Food Allergies What are they and can we

- Slides: 22
Food Allergies What are they and can we prevent them? Heather Mileski, RD Pediatric Gastroenterology and Nutrition, MCH
Outline n Define allergy n Differentiate between types of allergies n Discuss diagnostic tools available n Treatment n Consider preventative measures
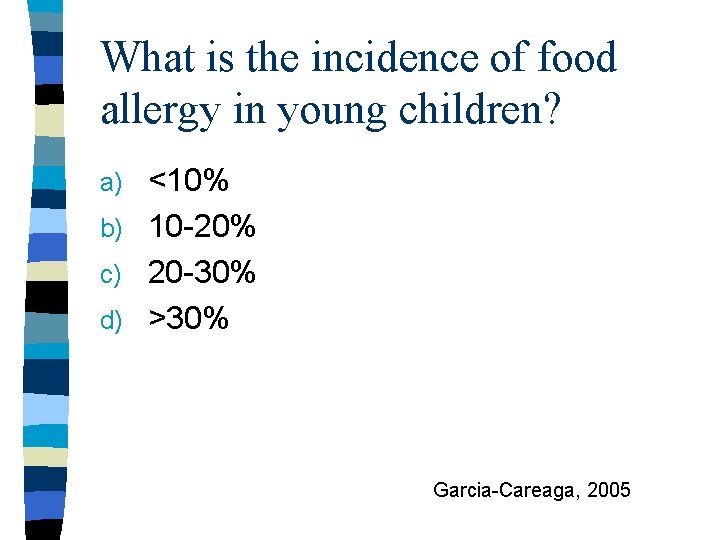
What is the incidence of food allergy in young children? <10% b) 10 -20% c) 20 -30% d) >30% a) Garcia-Careaga, 2005
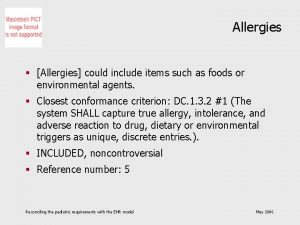
Definitions Allergy – “a pathological immune reaction to a food protein” Adverse food reaction – “an ill effect as a result of the intake of food” • Intolerances, sensitivities, enzyme deficiency (e. g. galactosemia, disaccharidase, etc), pharmacological effect (e. g. food dyes, preservatives, MSG, caffeine, etc)
Type 1: Ig. E-mediated (immune) n Immediate Hypersensitivity Disorder – Symptoms occur in minutes to hours – Can become anaphylactic – Common triggers are milk, soy, egg, peanut, shellfish, wheat – 80% resolve after several years with the exception of peanut and shellfish Garcia-Careaga et al, 2005

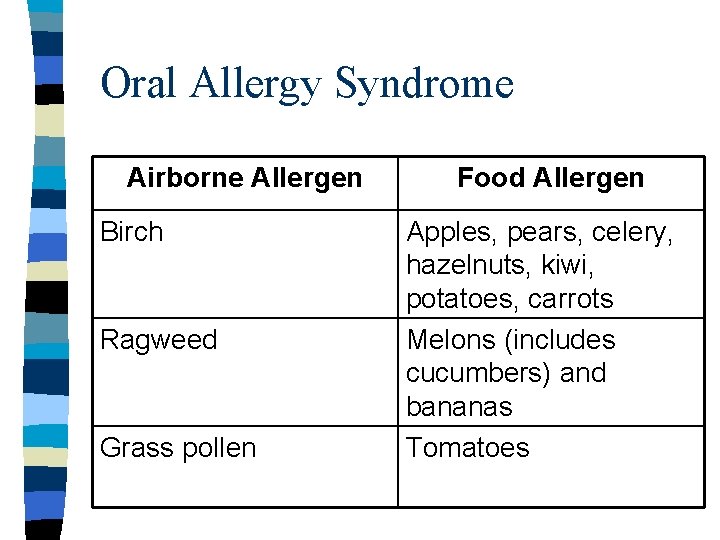
Type 1: Ig. E-mediated n Oral Allergy Syndrome/Pollen-Food Allergy Syndrome – Symptoms occur in minutes to hours – Reaction limited to oral cavity – Rarely systemic symptoms – Common triggers are RAW fruit and vegetables – Cross-reaction with airborne allergens
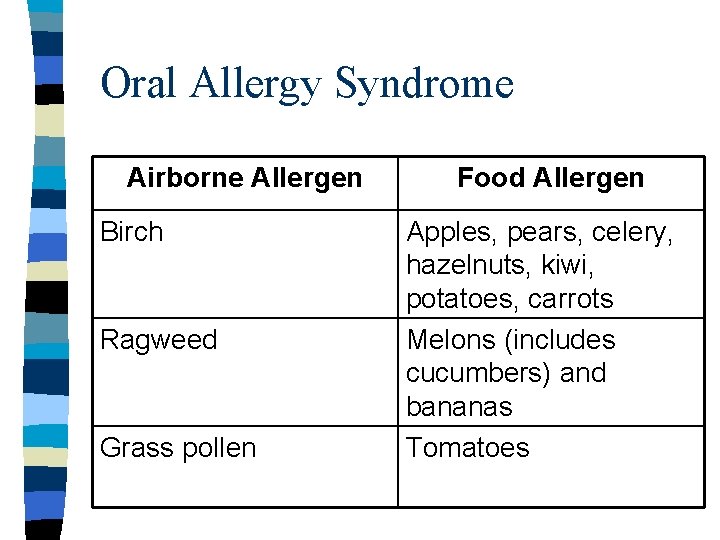
Oral Allergy Syndrome Airborne Allergen Birch Ragweed Grass pollen Food Allergen Apples, pears, celery, hazelnuts, kiwi, potatoes, carrots Melons (includes cucumbers) and bananas Tomatoes
Type III and IV: Non-Immune Mediated n Proctocolitis (Cow’s Milk Protein Colitis) – Occurs in infancy resolves between 6 months-2 years n Dietary Food Enteropathy – Occurs in infancy, usually resolves in first 2 years of life
Mixed Ig. E and Non-Ig. E n Eosinophilic Gastroenteritis – Eosinophilic infiltration of esophagus, stomach and small bowel mucosa n Eosinophilic Esophagitis n Both conditions diagnosed by biopsy
Other Adverse Food Reactions n Lactose Intolerance – Reaction to milk sugar NOT protein n Dietary Fructose Intolerance – Reaction to the sugar fructose n Food Sensitivities e. g. gluten
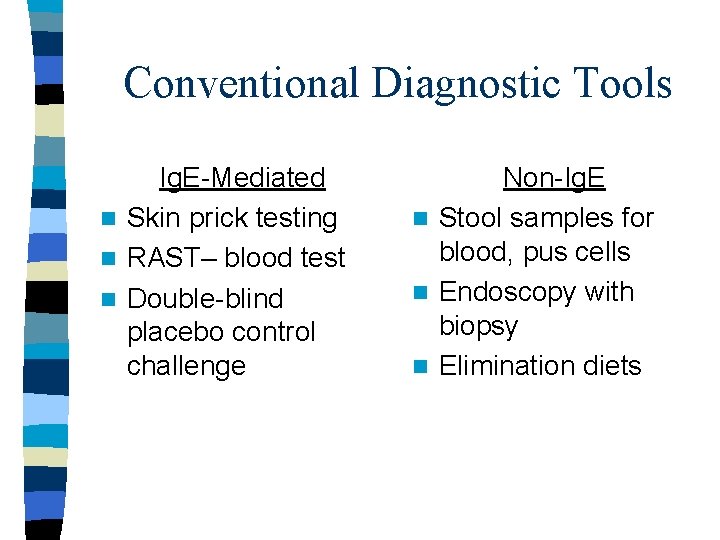
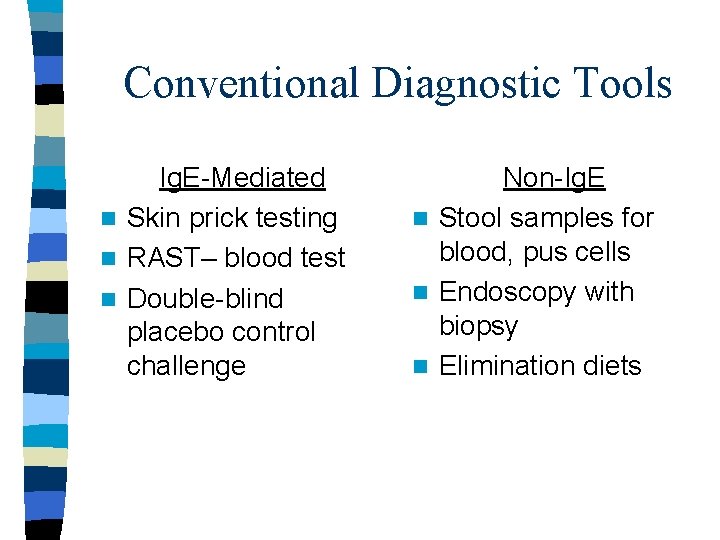
Conventional Diagnostic Tools Ig. E-Mediated n Skin prick testing n RAST– blood test n Double-blind placebo control challenge Non-Ig. E n Stool samples for blood, pus cells n Endoscopy with biopsy n Elimination diets
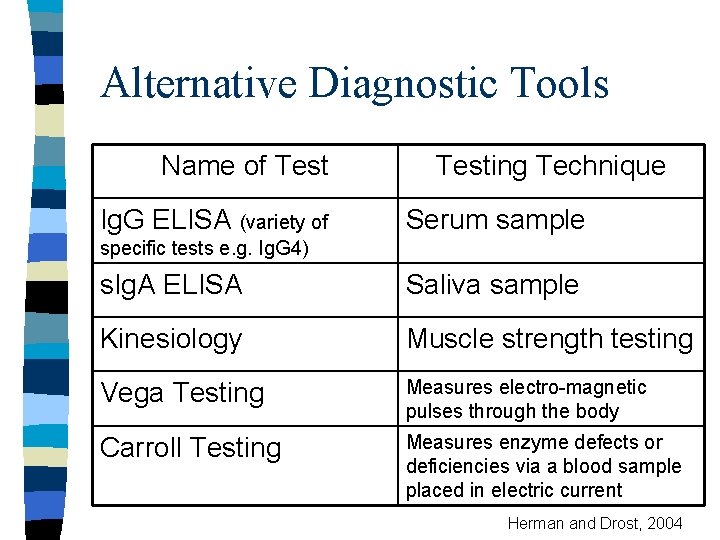
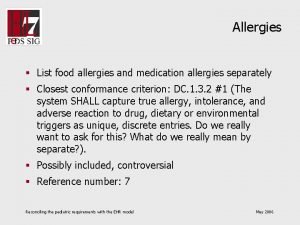
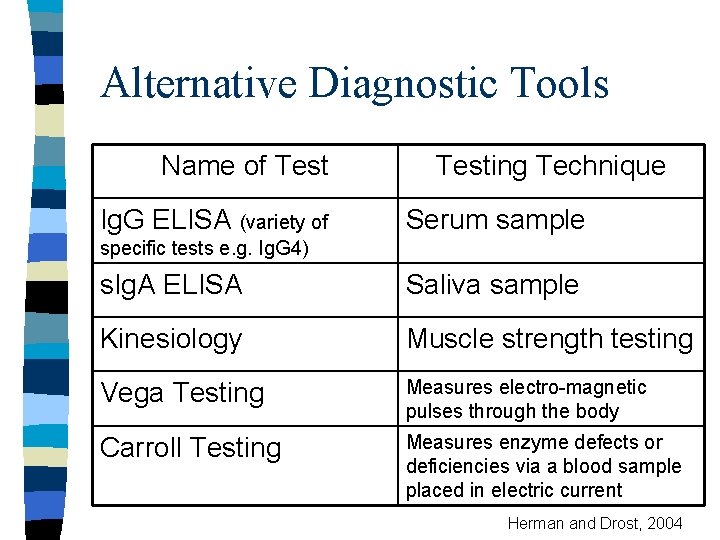
Alternative Diagnostic Tools Name of Test Ig. G ELISA (variety of Testing Technique Serum sample specific tests e. g. Ig. G 4) s. Ig. A ELISA Saliva sample Kinesiology Muscle strength testing Vega Testing Measures electro-magnetic pulses through the body Carroll Testing Measures enzyme defects or deficiencies via a blood sample placed in electric current Herman and Drost, 2004
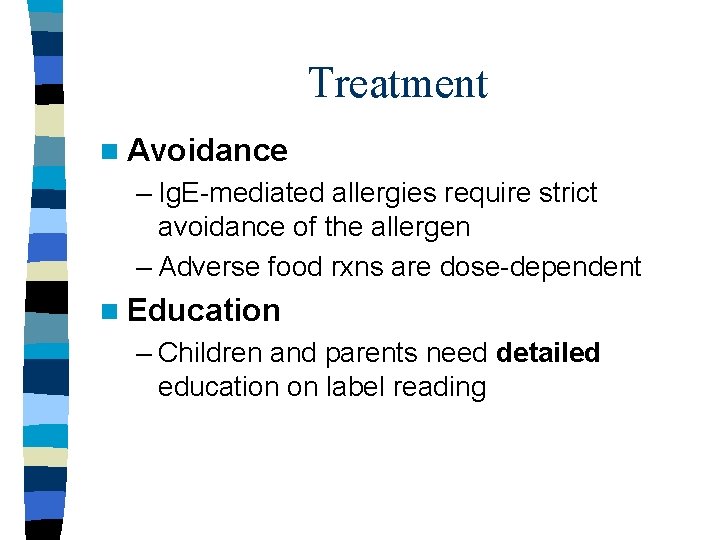
Treatment n Avoidance – Ig. E-mediated allergies require strict avoidance of the allergen – Adverse food rxns are dose-dependent n Education – Children and parents need detailed education on label reading
Which of the following is NOT a milk protein? Casein b) Lecithin c) Whey a)
Is Prevention Possible? n No evidence for prevention in general population n Some evidence in high risk infants – High risk = first degree relative with atopy (eczema, food allergy, asthma, allergic rhinitis)
Prevention Guidelines – AAP n n n Only for High Risk Infants 2000 Pregnancy possibly restrict peanut Exclusive breastfeeding for 6 months Eliminate peanuts & nuts from lactation diet (consider eggs, cow’s milk, fish) If bottle-fed use hypoallergenic formula (extensive of partial hydrolysate) Solids at 6 mo; cow’s milk at 12 mo; eggs at 24 mo; peanuts, nuts and fish at 36 mo
Prevention Guidelines 2004 Euro Academy of Allerg and Clin Immunol n Breastfeed exclusively for 4 months n If bottle-fed use extensively hydrolyzed formula n Solids at 4 to 6 months n Additional studies required to demonstrate any preventive effects of further dietary restriction
Prevention Guidelines – AAP Only for High Risk Infants n n 2008 No dietary restrictions during pregnancy or lactation Exclusive breastfeeding for 6 months If bottle-fed use extensively hydrolyzed formulas Solids at 4 to 6 months, no evidence to support delayed introduction of foods considered to be allergenic
Is Waiting Better? n Israeli population and peanuts n Swedish population and fish n German GINI study
Take Home Messages n Encourage exclusive breastfeeding for 6 months (WHO guidelines) n If bottle-feeding use extensively hydrolyzed formula if high risk infant n Avoid introduction of solid foods until 46 months of age n Stay tuned, this isn’t the end of the story!
References Garcia-Careaga et al. Gastrointestinal Manifestations of Food Allergies in Pediatric Patients. Nutr in Clin Prac 20: 526 -535, 2005. Herman, P & Drost, L. Evaluating the Clinical Relevance of Food Sensitivity Tests: A Single-Subject Experiment. Alt Med Review 9(2): 198 -207. Joneja, J. Food Allergy in Adults. Dietitians of Canada Current Issues, 2007. Joshi et al. Interpretation of Commercial Food Ingredient Labels by Parents of Food-Allergic Children. Ann Allergy Asthma Immunol 90: 84 -89, 2003. Muraro et al. Dietary Prevention of Allergic Diseases in Infants and Small Children. Pediatr Allergy Immunol 15: 291 -307, 2004. Pyrhonen et al. Occurrence of parent-reported food hypersensitivities and food allergies among children aged 1 -4 yr. Pediatr Allergy Immunol 20: 328 -338, 2009. Wennergren, G. What if it is the other way around? Early introduction of peanut and fish seems to be better than avoidance. Acta Paediatrica 98: 1085 -1087, 2009.
 Antigentest åre
Antigentest åre Diabetes and allergies
Diabetes and allergies Arthritis and food allergies
Arthritis and food allergies Food handlers can contaminate food when they answer
Food handlers can contaminate food when they answer Hand antiseptics may only be used if they are
Hand antiseptics may only be used if they are Seasonal allergies icd 9
Seasonal allergies icd 9 Beta glucan allergies
Beta glucan allergies Docteur simonis citadelle
Docteur simonis citadelle Fast food can be defined as any food that contributes
Fast food can be defined as any food that contributes Unit 2 food food food
Unit 2 food food food Food chain sequence
Food chain sequence Rankings: what are they and do they matter?
Rankings: what are they and do they matter? Blood types and who they can donate to
Blood types and who they can donate to Complete the sentences with if or when
Complete the sentences with if or when They seek him here they seek him there
They seek him here they seek him there I have not rejected you
I have not rejected you Jordan 14
Jordan 14 Grammar rules frustrate me they're not logical they are so
Grammar rules frustrate me they're not logical they are so For they not know what they do
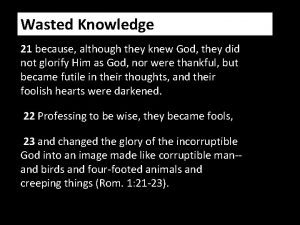
For they not know what they do Although they knew god they did not glorify him
Although they knew god they did not glorify him Look at the pictures and complete with can or can't
Look at the pictures and complete with can or can't Pictogram for skin burns
Pictogram for skin burns How much can they safely carry answer key
How much can they safely carry answer key