Directions Start Learning Points References Directions You are


- Slides: 15
Directions Start Learning Points References
Directions • You are working in a busy pediatric emergency department. • You will treat patients presenting with varied degrees of illness. • Choose options when prompted. You will receive feedback on your choice. • Feel free to peruse selected high-yield topics at the end of this lesson. Back
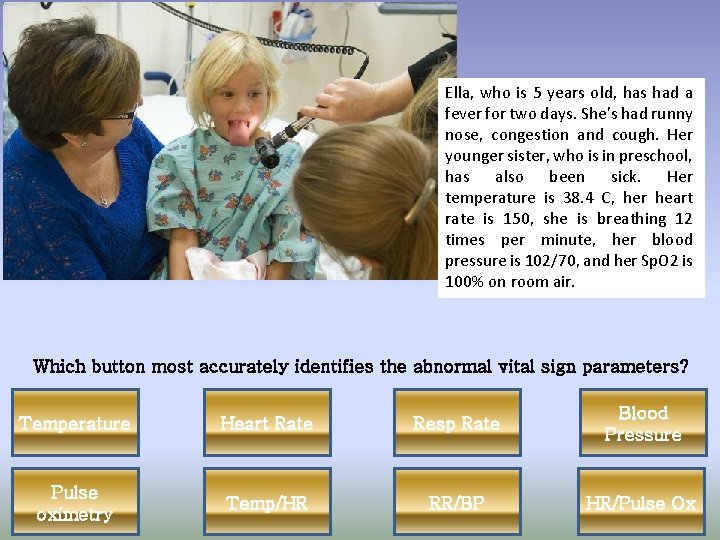
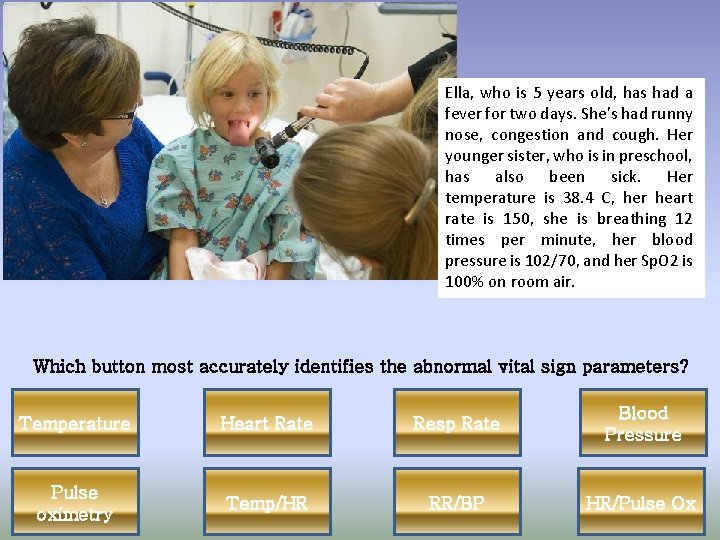
Ella, who is 5 years old, has had a fever for two days. She’s had runny nose, congestion and cough. Her younger sister, who is in preschool, has also been sick. Her temperature is 38. 4 C, her heart rate is 150, she is breathing 12 times per minute, her blood pressure is 102/70, and her Sp. O 2 is 100% on room air. Which button most accurately identifies the abnormal vital sign parameters? Temperature Heart Rate Resp Rate Blood Pressure Pulse oximetry Temp/HR RR/BP HR/Pulse Ox
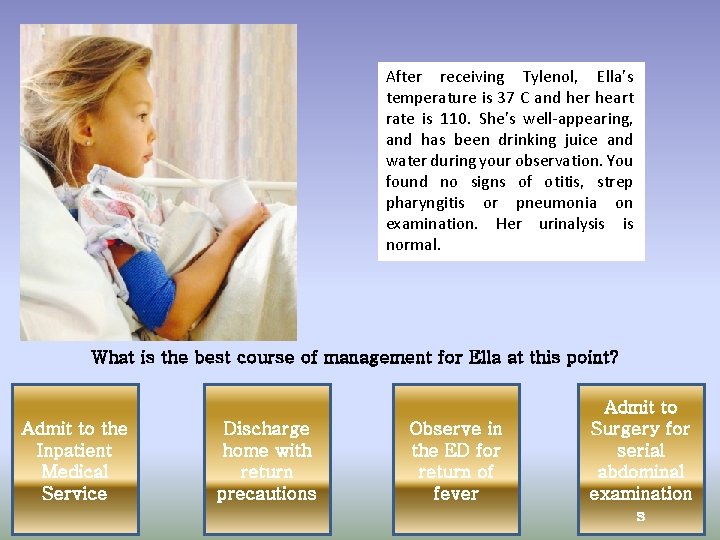
After receiving Tylenol, Ella’s temperature is 37 C and her heart rate is 110. She’s well-appearing, and has been drinking juice and water during your observation. You found no signs of otitis, strep pharyngitis or pneumonia on examination. Her urinalysis is normal. What is the best course of management for Ella at this point? Admit to the Inpatient Medical Service Discharge home with return precautions Observe in the ED for return of fever Admit to Surgery for serial abdominal examination s

That was incorrect. Try again. Back
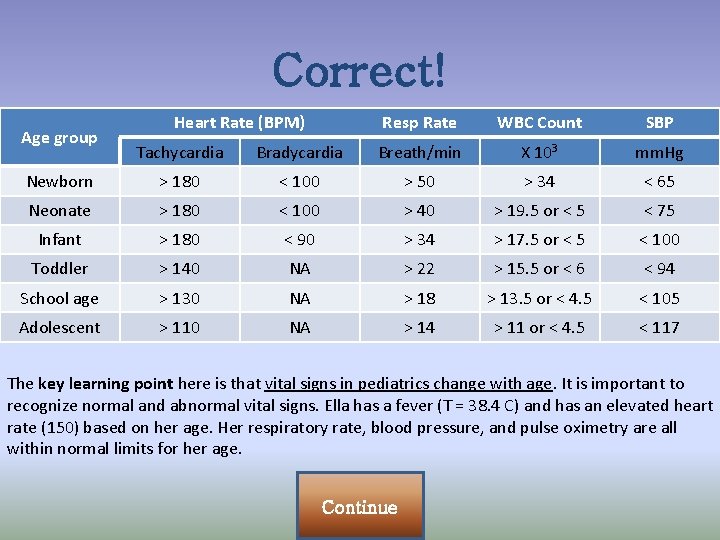
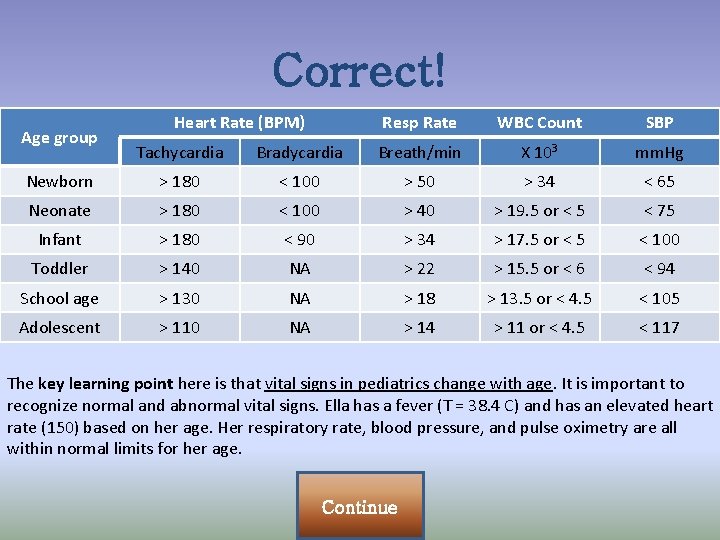
Correct! Age group Heart Rate (BPM) Resp Rate WBC Count SBP Tachycardia Bradycardia Breath/min X 103 mm. Hg Newborn > 180 < 100 > 50 > 34 < 65 Neonate > 180 < 100 > 40 > 19. 5 or < 5 < 75 Infant > 180 < 90 > 34 > 17. 5 or < 5 < 100 Toddler > 140 NA > 22 > 15. 5 or < 6 < 94 School age > 130 NA > 18 > 13. 5 or < 4. 5 < 105 Adolescent > 110 NA > 14 > 11 or < 4. 5 < 117 The key learning point here is that vital signs in pediatrics change with age. It is important to recognize normal and abnormal vital signs. Ella has a fever (T = 38. 4 C) and has an elevated heart rate (150) based on her age. Her respiratory rate, blood pressure, and pulse oximetry are all within normal limits for her age. Continue
Correct! Continue Ella’s temperature and heart rate are normal on repeat check. She’s demonstrated good oral tolerance, and she hasn’t had any report of excessive losses (vomiting or diarrhea). She’s not demonstrating any exam findings that suggest a need for antibiotics at this time. Based on her overall well appearance, it is not necessary to admit to the medical inpatient service, and further observation with this appearance is unnecessary. Without any signs of abdominal pain or poor oral tolerance, it is unnecessary to involve surgical services at this time. The key learning point here is to reassess patients after interventions (Tylenol) and ensure your patient is following an expected course. Additionally, be sure you provide good return precautions and follow up with primary care physicians.

Timmy, an 8 yo AA male, presents to the resuscitation bay by EMS. He is ill-appearing on arrival, and at times seems rather sleepy. You frequently have to stimulate him to keep his eyes open. His temperature is 39. 6 C, his heart rate is 155, his respiratory rate is 35, his blood pressure is 98/50, and his Sp. O 2 is 94% on non-rebreather at 8 LPM. His breath sounds are decreased on the left, with crackles throughout and labored breathing. His capillary refill is 3 -4 seconds. His abdominal exam is benign. Classify Timmy’s clinical presentation. Dehydrated Compensated Septic Shock SIRS Uncompensated Septic Shock
You’ve kept Timmy on supplemental oxygen to optimize his oxygenation and work of breathing. You’ve placed an initial IV, and your nurses are working on obtaining labs off of a second stick. Recognizing that Timmy is in compensated shock, what is your immediate plan? Chest X-ray Viral Respiratory PCR Tylenol Early Goal. Directed Therapy
Your attending agrees that Timmy needs Early Goal-Directed Therapy for his compensated septic shock. He then asks you what that entails. What is the cornerstone of Early Goal-Directed Therapy? Early Antibiotics and aggressive IV fluids Early transfer to Intensive Care Unit Early imaging Early Antipyretic administration
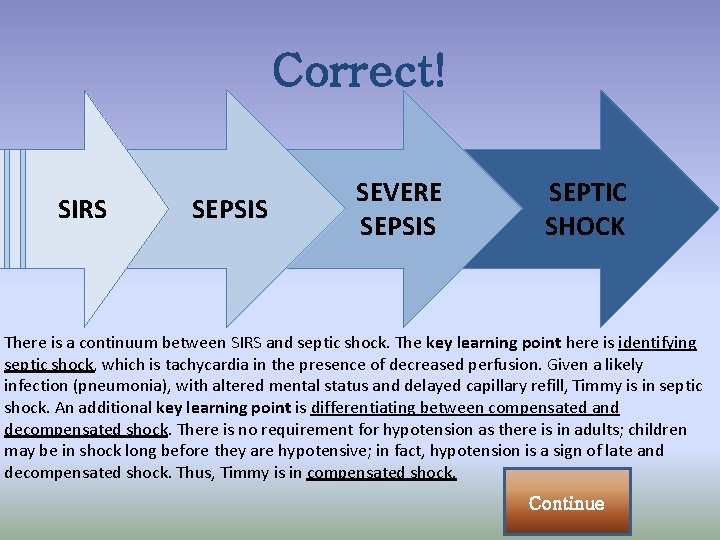
Correct! SIRS SEPSIS SEVERE SEPSIS SEPTIC SHOCK There is a continuum between SIRS and septic shock. The key learning point here is identifying septic shock, which is tachycardia in the presence of decreased perfusion. Given a likely infection (pneumonia), with altered mental status and delayed capillary refill, Timmy is in septic shock. An additional key learning point is differentiating between compensated and decompensated shock. There is no requirement for hypotension as there is in adults; children may be in shock long before they are hypotensive; in fact, hypotension is a sign of late and decompensated shock. Thus, Timmy is in compensated shock. Continue
Correct! The key learning point here is that early goal therapy has been shown to improve morbidity and mortailty in adult sepsis. Management guidelines have been developed in pediatrics to reflect these principles, and researchers in Pediatrics (including Peds EM) have demonstrated an improvement in outcomes in septic pediatric patients as well. Continue
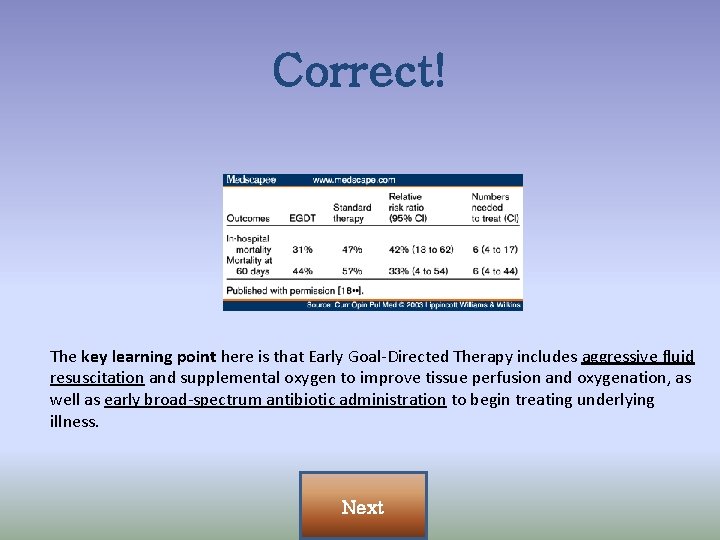
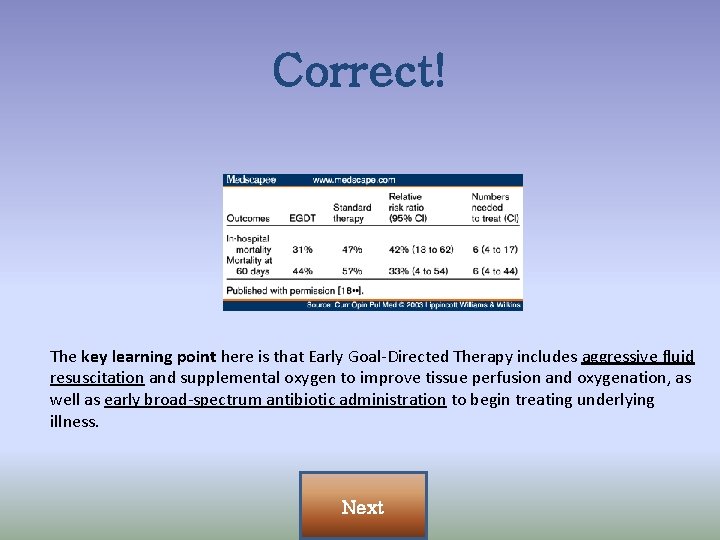
Correct! The key learning point here is that Early Goal-Directed Therapy includes aggressive fluid resuscitation and supplemental oxygen to improve tissue perfusion and oxygenation, as well as early broad-spectrum antibiotic administration to begin treating underlying illness. Next
Key Learning Points • Vital signs in pediatrics change with age. • Reassess patients after interventions. • Provide easy to follow return precautions for ill patients & ensure follow up plan in place. • Septic shock is tachycardia and signs of poor perfusion in setting of infection. • Pediatric patients can be in septic shock without hypotension (compensated sepsis). • Early Goal-Directed Therapy is the hallmark of Pediatric sepsis management. • EGDT includes early antibiotic administration and aggressive fluid resuscitation. Back
Selected High-Yield References • Brierley, J. , Carcillo, J. A. , Choong, K. , et al. (2009). Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine, 37(2), 666 -688. doi: 10. 1097/CCM. 0 b 013 e 31819323 c 6 • El-wiher, N. , Cornell, T. T. , Kissoon, N. , & Shanley, T. P. (2011). Management and Treatment Guidelines for Sepsis in Pediatric Patients. The Open Inflammation Journal, 4(Suppl 1 -M 11), 101 -109. doi: 10. 2174/1875041901104010101 • Maloney, P. J. (2013). Sepsis and septic shock. Emergency Medicine Clinics of North America, 31, 583 – 600. doi: 10. 1016/j. emc. 2013. 04. 0060733 -8627/13/$ • Watson, R. S. , Carcillo, J. A. , Linde-Zwirble, W. T. , et al. (2003). The epidemiology of severe sepsis in children in the United States. American Journal of Respiratory Critical Care Medicine, 167(5), 695701. doi: 10. 1164/rccm/200207 -682 OC Back