Dr P S M AMEER ALI M S

- Slides: 34
Dr. P. S. M AMEER ALI M. S PROFESSOR OF SURGERY Y. M. C. H
� Three main categories -injuries & emergencies -infections -tumors
PART 1
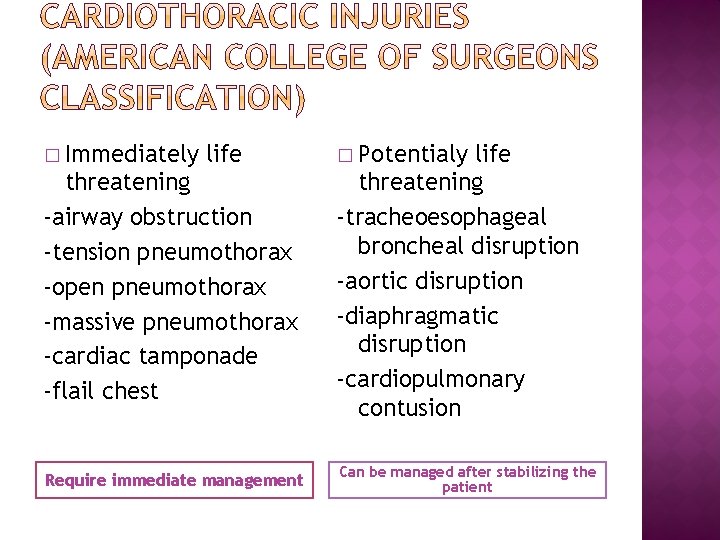
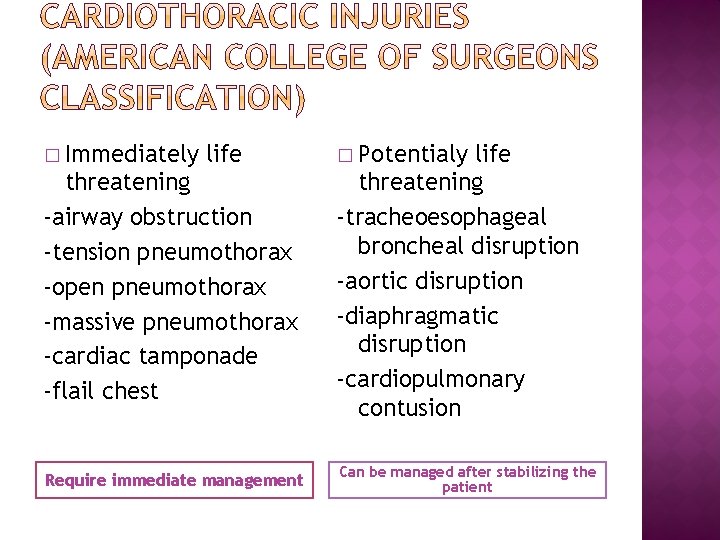
� Immediately life � Potentialy threatening -airway obstruction -tension pneumothorax -open pneumothorax -massive pneumothorax -cardiac tamponade -flail chest life threatening -tracheoesophageal broncheal disruption -aortic disruption -diaphragmatic disruption -cardiopulmonary contusion Require immediate management Can be managed after stabilizing the patient
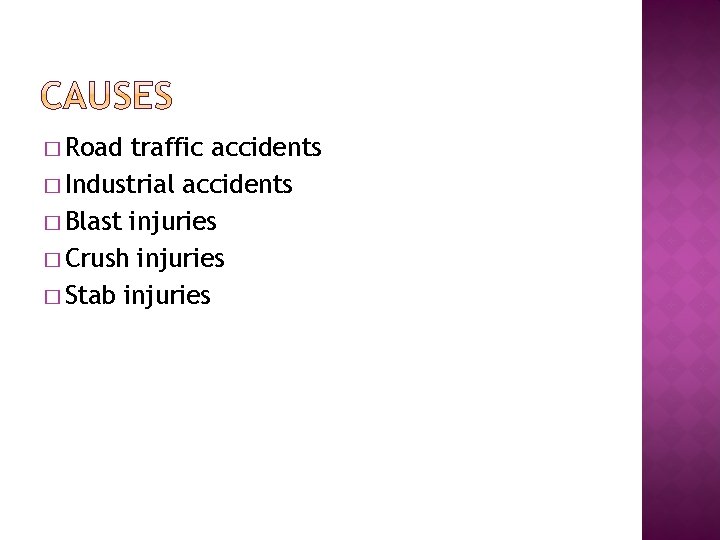
� Road traffic accidents � Industrial accidents � Blast injuries � Crush injuries � Stab injuries
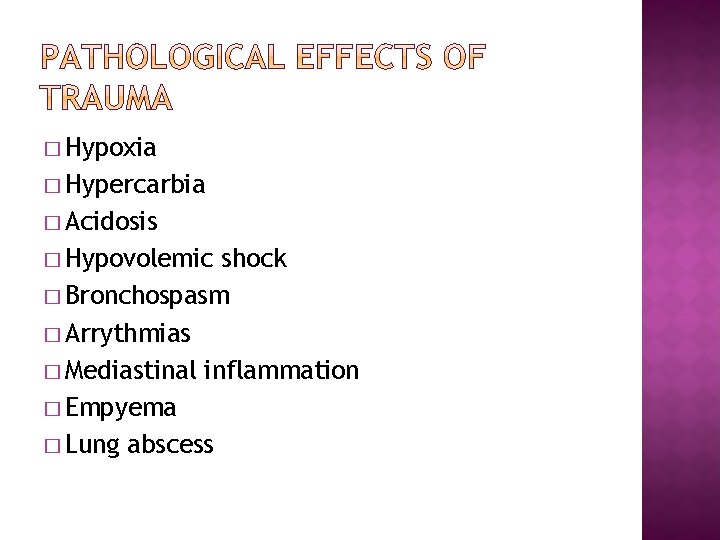
� Hypoxia � Hypercarbia � Acidosis � Hypovolemic shock � Bronchospasm � Arrythmias � Mediastinal inflammation � Empyema � Lung abscess
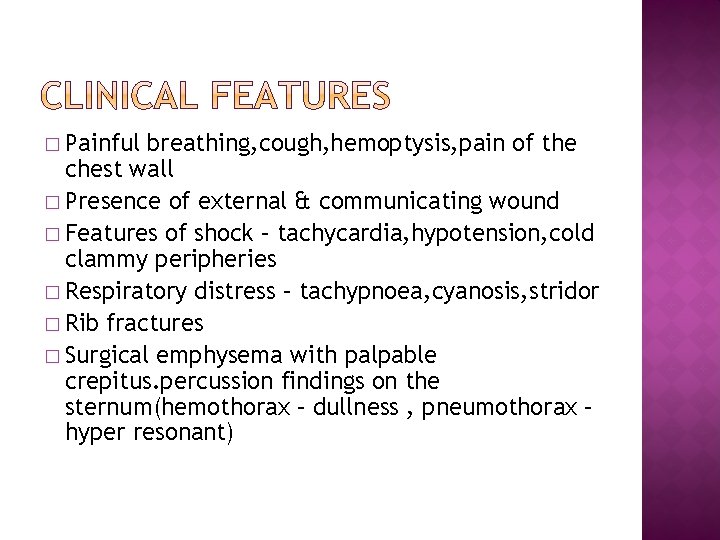
� Painful breathing, cough, hemoptysis, pain of the chest wall � Presence of external & communicating wound � Features of shock – tachycardia, hypotension, cold clammy peripheries � Respiratory distress – tachypnoea, cyanosis, stridor � Rib fractures � Surgical emphysema with palpable crepitus. percussion findings on the sternum(hemothorax – dullness , pneumothorax – hyper resonant)
� Chest x-ray(pneumothorax, hemothorax, rib and sternal fractures) � Complete blood count � Blood grouping and typing � Arterial blood gases (ABG) � Emergency ultrasound (FAST – focused abdominal sonography on trauma) � Emergency CT(thoracic, aortopulmonary, cardiac, diaphragmatic injuries)
� Principles of management : 1. Pulmonary physiotherapy 2. Aspiration of secretions 3. Pain relief 4. Respiratory support 5. Management of shock 6. Diagnosis of underlying pathology 7. Surgery when indicated 8. Management of complications
� Airway – prevention of aspiration, intubation, tracheostomy � Breathing – ICT placement, supportive measures � Circulation – fluid therapy, CVP monitoring � Thorough clinical assessment of patient � Look for other injuries(abdominal injuries, head injury, fractures, spine trauma)
� Uncomplicated rib fractures are treated with rest and analgesics � Hemo or pneumothorax should be taken care of by intercostal tube drainage with waterseal � Blood transfusion whenever required � Antibiotic coverage whenever required � Nasal oxygen, tracheobronchial toiletting � Endotracheal intubation and Ventilator support whenever required � Surgery(thoracotomy, sternotomy) whenever appropriate
� Fracture of 2 or more consecutive ribs with each rib having 2 or more fracture sites � These in between fractured rib parts are called flail segments � These flail segments move independently of the rest of the rib cage causing pathophysiological derangements like -paradoxical respiration -mediastinal flutter -pendular air movement -hypoventilation -pulmonary contusion
� Types ( anterior flail-near costochondral junction, lateral flail-in rib shaft , posterior flail – rare) � Complications – cardiorespiratory arrest, hemothorax, mediastinal infections, acute respiratory distress syndrome � Investigations – chest x-ray/CT (to identify fracture segment), arterial blood gases(to monitor respiratory efficiency)
� treatment 1. Iv fluids, bronchodilators, steroids, oxygen and antibiotic support 2. Intercostal tube drainage 3. Thoracotomy and stabilization of the flail segments by surgical fixation with kwiring, clipping or dynamic compression plates 4. Ventilatory support ( intermittent positive pressure ventilation)
� Presence of air between the layers of the pleura � Basically divided into 2 types(open type and closed type wherein closed type is sub divided into simple and tension pneumothorax) � causes: -traumatic -spontaneous
� Spontaneous pneumothorax(causes) -tuberculous -non tuberculous (due to rupture of emphysematous bullae , rupture of solitary lung cyst, cystic fibrosis, idiopathic � Spontaneous -acute -chronic -recurrent pneumothorax(types)
� Clinical features – 1. respiratory distress 2. tachycardia 3. hyperresonant chest on percussion 4. absent/restricted air entry on the affected side 5. tracheal deviation � Diagnosis – chest x-ray / CT thorax -radiolucency on the affected side -collapsed lung margin and reduced broncho vascular markings on the affected side
� Management : 1. Oxygen and immediate hospitalization 2. Intercostal tube drainage with under water seal 3. Treatment of underlying cause 4. Thoracotomy if cause is due to ruptured cyst or if there is presence of bronchopleural fistula
� Iatrogenic drainage of air or fluid collected in the pleural cavity safely to allow the underlying lung to expand � Indications : -pneumothorax -hemopneumothorax -empyema thoracis -post thoracotomy patients to facilitate pleural cavity drainage
Procedure : -ICT is placed in the triangle of safety (5 th intercostal space in the mid axillary line, latissimus dorsi, pectoralis major) -under local anesthesia, incision is made in the skin over the lower part of the intercostal space to avoid injury to neurovascular bundle -then the ICT is inserted and the other end is immersed into an underwater seal. movement of air column in the ICT indicates that the ICT is functioning and the ICT is fixed to the overlying skin by means of a secure purse string suture -subsequently chest x-ray is taken to confirm its position -patient is then adviced to breathe normally �
� ICT is kept for 3 days at least to drain a pneumothorax and 6 days to drain a hemo or pyothorax. � Check x-rays are taken every 48 hours to note progress � Complications : 1. infection 2. displacement and inadequate functioning 3. injury to the intercostal neurovascular bundle 4. lung contusion due to rough insertion and handling of the intercostal tube 5. pain at the ICT site
� It is the situation where air enters the pleural space repeatedly and is unable to escape, so positive pressure builds up in the pleural cavity causing compression of the lung and mediastinal shift resulting in severe cardiorespiratory compromise � It’s a cause for sudden death and is a cardiovascular emergency � C/F : Tachypnoea, absent breath sounds, cyanosis, hypotension, chest pain, diaphoresis and finally cardiorespiratory arrest
� Chest x-ray or CT thorax is diagnostic � Management : 1. Wide bore needle into the 2 nd intercostal space along mid clavicular line and the opposite end into a sterile collection bag(to prevent inward sucking of air) 2. Nasal oxygen and immediate hospitalization 3. Subsequent passage of ICT with underwater seal 4. Antibiotics & analgesics 5. In severe cases ventilatory support(intermittent positive pressure ventilation)
� Presence � Causes of blood in the pleural cavity : 1. Trauma(due to rib fractures) 2. iatrogenic/post operative (pulmonary, cardiac and esophageal surgeries, cervical symphatectomy, complication of central venous line insertion) 3. Tumors of lung, mediastinum and pleura 4. Expansile aneurysms 5. spontaneous/idiopathic
� C/F : Chest pain, dyspnoea, tachycardia and hypotension in severe cases with diaphoresis, dullness on chest percusssion and decreased breath sounds on the affected side, hypovolemic shock and cardiorespiratory collapse. � Diagnosis : -chest x-ray(translucency on the affected side) -diagnostic pleural tap -CT thorax
� Management : 1. Oxygen and immediate hospitalization 2. Intercostal tube drainage with under water seal 3. Antibiotics and bronchodilators 4. Thoracotomy in severe cases
� It refers to surgical exploration of the chest and thoracic cavity � Types : 1. Posterolateral thoracotomy 2. Median sternotomy 3. Axillary thoracotomy 4. Antro lateral thoracotomy
� Indications : (emergencies) 1. Hemothorax > 1500 ml on ICT 2. Hourly collection of ICT > 200 ml 3. Persistent drainage of fresh blood in ICT 4. Diaphragmatic injury 5. Associated liver & spleen injuries 6. Bronchus & pulmonary vasculature injury 7. Hemopericardium 8. Aneurysmal aortic disease & aortic injury 9. Esophageal & thoracic duct injury
� Elective indications 1. Mediastinal tumor excision 2. Lung resections 3. Pleural tumor excision 4. Pulmonary embolectomy 5. Cardiac bypass & cardiac transplants
� Presence of emboli or thrombi in the lung or pulmonary vasculature � Types : minimal emboli and massive emboli � Minimal emboli present with pulmonary hypertension and features of bronchopneumonia � Massive emboli can result in total cardiorespiratory compromise with collapse and sudden death � Emboli can be present either in branches of pulmonary artery or at the bifurcation of the pulmonary trunk
� Risk factors 1. DVT of lower limbs 2. Post operative patients 3. Prolonged immobilization 4. Pregnancy 5. Obesity 6. Carcinoma Effects of pulmonary embolism : Decreased cardiac output, pulmonary vasospasm, bronchospasm, cardiopulmonary arrest.
C/F : dyspnoea, chest pain, hemoptysis, tachycardia, cyanosis, pleural rub with cardiac gallop on auscultation. Diagnosis : 1. Chest x-ray : palla’s sign(enlarged descending pulmonary artery) , westermark’s sign(decreased peripheral bronchovascular markings) 2. ECG – S 1(abnormal s wave in lead 1) Q 3(abnormal q wave in lead 3) T 3(t wave inversion in lead 3)
3. D-dimer assay( >500 microgram/ml) 4. Spiral CT 5. Pulmonary angiogram 6. Doppler study of the lower limbs to locate the DVT Management : 1. thrombolytics(streptokinase, tissue plasminogen activator) and anti coagulants. 2. Pulmonary embolectomy with cardiac bypass 3. Venous thrombectomy using fogarty catheter 4. Inferior vena cava filters 5. Ventilator support
