Effects of different NUC on the development of

















- Slides: 17

Effects of different NUC on the development of HCC and liver-related outcomes: Entecavir vs Tenofovir

Major Risk Factors for HCC Chan SL et al. J Clin Oncol. 2016

Antiviral therapy reduces but dose not eliminate HCC Liaw et al. N Engl J Med. 2004; 351: 1521 Wong GL et al. Hepatology 2013; 58: 1537

The risk of HCC declined after 5 year of treatment with ETV or TDF in cirrhotic pts, but… 1951 Caucasian Patients, previously Tx-naïve or experienced N=1379 N=526 (27%) Older age (especially ≥ 50 years), lower platelets, and liver stiffness ≥ 12 k. Pa at year 5 : the main risk factors for late HCC development (PAGE-B score) Papatheodoridis et al. Hepatology 2017; 66: 5

HCC Development after the First 5 Years of Treatment N=658 N=206 N=66 • Cirrhosis is the key predictor- even if liver stiffness improves by antiviral treatment, HCC still occurs Papatheodoridis et al. 2018 The Liver Meeting abstract

REALM: Global Prospective Observational Study up to 10 Years from Asia, USA, Germany, Russian Cirrhosis 20% lamivudine or telbivudine Hou J et al. 2017 The Liver Meeting abstract

REALM: Global Prospective Observational Study up to 10 Years N. S Hou J et al. 2017 The Liver Meeting abstract

REALM-SON: Virologic Response and Risk of Outcome Events China subgroup analysis from REALM study (ETV 2, 667 vs other NUC 2, 665) Hou J et al. 2017 The Liver Meeting abstract

Data from Hong Kong Electronic DB 2008 -2018 Tx-naïve G. Wong et al. 2019 ILCA

Data from Hong Kong Electronic DB G. Wong et al. 2019 ILCA

Data from Hong Kong Electronic DB G. Wong et al. 2019 ILCA

Results : primary outcome (HCC development) G. Wong et al. 2019 ILCA

Data from Another Korean Cohort (1) CHB + compensated cirrhosis N=2897, 240 HCC 5 yr risk of HCC (ETV vs TDF): 8. 7% vs 7. 9% Compensated cirrhosis (31%) N=760, 174 HCC 5 yr risk of HCC: 20. 9% vs 16. 0% Kim SU et al. J Hepatol. 2019 Epub

Data from Another Korean Cohort (2) Lee SW et al. 2019 ILCA abstract

Data from Another Korean Cohort (2) Cumulative incidences of HCC Lee SW et al. 2019 ILCA abstract

Data from Another Korean Cohort (2) Cumulative incidences of LT or liver-related death HR 0. 38 (95% CI 0. 17 -0. 83, P=0. 02) n. s Lee SW et al. 2019 ILCA abstract

Different Population, Different Results 아산 공단검진자료 연고대, 분당차, 경북 대 가톨릭대 홍콩 Tx initiation, year 2010 -2016 2012 -2014 2007 -2018 2008 -2018 ETV: TDF, naïve 1560: 1141 11464: 12692 1484: 1413 1741: 1541 (experienced: 349: 383) 28041: 1309 (female, younger) Exclusion 1년이내 HCC, 6개 월이내 LT/death 6개월이내 HCC/LT/death LC 935: 653 (약 60%) 2991 vs 3488 (약 27%, decom 3. 5%) 499: 411(com. LC only, 약 31%) NA (약 1/3) 3650: 35 (12. 6% vs 2. 7%) PS-matched LC 511: 505 2891: 2919 380: 380 NA 1120: 35 HCC risk in LC 3. 62 vs 2. 12 (/100 patients-years) HR 0. 65 (p=0. 02) 2. 76 vs 2. 08 (/100 patients-years) HR 0. 67 (p<0. 001) 5 yr: 20. 9% vs 16. 0% HR 0. 854 (p=0. 356) NA HR 0. 32 (0. 11 -0. 97) p=0. 044 HCC risk in all naïve pt 2. 17 vs 1. 37 (/100 patients-years) HR 0. 68 (p=0. 04) 1. 20 vs 0. 92 (/100 patients-years) HR 0. 68 (p<0. 001) 5 yr: 8. 7% vs 7. 9% HR 1. 021 (p=0. 884) 5 yr: 6. 058 vs 6. 476 HR 0. 993 (p=0. 96) 5 yr: 3. 1% vs 1. 2% HR 0. 36 (0. 16 -0. 80) p=0. 013 LT or death risk in LC 1. 66 vs 1. 35 (/100 patients-years) HR 0. 87 (p=0. 65) 1. 08 vs 0. 91 (/100 patients-years) HR 0. 86 (p=0. 25) 5 yr: 3. 4% vs 5. 4% HR 1. 917 (p=0. 08) NA NA LT or death risk in all naïve pt 1. 17 vs 0. 87 (/100 patients-years) HR 0. 80 (p=0. 44) 0. 53 vs 0. 46 (/100 patients-years) HR 0. 91 (p=0. 35) 5 yr: 2. 2% vs 2. 6% HR 1. 248 (p=0. 385) 5 yr: 1. 307 vs 0. 643 HR 0. 534 (p=0. 16) (liver-related death) NA Reimbursement: ETV 2007. 1월, TDF 2012. 12월
 Diencephalonun bölümleri
Diencephalonun bölümleri Nucleus accessorius nervi oculomotorii
Nucleus accessorius nervi oculomotorii Perbedaan nuc dan ncc
Perbedaan nuc dan ncc Fissura prima cerebellum
Fissura prima cerebellum Colliculus facialis
Colliculus facialis Sulcus pontocruralis nedir
Sulcus pontocruralis nedir Nuc grading system 2020
Nuc grading system 2020 Piramidal traktus bulguları
Piramidal traktus bulguları Mesencephalon kesiti
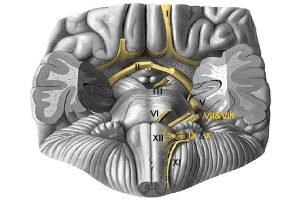
Mesencephalon kesiti Ventral view of brainstem
Ventral view of brainstem Gl parotidea parasempatik innervasyonu
Gl parotidea parasempatik innervasyonu Nuc ruber
Nuc ruber Nuc gracilis
Nuc gracilis Positive effects of primate cities on economic development
Positive effects of primate cities on economic development Why do different polymers have different properties?
Why do different polymers have different properties? Technicolor test
Technicolor test Sound will travel at different speeds in different mediums.
Sound will travel at different speeds in different mediums. Lrefraction
Lrefraction