Fatal complication in varicose vein treatment with vein




- Slides: 14
Fatal complication in varicose vein treatment with vein stenting Jenny Plácido-Disla, MD Bora Toklu, MD Ramesh M Gowda, MD Mount Sinai Heart at Mount Sinai Beth Israel, New York, NY

Jenny Plácido-Disla, MD (presenter) Bora Toklu, MD Ramesh M Gowda, MD We have no relevant financial relationships.
Learning objectives v. Indications for revascularization in varicose vein treatment v. Complications in venous stent placement v. Risk factors for venous stent migration

Clinical Presentation • A 55 year-old woman with past medical history of varicose veins presented to emergency department with sudden onset of chest pain and altered mental status. The morning prior to the day of presentation, patient underwent bilateral iliac vein and a single suprarenal inferior vena cava stenting for varicose vein treatment. A few hours after venous stenting was performed, patient developed severe chest pain prompting an EMS call. Upon arrival to the hospital, patient was found to be hypotensive with systolic blood pressure in 60 s mm. Hg. Patient was emergently intubated and started on vasopressors.

Physical Exam Vital Signs: BP 102/74, HR 88 on norepinephrine 10 mcg/min, RR 14, Sat 88% on 100% FIO 2 Mechanical ventilator settings: A/C, TV: 450/RR: 14/ 100% FIO 2/PEEP: 5 Physical exam: – Neck: supple, no JVD – General: pale appearing, sedated and intubated on mechanical ventilation – Heart: audible S 1 and S 2, rate rhythm regular, II/VI systolic ejection murmur at the apex – Lung: Clear to auscultation bilaterally – Abdomen: soft, non-tender – Extremities: cold extremities, distal pulses intact, no peripheral edema
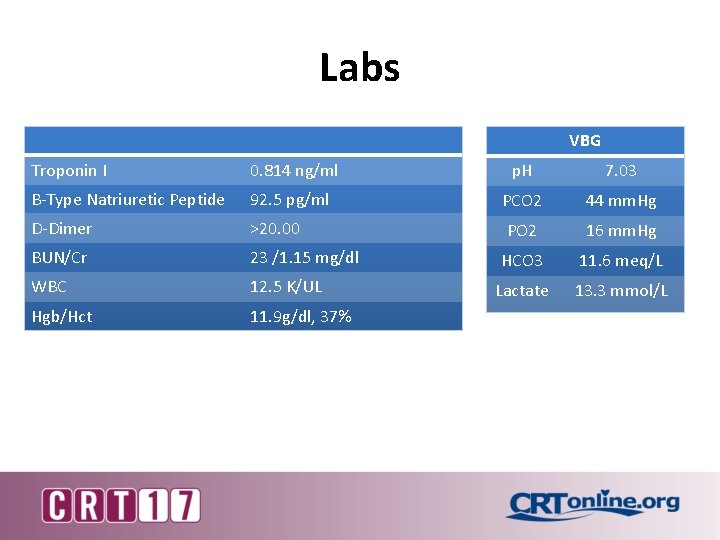
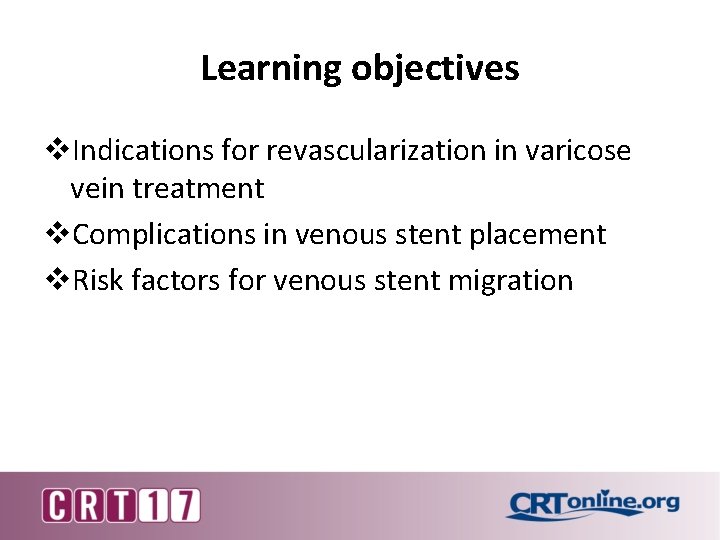
Labs VBG Troponin I 0. 814 ng/ml p. H 7. 03 B-Type Natriuretic Peptide 92. 5 pg/ml PCO 2 44 mm. Hg D-Dimer >20. 00 PO 2 16 mm. Hg BUN/Cr 23 /1. 15 mg/dl HCO 3 11. 6 meq/L WBC 12. 5 K/UL Lactate 13. 3 mmol/L Hgb/Hct 11. 9 g/dl, 37%
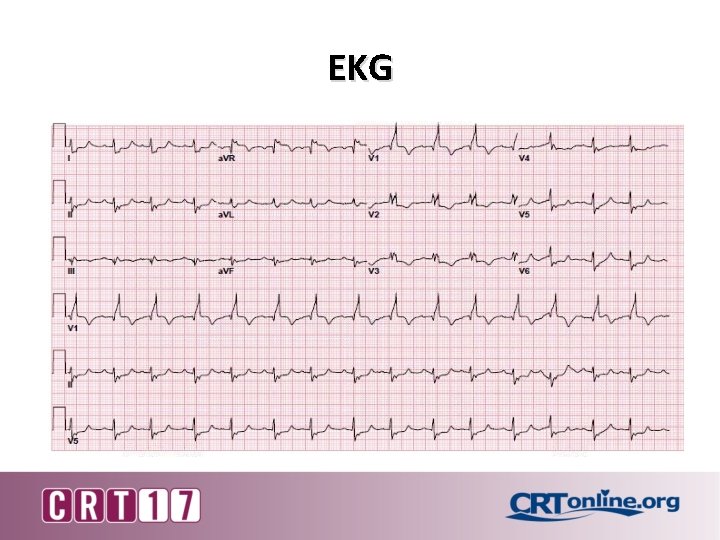
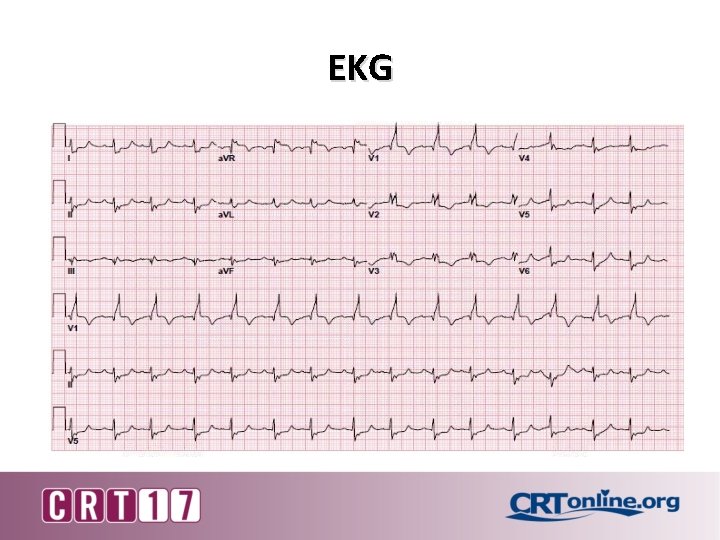
EKG
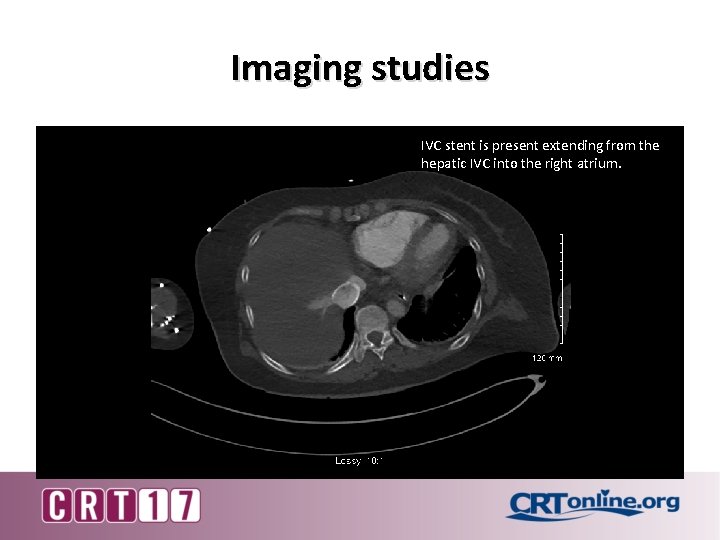
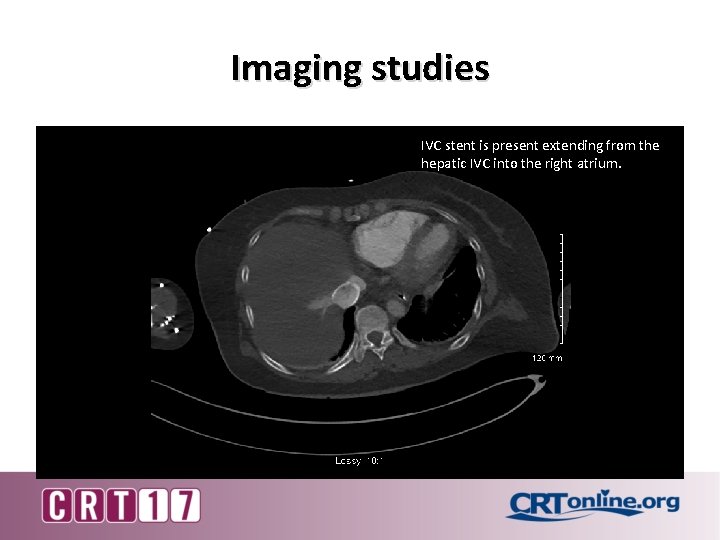
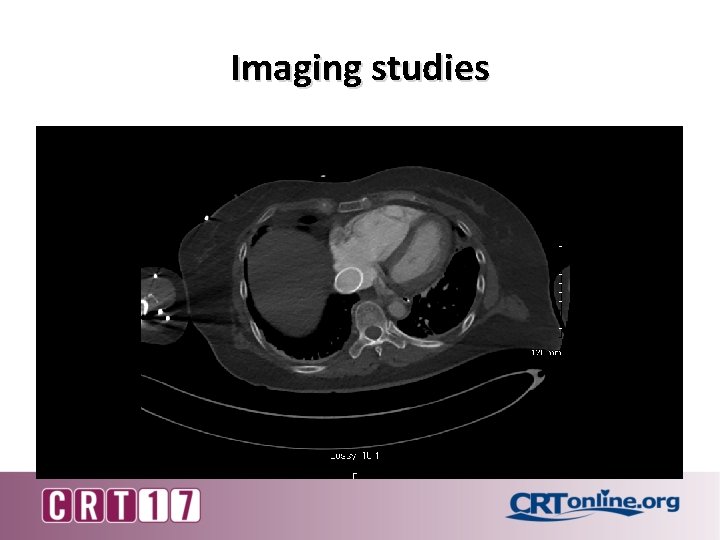
Imaging studies IVC stent is present extending from the hepatic IVC into the right atrium.
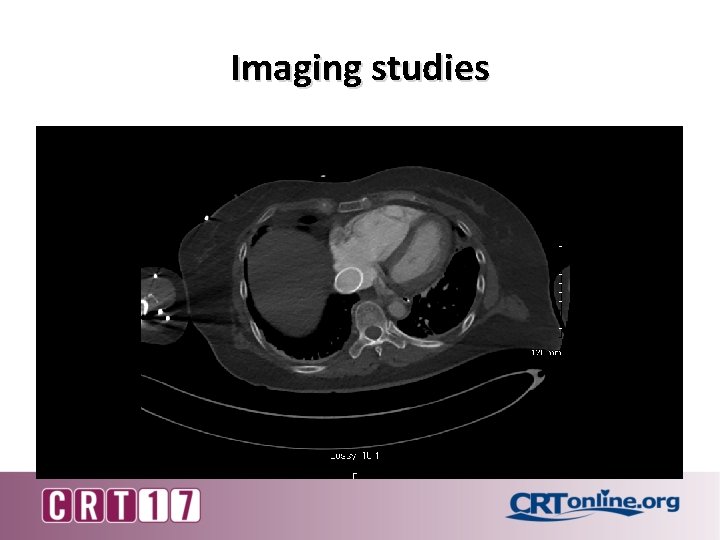
Imaging studies

Imaging studies
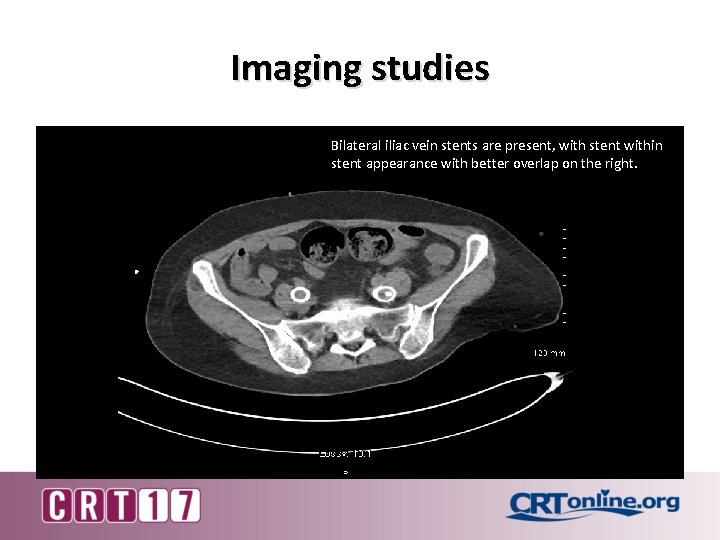
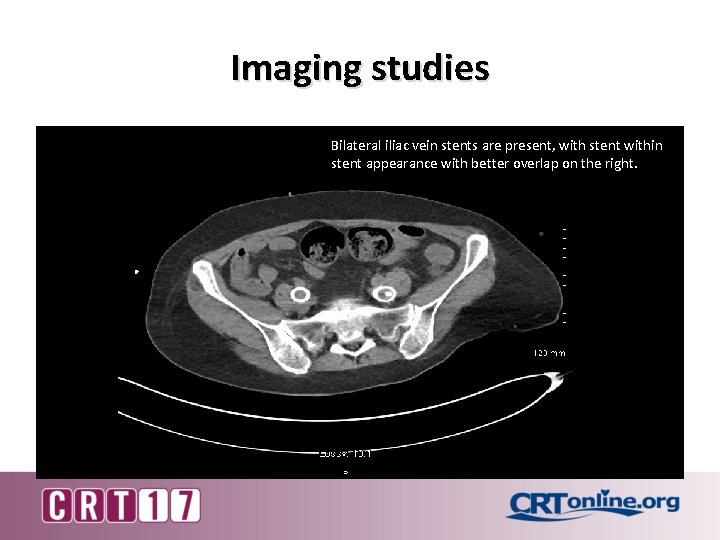
Imaging studies Bilateral iliac vein stents are present, with stent within stent appearance with better overlap on the right.
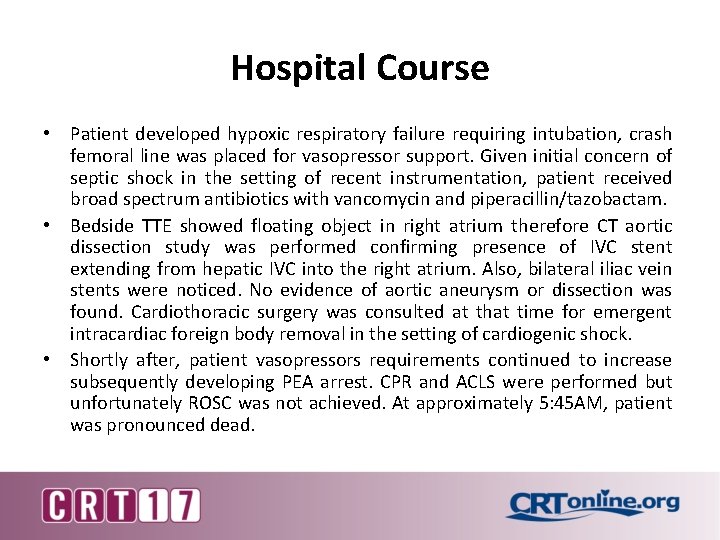
Hospital Course • Patient developed hypoxic respiratory failure requiring intubation, crash femoral line was placed for vasopressor support. Given initial concern of septic shock in the setting of recent instrumentation, patient received broad spectrum antibiotics with vancomycin and piperacillin/tazobactam. • Bedside TTE showed floating object in right atrium therefore CT aortic dissection study was performed confirming presence of IVC stent extending from hepatic IVC into the right atrium. Also, bilateral iliac vein stents were noticed. No evidence of aortic aneurysm or dissection was found. Cardiothoracic surgery was consulted at that time for emergent intracardiac foreign body removal in the setting of cardiogenic shock. • Shortly after, patient vasopressors requirements continued to increase subsequently developing PEA arrest. CPR and ACLS were performed but unfortunately ROSC was not achieved. At approximately 5: 45 AM, patient was pronounced dead.
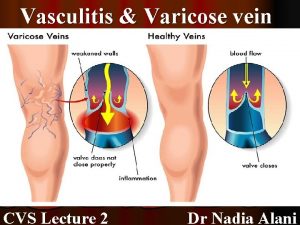
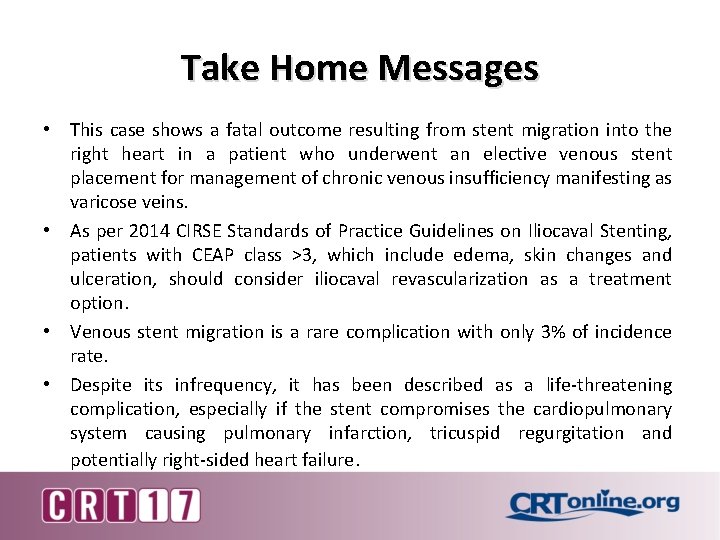
Take Home Messages • This case shows a fatal outcome resulting from stent migration into the right heart in a patient who underwent an elective venous stent placement for management of chronic venous insufficiency manifesting as varicose veins. • As per 2014 CIRSE Standards of Practice Guidelines on Iliocaval Stenting, patients with CEAP class >3, which include edema, skin changes and ulceration, should consider iliocaval revascularization as a treatment option. • Venous stent migration is a rare complication with only 3% of incidence rate. • Despite its infrequency, it has been described as a life-threatening complication, especially if the stent compromises the cardiopulmonary system causing pulmonary infarction, tricuspid regurgitation and potentially right-sided heart failure.
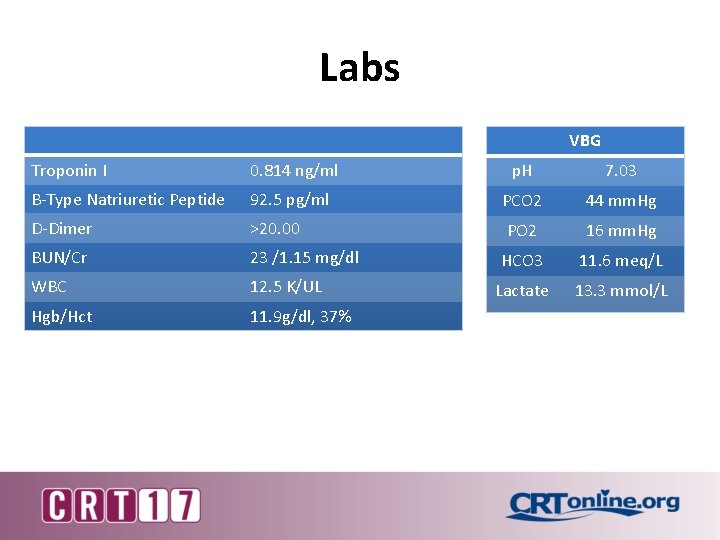
Take Home Messages • Risk factors for stent migration include stent undersizing, stent malapposition, inaccurate vessel measurement and lesions without a significant degree of obstruction. • The mortality rate of foreign body embolization to the heart ranges from 24 -60%, therefore timely intervention is indicated to prevent severe complications, such as cardiac arrhythmias, valve injury and/or myocardial perforation. • Unfortunately, our patient had a rapid deterioration complicated by cardiac arrest, therefore no intervention was performed. Appropriate indications and procedural technique is indispensable in order to avoid potentially life-threatening complications.
 Hsp vs itp
Hsp vs itp Pratt test varicose veins
Pratt test varicose veins Trendelenburg procedure
Trendelenburg procedure 1984 julia
1984 julia Anoplophora luciphor
Anoplophora luciphor Left posterior oblique
Left posterior oblique Hyperestrinism cirrhosis
Hyperestrinism cirrhosis Most common complication of central venous catheter
Most common complication of central venous catheter The necklace plot
The necklace plot Diabetic foot
Diabetic foot Pyramid principle situation complication answer solution
Pyramid principle situation complication answer solution Complication of blood transfusion
Complication of blood transfusion What is the purpose of narrative text
What is the purpose of narrative text Situation complication question answer
Situation complication question answer Most common complication of central venous catheter
Most common complication of central venous catheter