Evolution of Contraception Potions to Progestins Jennifer Mc



- Slides: 48
Evolution of Contraception: Potions to Progestins Jennifer Mc. Donald DO
Basics • 48% pregnancies in the US are unintended • Age group with second highest rate of unintended pregnancy is women 40 -44 • Half of all unintended pregnancies end in abortion • 45% of abortions occur in women 25 -30 years old and 24% occurred >30 years old
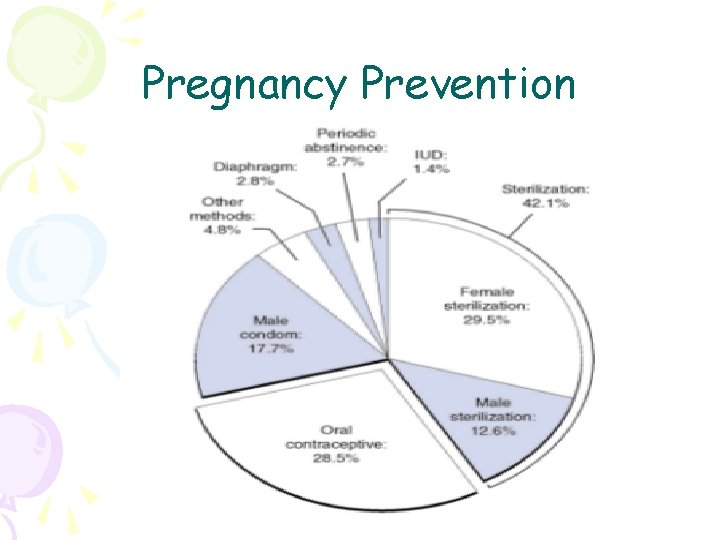
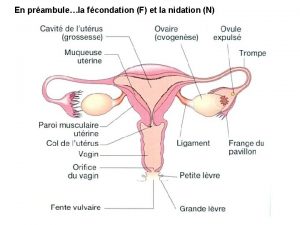
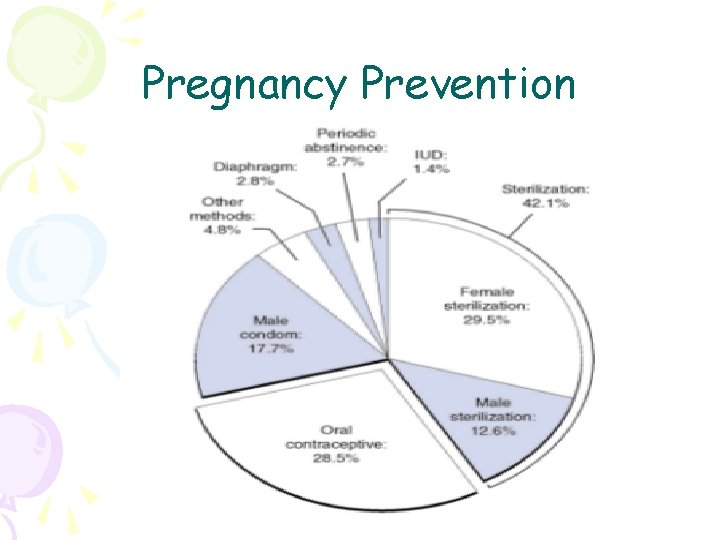
Pregnancy Prevention
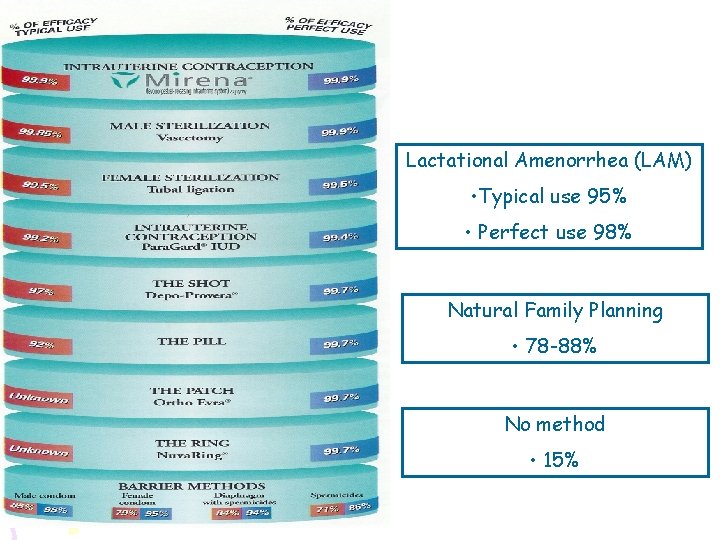
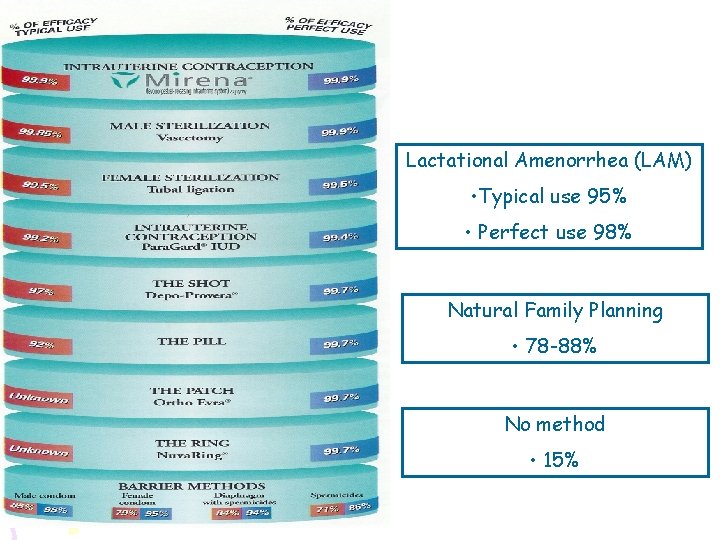
Lactational Amenorrhea (LAM) • Typical use 95% • Perfect use 98% Natural Family Planning • 78 -88% No method • 15%
Ancient “Technology” • Vaginally administered honey • Drinking the water used to wash the dead • “Sponges” made from crocodile dung or fermented dough • Lemon wedges over the cervix • Middle Ages women died of lead, arsenic, mercury, or strychnine poisoning after drinking for theoretical contraceptive or abortifacient effects • Earwax of a mule worn as an amulet to ward off pregnancy
“Modern” Contraception • 1930 s Austrian physiologist suggested extracts of ovarian hormones could inhibit fertility • Researched hampered by unavailability of hormones • 1960 s FDA approved first oral contraceptive • Estimates suggest that by the end of their reproductive years 80% of US women will have used OCs for an average of 5 years
Development of Non-hormonal Means • First IUD made of silk suture in 1929 reported a 3% pregnancy rate • 1930 s rings wrapped in silver wire 1. 6% pregnancy rate • 1960 s first copper IUDs introduced • 1980 s litigation involving Dalkon Shield led to decrease in IUD use • Today IUDs used by 2% US women • 2 available forms: Progesterone (Mirena/Progestasert) and copper (Paraguard)
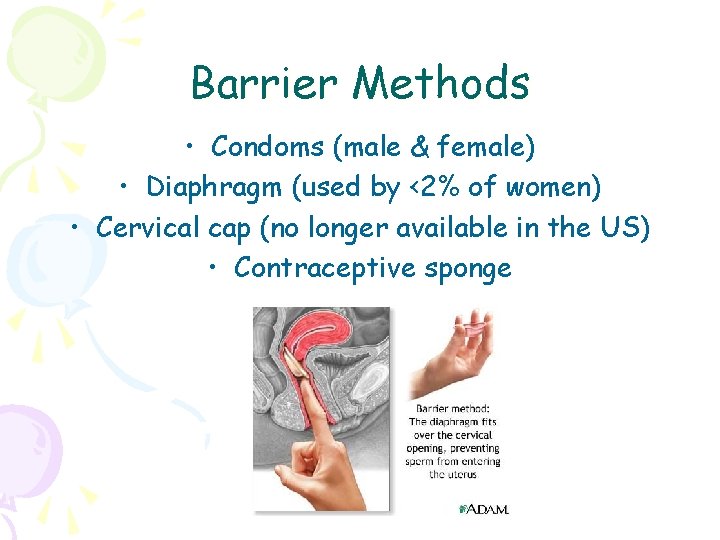
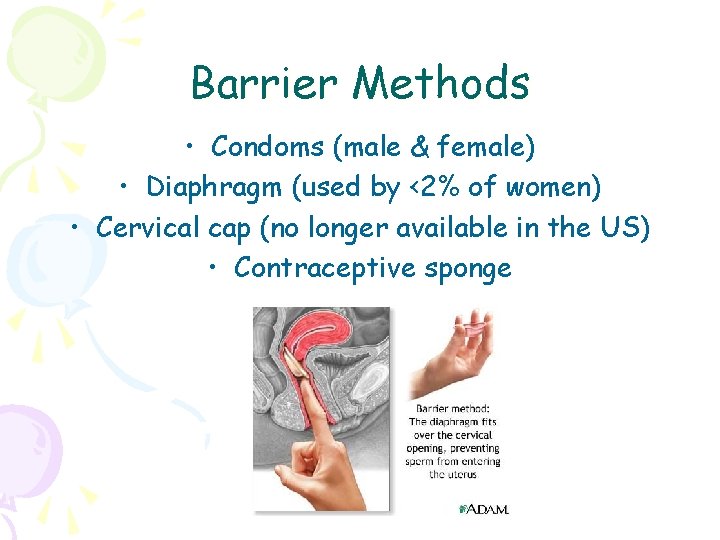
Barrier Methods • Condoms (male & female) • Diaphragm (used by <2% of women) • Cervical cap (no longer available in the US) • Contraceptive sponge
Progestin Only Options Injection Depo Provera Intrauterine Devices Mirena – good for up to 5 years Progestasert – inserted yearly Implants Implanon – good up to 3 years
Mechanism of Action Progestin Only Forms • Blocks LH • Maintains thickness of cervical mucous • Reduces mobility of fallopian tubes • Changes uterine lining making it unfavorable for implantation
Side Effects Progestin Only • Headache • Vaginitis • Breast pain • Weight gain • Acne Most disappear within a few months of starting
Depo Provera • FDA approval for contraception in 1991 • Given as an IM injection every 11 -13 weeks • Suppresses ovulation • Depresses ovarian steroidogenesis • Estradiol can dip into menopausal ranges leading to increased bone mineral resorption • Continuous use should not exceed 2 years (not lifetime) • Menstrual changes • 50% amenorrheic by 12 months • 75% amenorrheic by 24 months
Depo Provera cont. • Weight gain more variable than with other methods • Return to fertility can be delayed (median 910 months) • May be used in breast feeding • May be used in women with contraindications to estrogen containing products (eg. Smokers over 35, thrombophilias)
Implanon • Available in Europe and Asia for 8 years and used by 2 million women • Easier insertion and removal than its predecessor Norplant • 99% efficacious (Pearl index 0. 38)
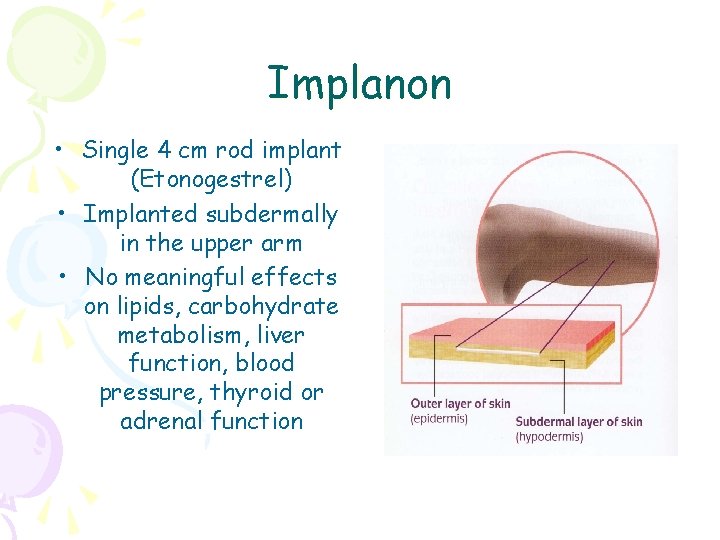
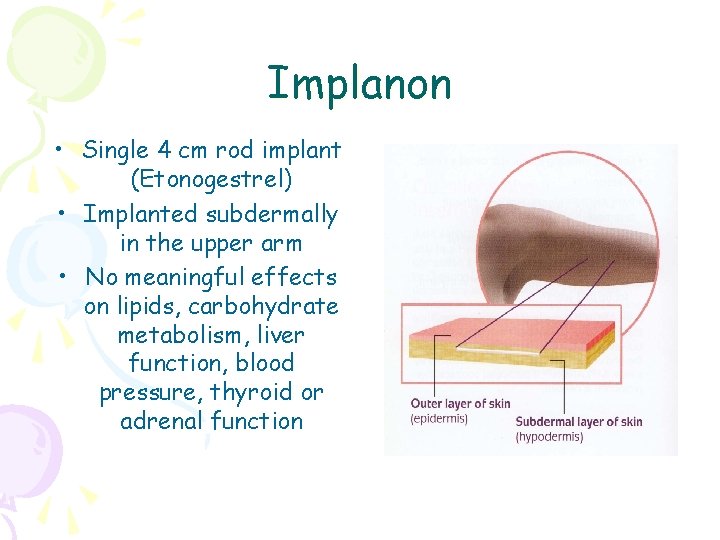
Implanon • Single 4 cm rod implant (Etonogestrel) • Implanted subdermally in the upper arm • No meaningful effects on lipids, carbohydrate metabolism, liver function, blood pressure, thyroid or adrenal function
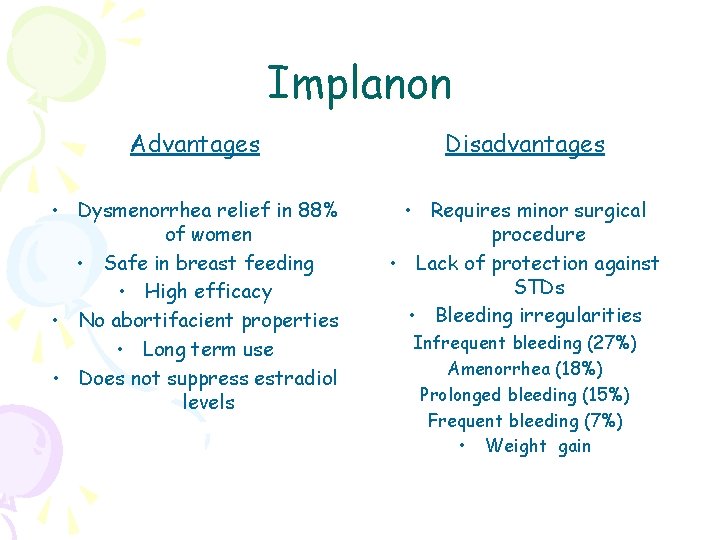
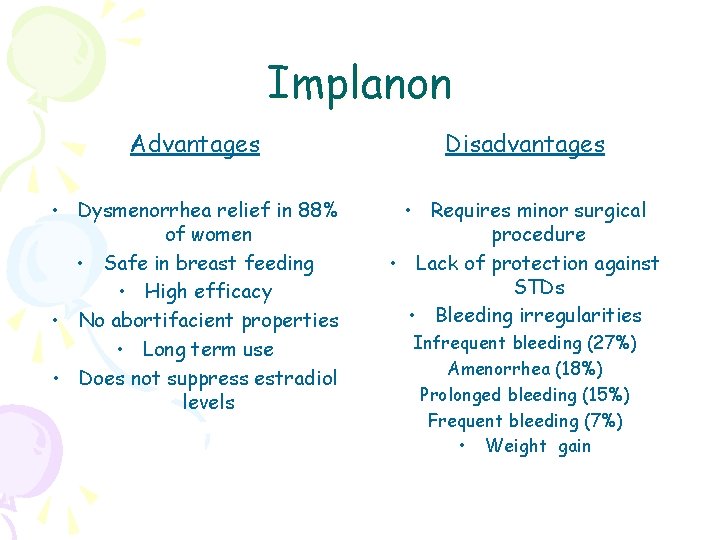
Implanon Advantages Disadvantages • Dysmenorrhea relief in 88% of women • Safe in breast feeding • High efficacy • No abortifacient properties • Long term use • Does not suppress estradiol levels • Requires minor surgical procedure • Lack of protection against STDs • Bleeding irregularities Infrequent bleeding (27%) Amenorrhea (18%) Prolonged bleeding (15%) Frequent bleeding (7%) • Weight gain
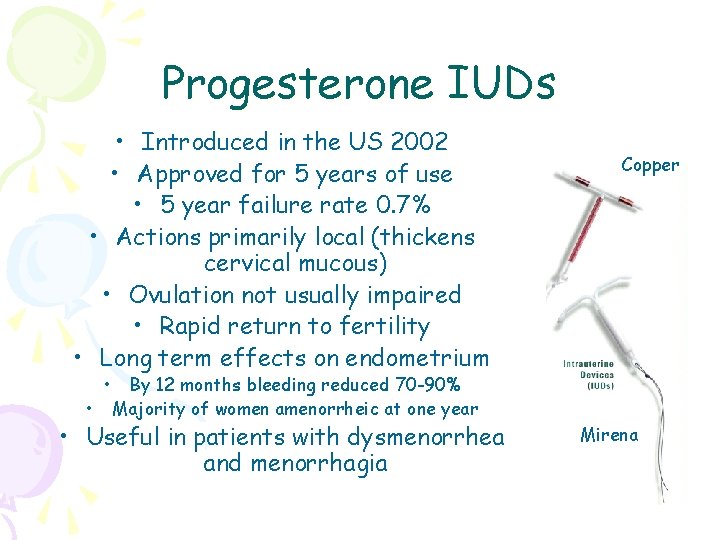
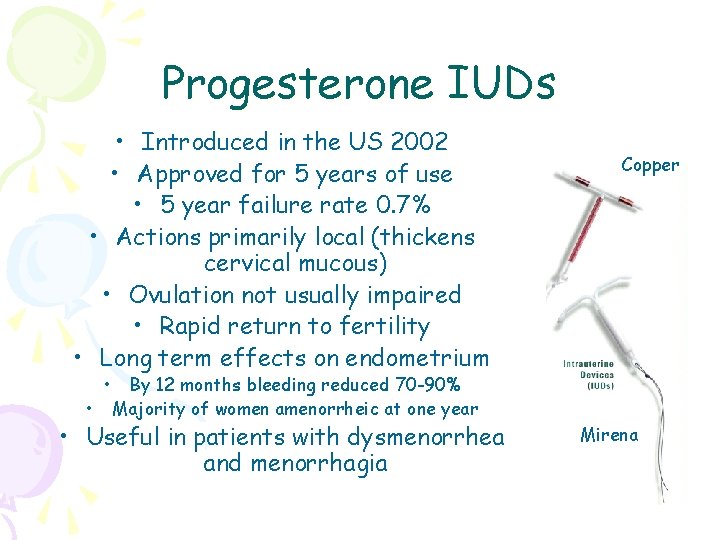
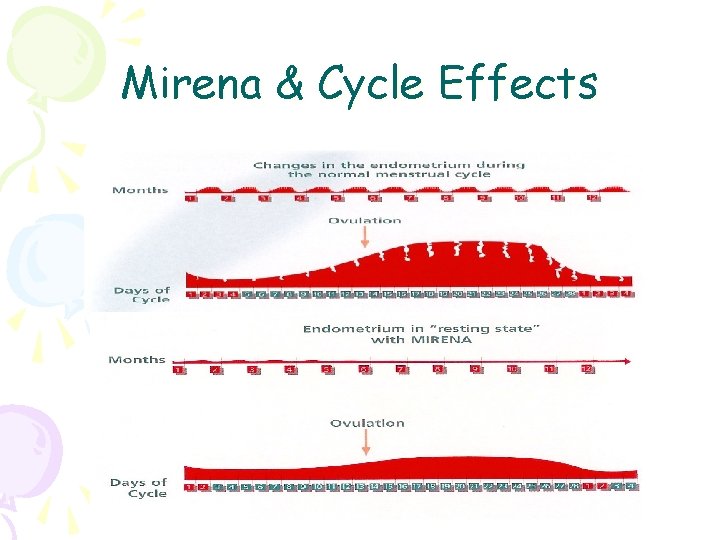
Progesterone IUDs • Introduced in the US 2002 • Approved for 5 years of use • 5 year failure rate 0. 7% • Actions primarily local (thickens cervical mucous) • Ovulation not usually impaired • Rapid return to fertility • Long term effects on endometrium • • Copper By 12 months bleeding reduced 70 -90% Majority of women amenorrheic at one year • Useful in patients with dysmenorrhea and menorrhagia Mirena
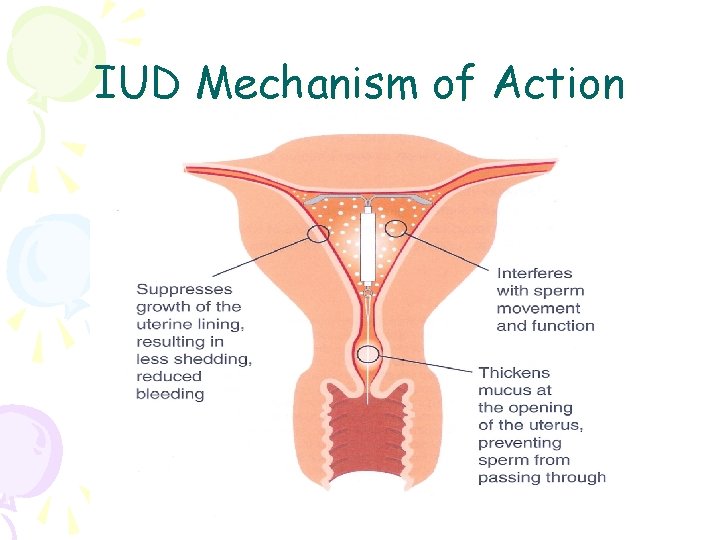
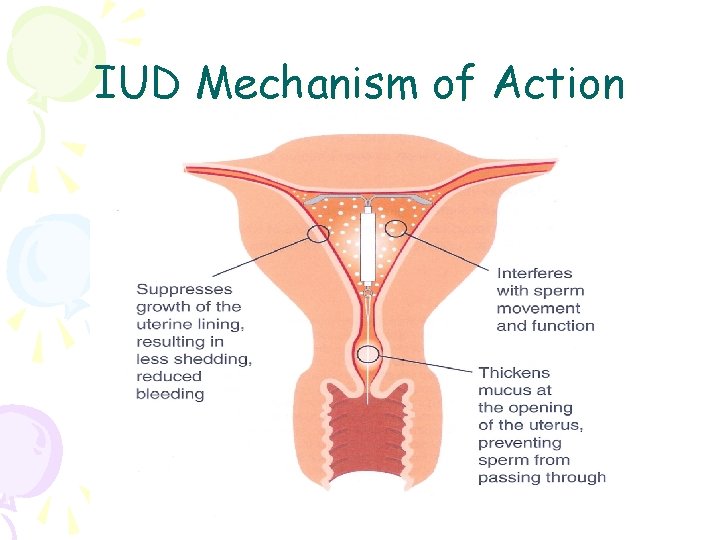
IUD Mechanism of Action
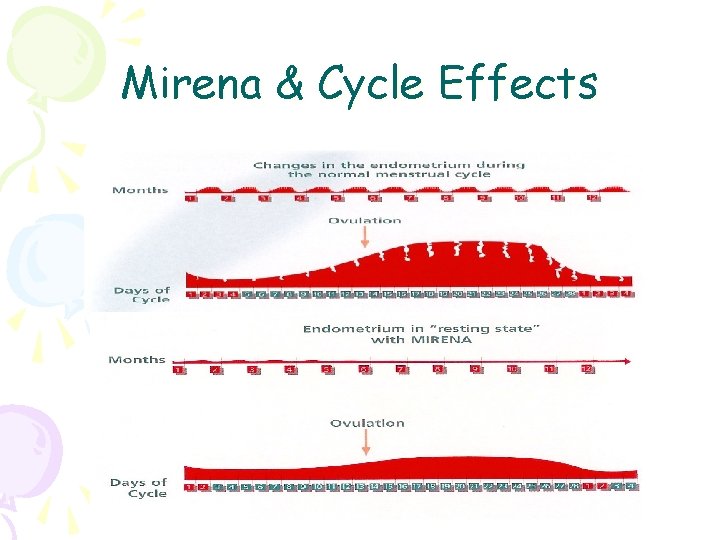
Mirena & Cycle Effects
Who Shouldn’t Use the IUD • History of pelvic inflammatory disease • Copper allergy (Copper IUDs only) • Multiple sexual partners • Uterine abnormalities • Untreated infections of the cervix or uterus • History of ectopic pregnancy
Oral Contraceptives • Combination of ethinyl estradiol and one of several progestins or progestin alone Mechanism of Action • Inhibit the LH surge needed for ovulation (progestin) • Modulating Gn. RH release/FSH production (estrogen) • Alter cervical mucous • Induce atrophic changes in the endometrium
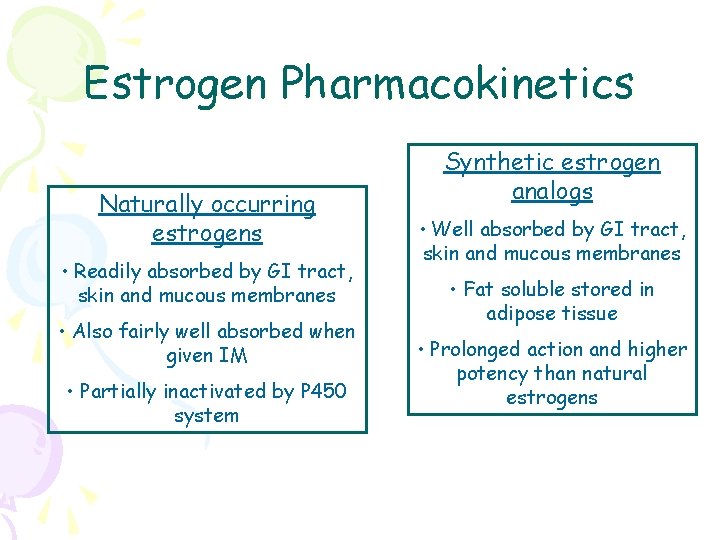
Estrogen Pharmacokinetics Naturally occurring estrogens • Readily absorbed by GI tract, skin and mucous membranes • Also fairly well absorbed when given IM • Partially inactivated by P 450 system Synthetic estrogen analogs • Well absorbed by GI tract, skin and mucous membranes • Fat soluble stored in adipose tissue • Prolonged action and higher potency than natural estrogens
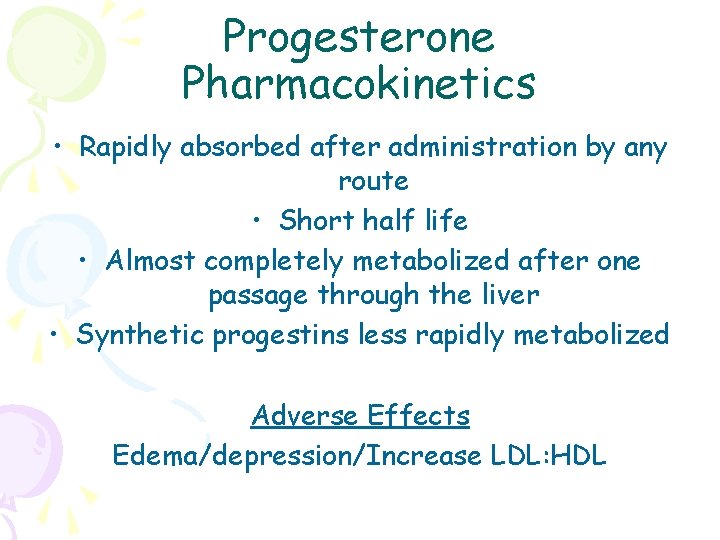
Progesterone Pharmacokinetics • Rapidly absorbed after administration by any route • Short half life • Almost completely metabolized after one passage through the liver • Synthetic progestins less rapidly metabolized Adverse Effects Edema/depression/Increase LDL: HDL
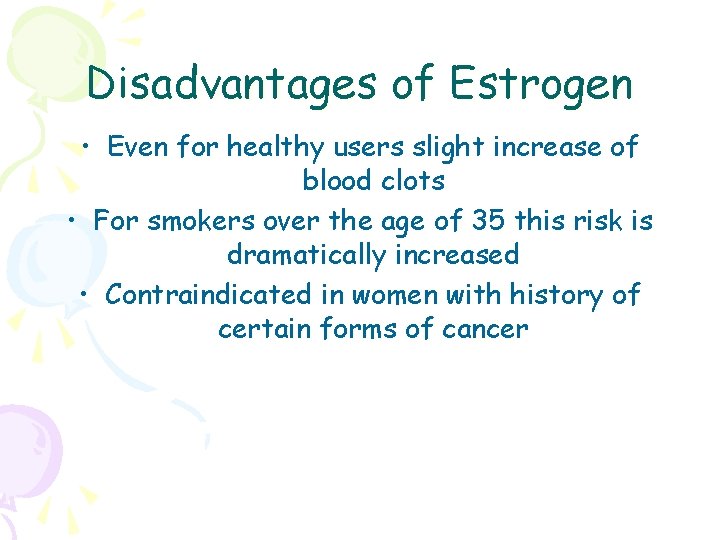
Disadvantages of Estrogen • Even for healthy users slight increase of blood clots • For smokers over the age of 35 this risk is dramatically increased • Contraindicated in women with history of certain forms of cancer
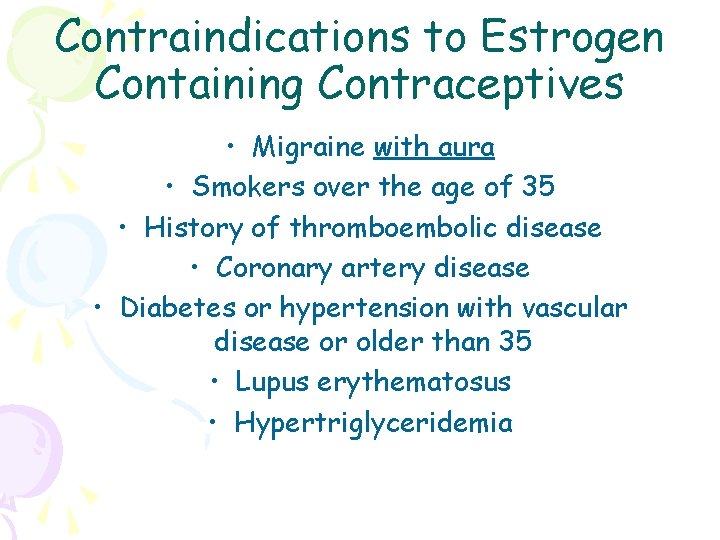
Contraindications to Estrogen Containing Contraceptives • Migraine with aura • Smokers over the age of 35 • History of thromboembolic disease • Coronary artery disease • Diabetes or hypertension with vascular disease or older than 35 • Lupus erythematosus • Hypertriglyceridemia
OCs – Noncontraceptive Benefits • Lower incidence of endometrial and ovarian cancers • Fewer ovarian cysts • Decreased risk of ectopic pregnancy • Minimize acne • Regulation of menses – lighter flow • Reduction in dysmenorrhea • Reduction in symptomatic fibrocystic breast disease • Decrease upper genital tract infection (PID)
OCs – Disadvantages • No protection against STDs • Increase in thromboembolic events • Compliance issues • Nausea/weight gain/breast tenderness • May precipitate migraine headaches
Oral Contraceptives • Combination pills • Progestin only pills • Post-coital (Emergency) contraception Mechanism of Action Suppression of ovulation by feedback inhibition of endogenous estrogen
Combination Formulations • Estrogen prevents ovulation • Progestin prevents implantation and makes cervical mucus impenetrable to sperm • Perfect use efficacy 99% • Rapid return to fertility on discontinuation Monophasic Triphasic Extended Cycle Ethinyl estradiol* Estrogen in 99% of all OCPs
Ortho Evra • Introduced in 2002 • Combination estrogen/progestin • Inhibits ovulation similar to OCPs • Each worn for 1 week at a time for 3 consecutive weeks • Fourth week is patch free • Return to fertility within one month • Weight > 198 pounds associated with higher pregnancy rates
Nuva Ring • Introduced in mid-2002 • Combination therapy • Half the estrogen dose than traditional oral contraceptives • Inserted at the top of the vagina • Slow, continuous release of hormone over a 3 week period • Return of fertility within one month


Progestin Only Pills • “Mini-pill” • Safe in breast feeding • Ovulation not necessarily affected • Must be taken at the same time every day to ensure effectiveness
Improper Counseling • 42% women will discontinue method without consulting health care provider • Poor compliance • 47% users miss one or more pills/cycle • 22% miss two or more
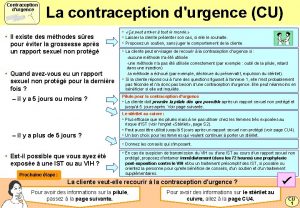
Emergency Contraception • High dose estrogen/progestin administered within 72 hours of unprotected intercourse • Two doses 12 hours apart • Single mechanism of action not identified • Inhibition or delay of ovulation • Histologic/biochemical changes in the endometrium • Alterations in tubal transport • 98% patients will menstruate by 21 days after treatment
Emergency Contraception Preven Emergency Contraceptive Kit Plan B • High incidence of nausea & vomiting • Effectiveness rate 75% If 100 women had unprotected intercourse in the middle two weeks of their cycle 8 would become pregnant. Use of emergency contraception would reduce this number to 2 (75% reduction)
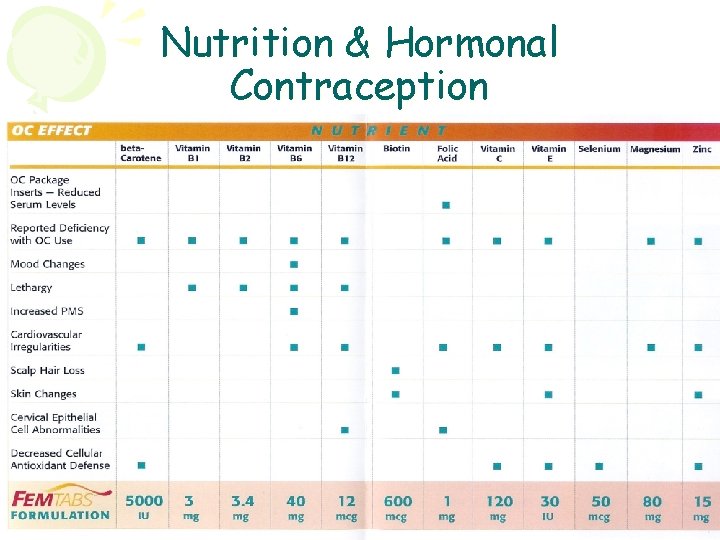
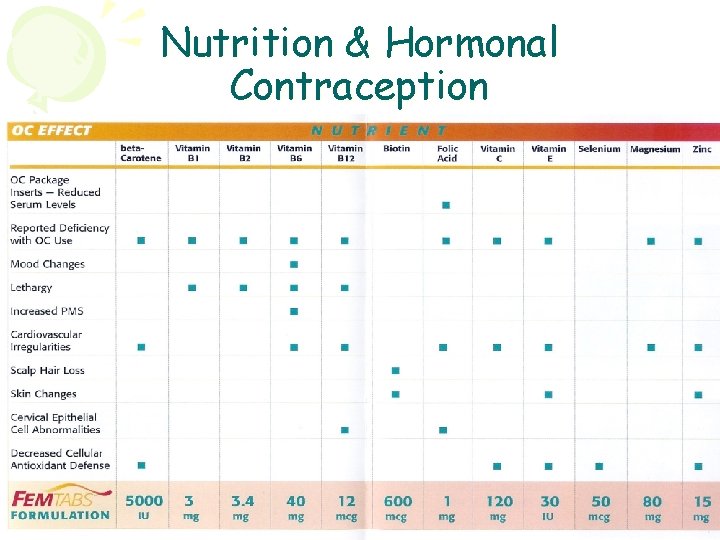
Nutrition & Hormonal Contraception
Hormonal Contraception & Cancer Ovarian Cancer • Reduces risk by 30 -50% • Even in women with genetic predisposition • Believed to be due to progestin component • Protection after 5 years of use and persists for up to 20 years Uterine Cancer • Reduces risk by 40 -50% Cervical Cancer • Unknown whether increased risk arises from true oncogenic effect or discontinued condom use and risk taking behavior (increased risk of HPV acquisition) Breast Cancer • Studies conflicting • Risk was higher with older higher dose pills • Study in 2002 no association between Ocs and breast cancer after 15 years of use
Surgical Sterilization • One of most common methods of contraception in the US (25%) • In every case should be considered permanent • Patency of fallopian tube disrupted by excision, ligation, cauterization, or occlusion by rings or clips • 10 year failure rates range from 0. 75% to 3. 65% • Male sterilization involves disruption of vas deferens • First year failure rate 0. 15%
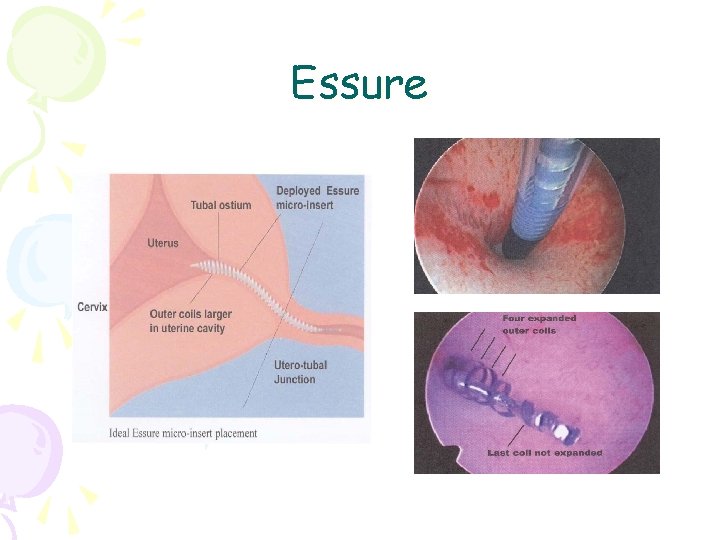
Essure Tubal Occlusion • Available in the US since 2002 • Micro-insert composed of stainless steel inner coil, nitinol elastic outer coil and PET fibers • Inserted in the proximal section of each fallopian tube under hysteroscopic guidance • Elicits an intended benign occlusive tissue response • Clinical trials 2 year failure rate 0%
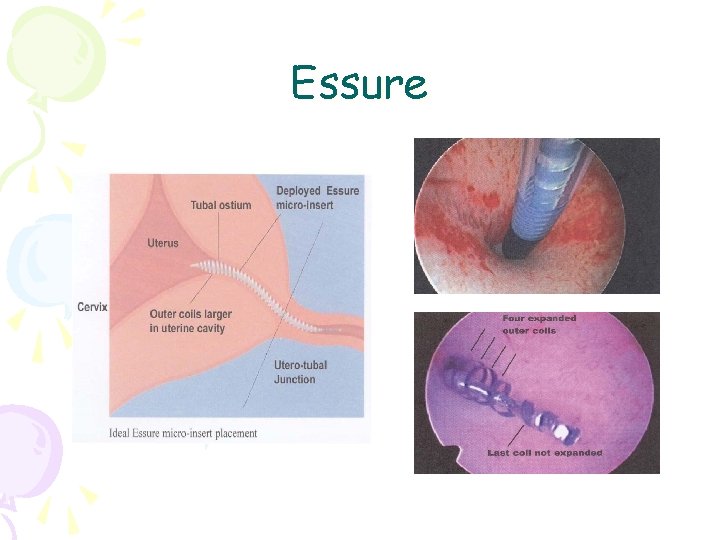
Essure
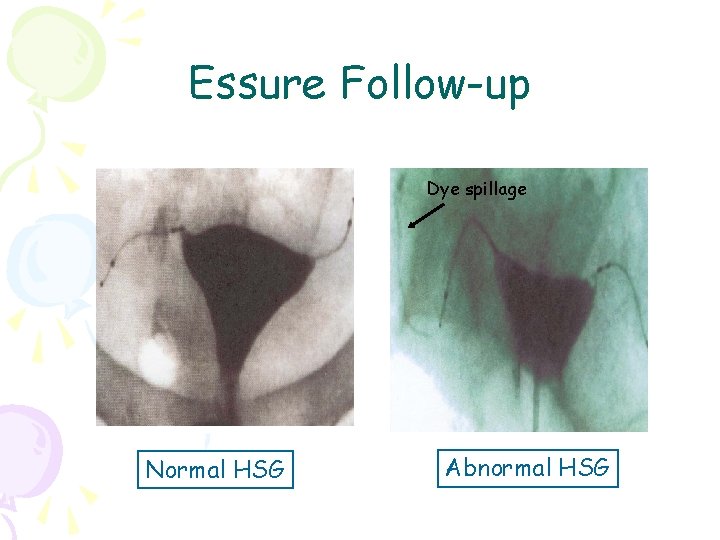
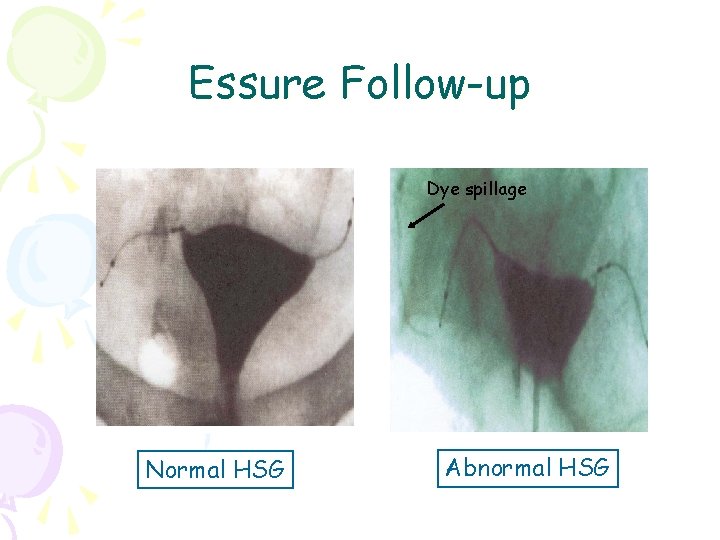
Essure Follow-up Dye spillage Normal HSG Abnormal HSG
Essure Advantages • Non-incisional • Non-hormonal • Can be performed without general anesthesia • Rapid recovery - discharged 45 minutes after and 92% returned to work the next day • Highly effective • Available to patients with not eligible for invasive sterilization
Essure Disadvantages • Chance that both micro-inserts can not be placed (14% in clinical trials) - 83% were placed on second attempt • Must rely on back-up contraception for 3 months • Removal of inserts requires surgery and may result in hysterectomy

Natural Family Planning Fertility Awareness Methods • Basal body temperature • Ovulation method • Symptothermal Success based on: • Method’s accuracy in determining fertile days • Ability to comply with method diligently • Couple’s ability to avoid intercourse on fertile days
Ovulation Method Billings Method • Monitoring cervical secretions • Avoid unprotected intercourse during preovulatory days until the 4 th day after the “peak” secretions day (last day of watery discharge)
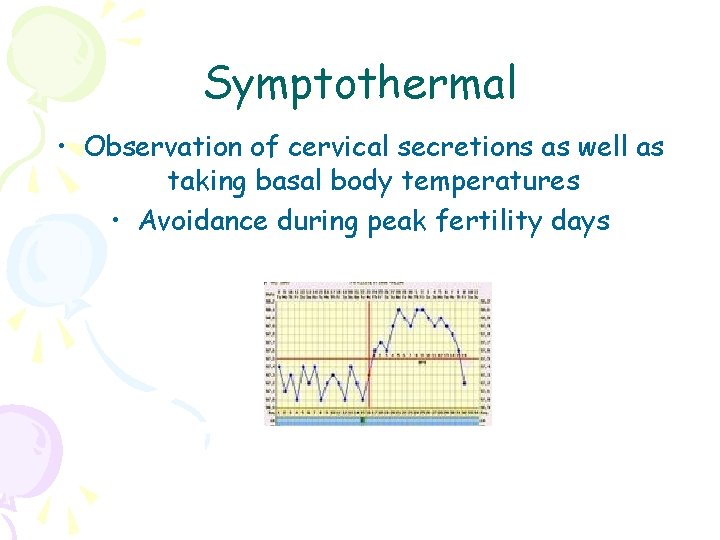
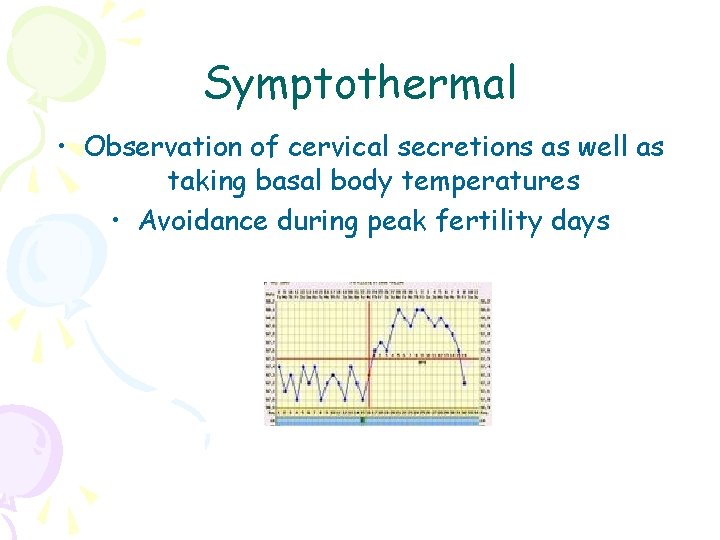
Symptothermal • Observation of cervical secretions as well as taking basal body temperatures • Avoidance during peak fertility days
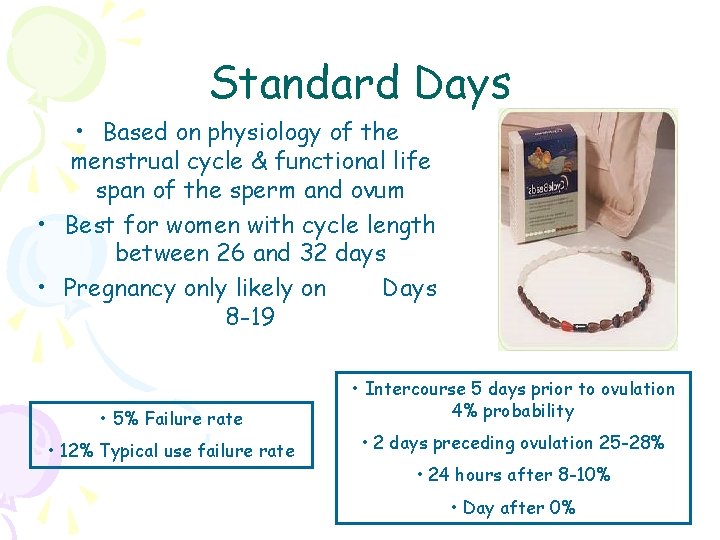
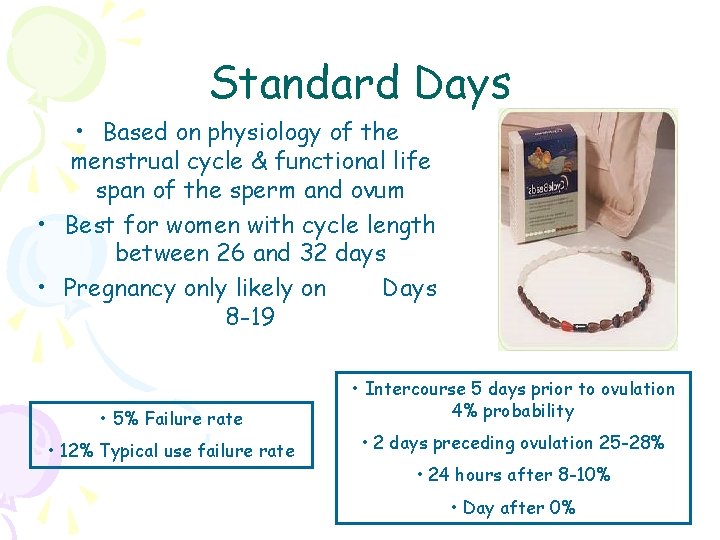
Standard Days • Based on physiology of the menstrual cycle & functional life span of the sperm and ovum • Best for women with cycle length between 26 and 32 days • Pregnancy only likely on Days 8 -19 • Intercourse 5 days prior to ovulation • 5% Failure rate • 12% Typical use failure rate 4% probability • 2 days preceding ovulation 25 -28% • 24 hours after 8 -10% • Day after 0%
 Potions menu
Potions menu Tableau comparatif contraception
Tableau comparatif contraception Victorian era birth control
Victorian era birth control Diaphragme contraception caya
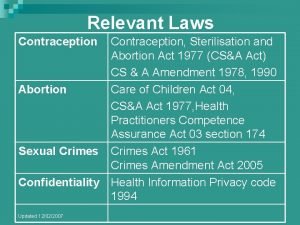
Diaphragme contraception caya Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 Cape cervicale caya
Cape cervicale caya Voluntary surgical contraception
Voluntary surgical contraception Contraception for over 40s
Contraception for over 40s Lactational amenorrhea method
Lactational amenorrhea method Pgn full form in contraception
Pgn full form in contraception Contraception
Contraception Elephant life cycle picture
Elephant life cycle picture Dr jennifer fraser
Dr jennifer fraser Jennifer bruton
Jennifer bruton Jennifer madans
Jennifer madans Jennifer belknap williamson
Jennifer belknap williamson Jennifer evans-cowley
Jennifer evans-cowley Jennifer harper-lee
Jennifer harper-lee Jennifer gress
Jennifer gress Jennifer haythornthwaite
Jennifer haythornthwaite Jennifer aquila
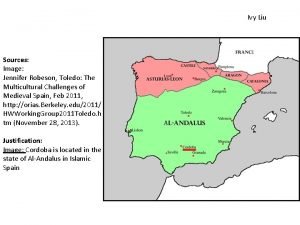
Jennifer aquila Jennifer robeson
Jennifer robeson Jennifer lindstrom md
Jennifer lindstrom md Jennifer bonham
Jennifer bonham Sherman oaks jennifer aniston
Sherman oaks jennifer aniston Jennifer madans
Jennifer madans Dogs by jennifer blizin gillis
Dogs by jennifer blizin gillis Jennifer peluso
Jennifer peluso De donde vengo proyecto de vida
De donde vengo proyecto de vida Jennifer hoban
Jennifer hoban Jennifer aniston
Jennifer aniston Anthrax history
Anthrax history Dr jennifer brennan
Dr jennifer brennan Brenton diaz
Brenton diaz Jennifer schaus and associates
Jennifer schaus and associates Jennifer belissent, ph.d.
Jennifer belissent, ph.d. Jennifer cuevas ruiz
Jennifer cuevas ruiz Jennifer pae
Jennifer pae Trauma informed legal advocacy
Trauma informed legal advocacy Dr jennifer roberts
Dr jennifer roberts Jennifer farthing
Jennifer farthing Jennifer martinez niehs
Jennifer martinez niehs M.s. 890
M.s. 890 Ralph crame
Ralph crame Jennifer reineke
Jennifer reineke Jennifer stiddard
Jennifer stiddard Jennifer obaditch
Jennifer obaditch Jennifer middleton md
Jennifer middleton md Jennifer baird md
Jennifer baird md