FONTAN OPERATION HOW I DO IT Piya Samankatiwat







- Slides: 59
FONTAN OPERATION: HOW I DO IT? Piya Samankatiwat Cardiothoracic Unit Ramathibodi hospital
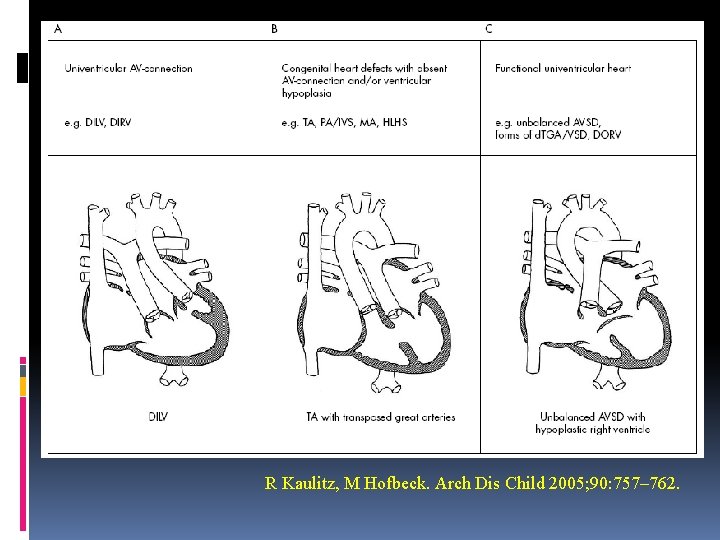
What is the ‘single ventricle’? Prof. Richard van Praagh ‘One ventricular chamber receives blood from both tricuspid and mitral valve or a common atrioventricular valve’ Therefore, this excludes tricuspid atresia and mitral atresia.
So !!! you are in doubt what the univentricular physiology is. Prof. Robert H Anderson emphasised that ‘the entire atrioventricular junction is connected to only one chamber in the ventricular mass’ DILV Absent of one atrioventricular connection Common AV valve with one completely well-developed ventricule Only one fully developed ventricle Heterotaxy syndrome Rare miscellaneous forms
Univentricular heart Congenital heart surgery nomenclature and database Common inlet atrioventricular connection Absence of one atrioventricular connection DILV DIRV Tricuspid atresia Mitral atresia Common atrioventricular valve with one welldeveloped ventricle (unbalanced AVSD) Heterotaxia syndrome with only one fully developed ventricle Other rare forms of univentricular heart
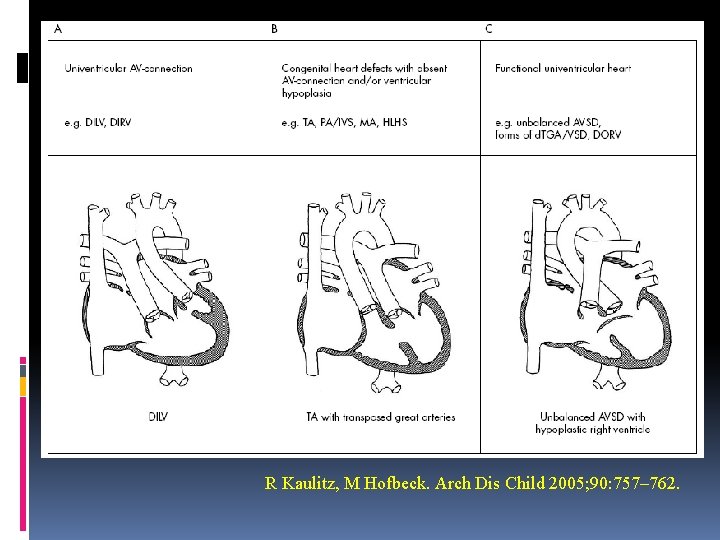
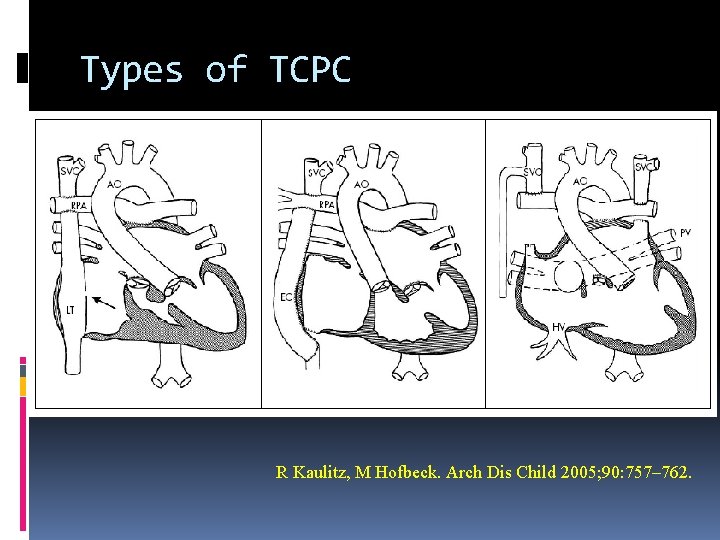
R Kaulitz, M Hofbeck. Arch Dis Child 2005; 90: 757– 762.
Evolution of surgery for single functioning ventricle 1940 s Blalock-Taussig shunt 1952 PA banding by Muller WH and Dammann JF 1954 Shumacker and 1 st cavopulmonary connection 1956 separation of single ventricle at Mayo Clinics 1971 Fontan’s and Kreutzer’s
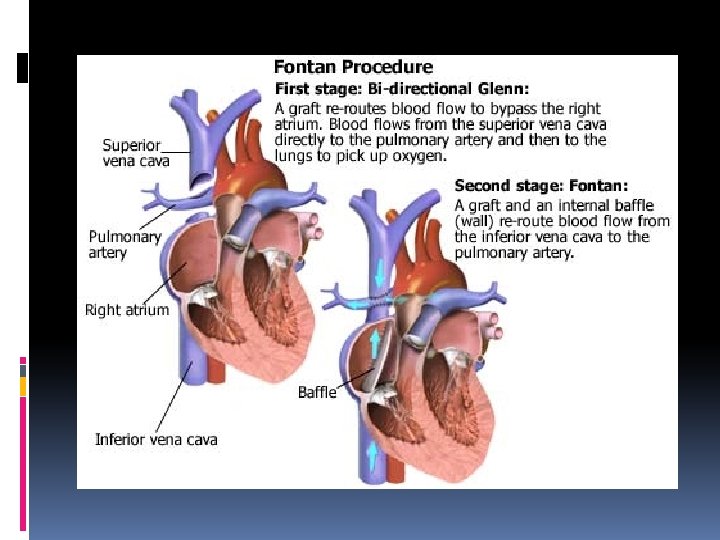
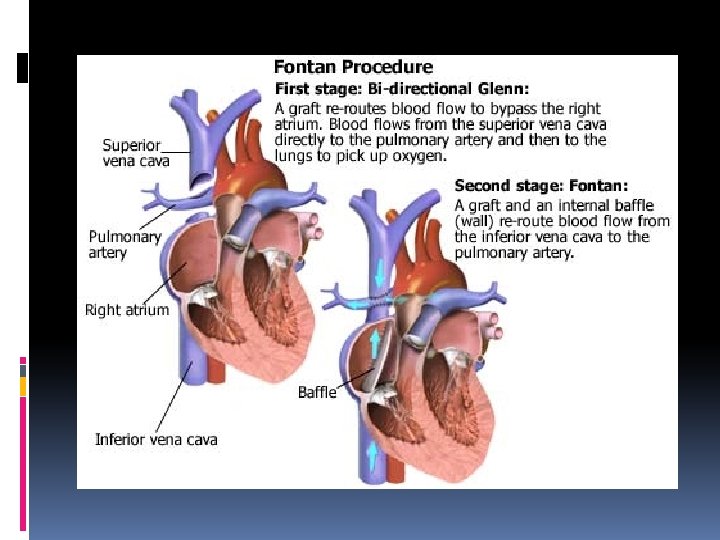
Fontan procedure Background 1971 Fontan and Baudet first introduced a new procedure for repair of tricuspid atresia in clinical practice 1970 s to 1980 s became widely accepted as the palliative procedure of choice in univentricular heart physiology Physiological, not anatomical correction
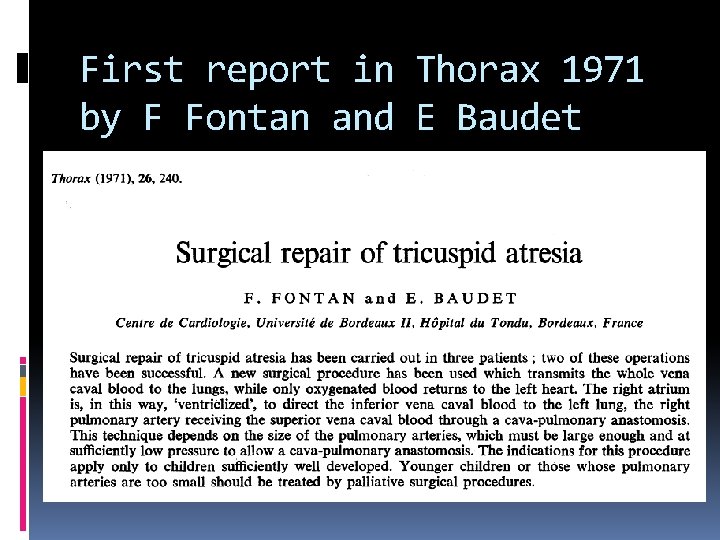
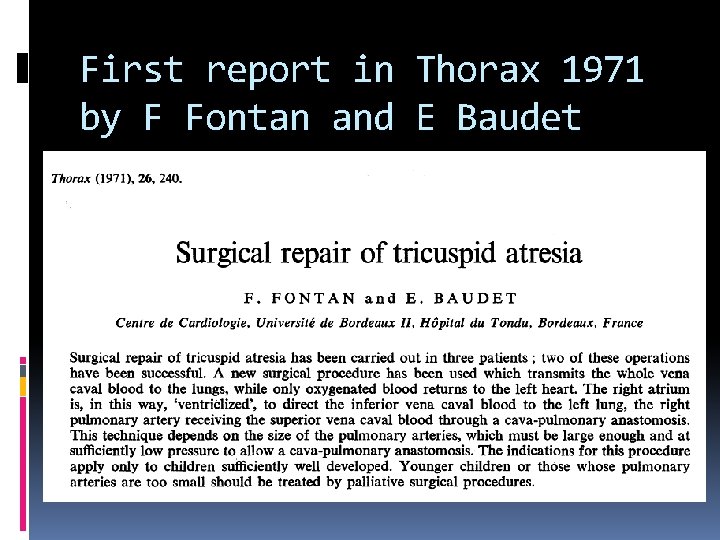
First report in Thorax 1971 by F Fontan and E Baudet
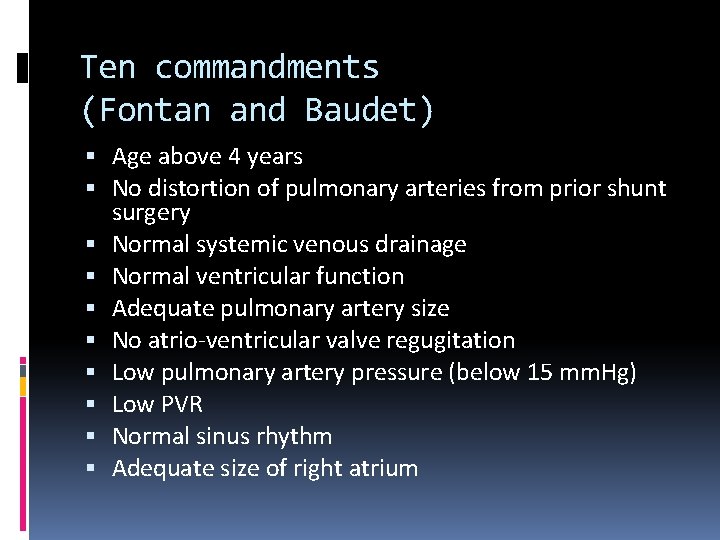
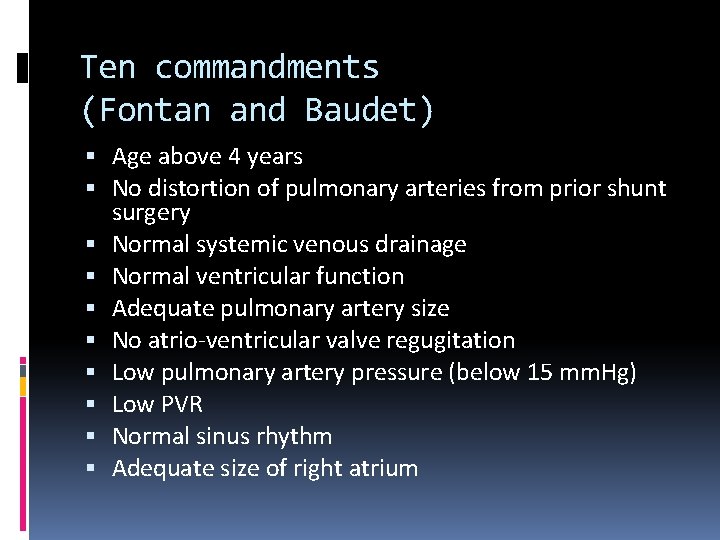
Ten commandments (Fontan and Baudet) Age above 4 years No distortion of pulmonary arteries from prior shunt surgery Normal systemic venous drainage Normal ventricular function Adequate pulmonary artery size No atrio-ventricular valve regugitation Low pulmonary artery pressure (below 15 mm. Hg) Low PVR Normal sinus rhythm Adequate size of right atrium
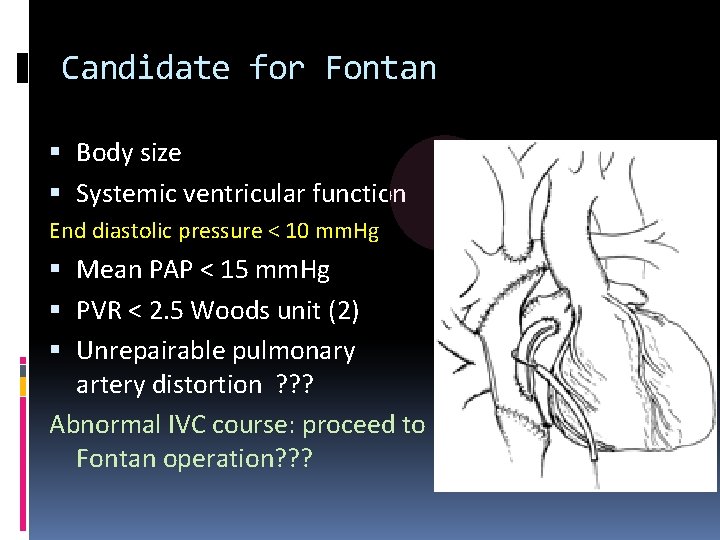
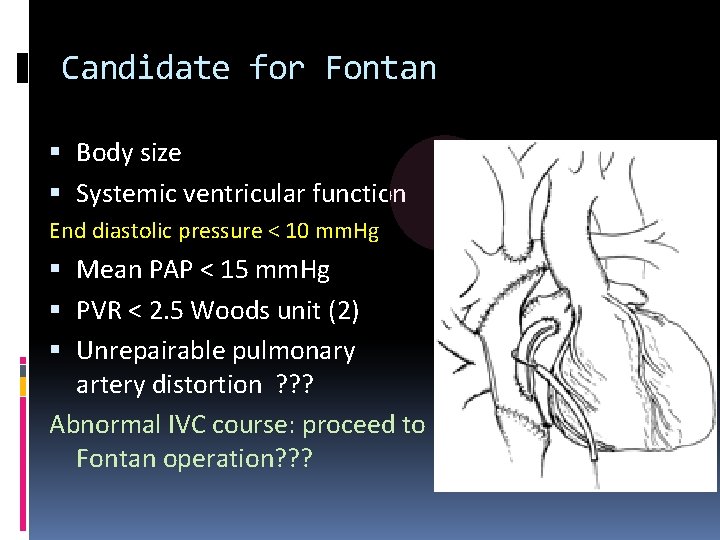
Candidate for Fontan Body size Systemic ventricular function End diastolic pressure < 10 mm. Hg Mean PAP < 15 mm. Hg PVR < 2. 5 Woods unit (2) Unrepairable pulmonary artery distortion ? ? ? Abnormal IVC course: proceed to Fontan operation? ? ?
Principle of surgery for UVH Protect the lung: prevent pulmonary HT with PA banding Correct cyanosis: BT shunt Atrial septostomy/septectomy Relieve ventricular outflow tract obstruction Correct obstruction of pulmonary venous connection Correct valvular regurgitation
Operations: pre-Fontan palliation Pulmoanry artery banding Modified BT shunt Atrioventricular valve repair Correction of TAPVC (if present) DKS or Norwood principle Glenn’s shunt: superior cavopulmonary connection
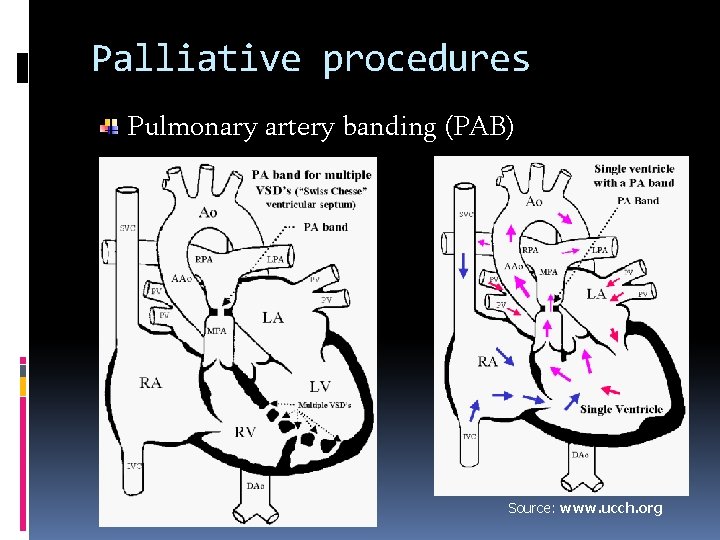
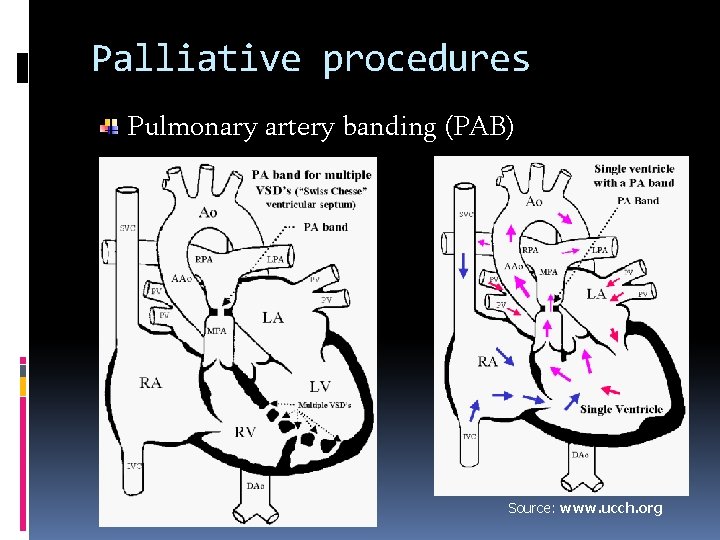
Palliative procedures Pulmonary artery banding (PAB) Source: www. ucch. org
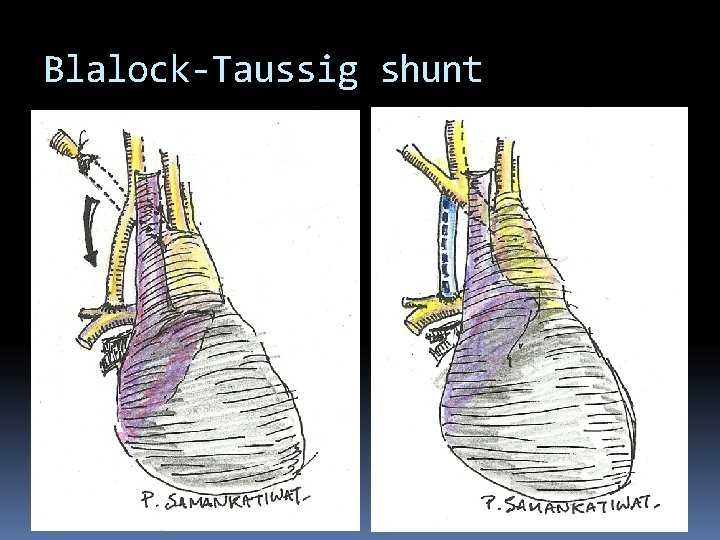
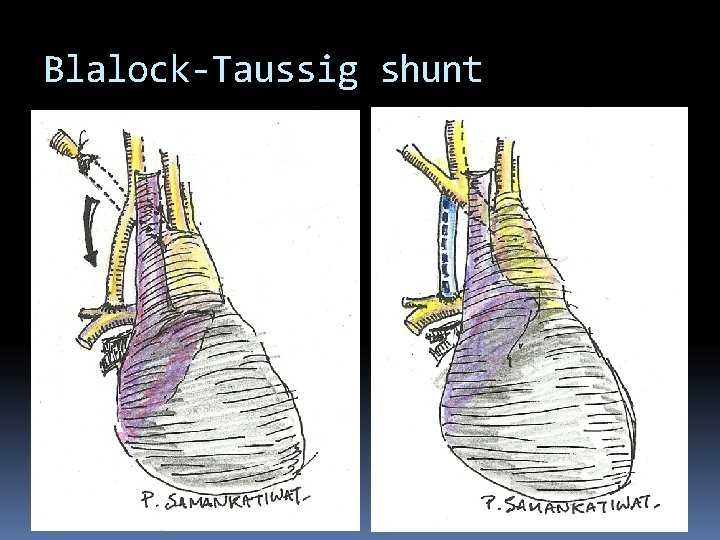
Blalock-Taussig shunt
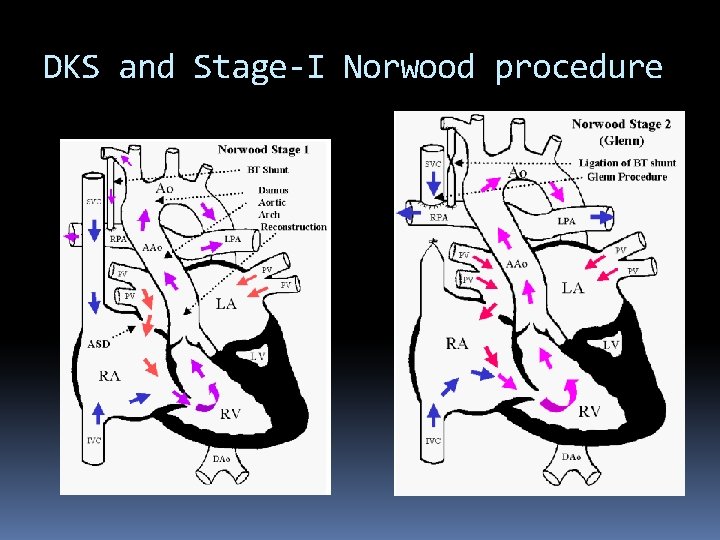
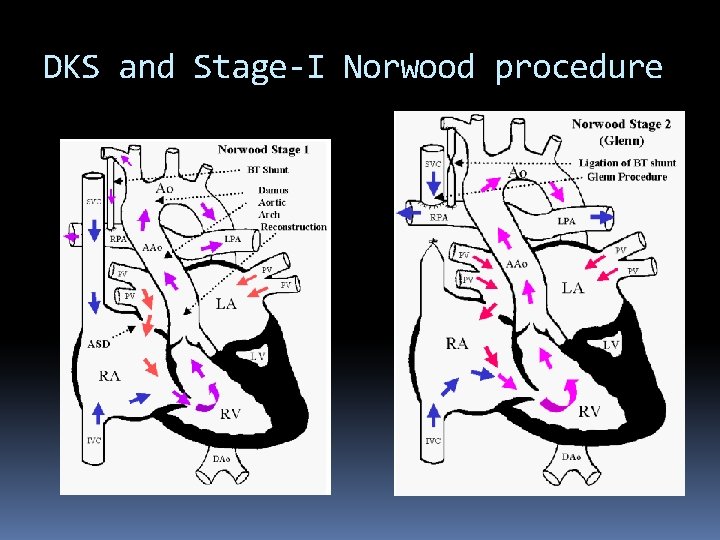
DKS and Stage-I Norwood procedure
Glenn procedure SVC to pulmonary artery Patient selection: good candidate Pulmonary arterial pressure (PAP) mean < 20 mm. Hg Size of branch pulmonary arteries Preparation Bypass circuit: aortic/ SVC –RA venous cannulation
Special considerations for Glenn Additional sources of pulmonary blood flow Bilateral BDG Kawashima operation Hemi-Fontan procedure
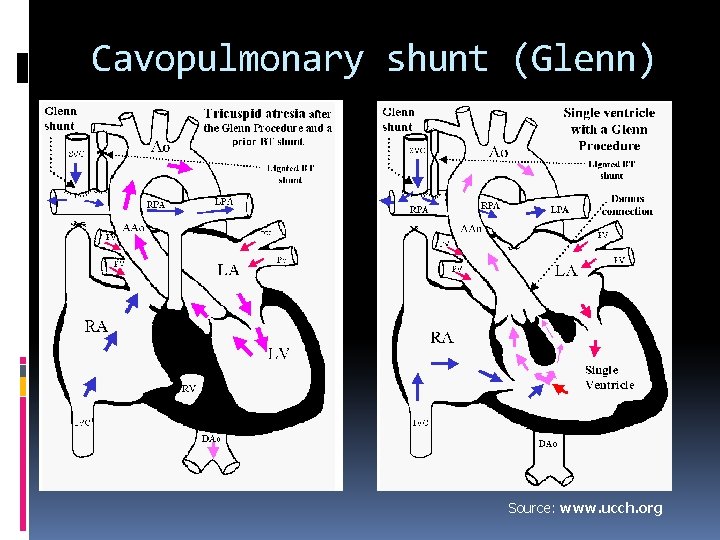
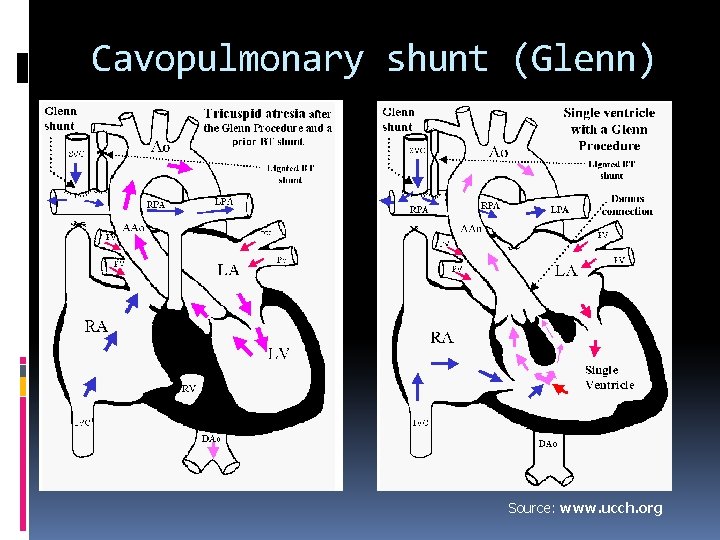
Cavopulmonary shunt (Glenn) Source: www. ucch. org
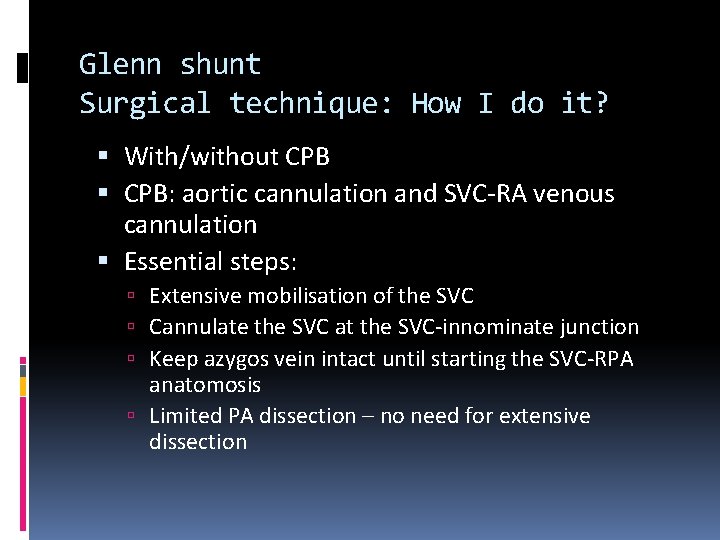
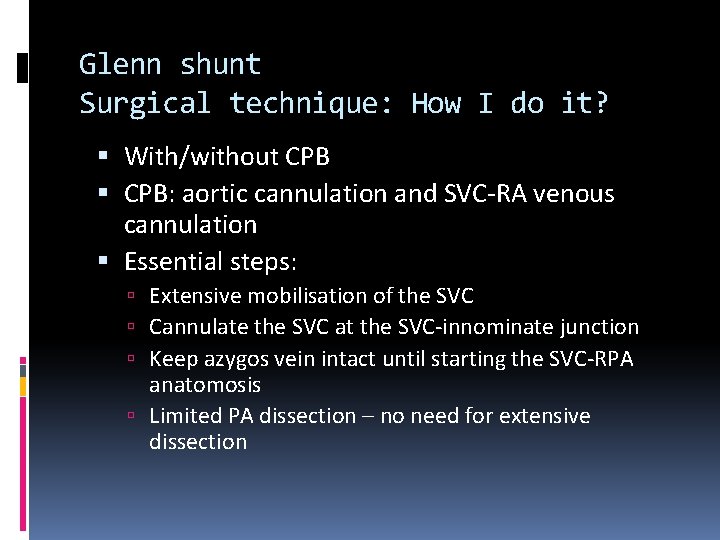
Glenn shunt Surgical technique: How I do it? With/without CPB: aortic cannulation and SVC-RA venous cannulation Essential steps: Extensive mobilisation of the SVC Cannulate the SVC at the SVC-innominate junction Keep azygos vein intact until starting the SVC-RPA anatomosis Limited PA dissection – no need for extensive dissection
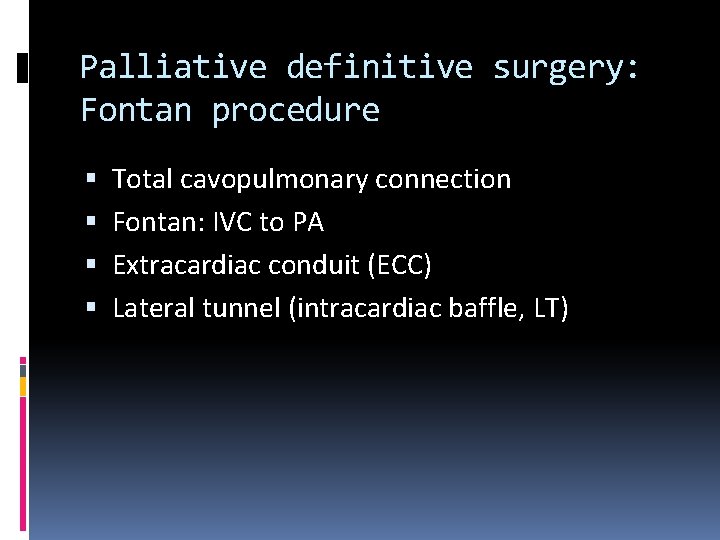
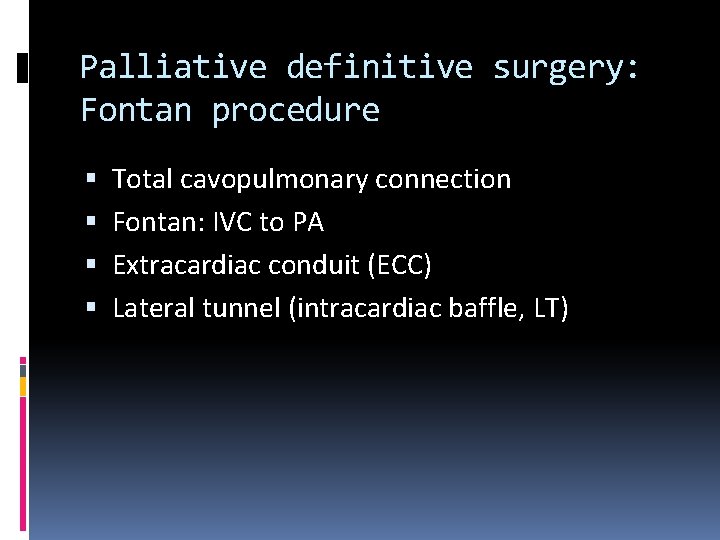
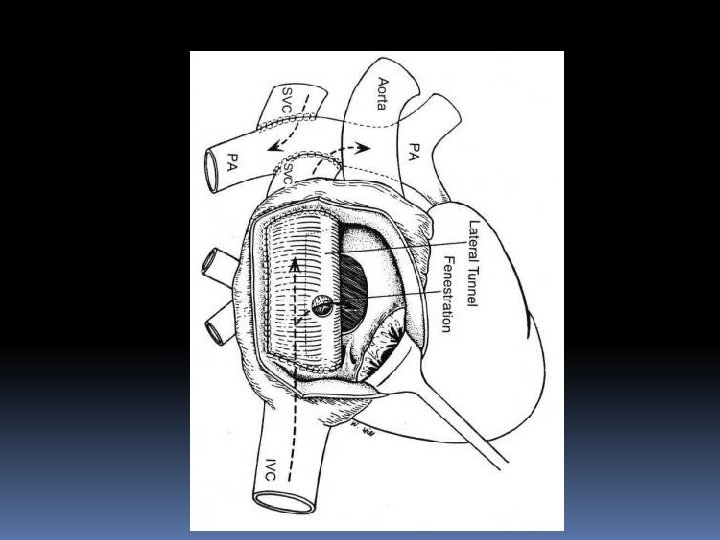
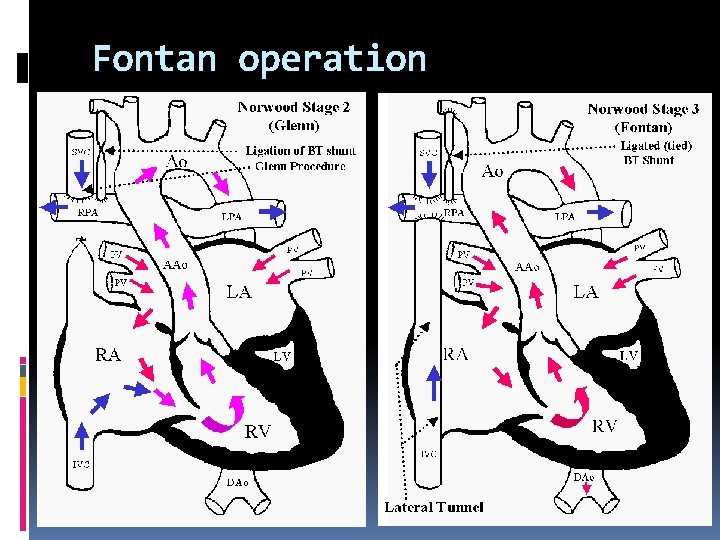
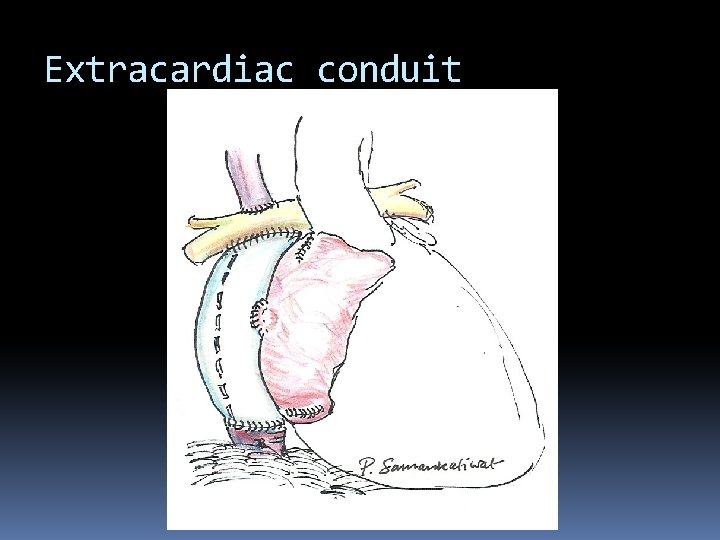
Palliative definitive surgery: Fontan procedure Total cavopulmonary connection Fontan: IVC to PA Extracardiac conduit (ECC) Lateral tunnel (intracardiac baffle, LT)
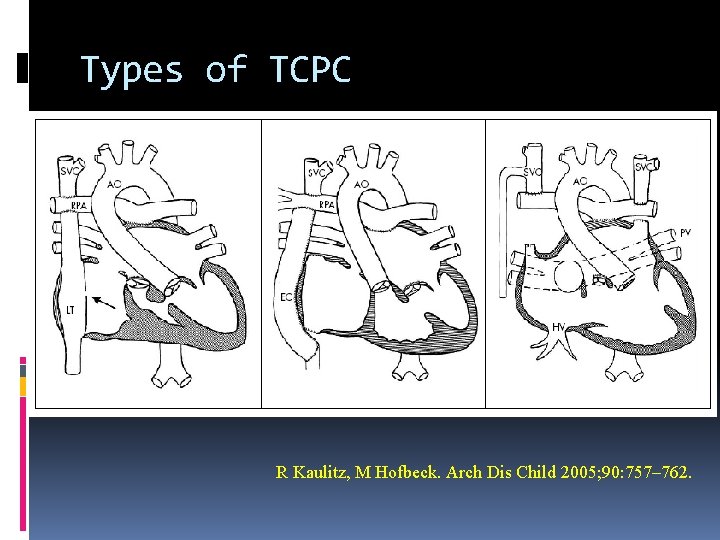
Types of TCPC R Kaulitz, M Hofbeck. Arch Dis Child 2005; 90: 757– 762.
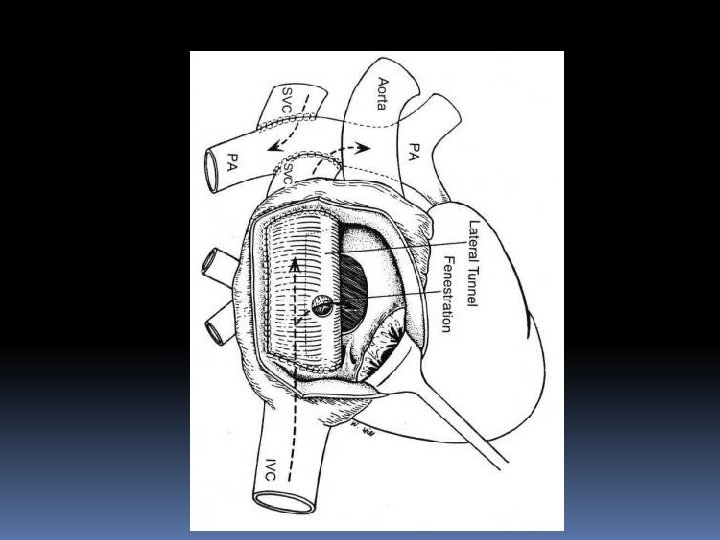
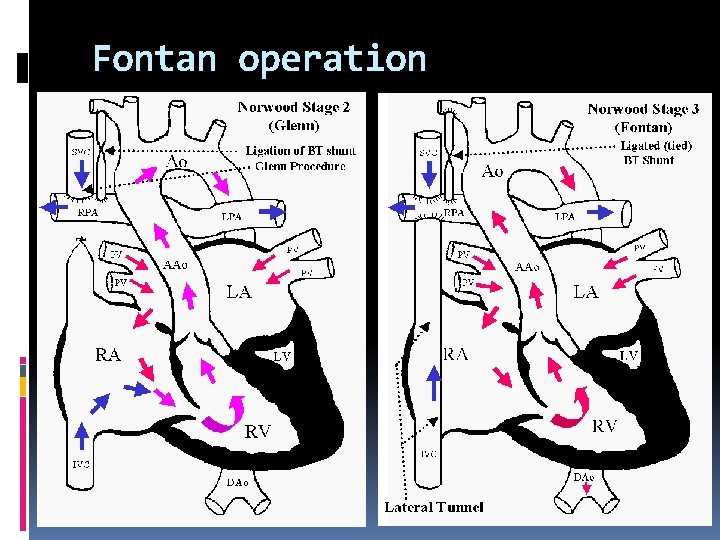
Fontan operation
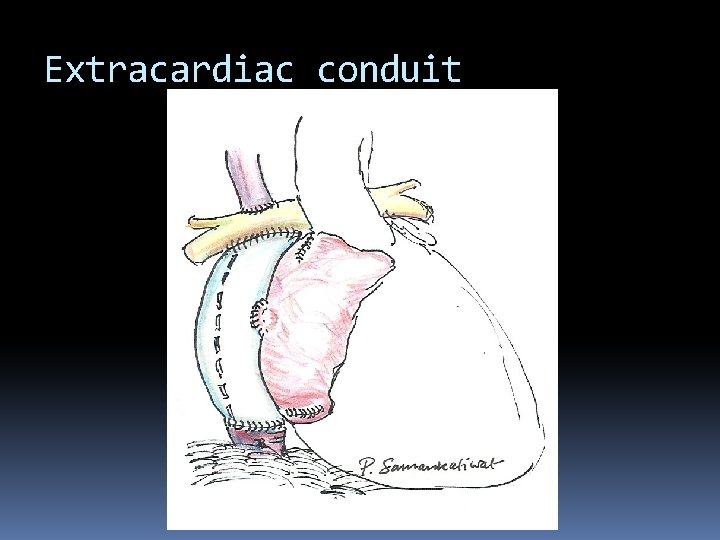
Extracardiac conduit
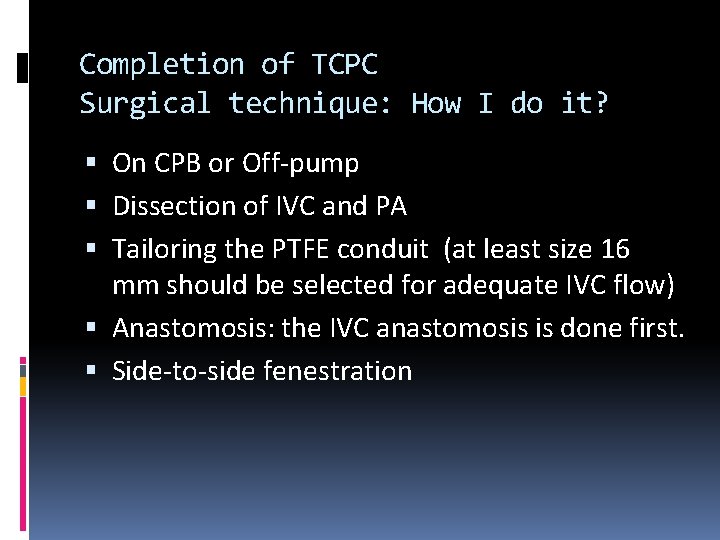
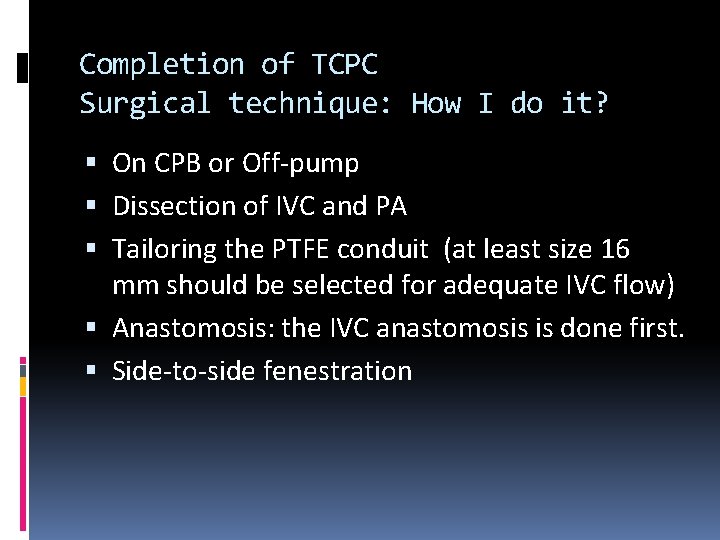
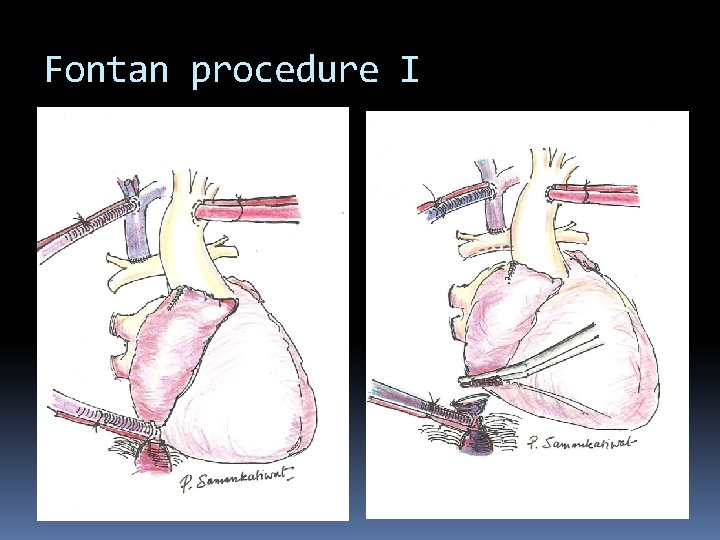
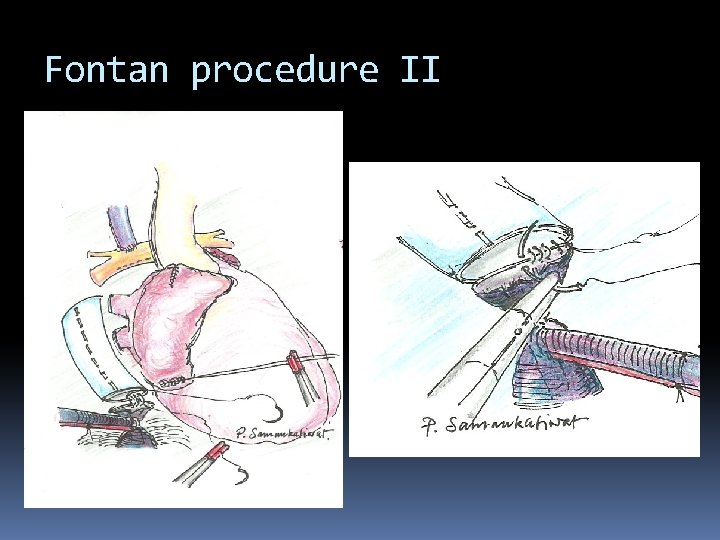
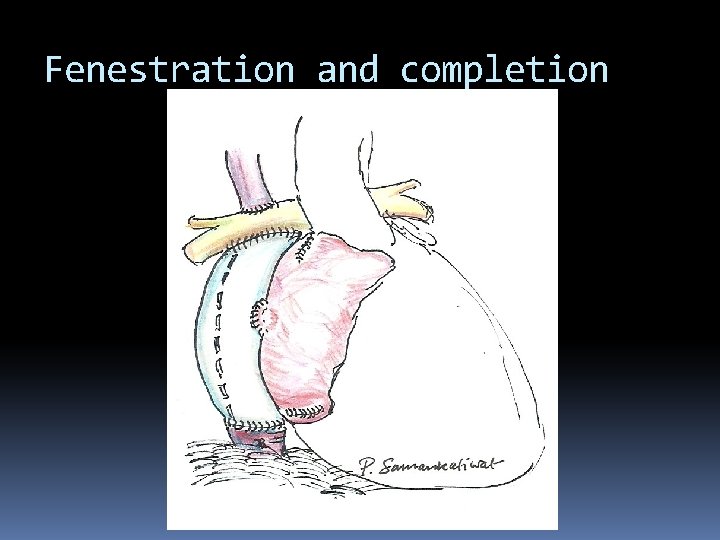
Completion of TCPC Surgical technique: How I do it? On CPB or Off-pump Dissection of IVC and PA Tailoring the PTFE conduit (at least size 16 mm should be selected for adequate IVC flow) Anastomosis: the IVC anastomosis is done first. Side-to-side fenestration
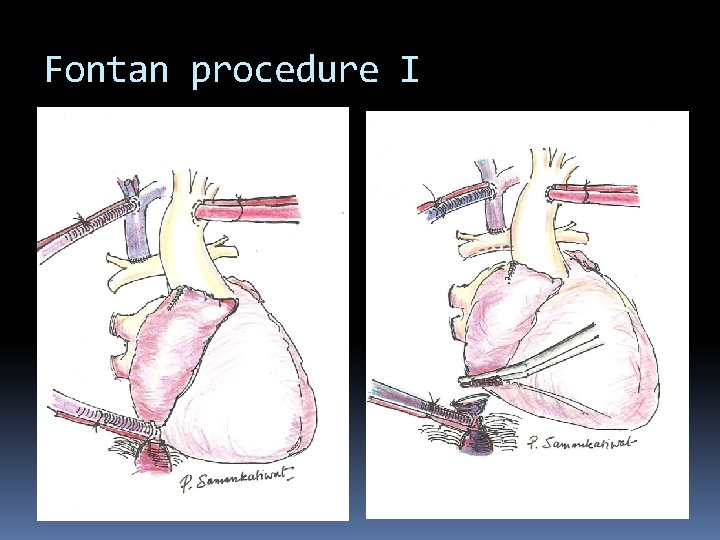
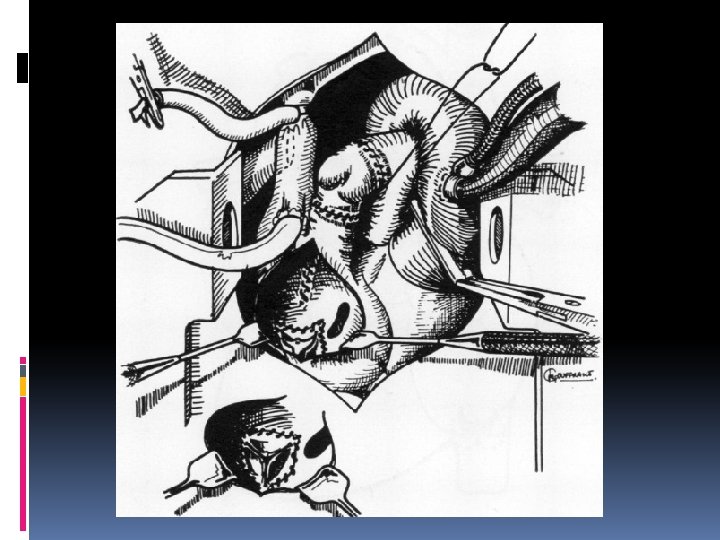
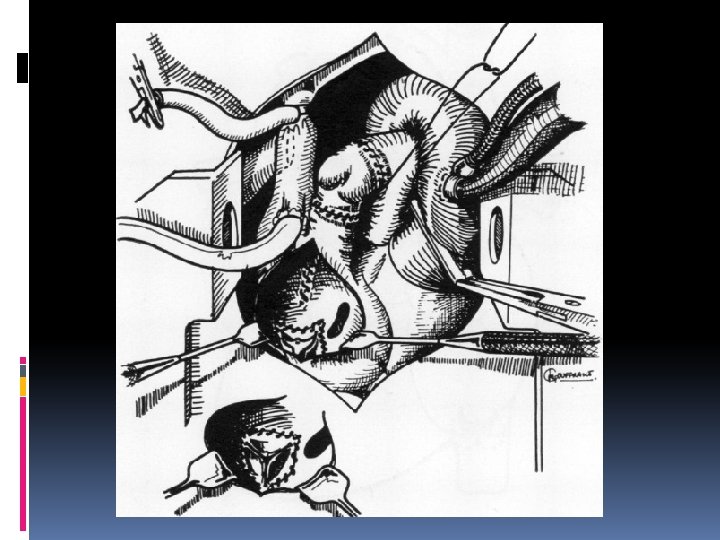
Fontan procedure I
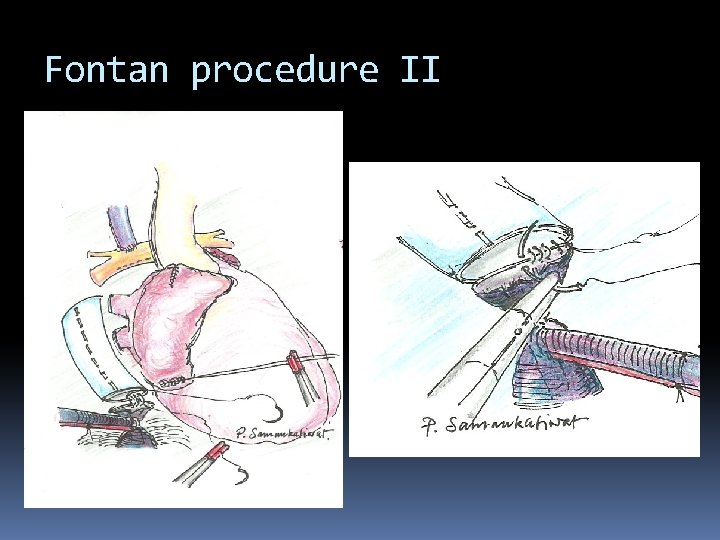
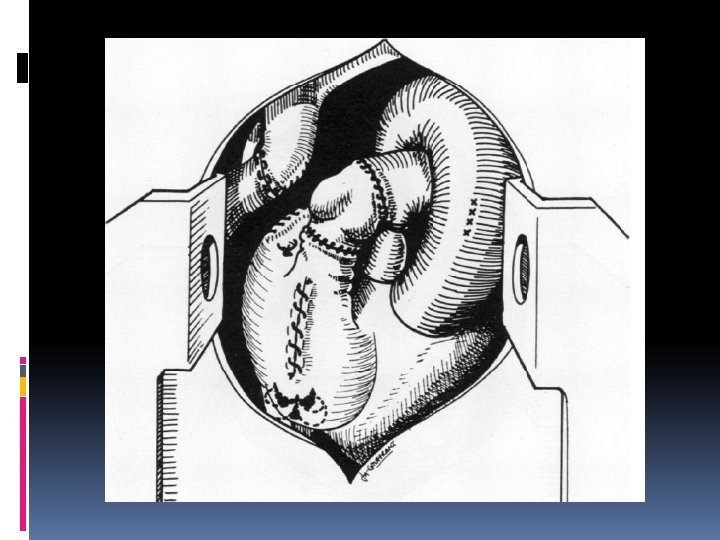
Fontan procedure II
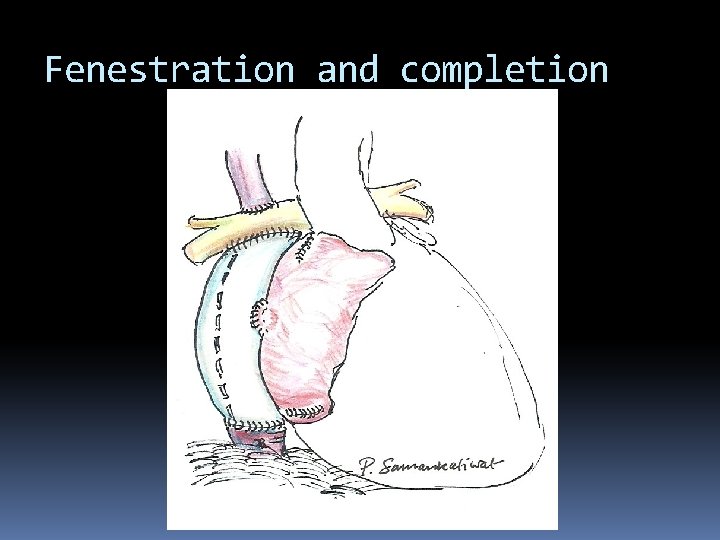
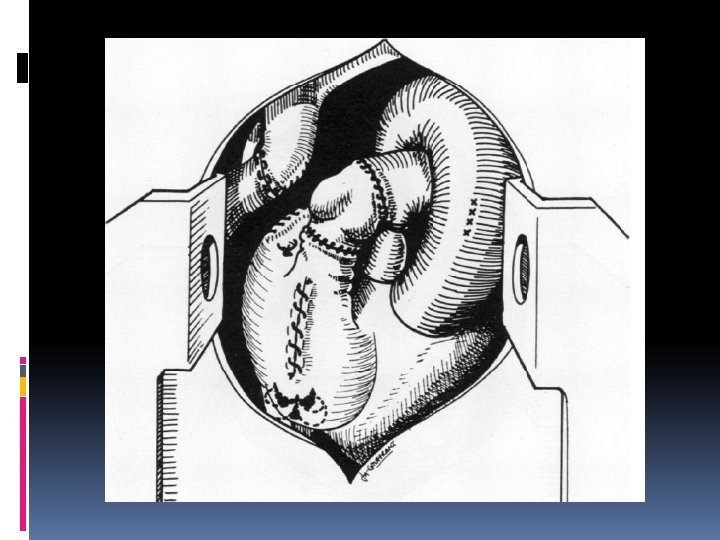
Fenestration and completion
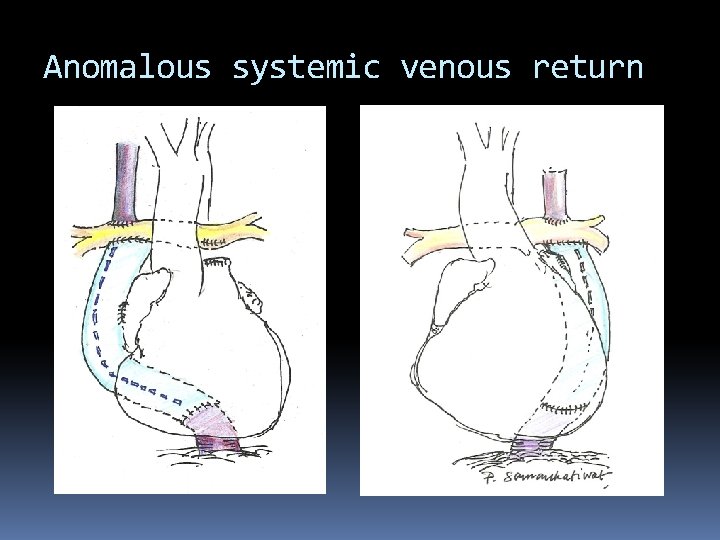
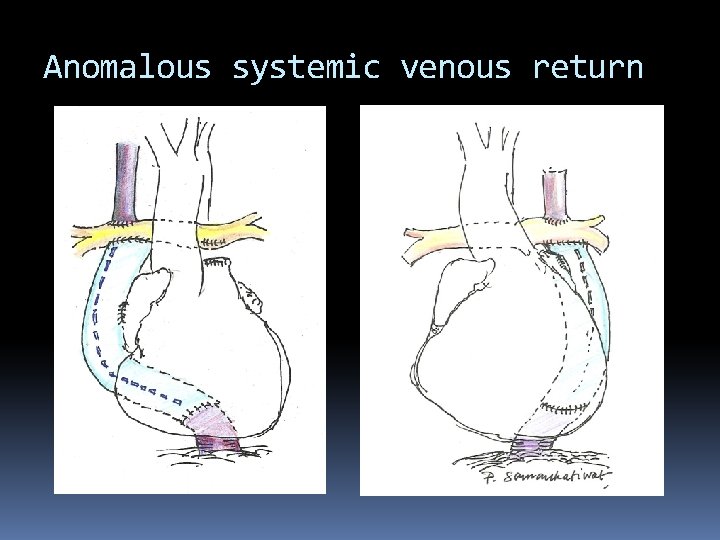
Anomalous systemic venous return
Challenges Anatomical and technical Branch pulmonary artery stenosis and disconnected pulmonary artery Dextrocardia and Mesocardia Abnormal anatomy or position of the IVC Fenestration or non-fenestration Physiological Pulmonary hypertension
Advantage of fenestration Debate on routine fenestration Beneficial in high-risk Fontan Standard-risk group controversial Randomised-controlled trial 49 cases underwent Fontan (< 2 risk factors) 25 fenestrated, 24 non-fenestrated 6 LT, 43 ECC Fenestrated group: less hospital stay, shorter duration of pleural drainage and less additional procedures Lemler MS, Scott WA, Leonard SR, et al. Circulation 2002; 105; 207 -212
Factors associated with poor outcome Systemic ventricular dysfunction (EDP > 12) Increased pulmonary arterial pressure (mean > 15) Increased pulmonary vascular resistance (>2) Atrioventricular valve regurgitation Distorted pulmonary artery Anomalous pulmonary venous connection
Postoperative care Cardiac output depends primarily on pulmonary vascular resistance (PVR) and systemic ventricular function Positioning Extubation as early as possible Inotropes Vasodilators Reduction of pulmonary arterial pressure Anticoagulation: warfarin (how long? ? ? ) Only aspirin: enough? ? ? Ann Thorac Surg. 2002 Jan; 73(1): 64 -8. (St Christopher Hospital, Philadelphia)
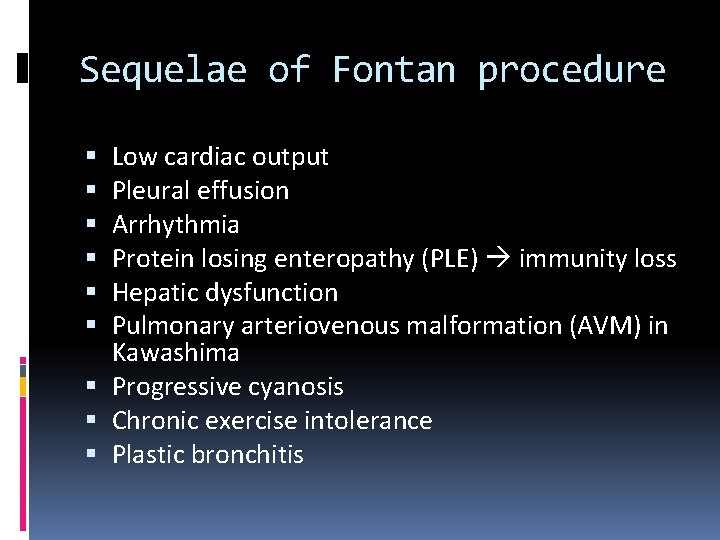
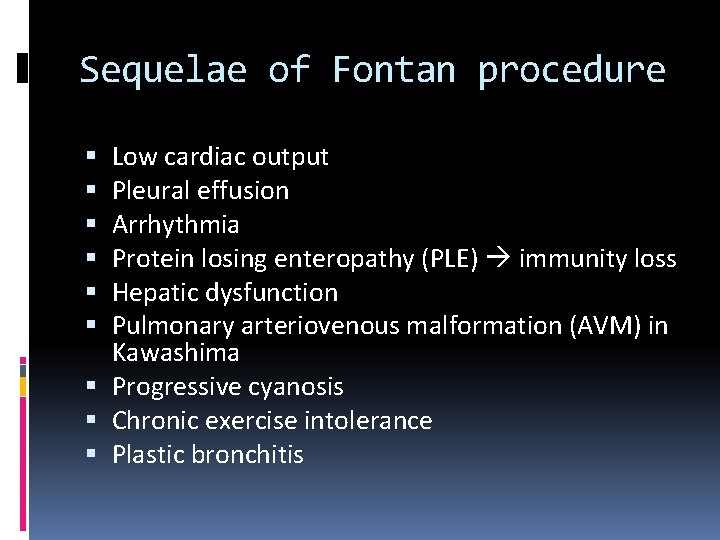
Sequelae of Fontan procedure Low cardiac output Pleural effusion Arrhythmia Protein losing enteropathy (PLE) immunity loss Hepatic dysfunction Pulmonary arteriovenous malformation (AVM) in Kawashima Progressive cyanosis Chronic exercise intolerance Plastic bronchitis
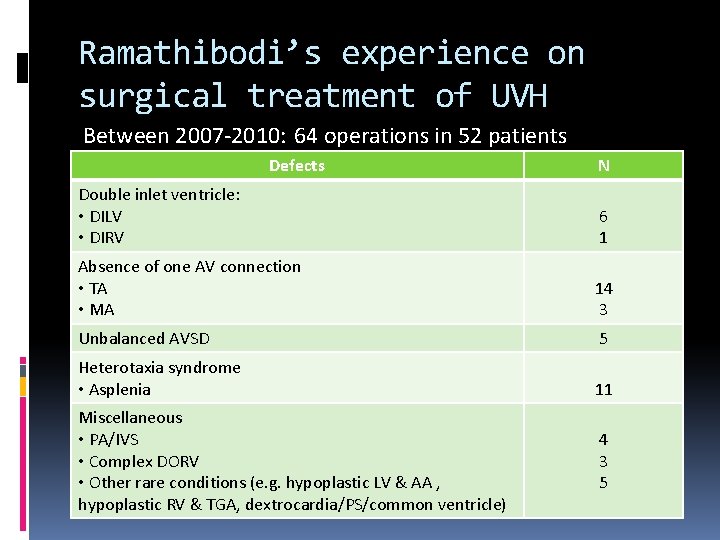
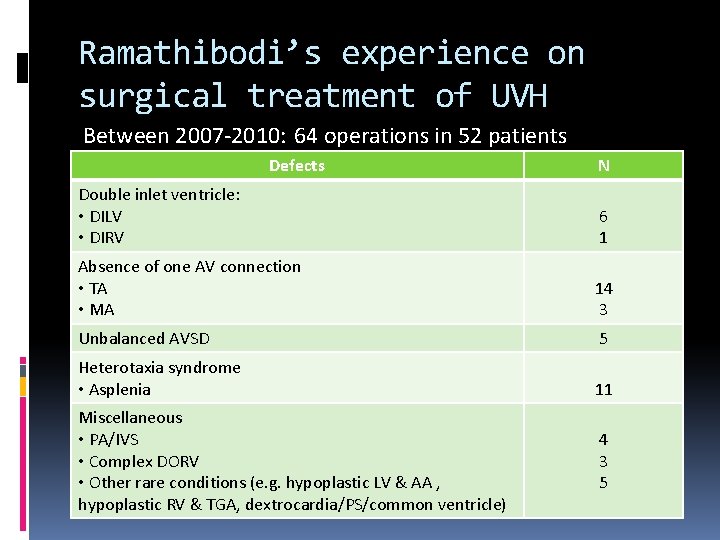
Ramathibodi’s experience on surgical treatment of UVH Between 2007 -2010: 64 operations in 52 patients Defects N Double inlet ventricle: • DILV • DIRV 6 1 Absence of one AV connection • TA • MA 14 3 Unbalanced AVSD 5 Heterotaxia syndrome • Asplenia 11 Miscellaneous • PA/IVS • Complex DORV • Other rare conditions (e. g. hypoplastic LV & AA , hypoplastic RV & TGA, dextrocardia/PS/common ventricle) 4 3 5
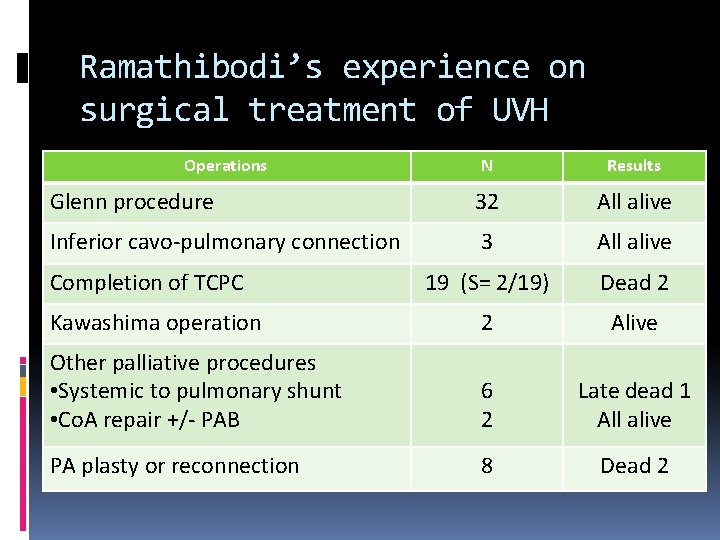
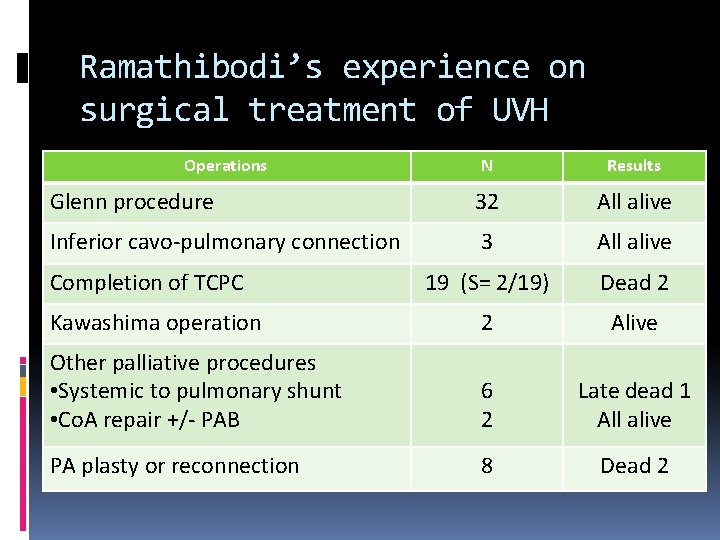
Ramathibodi’s experience on surgical treatment of UVH Operations N Results Glenn procedure 32 All alive Inferior cavo-pulmonary connection 3 All alive 19 (S= 2/19) Dead 2 Kawashima operation 2 Alive Other palliative procedures • Systemic to pulmonary shunt • Co. A repair +/- PAB 6 2 Late dead 1 All alive PA plasty or reconnection 8 Dead 2 Completion of TCPC

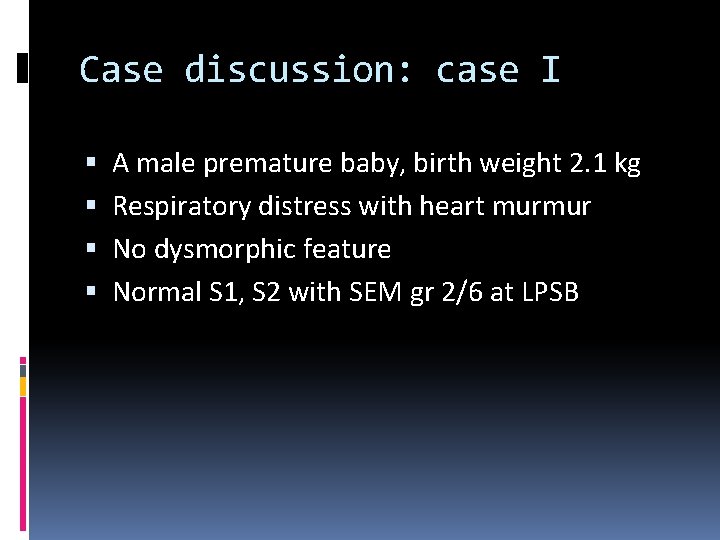
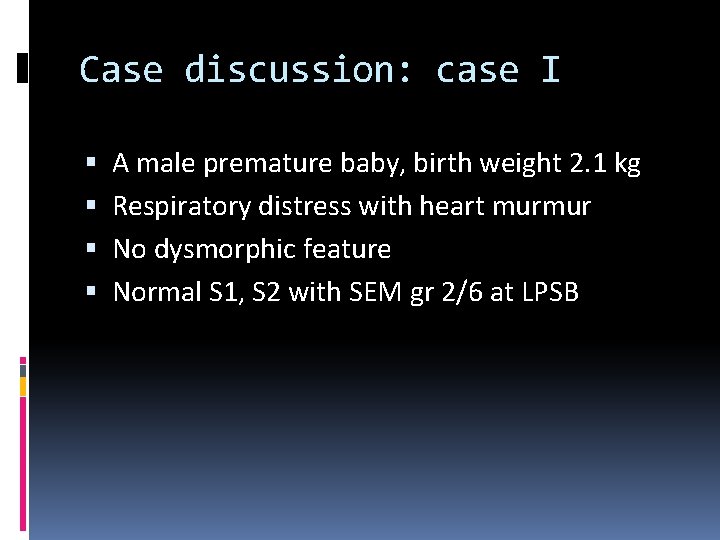
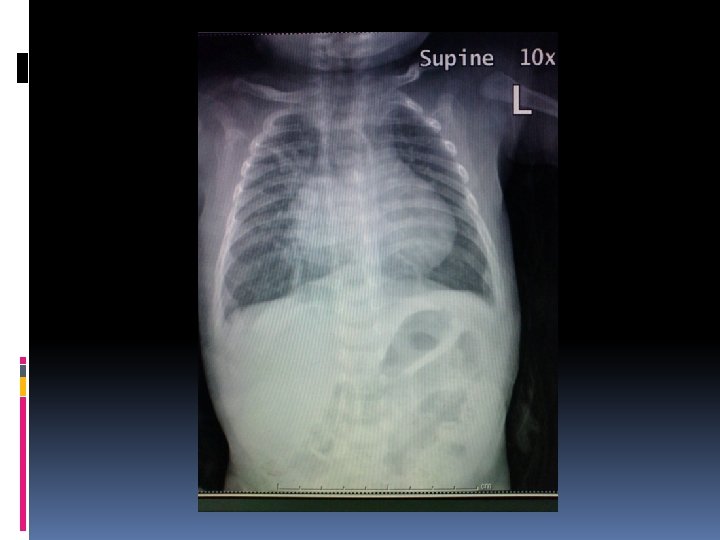
Case discussion: case I A male premature baby, birth weight 2. 1 kg Respiratory distress with heart murmur No dysmorphic feature Normal S 1, S 2 with SEM gr 2/6 at LPSB

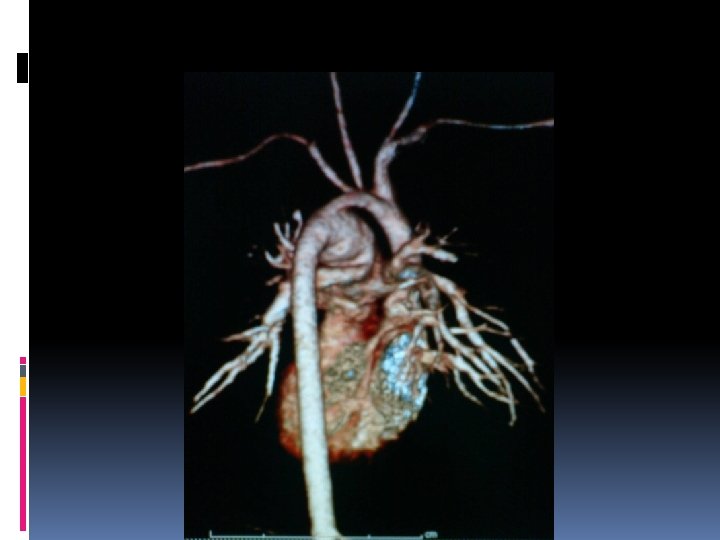
Investigation Echocardiography Single functioning morphologic RV, DIRV, DORV, rudimentary LV, large bulboventricular foramen Mild MS, No AS, No PS hypoplastic aortic arch 3 mm, severe Co. A 2. 5 mm, PDA 3. 3 mm CTA heart


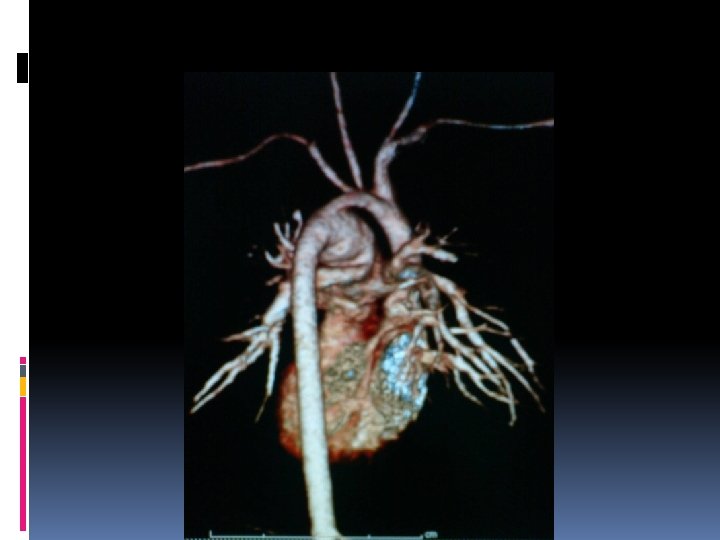
Operation and findings Severe coarctation of the aorta and hypoplastic aortic arch Hypoplastic LV Deep hypothermia + circulatory arrest Resection and end-to-end anastomosis Pulmonary artery banding
Case II 1 -y-2 -mo-old boy Cyanotic since birth Systolic ejection murmur gr 4/6 at LPSB

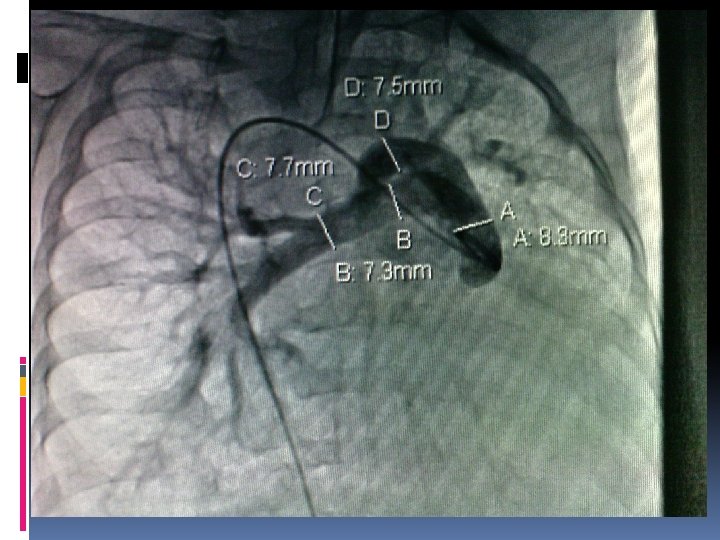
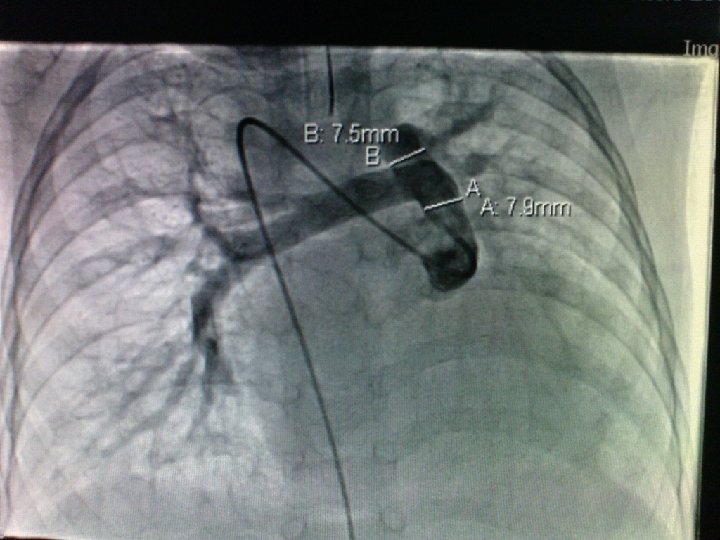
Investigation Echocardiography truncus arteriosus type I with moderate truncal valve regurgitation Cardiac catheterisation truncus arteriosus type I with PHT PVR 6 Woods unit

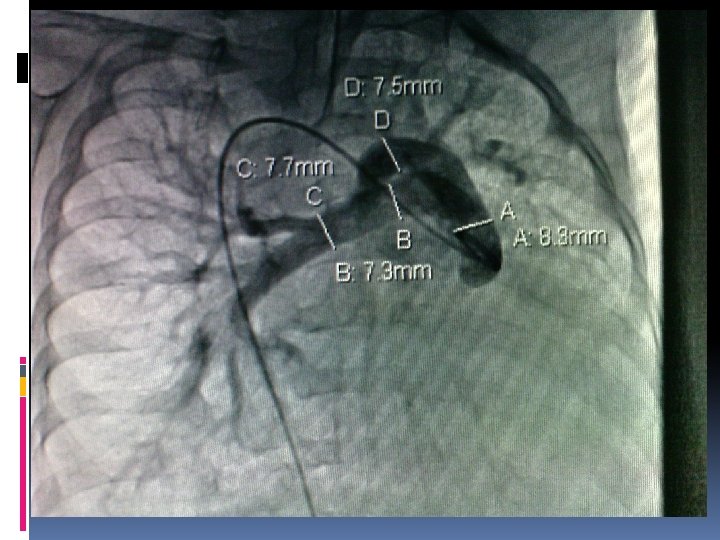
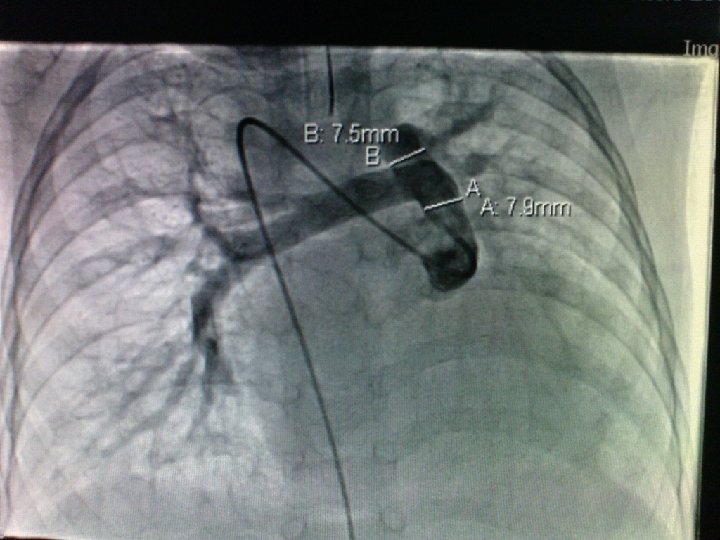
Findings and procedure Truncus type I, right sided aortic arch RPA & LPA 10 mm Tricuspid truncal valve with regurgitation due to redundancy of posterior truncal cusp Rastelli operation (using 13 mm pulmonary homograft)
