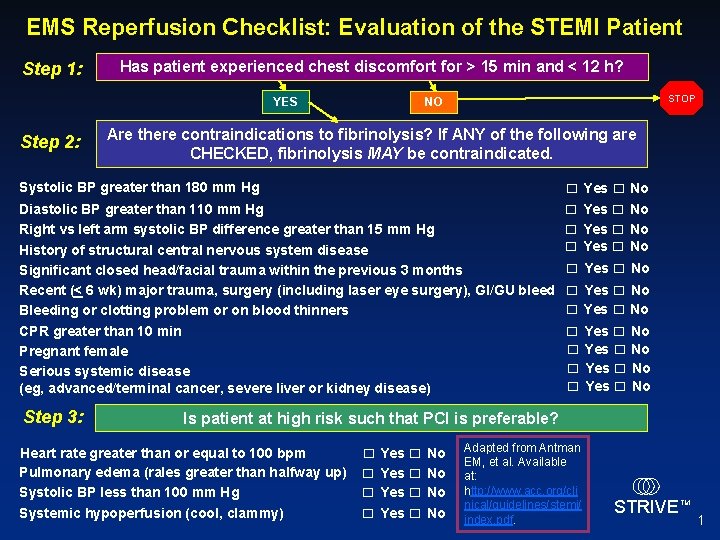
EMS Reperfusion Checklist Evaluation of the STEMI Patient

- Slides: 10
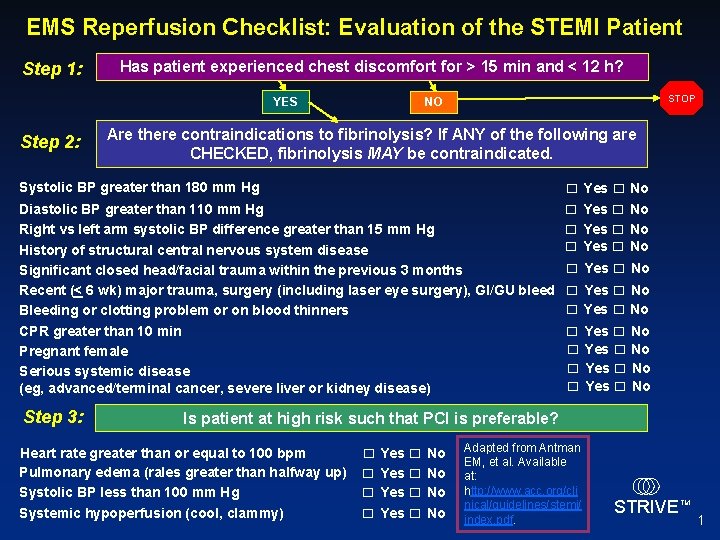
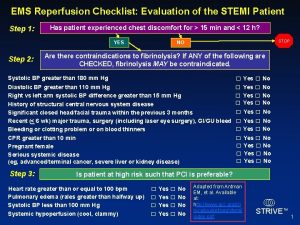
EMS Reperfusion Checklist: Evaluation of the STEMI Patient Step 1: Has patient experienced chest discomfort for > 15 min and < 12 h? YES Step 2: STOP NO Are there contraindications to fibrinolysis? If ANY of the following are CHECKED, fibrinolysis MAY be contraindicated. Systolic BP greater than 180 mm Hg Diastolic BP greater than 110 mm Hg Right vs left arm systolic BP difference greater than 15 mm Hg History of structural central nervous system disease Significant closed head/facial trauma within the previous 3 months Recent (< 6 wk) major trauma, surgery (including laser eye surgery), GI/GU bleed Bleeding or clotting problem or on blood thinners CPR greater than 10 min Pregnant female Serious systemic disease (eg, advanced/terminal cancer, severe liver or kidney disease) Step 3: □ Yes □ No □ Yes □ No □ Yes □ No Is patient at high risk such that PCI is preferable? Heart rate greater than or equal to 100 bpm Pulmonary edema (rales greater than halfway up) Systolic BP less than 100 mm Hg Systemic hypoperfusion (cool, clammy) □ Yes □ No Adapted from Antman EM, et al. Available at: http: //www. acc. org/cli nical/guidelines/stemi/ index. pdf. STRIVE TM 1
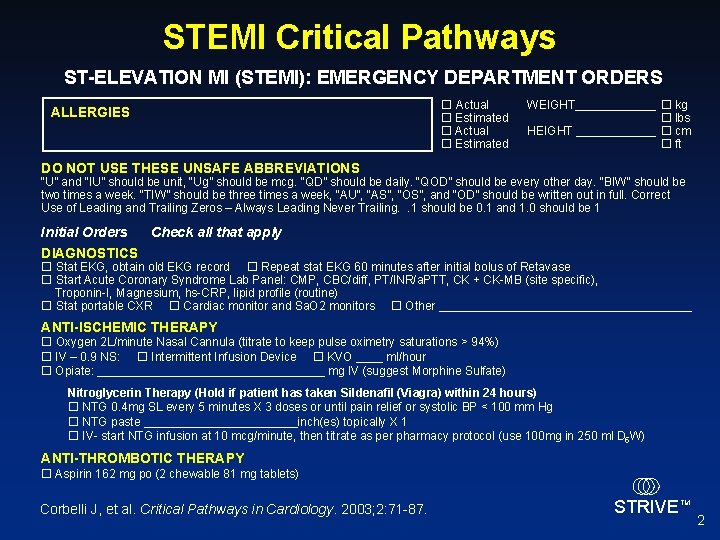
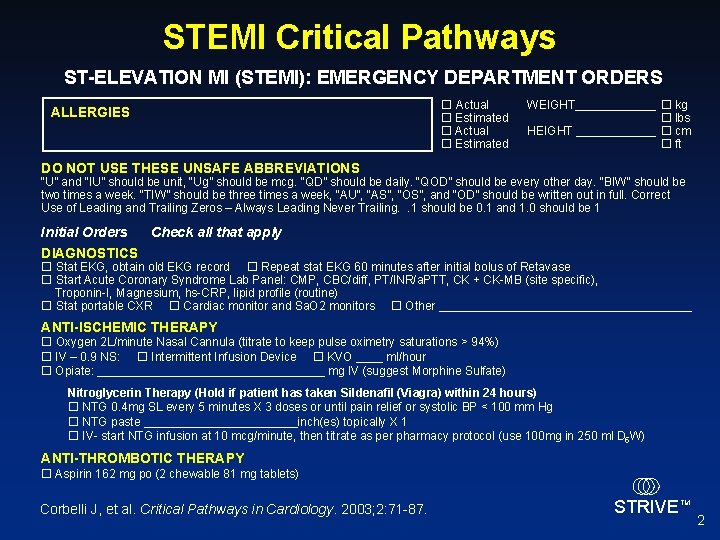
STEMI Critical Pathways ST-ELEVATION MI (STEMI): EMERGENCY DEPARTMENT ORDERS ALLERGIES Actual Estimated WEIGHT______ kg lbs HEIGHT ______ cm ft DO NOT USE THESE UNSAFE ABBREVIATIONS “U” and “IU” should be unit, “Ug” should be mcg. “QD” should be daily. “QOD” should be every other day. “BIW” should be two times a week. “TIW” should be three times a week, “AU”, “AS”, “OS”, and “OD” should be written out in full. Correct Use of Leading and Trailing Zeros – Always Leading Never Trailing. . 1 should be 0. 1 and 1. 0 should be 1 Initial Orders Check all that apply DIAGNOSTICS Stat EKG, obtain old EKG record Repeat stat EKG 60 minutes after initial bolus of Retavase Start Acute Coronary Syndrome Lab Panel: CMP, CBC/diff, PT/INR/a. PTT, CK + CK-MB (site specific), Troponin-I, Magnesium, hs-CRP, lipid profile (routine) Stat portable CXR Cardiac monitor and Sa. O 2 monitors Other ___________________ ANTI-ISCHEMIC THERAPY Oxygen 2 L/minute Nasal Cannula (titrate to keep pulse oximetry saturations > 94%) IV – 0. 9 NS: Intermittent Infusion Device KVO ____ ml/hour Opiate: _________________ mg IV (suggest Morphine Sulfate) Nitroglycerin Therapy (Hold if patient has taken Sildenafil (Viagra) within 24 hours) NTG 0. 4 mg SL every 5 minutes X 3 doses or until pain relief or systolic BP < 100 mm Hg NTG paste ____________inch(es) topically X 1 IV- start NTG infusion at 10 mcg/minute, then titrate as per pharmacy protocol (use 100 mg in 250 ml D 5 W) ANTI-THROMBOTIC THERAPY Aspirin 162 mg po (2 chewable 81 mg tablets) Corbelli J, et al. Critical Pathways in Cardiology. 2003; 2: 71 -87. STRIVE TM 2
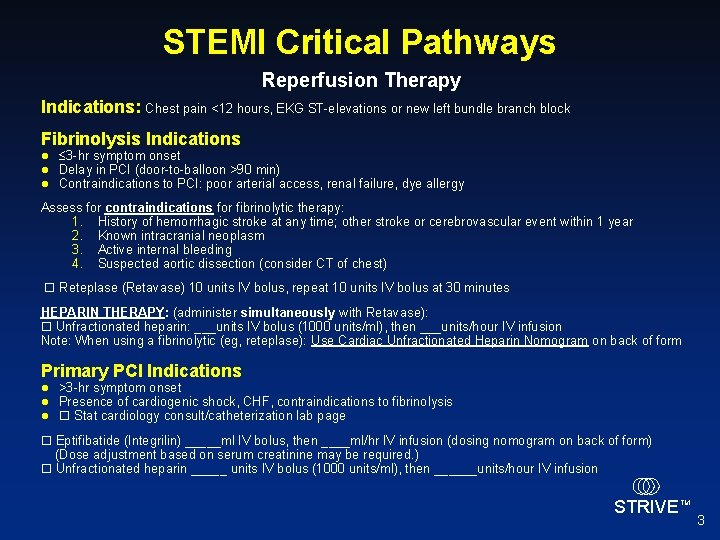
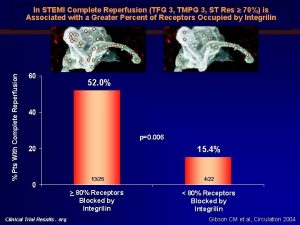
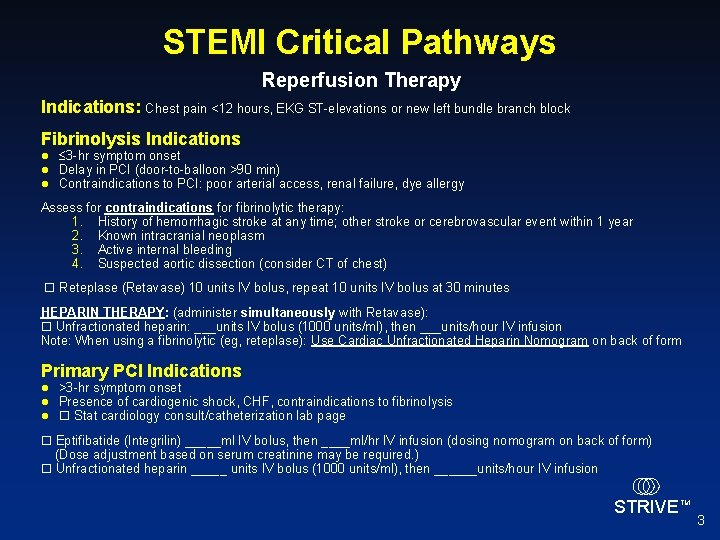
STEMI Critical Pathways Reperfusion Therapy Indications: Chest pain <12 hours, EKG ST-elevations or new left bundle branch block Fibrinolysis Indications l l l 3 -hr symptom onset Delay in PCI (door-to-balloon >90 min) Contraindications to PCI: poor arterial access, renal failure, dye allergy Assess for contraindications for fibrinolytic therapy: 1. History of hemorrhagic stroke at any time; other stroke or cerebrovascular event within 1 year 2. Known intracranial neoplasm 3. Active internal bleeding 4. Suspected aortic dissection (consider CT of chest) Reteplase (Retavase) 10 units IV bolus, repeat 10 units IV bolus at 30 minutes HEPARIN THERAPY: (administer simultaneously with Retavase): Unfractionated heparin: ___units IV bolus (1000 units/ml), then ___units/hour IV infusion Note: When using a fibrinolytic (eg, reteplase): Use Cardiac Unfractionated Heparin Nomogram on back of form Primary PCI Indications l l l >3 -hr symptom onset Presence of cardiogenic shock, CHF, contraindications to fibrinolysis Stat cardiology consult/catheterization lab page Eptifibatide (Integrilin) _____ml IV bolus, then ____ml/hr IV infusion (dosing nomogram on back of form) (Dose adjustment based on serum creatinine may be required. ) Unfractionated heparin _____ units IV bolus (1000 units/ml), then ______units/hour IV infusion STRIVE TM 3
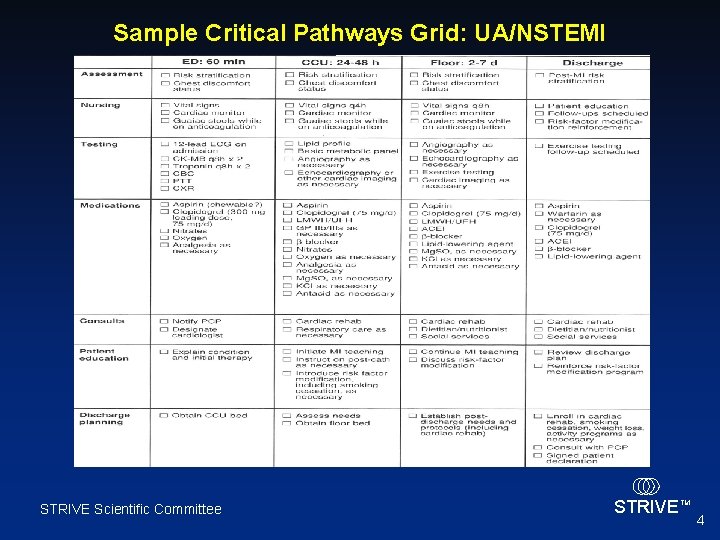
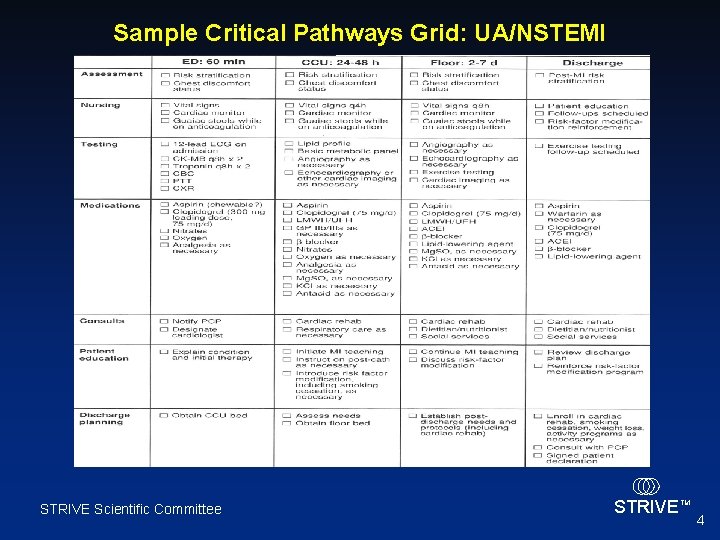
Sample Critical Pathways Grid: UA/NSTEMI STRIVE Scientific Committee STRIVE TM 4
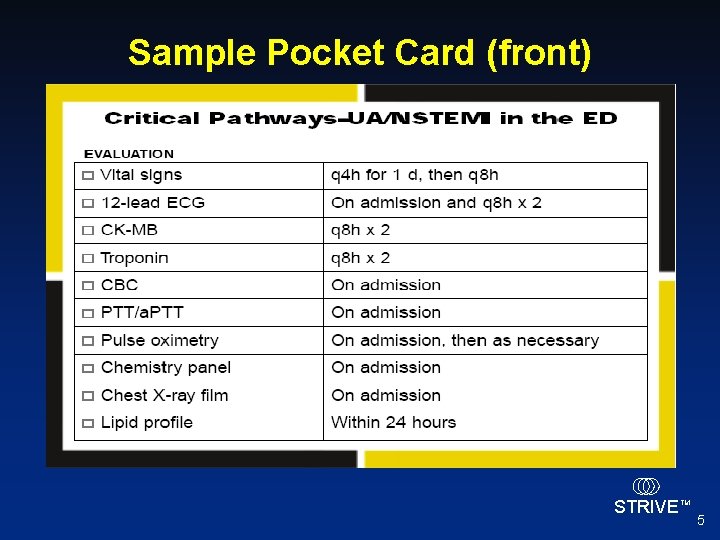
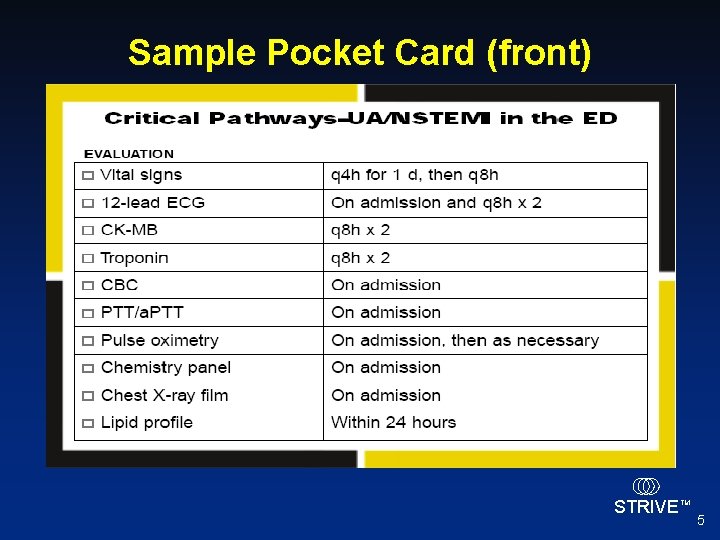
Sample Pocket Card (front) STRIVE TM 5
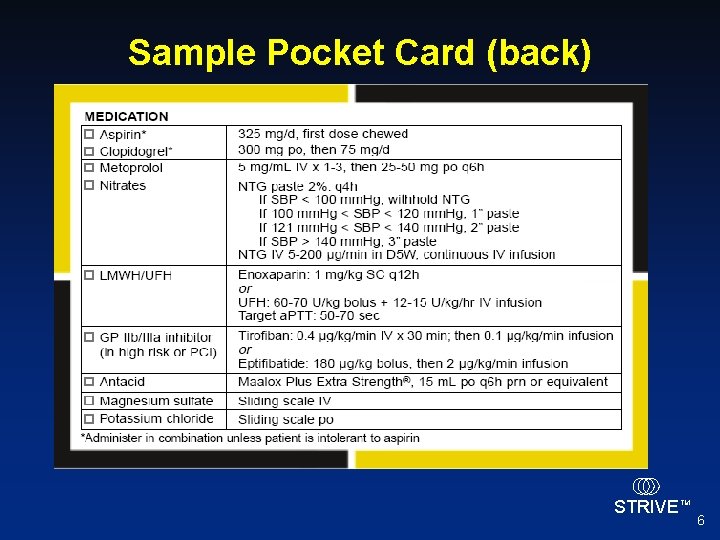
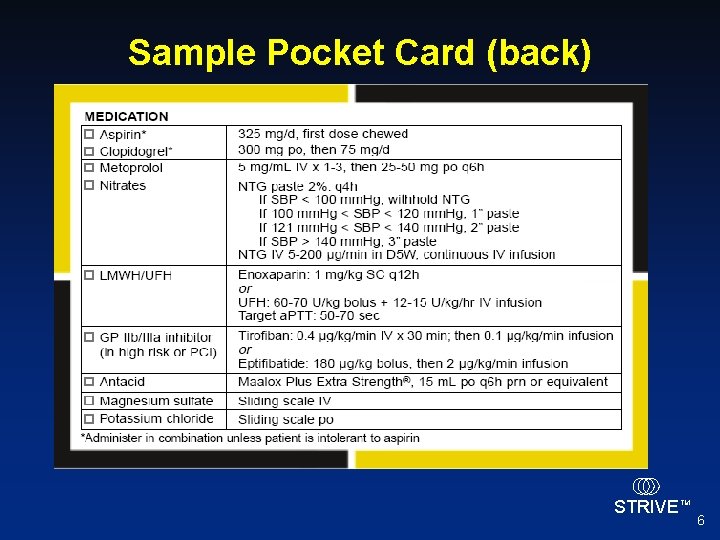
Sample Pocket Card (back) STRIVE TM 6
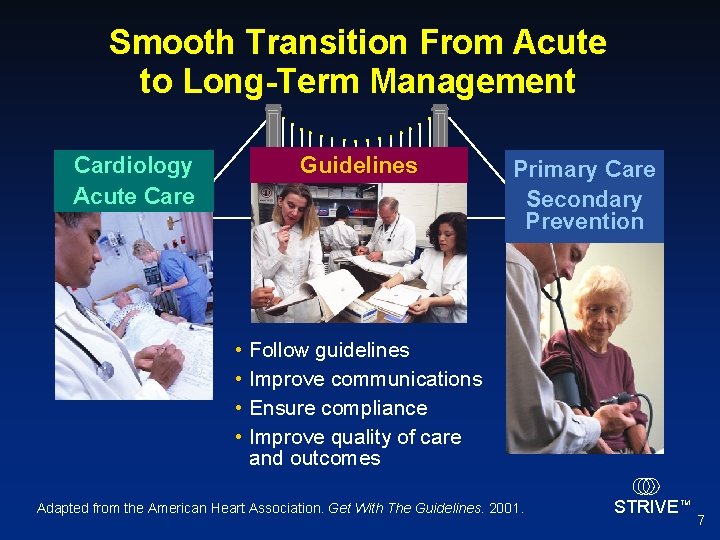
Smooth Transition From Acute to Long-Term Management Cardiology Acute Care Guidelines • • Primary Care Secondary Prevention Follow guidelines Improve communications Ensure compliance Improve quality of care and outcomes Adapted from the American Heart Association. Get With The Guidelines. 2001. STRIVE TM 7

Discharge Protocols l Enhance communication with patient and between specialist(s) and primary care physicians 1 l Medications: aspirin, clopidogrel, ACE inhibitor, β-blocker, statin 1 l Diet, exercise, smoking cessation recommendations 1 l Patient symptom awareness, “Act in Time” protocol 2 l Wallet-/purse-sized copy of ECG 3 l Follow-up appointments 1 1. American Heart Association Web site. Get With The Guidelines. Available at: http: //www. americanheart. org/presenter. jhtml? identifier=1165. 2. Act in Time to Heart Attack Signs Campaign. Available at: http: //www. nhlbi. nih. gov/actintime/index. htm. 3. Greenberg DI, et al. J Cardiovasc Manag. 2004; 15: 16 -18. STRIVE TM 8
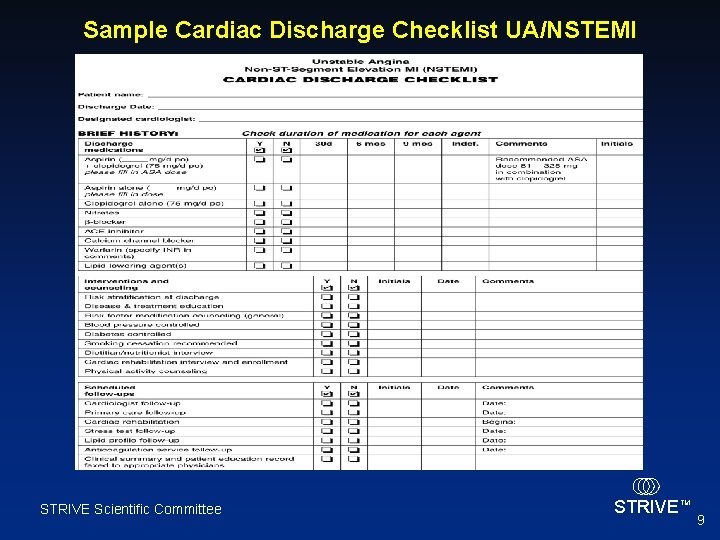
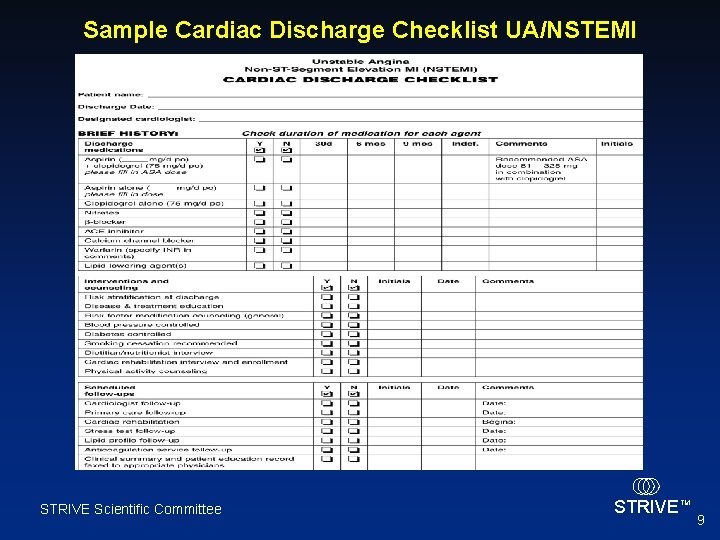
Sample Cardiac Discharge Checklist UA/NSTEMI STRIVE Scientific Committee STRIVE TM 9
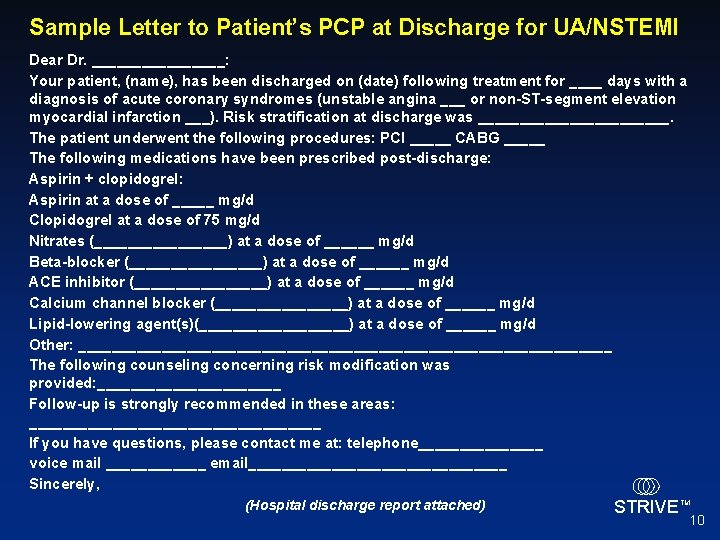
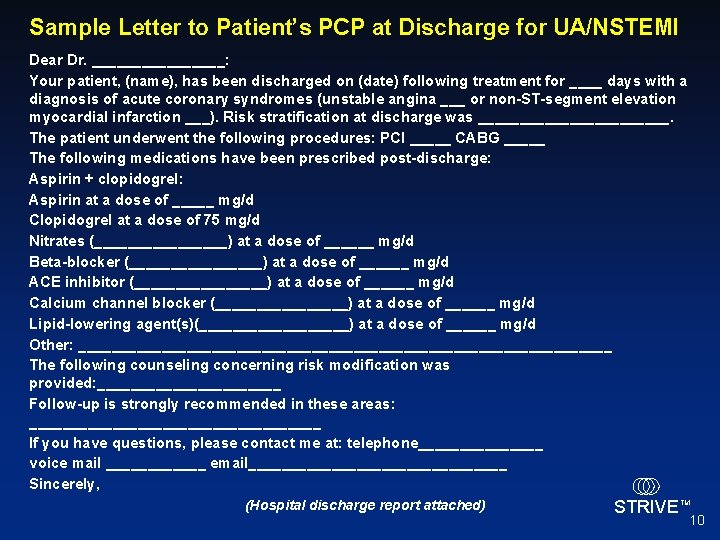
Sample Letter to Patient’s PCP at Discharge for UA/NSTEMI Dear Dr. ________: Your patient, (name), has been discharged on (date) following treatment for ____ days with a diagnosis of acute coronary syndromes (unstable angina ___ or non-ST-segment elevation myocardial infarction ___). Risk stratification at discharge was ____________. The patient underwent the following procedures: PCI _____ CABG _____ The following medications have been prescribed post-discharge: Aspirin + clopidogrel: Aspirin at a dose of _____ mg/d Clopidogrel at a dose of 75 mg/d Nitrates (________) at a dose of ______ mg/d Beta-blocker (________) at a dose of ______ mg/d ACE inhibitor (________) at a dose of ______ mg/d Calcium channel blocker (________) at a dose of ______ mg/d Lipid-lowering agent(s)(_________) at a dose of ______ mg/d Other: ________________________________ The following counseling concerning risk modification was provided: ___________ Follow-up is strongly recommended in these areas: __________________ If you have questions, please contact me at: telephone________ voice mail ______ email________________ Sincerely, (Hospital discharge report attached) STRIVE TM 10