Eating Disorders Dr Jackie Hoare Liaison Psychiatry GSH
- Slides: 26
Eating Disorders Dr Jackie Hoare Liaison Psychiatry GSH
Anorexia nervosa (AN) �is an illness characterised by extreme concern about body weight �with serious disturbances in eating behavior �leading to a self-imposed starvation state �Severe weight loss. �Body image becomes the predominant measure of self -worth �denial of the seriousness of the illness.
International Classification of Diseases, revision 10 (ICD-10) (WHO 1992), �(a) refusal to maintain weight within the normal range for height and age � (b) fear of weight gain; �(c) body image disturbance �(d) absence of menstrual cycles or �amenorrhea in women (and loss of sexual interest in men).
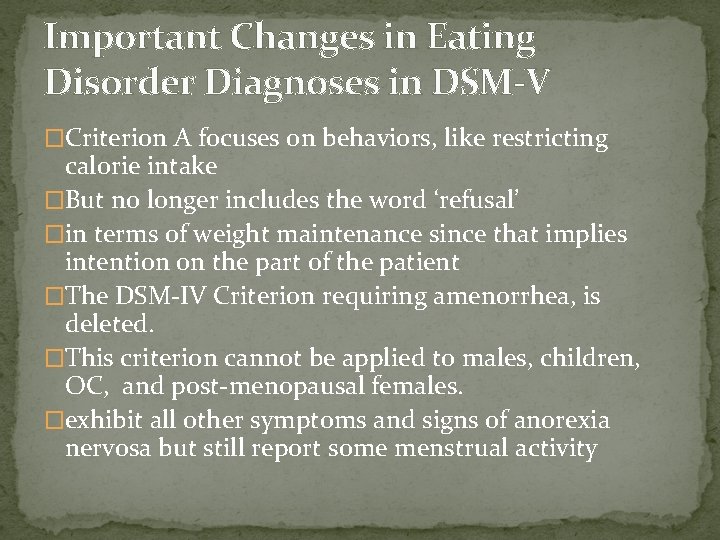
Important Changes in Eating Disorder Diagnoses in DSM-V �Criterion A focuses on behaviors, like restricting calorie intake �But no longer includes the word ‘refusal’ �in terms of weight maintenance since that implies intention on the part of the patient �The DSM-IV Criterion requiring amenorrhea, is deleted. �This criterion cannot be applied to males, children, OC, and post-menopausal females. �exhibit all other symptoms and signs of anorexia nervosa but still report some menstrual activity
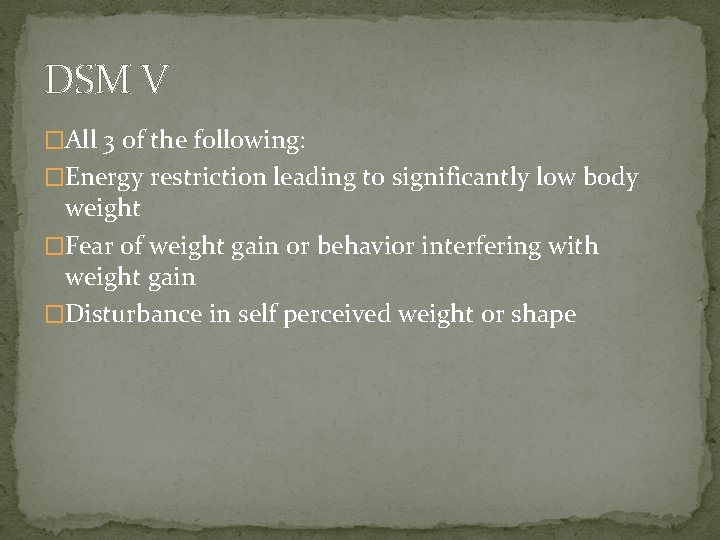
DSM V �All 3 of the following: �Energy restriction leading to significantly low body weight �Fear of weight gain or behavior interfering with weight gain �Disturbance in self perceived weight or shape
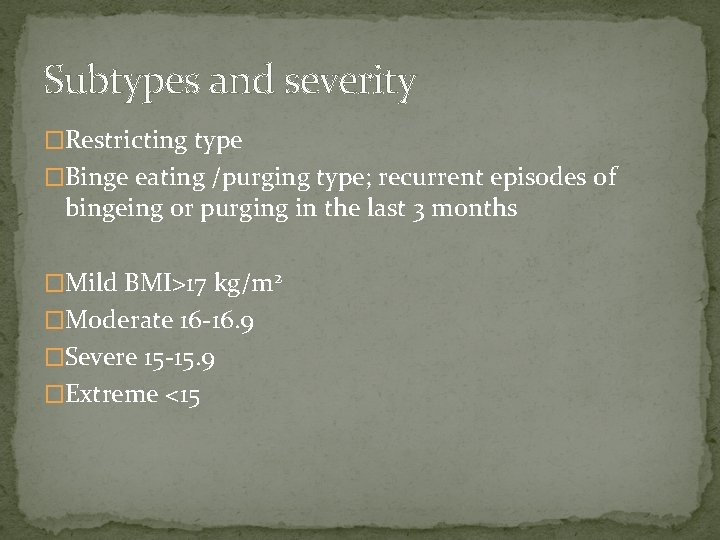
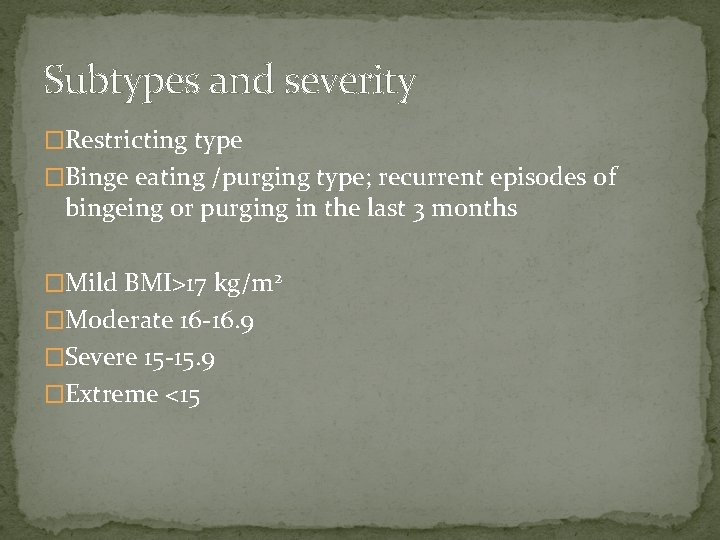
Subtypes and severity �Restricting type �Binge eating /purging type; recurrent episodes of bingeing or purging in the last 3 months �Mild BMI>17 kg/m 2 �Moderate 16 -16. 9 �Severe 15 -15. 9 �Extreme <15
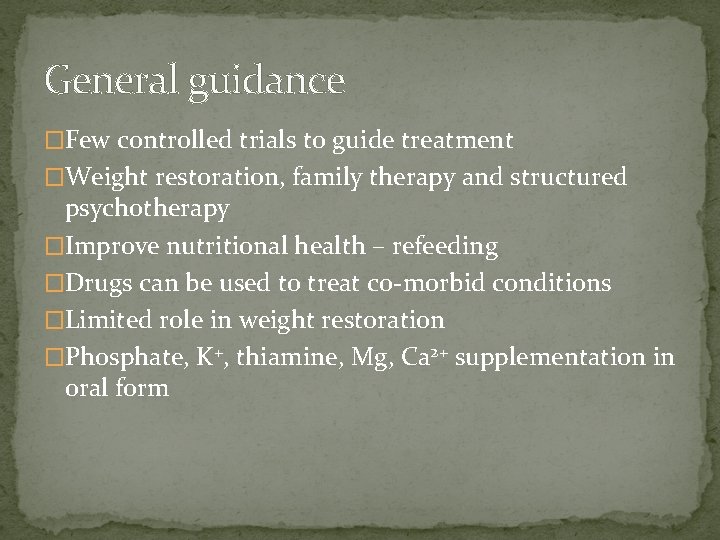
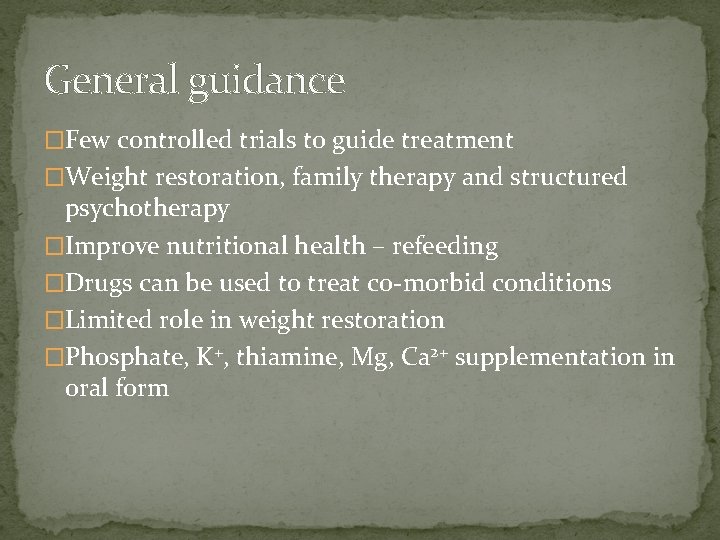
General guidance �Few controlled trials to guide treatment �Weight restoration, family therapy and structured psychotherapy �Improve nutritional health – refeeding �Drugs can be used to treat co-morbid conditions �Limited role in weight restoration �Phosphate, K+, thiamine, Mg, Ca 2+ supplementation in oral form
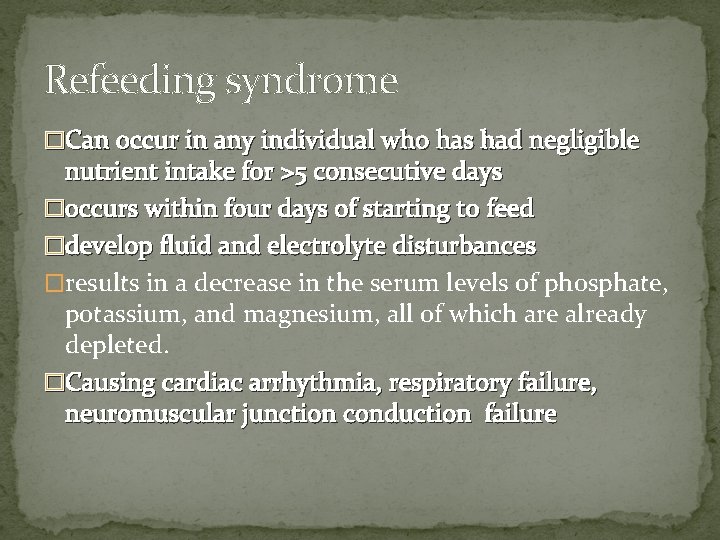
Refeeding syndrome �Can occur in any individual who has had negligible nutrient intake for >5 consecutive days �occurs within four days of starting to feed �develop fluid and electrolyte disturbances �results in a decrease in the serum levels of phosphate, potassium, and magnesium, all of which are already depleted. �Causing cardiac arrhythmia, respiratory failure, neuromuscular junction conduction failure
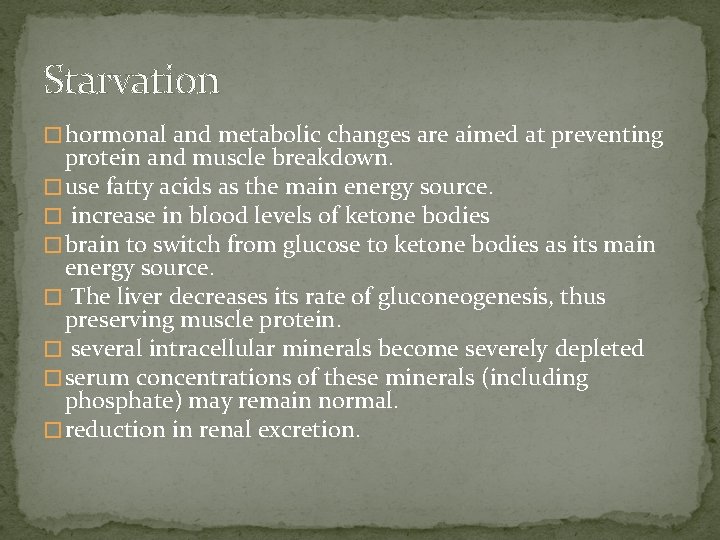
Starvation � hormonal and metabolic changes are aimed at preventing protein and muscle breakdown. � use fatty acids as the main energy source. � increase in blood levels of ketone bodies � brain to switch from glucose to ketone bodies as its main energy source. � The liver decreases its rate of gluconeogenesis, thus preserving muscle protein. � several intracellular minerals become severely depleted � serum concentrations of these minerals (including phosphate) may remain normal. � reduction in renal excretion.
Refeeding � During refeeding, glycaemia leads to increased insulin and decreased secretion of glucagon. � Insulin stimulates glycogen, fat, and protein synthesis. � Insulin stimulates the absorption of potassium into the cells through the sodium-potassium ATPase symporter, which also transports glucose into the cells. � Magnesium and phosphate are also taken up into the cells. � Water follows by osmosis. � These processes result in a decrease in the serum levels of phosphate, potassium, and magnesium � The clinical features of the refeeding syndrome occur as a result of the functional deficits of these electrolytes and the rapid change in basal metabolic rate.
Treatment � Refeeding syndrome can be fatal if not recognized and treated properly. � An awareness of the condition and a high index of suspicion are required in order to make the diagnosis. � The electrolyte disturbances can occur within the first few days � Close monitoring of blood biochemistry is therefore necessary in the early refeeding period. � rate of feeding should be slowed down and essential electrolytes should be replenished. � Fluid repletion should be carefully controlled to avoid fluid overload
Osteoporosis �Bone loss complication serious consequences �Hormonal treatment with oestrogen or dehydroepiandrosterone (DHEA) no positive effect on bone density �Oestrogen not recommended in children and adolescents – risk premature fusion of bones
Acute illness: antidepressants � 2009 Cochrane review: no evidence from 4 placebo controlled trials �On weight gain, eating disorder or associated psychopathology �Suggested neurochemical abnormalities in starvation may explain non-response �Co-prescribing supplementation incl. tryptophan with fluoxetine does not increase efficacy
Other psychotropic drugs �Olanzapine, benzodiazepines or promethazine to reduce anxiety with refeeding � 1 RCT showed 88% of patients given olanzapine achieved weight restoration (55% placebo) �Quetiapine may improve psychological symptoms but few data
Relapse prevention and co-morbid disorders �Small trial suggested that fluoxetine useful in improving outcome and preventing relapse after weight restoration �Other studies found no benefit �Antidepressants often used to treat co-morbid depression and OCD �However these conditions may resolve with weight gain alone
Avoidant/restrictive food intake disorder �Significant disturbance in eating manifested by persistent failure to meet nutritional/energy requirement associated with 1 of: �Significant weight loss �Significant nutritional deficiency �Dependence on enteral feeding or supplements �Interference with psychosocial functioning �NOT due to lack of food or body image disturbance
Clinically Significant Restrictive Eating Problems Are Key � Avoidant/Restrictive Food Intake Disorder (ARFID) has replaced Feeding Disorder of Infancy and Early Childhood and EDNOS which was described in the DSM-IV. � While few data on ARFID have been published, it appears that it usually presents in infancy or childhood, but it can also present or persist into adulthood. � The course of illness for individuals relatively unknown. � Avoidance due to sensory characteristics of food, emotional difficulties, food beliefs etc. � ARFID may be associated with impaired social functioning and affect family functioning, especially if there is great stress surrounding mealtimes.
Distinguishing ARFID from Other Disorders � The presence of other psychological disorders may be risk factors for ARFID, such as anxiety disorders, obsessivecompulsive disorders, attention deficit disorders, and autism spectrum disorders � If an individual presents with one of these illnesses and an eating problem, a diagnosis of ARFID should be given only when the feeding disturbance itself is causing significant clinical impairment � individuals with a history of gastrointestinal conditions such as gastroesophageal reflux may develop feeding disturbances, but a diagnosis of ARFID should be assigned only when the feeding disturbances require significant treatment beyond that needed for the gastrointestinal problems.
Treating ARFID �Little is currently known about effective treatment interventions for individuals presenting with ARFID � given the prominent avoidance behaviors, it seems likely that behavioral interventions, such as forms of exposure therapy � depression or anxiety that affects feeding, cognitive behavioral therapy and other treatments for the underlying condition
Bulimia nervosa �Bulimia nervosa is characterized by recurrent and frequent episodes of eating unusually large amounts of food � feeling a lack of control over the eating. �purging (e. g. , vomiting, excessive use of laxatives or diuretics), fasting and/or excessive exercise � DSM-5 criteria reduce the frequency of binge eating and compensatory behaviors to once a week from twice weekly as specified in DSM-IV.
BN treatment � Psychological treatments first choice � Adults mat be offered antidepressants � SSRI’s esp fluoxetine � 60 mg effective dose � Can reduce frequency of binge eating and purging � Long term effects unknown � Early response at 3 weeks strong indicator of response overall � Used off licensed in adolescents � Some evidence for topiramate, duloxetine, lamotrigine and sertraline reduce binges
Binge eating disorder � Binge eating disorder will now have its own category as an eating disorder. � In the DSM-IV, under the category Eating Disorder Not Otherwise Specified � “recurring episodes of eating significantly more food in a short period of time than most people would eat under similar circumstances, with episodes accompanied by feelings of lack of control. ” � eat quickly and uncontrollably, despite hunger signals or feelings of fullness. � feelings of guilt, shame, or disgust � behavior will have typically taken place at least once a week over a period of three months.
BED treatment �NICE recommends �Evidenced based self help programme of CBT as first line �Trial of SSRI as an alternative or additional first step
�Although AN is not a common condition �its morbidity and mortality are amongst the highest psychiatric disorders �due to malnutrition, purging �behavior and suicide. � 18 -fold increase in mortality in patients with AN
Diagnostic Crossover in Anorexia Nervosa and Bulimia Nervosa: Implications for DSM-V Kamryn T. Eddy, �Over 7 years, the majority of women with anorexia nervosa experienced diagnostic crossover: more than half crossed between the restricting and binge eating/purging anorexia nervosa subtypes over time; one-third crossed over to bulimia nervosa but were likely to relapse into anorexia nervosa. Women with bulimia nervosa were unlikely to cross over to anorexia nervosa
Conclusion �Key is MDT �Dietician, psychology, medicine, psychiatry, OT and social worker �Clearly defined case manager , roles of team members in case defined
 Kate moss anorexia
Kate moss anorexia Chimps eating termites
Chimps eating termites How to be anorexic
How to be anorexic York eating disorders service
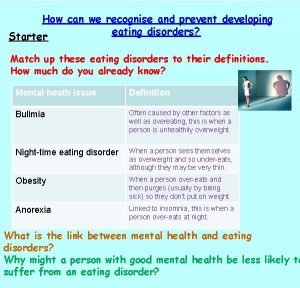
York eating disorders service Chapter 11 lesson 2 body image and eating disorders
Chapter 11 lesson 2 body image and eating disorders Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Hypothalamus and eating disorders
Hypothalamus and eating disorders Eating disorders in uae
Eating disorders in uae Marzipan criteria
Marzipan criteria How to spot eating disorders
How to spot eating disorders Sarah fogarty
Sarah fogarty Psychodynamic explanation of anorexia
Psychodynamic explanation of anorexia Rachel hoare tcd
Rachel hoare tcd Abyssinian crisis map
Abyssinian crisis map Mesa vs hoare semantics
Mesa vs hoare semantics Logique de hoare
Logique de hoare Stott hoare byod
Stott hoare byod Car hoare
Car hoare National network of child psychiatry access programs
National network of child psychiatry access programs National network of child psychiatry access programs
National network of child psychiatry access programs Mse psychiatry
Mse psychiatry Jamaica hospital psychiatry residency
Jamaica hospital psychiatry residency Mood mse
Mood mse Asclepiades father of psychiatry
Asclepiades father of psychiatry Psychiatry shelf exam percentiles
Psychiatry shelf exam percentiles Criminal psychology means
Criminal psychology means Community geriatric psychiatry
Community geriatric psychiatry