma and lymphoma (clonotyping TCR and BCR)
Tumor antigens b) Tumor - associated antigens (TAA) present also on normal cells differences in quantity, time and local expression auxiliary diagnostic markers
Tumor - associated antigens (TAA) onkofetal antigens -on normal embryonic cells and some tumor cells -fetoprotein (AFP) - hepatom carcinoembryonic antigen (CEA) - colon cancer melanoma antigens - MAGE-1, Melan-A
Tumor - associated antigens (TAA) antigen HER 2/neu eceptor for epithelial growth factor, mammary carcinoma EPCAM – epithelial cell adhesion molecule, metastases differentiation antigens of leukemic cells - present on normal cells of leukocytes linage CALLA -acute lymphoblastic leukemia (CD 10 pre-B cells)
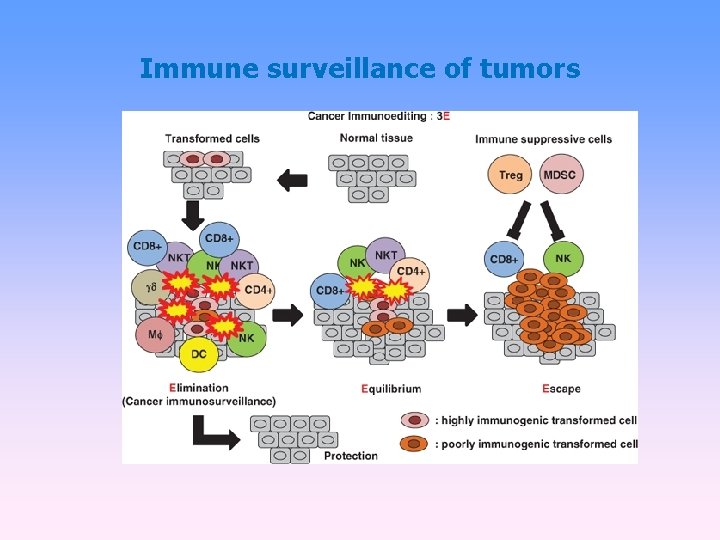
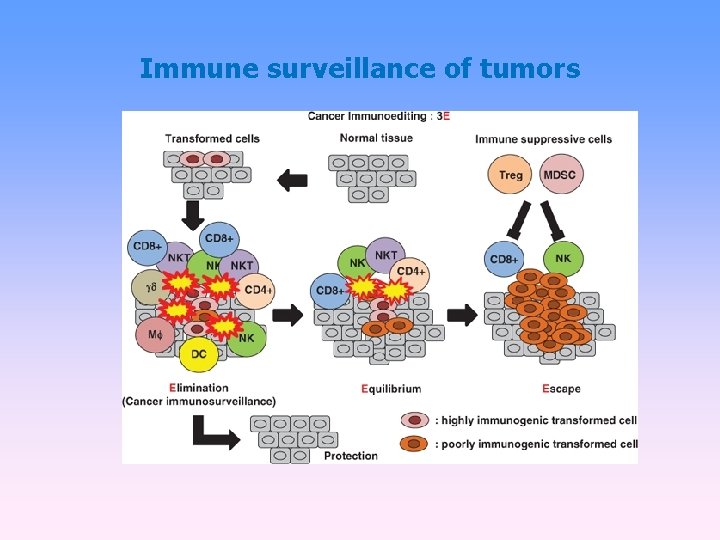
Immune surveillance of tumors
Anti-tumor immune mechanisms If tumor cells are detected, in defense may be involved non-specific mechanisms (neutrophilic granulocytes, macrophages, NK cells, complement) and antigen-specific mechanisms (TH 1 and TC cells, antibodies).
Anti – tumor defense tumor cells are weakly immunogenic regulatory T cells promote progression of cancer occurs when tumor antigens are presented to T cells by dendritic cells activated in the inflammatory environment
Anti – tumor defense DC are necessary for activation of antigen specific mechanisms predominance of TH 1 (IFN , TNF ) specific cell-mediated cytotoxic reactivity – TC activation of TH 2 → stimulation of B cells→ tumor specific antibodies production (involved in the ADCC) tumor cells are destroyed by cytotoxic NK cells (ADCC) interferons - antiproliferative, cytotoxic effect on tumor cells - INF - DC maturation
Mechanisms of tumor resistance to the immune system high variability of tumor cells low expression of tumor antigens sialylation some anticancer substances have a stimulating effect production of factors inactivating T lymphocytes expression of Fas. L → T lymphocyte apoptosis inhibition of the function or durability dendritic cells (NO, IL-10, TGF- )

Transplantation
Transplantation = transfer of tissue or organ autologous - donor = recipient syngeneic - genetically identical donor and recipient (identical twins) allogeneic - genetically nonidentical donor of the same species xenogenic - the donor of another species implant - artificial tissue compensation
Allotransplantation differences in donor-recipient MHC gp and secondary histocompatibility Ag alloreactivity of T lymphocytes - the risk of rejection and graft-versus-host disease
Tests prior to transplantation ABO compatibility (matching blood group) -risk of hyperacute or accelerated rejection (= formation of Ab against A or B Ag on graft vascular endothelium) HLA typing (matching tissue type) - determining of HLA alelic forms by phenotyping or genotyping Cross-match - detection of preformed alloantibodies (after blood transfusions, transplantation, repeated childbirth) Mixed lymphocyte reaction - testing of T lymphocytes alloreactivity
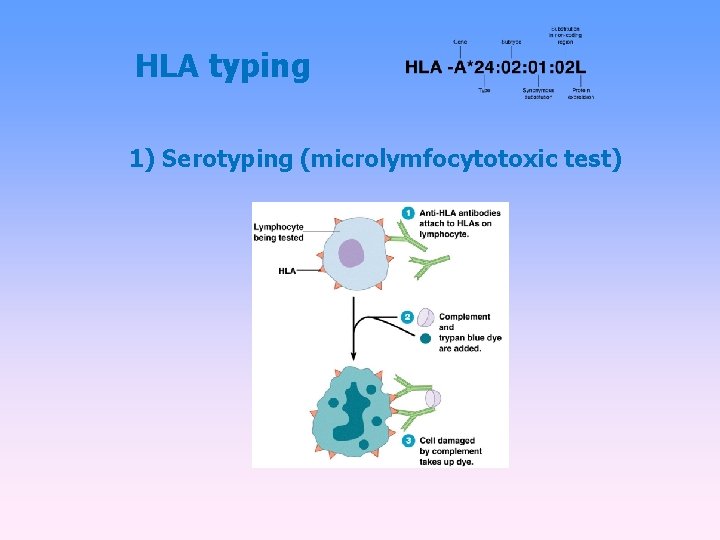
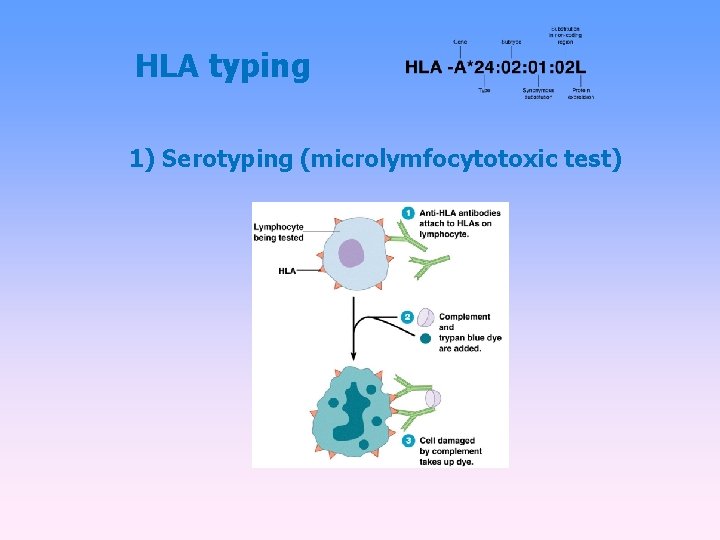
HLA typing 1) Serotyping (microlymfocytotoxic test)
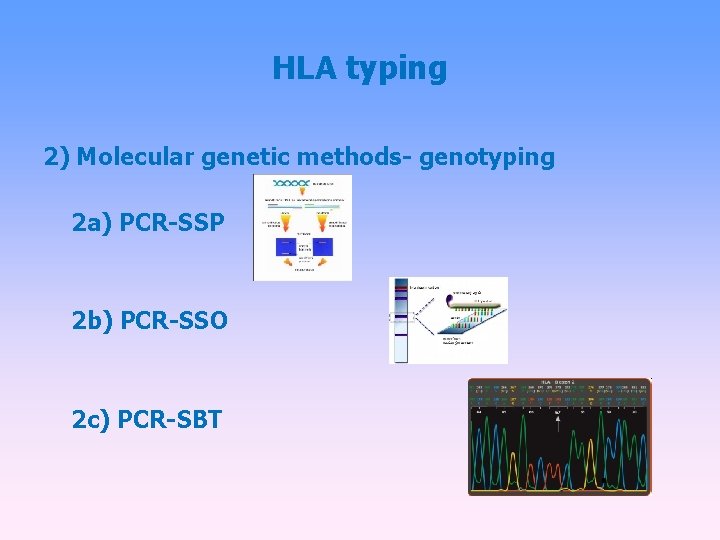
HLA typing 2) Molecular genetic methods- genotyping 2 a) PCR-SSP 2 b) PCR-SSO 2 c) PCR-SBT
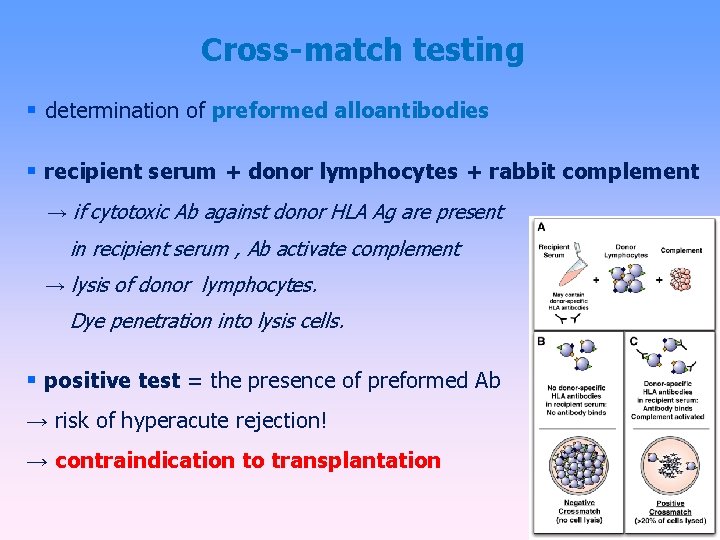
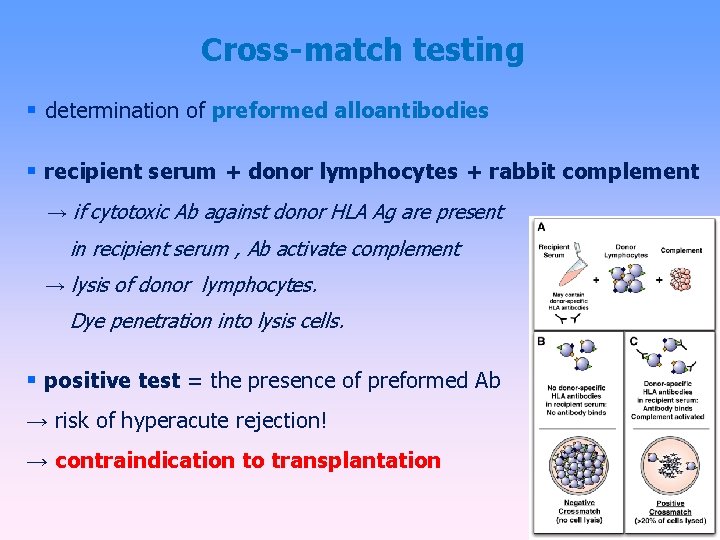
Cross-match testing determination of preformed alloantibodies recipient serum + donor lymphocytes + rabbit complement → if cytotoxic Ab against donor HLA Ag are present in recipient serum , Ab activate complement → lysis of donor lymphocytes. Dye penetration into lysis cells. positive test = the presence of preformed Ab → risk of hyperacute rejection! → contraindication to transplantation
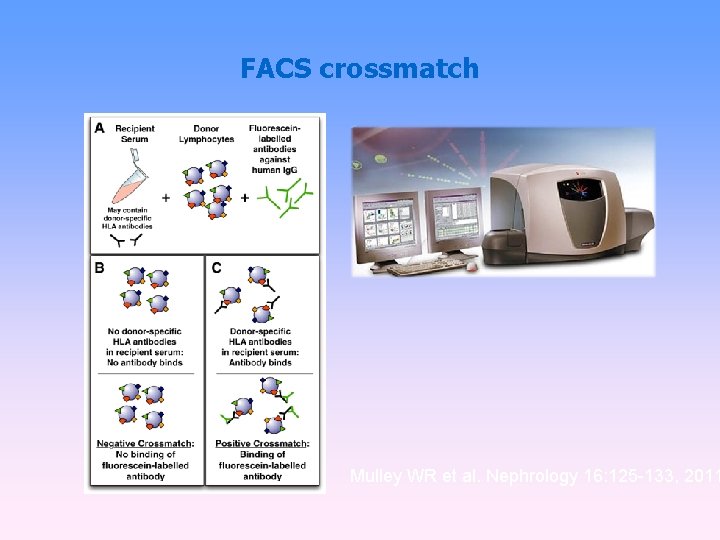
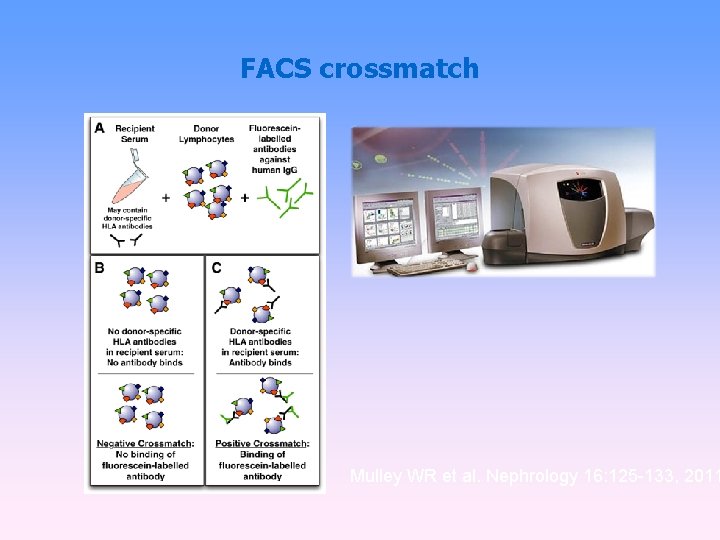
FACS crossmatch Mulley WR et al. Nephrology 16: 125 -133, 2011
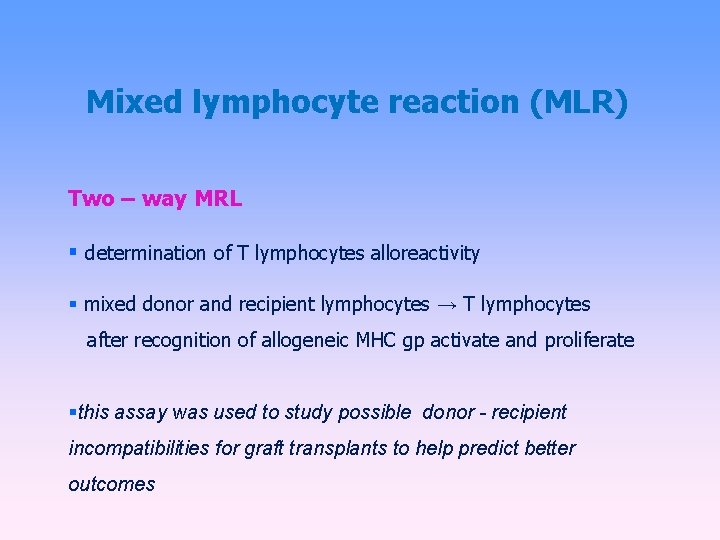
Mixed lymphocyte reaction (MLR) Two – way MRL determination of T lymphocytes alloreactivity mixed donor and recipient lymphocytes → T lymphocytes after recognition of allogeneic MHC gp activate and proliferate this assay was used to study possible donor - recipient incompatibilities for graft transplants to help predict better outcomes
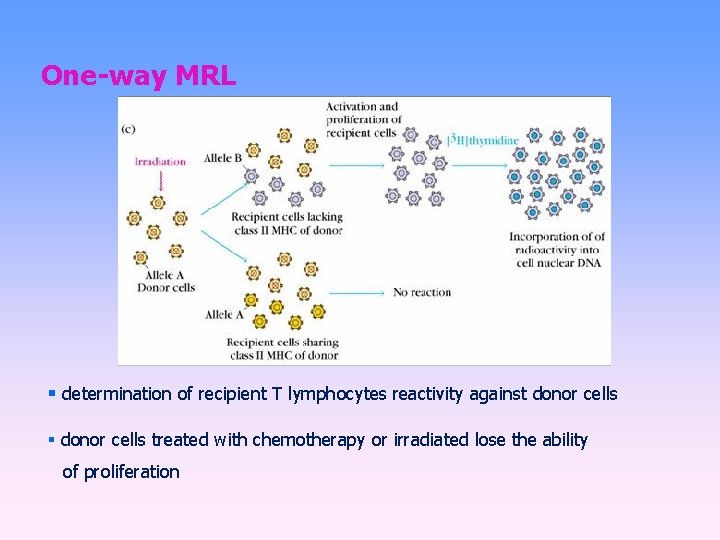
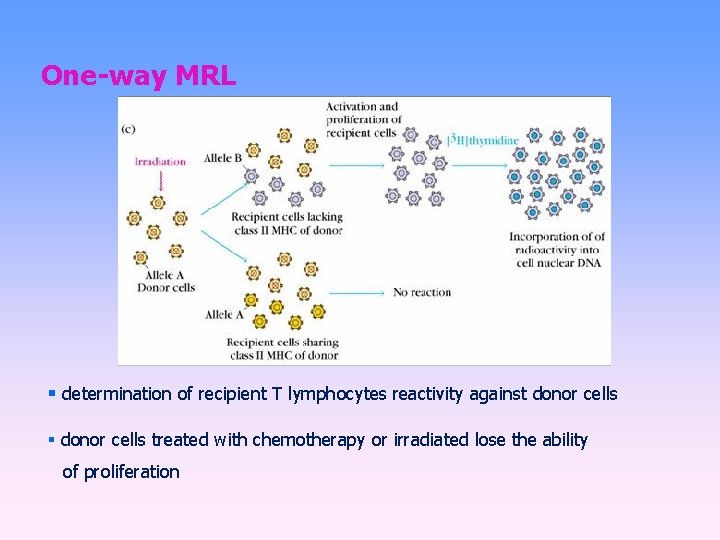
One-way MRL determination of recipient T lymphocytes reactivity against donor cells treated with chemotherapy or irradiated lose the ability of proliferation
Rejection hyperacute accelerated acute chronic
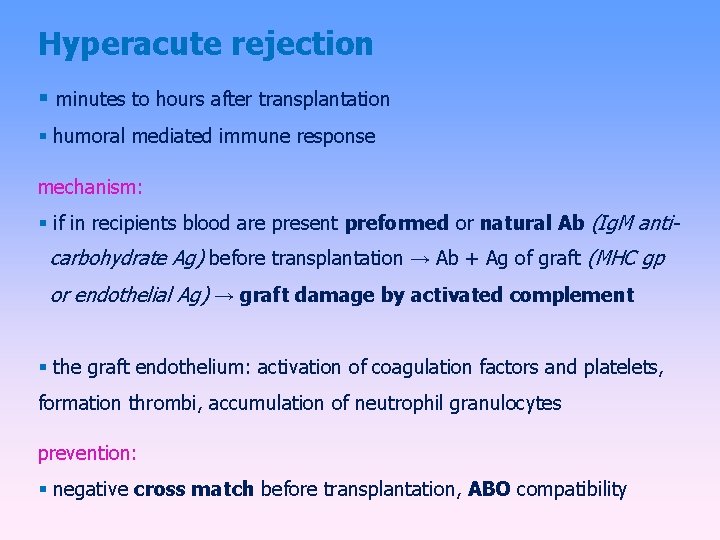
Hyperacute rejection minutes to hours after transplantation humoral mediated immune response mechanism: if in recipients blood are present preformed or natural Ab (Ig. M anti- carbohydrate Ag) before transplantation → Ab + Ag of graft (MHC gp or endothelial Ag) → graft damage by activated complement the graft endothelium: activation of coagulation factors and platelets, formation thrombi, accumulation of neutrophil granulocytes prevention: negative cross match before transplantation, ABO compatibility
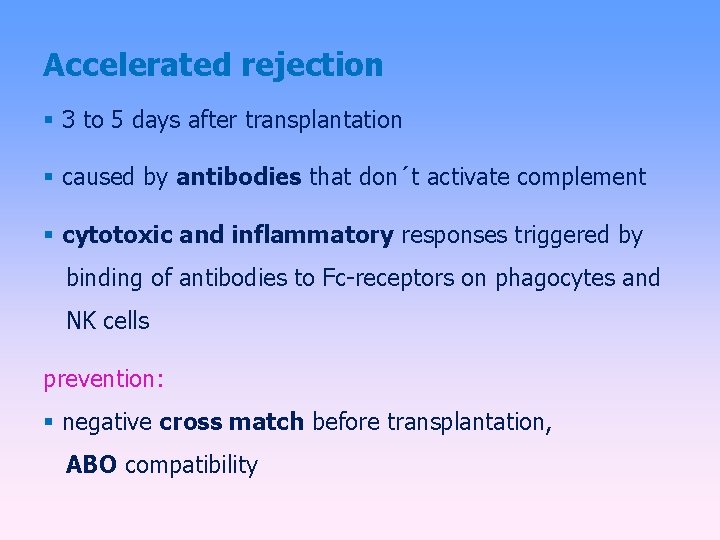
Accelerated rejection 3 to 5 days after transplantation caused by antibodies that don´t activate complement cytotoxic and inflammatory responses triggered by binding of antibodies to Fc-receptors on phagocytes and NK cells prevention: negative cross match before transplantation, ABO compatibility
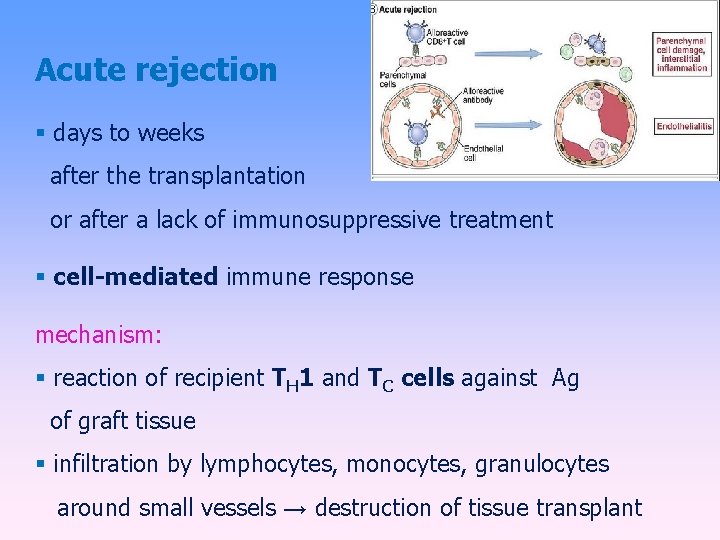
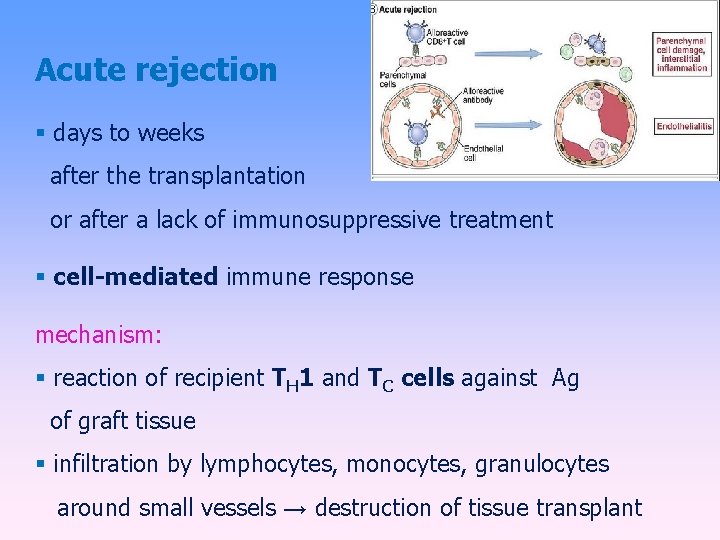
Acute rejection days to weeks after the transplantation or after a lack of immunosuppressive treatment cell-mediated immune response mechanism: reaction of recipient TH 1 and TC cells against Ag of graft tissue infiltration by lymphocytes, monocytes, granulocytes around small vessels → destruction of tissue transplant
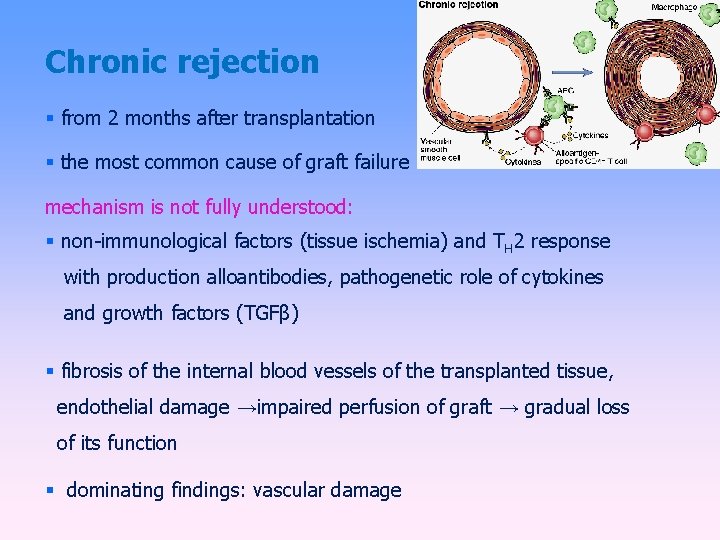
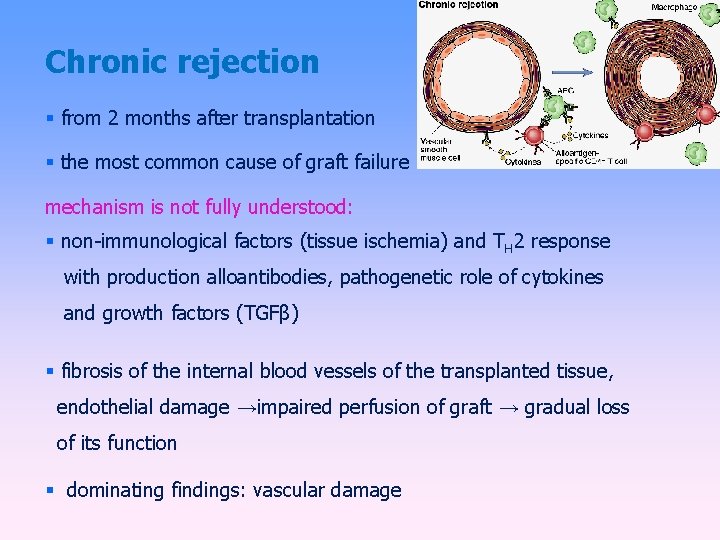
Chronic rejection from 2 months after transplantation the most common cause of graft failure mechanism is not fully understood: non-immunological factors (tissue ischemia) and TH 2 response with production alloantibodies, pathogenetic role of cytokines and growth factors (TGFβ) fibrosis of the internal blood vessels of the transplanted tissue, endothelial damage →impaired perfusion of graft → gradual loss of its function dominating findings: vascular damage
Rejection Factors: The genetic difference between donor and recipient, especially in the genes coding for MHC gp (HLA) Type of tissue / organ - the strongest reactions against vascularized tissues containing many APC (skin) The activity of the recipient immune system – the immunodeficiency recipient has a smaller rejection reaction; immunosuppressive therapy after transplantation – suppression of rejection Status of transplanted organ - the length of ischemia, the method of preservation, traumatization of organ at collection
Graft-versus-host (Gv. H) disease after bone marrow transplantation Gv. H also after blood transfusion to immunodeficiency recipients T-lymphocytes in the graft bone marrow recognize recipient tissue Ag as foreign (alloreactivity)
Acute Gv. H disease days to weeks after the transplantation of stem cells damage of liver, skin and intestinal mucosa prevention: appropriate donor selection, the removal of T lymphocytes from the graft and effective immunosuppression
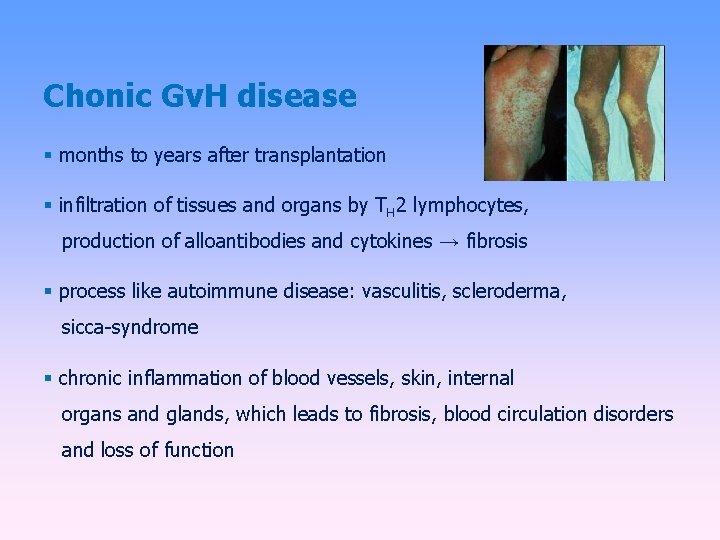
Chonic Gv. H disease months to years after transplantation infiltration of tissues and organs by TH 2 lymphocytes, production of alloantibodies and cytokines → fibrosis process like autoimmune disease: vasculitis, scleroderma, sicca-syndrome chronic inflammation of blood vessels, skin, internal organs and glands, which leads to fibrosis, blood circulation disorders and loss of function
Graft versus leukemia effect (Gv. L) donor T lymphocytes react against residual leukemick cells of recipient (setpoint response) mechanism is consistent with acute Gv. H associated with a certain degree of Gv. H (adverse reactions)
Immunopathological (hypersensitivity) reactions
Immunopathological reactions Immune response which caused damage to the body (Consequence of immune response against pathogens, inappropriate responses to harmless antigens; autoimmunity)
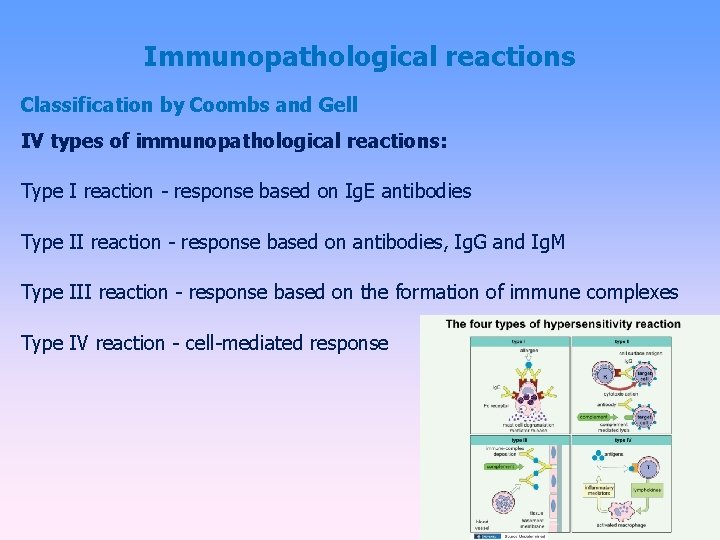
Immunopathological reactions Classification by Coombs and Gell IV types of immunopathological reactions: Type I reaction - response based on Ig. E antibodies Type II reaction - response based on antibodies, Ig. G and Ig. M Type III reaction - response based on the formation of immune complexes Type IV reaction - cell-mediated response
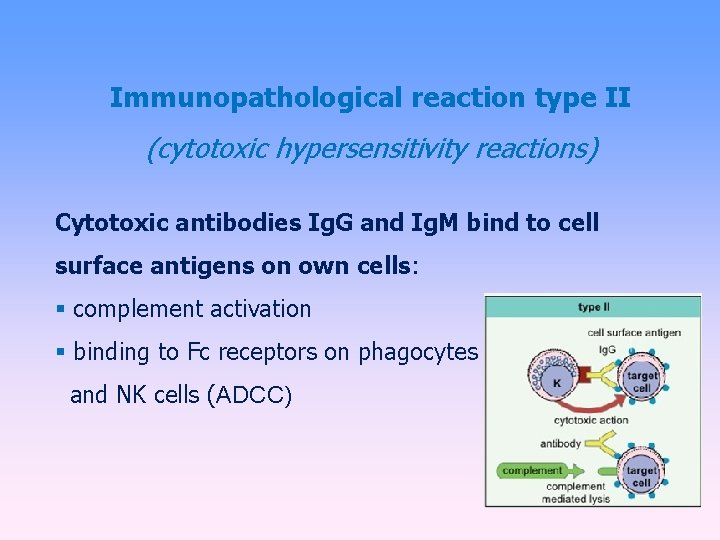
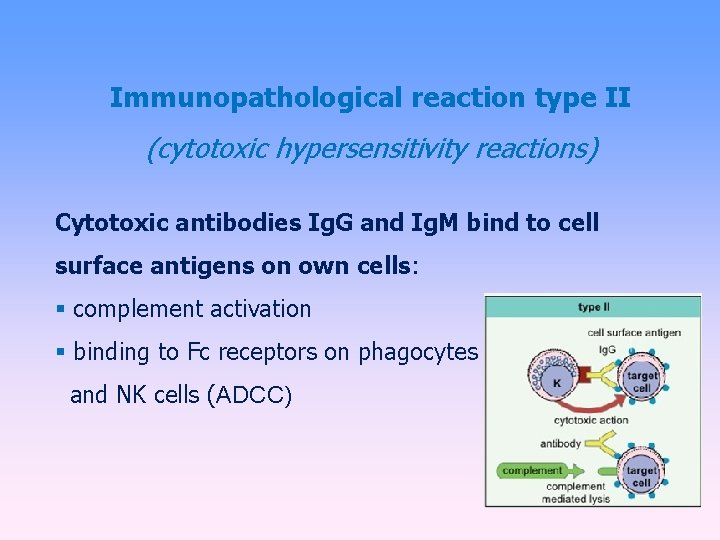
Immunopathological reaction type II (cytotoxic hypersensitivity reactions) Cytotoxic antibodies Ig. G and Ig. M bind to cell surface antigens on own cells: complement activation binding to Fc receptors on phagocytes and NK cells (ADCC)
Examples of immunopathological reaction type II Transfusion reactions after administration of incompatibile blood: binding of antibodies to antigens on erythrocytes → activation of the classical pathway of complement → cell lysis Hemolytic disease of newborns: caused by antibodies against Rh. D antigen
Examples of immunopathological reaction type II Autoimmune diseases: organ-specific cytotoxic antibodies (antibodies against erythrocytes, neutrophils, thrombocytes, glomerular basement membrane. . . ) blocking or stimulating antibodies Graves - Basedow's disease - stimulating antibodies against the receptor for TSH Myasthenia gravis - blocking of acetylcholin receptor→ blocking of neuromuscular transmission Pernicious anemia - blocking the absorption of vitamin B 12 Antiphospholipid syndrome - antibodies against fosfolipids Fertility disorder - antibodies against sperms or oocytes
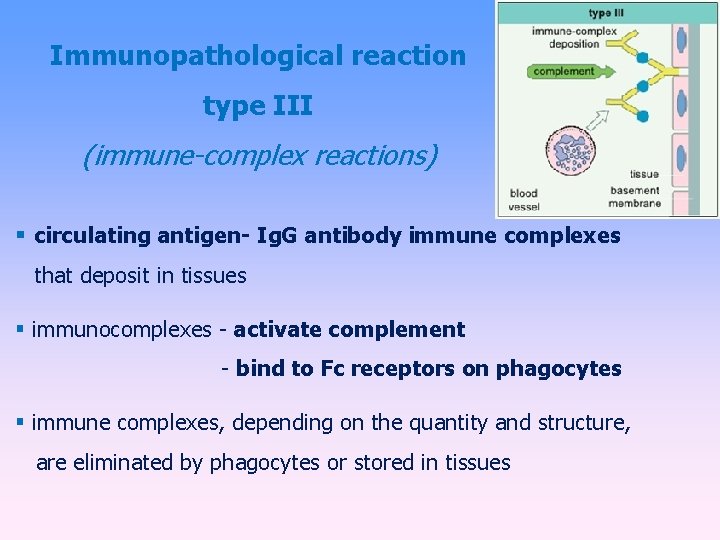
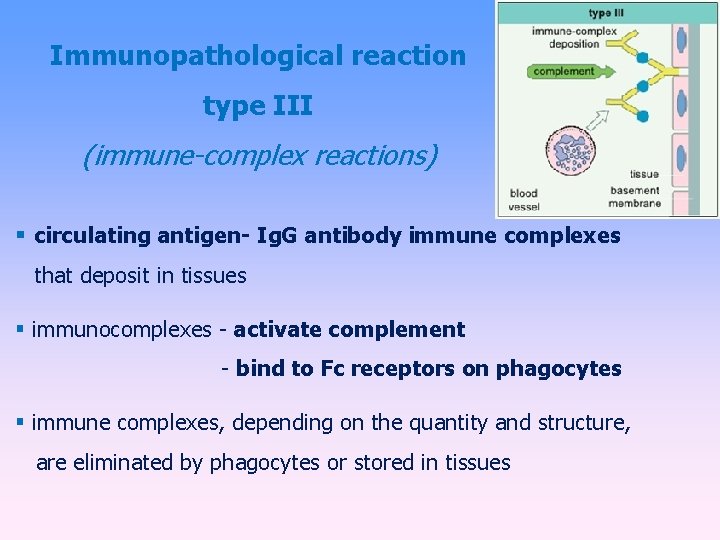
Immunopathological reaction type III (immune-complex reactions) circulating antigen- Ig. G antibody immune complexes that deposit in tissues immunocomplexes - activate complement - bind to Fc receptors on phagocytes immune complexes, depending on the quantity and structure, are eliminated by phagocytes or stored in tissues
Immunopathological reactions type III pathological immunocomplexes response arises when is a large dose of antigen, or antigen in the body remains; arise 10 -14 days after aplication of Ag and induced inflamation (can get to chronic state) immune complexes are deposited in the kidneys (glomerulonephritis), on the surface of endothelial cells (vasculitis) and in synovie joint (arthritis)
Serum sickness therapeutic application of xenogeneic serum (antiserum to snake venom) creation of immune complexes and their storage in the vessel walls of different organs clinical manifestations: urticaria, arthralgia, myalgia Systemic lupus erythematosus antibodies against nuclear antigens, ANA, anti-ds. DNA Farmer's lung Ig. G antibody against inhaled antigens (molds, hay) Post-streptococcal glomerulonephritis, cryoglobulinemia, revmatoid arthritis, post-infectious arthritis
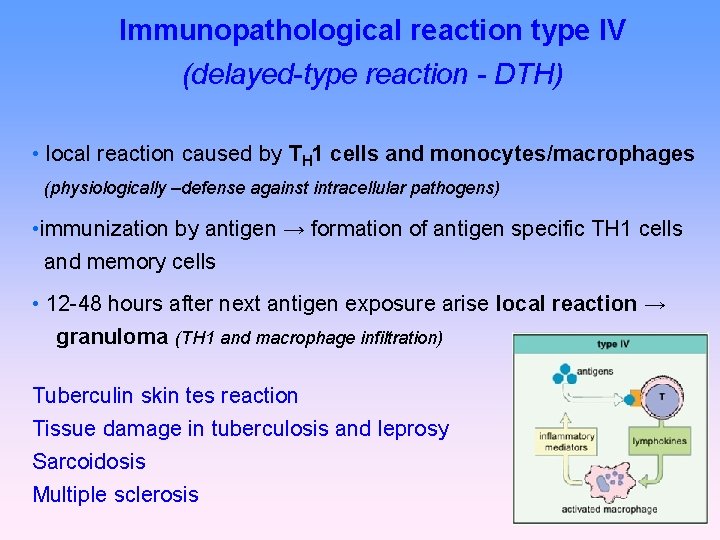
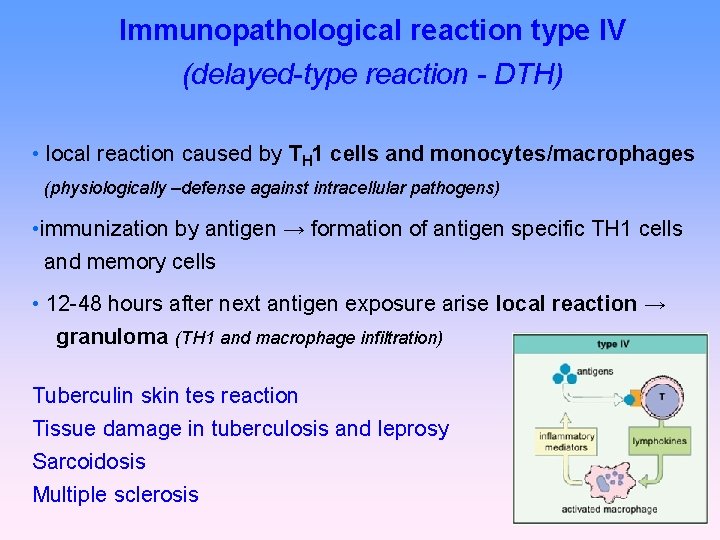
Immunopathological reaction type IV (delayed-type reaction - DTH) • local reaction caused by TH 1 cells and monocytes/macrophages (physiologically –defense against intracellular pathogens) • immunization by antigen → formation of antigen specific TH 1 cells and memory cells • 12 -48 hours after next antigen exposure arise local reaction → granuloma (TH 1 and macrophage infiltration) Tuberculin skin tes reaction Tissue damage in tuberculosis and leprosy Sarcoidosis Multiple sclerosis
Subtype IV - Cellular cytotoxic response (Tc activation) • similar to DTH reaction • TH 1 cells activate CD 8 + T lymphocytes • • • viral rashes viral hepatitis acute rejection of transplanted organ some autoimmune thyroiditis contact dermatitis
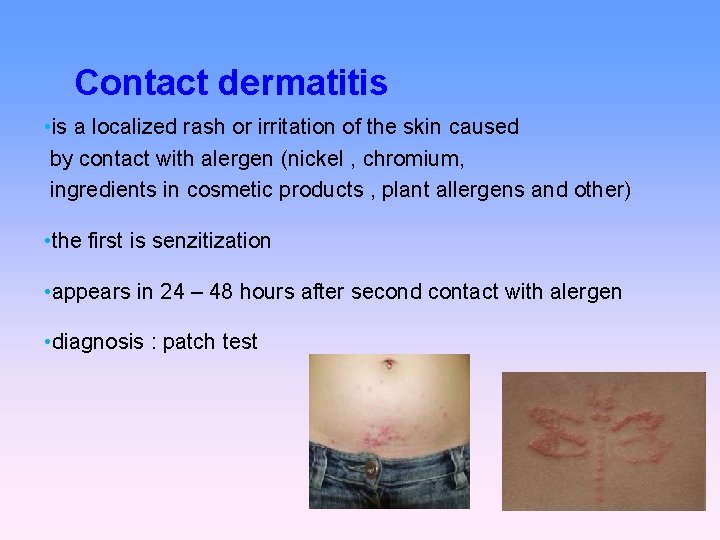
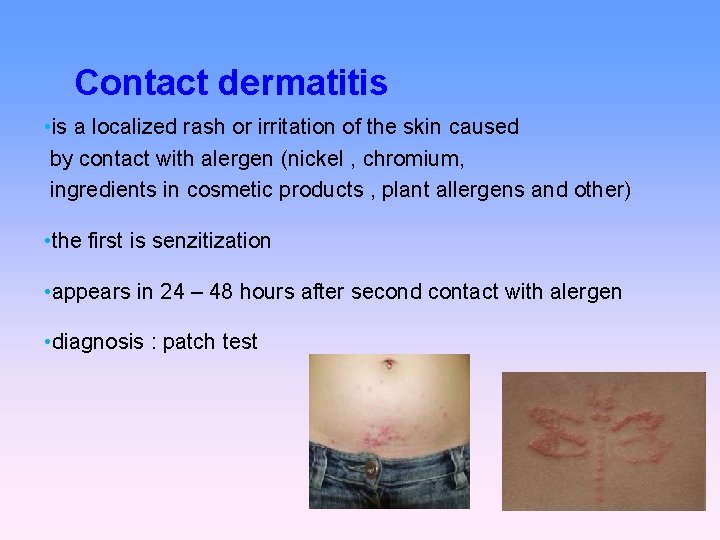
Contact dermatitis • is a localized rash or irritation of the skin caused by contact with alergen (nickel , chromium, ingredients in cosmetic products , plant allergens and other) • the first is senzitization • appears in 24 – 48 hours after second contact with alergen • diagnosis : patch test
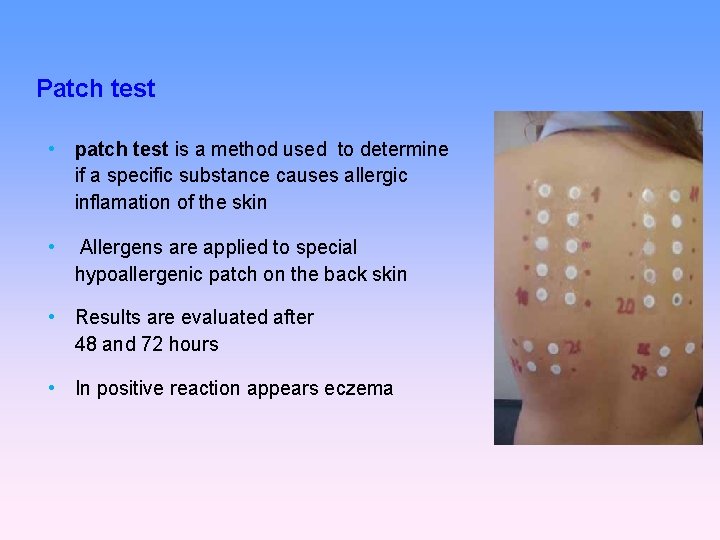
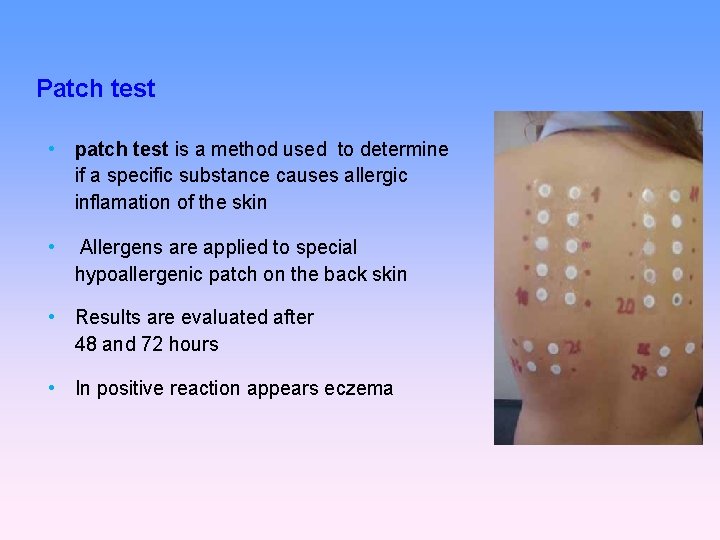
Patch test • patch test is a method used to determine if a specific substance causes allergic inflamation of the skin • Allergens are applied to special hypoallergenic patch on the back skin • Results are evaluated after 48 and 72 hours • In positive reaction appears eczema

Thank you for your attention
• Tumour immunology and immunotherapy • https: //www. youtube. com/watch? v=K 09 xz. I Q 8 zsg • This is how your immune system fights cancer • https: //www. youtube. com/watch? v=UM 2 fq. FZV 3 o
 Tumor immunology
Tumor immunology Blood type antigen antibody chart
Blood type antigen antibody chart Thymus independent antigens
Thymus independent antigens Complete antigens
Complete antigens Thymus independent antigens
Thymus independent antigens Antigen characteristics
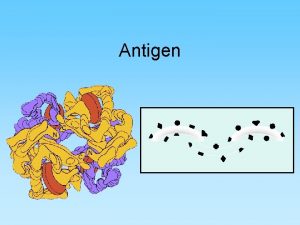
Antigen characteristics Lattice formation antigen antibody reaction
Lattice formation antigen antibody reaction Nature reviews immunology
Nature reviews immunology Janus kinase
Janus kinase Pcams immunology
Pcams immunology History of immunology
History of immunology Server medical art
Server medical art Fea course
Fea course Nature reviews immunology
Nature reviews immunology Abbas basic immunology
Abbas basic immunology Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology Neutrophil extracellular traps
Neutrophil extracellular traps Central tolerance and peripheral tolerance
Central tolerance and peripheral tolerance Bmc immunology
Bmc immunology Pals immunology
Pals immunology Abbas basic immunology
Abbas basic immunology Assisting in microbiology and immunology
Assisting in microbiology and immunology Avidity in immunology
Avidity in immunology Molecular immunology ppt
Molecular immunology ppt Sle clinical features
Sle clinical features Kuby immunology
Kuby immunology Baltimore classification
Baltimore classification Immunology diploma
Immunology diploma Nature reviews immunology
Nature reviews immunology American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Trends in immunology
Trends in immunology 17 tc
17 tc How to calculate specific gravity
How to calculate specific gravity Plummet method specific gravity
Plummet method specific gravity Tumor
Tumor Seroso
Seroso Dendritik hücre aşıları
Dendritik hücre aşıları Lengua geográfica
Lengua geográfica Pituitary gland tumor mri images
Pituitary gland tumor mri images Gist
Gist Trias tumor buli
Trias tumor buli Benign and malignant tumor
Benign and malignant tumor Kode icd 10 tumor supraclavicular
Kode icd 10 tumor supraclavicular How big is 1 cm tumor
How big is 1 cm tumor Campanacci classification gct
Campanacci classification gct Cest la vie význam
Cest la vie význam