DEALING WITH MEDICAL UNCERTAINTY MEDICAL CERTIFICATION OF CAUSE
- Slides: 17
DEALING WITH MEDICAL UNCERTAINTY MEDICAL CERTIFICATION OF CAUSE OF DEATH, TONGA NOVEMBER, 2018
Uncertainty is a fact of life (and death) as a doctor • • • The medical certificate records the facts surrounding the cause of death – to the best of your knowledge There will always be an element of uncertainty in this diagnosis In most cases there is some information available about the cause of death Ill-defined or unknown (or variants of this – old age, sudden death, DOA) should only be used where it is not possible to make a reasonable or “most likely” diagnosis Similar to a principal diagnosis (vs differential diagnosis) – except that you only get to do it once~
Ill-defined cases • Leaving a cause of death as an ill-defined cause means that it is not counted in the statistics – and therefore may have policy, resource and funding implications • For example – if we do not record probable cancer related deaths because we have not done a biopsy, cancer does not appear to be as big a problem in the country as it may be.
Common Sources of Uncertainty • Complex medical histories/ multiple co-morbidities • Diagnostic tests were not available • Missing information/ not familiar with the case (i. e. DOA cases)
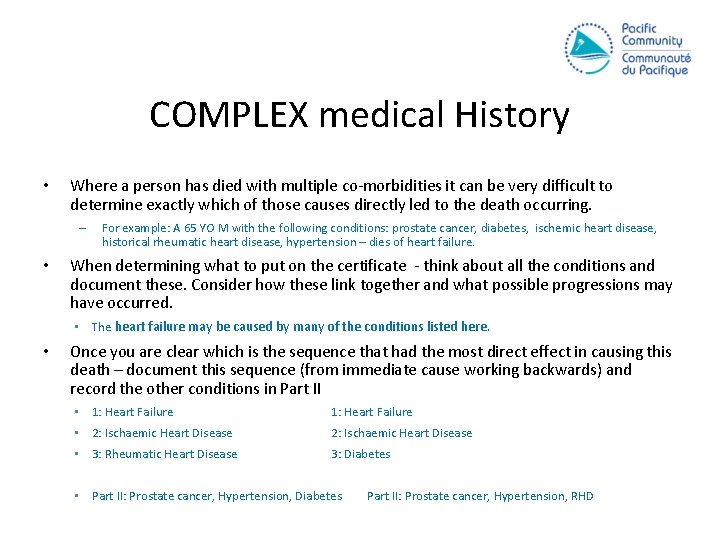
COMPLEX medical History • Where a person has died with multiple co-morbidities it can be very difficult to determine exactly which of those causes directly led to the death occurring. – • For example: A 65 YO M with the following conditions: prostate cancer, diabetes, ischemic heart disease, historical rheumatic heart disease, hypertension – dies of heart failure. When determining what to put on the certificate - think about all the conditions and document these. Consider how these link together and what possible progressions may have occurred. • The heart failure may be caused by many of the conditions listed here. • Once you are clear which is the sequence that had the most direct effect in causing this death – document this sequence (from immediate cause working backwards) and record the other conditions in Part II • 1: Heart Failure • 2: Ischaemic Heart Disease • 3: Rheumatic Heart Disease 3: Diabetes • Part II: Prostate cancer, Hypertension, Diabetes Part II: Prostate cancer, Hypertension, RHD
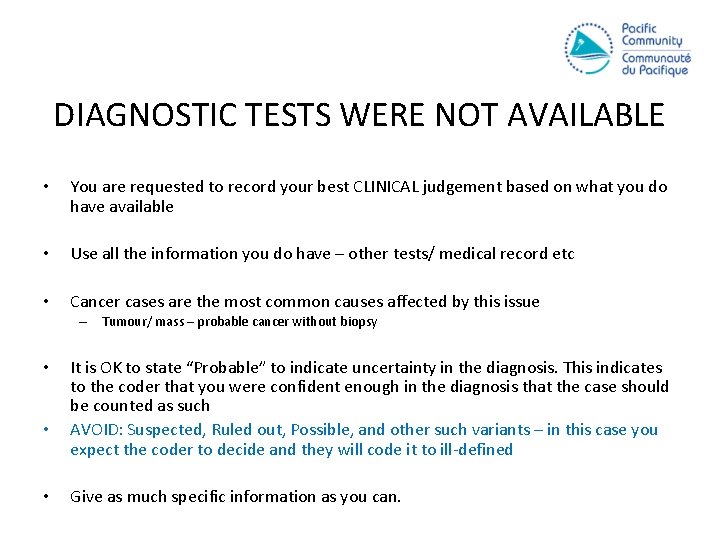
DIAGNOSTIC TESTS WERE NOT AVAILABLE • You are requested to record your best CLINICAL judgement based on what you do have available • Use all the information you do have – other tests/ medical record etc • Cancer cases are the most common causes affected by this issue – Tumour/ mass – probable cancer without biopsy • • • It is OK to state “Probable” to indicate uncertainty in the diagnosis. This indicates to the coder that you were confident enough in the diagnosis that the case should be counted as such AVOID: Suspected, Ruled out, Possible, and other such variants – in this case you expect the coder to decide and they will code it to ill-defined Give as much specific information as you can.
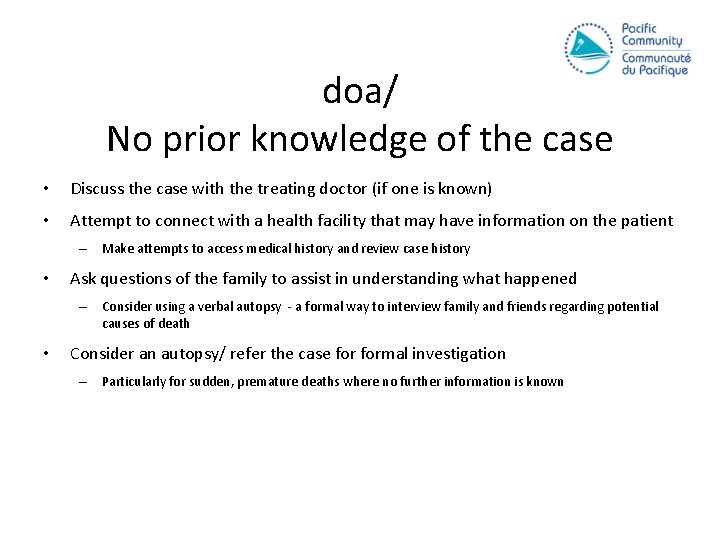
doa/ No prior knowledge of the case • Discuss the case with the treating doctor (if one is known) • Attempt to connect with a health facility that may have information on the patient – Make attempts to access medical history and review case history • Ask questions of the family to assist in understanding what happened – Consider using a verbal autopsy - a formal way to interview family and friends regarding potential causes of death • Consider an autopsy/ refer the case formal investigation – Particularly for sudden, premature deaths where no further information is known
Policy and legislation • be aware of legislation, hospital policy • how do these translate to your obligations as a certifying doctor? • talk to hospital director, hospital review committee if you are unclear of legislation and policy requirements SAMOA BDM ACT 2002 47. (5) Every doctor required to provide a medical certificate under subsection (3) must (a) Carefully question every person who was present at the death and who recently was with the deceased before death; and (b) Make such other inquires as in the opinion of the doctor are reasonable in the circumstances to determine the cause of the death.
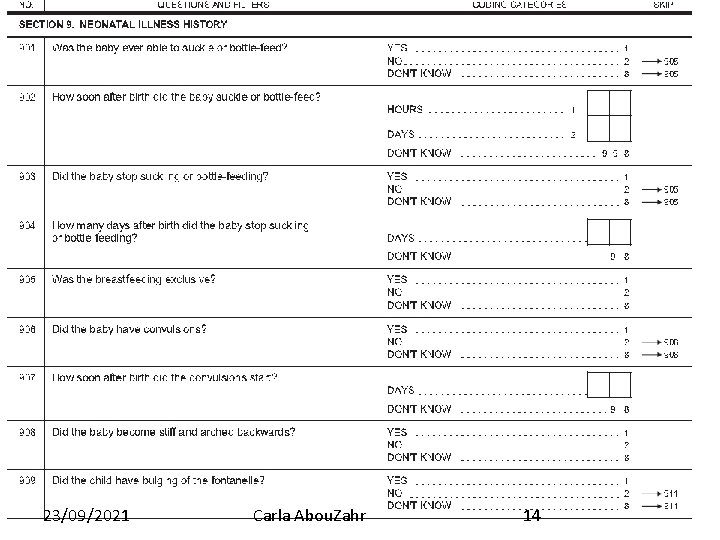
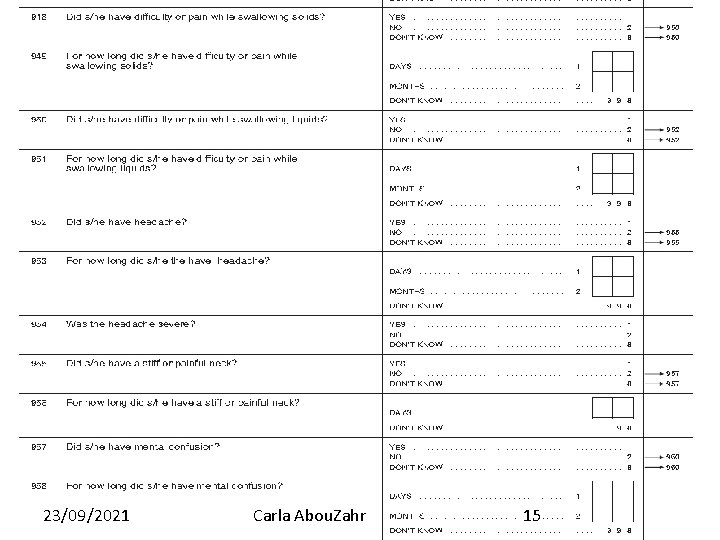
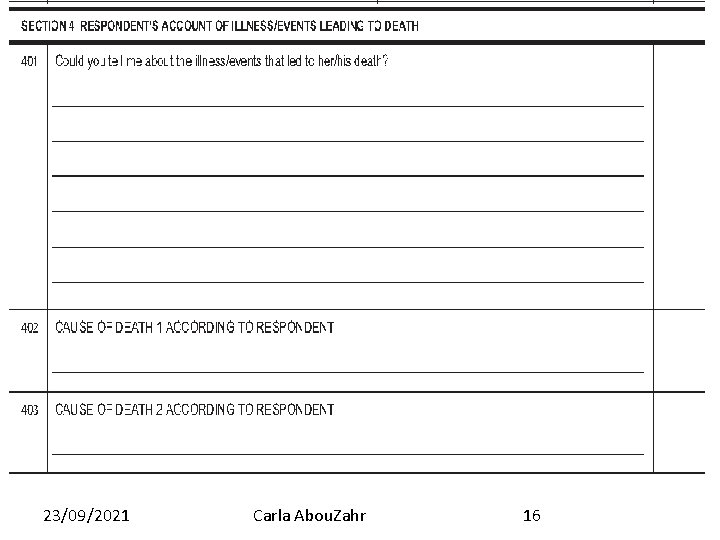
Components of the WHO verbal autopsy guidelines I. II. Questionnaire for interview with family members and/or caregivers : Ø Neonates (<4 weeks) Ø Infant and children (4 weeks to 14 years) Ø Adults, 15 years and over Application of ICD-10 to verbal autopsy interviews Ø Certification by medically trained personnel Ø Professionalised coding; use of automated algorithms 9
Using VA to Complement A medical diagnosis • Verbal autopsy tools were designed to assist in determining population level cause of death patterns in areas where doctors are not available to determine cause of death • They are reasonably accurate at the population level, but much less so at the individual level • However – the structured questionnaire can be used by doctors to ADD to their examination and assist in making a diagnosis. • Verbal autopsy is not designed to replace the medical opinion
Verbal autopsy questionnaires § Respondent should be primary caregiver (usually family member) who was with the deceased prior to death. § Short recall periods preferable (< 1 year). § Careful determinant of timing of the interview- consider appropriate mourning periods § Local adaptation of questionnaire usually needed. § Interviewer does not need to be medical doctor but should have some medical knowledge (e. g. community health worker) and training § Response-based sequencing
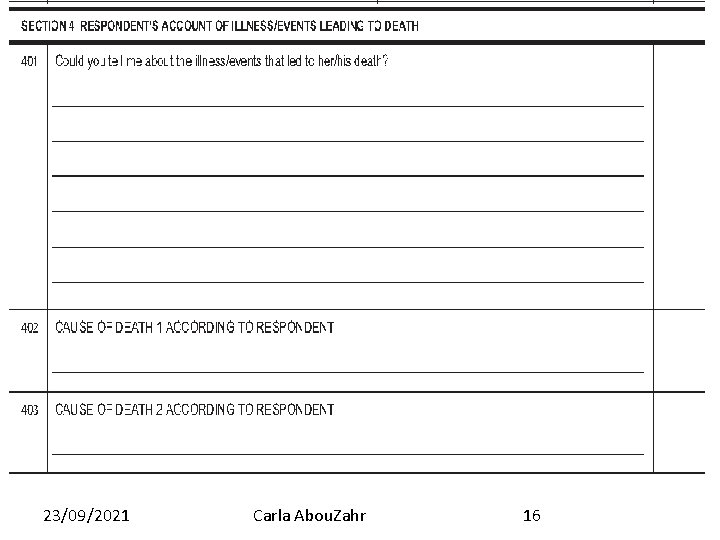
Verbal autopsy questionnaires • Common elements Ø Unique ID or reference number Ø Date, place, time of interview; identity of interviewee Ø Informed consent statement Ø Respondent characteristics Ø Time, place and date of death Ø Name, sex and age of deceased Ø Causes of death and events leading up to the death, according to the respondent
Verbal autopsy questionnaires • Additional elements Ø History of previously known medical conditions (of the deceased or of the mother in the case of an infant death) Ø History of injury or accident Ø Treatment and health service use during the period of final illness Ø Data abstracted from death certificates, antenatal or maternal and child health clinic cards Ø Other medical records and relevant documentary evidence at the household level.
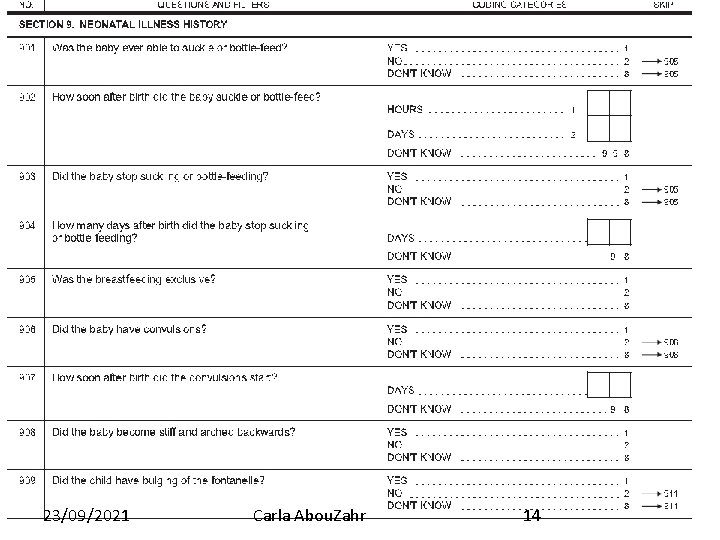
23/09/2021 Carla Abou. Zahr 14
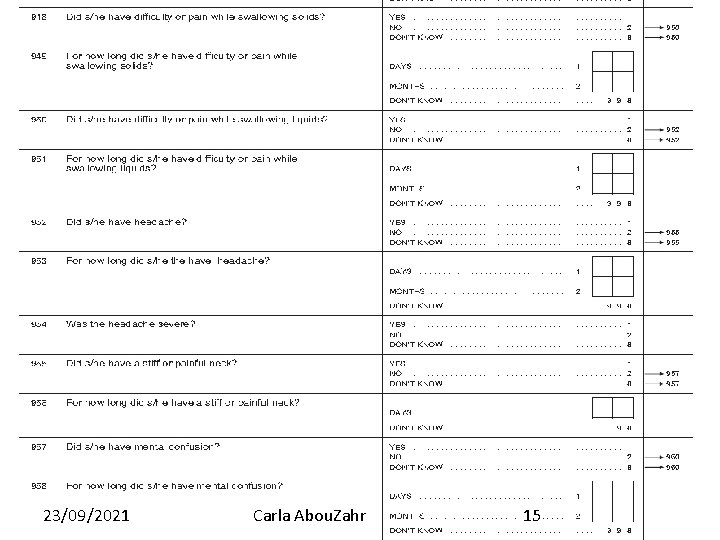
23/09/2021 Carla Abou. Zahr 15
23/09/2021 Carla Abou. Zahr 16
RESOURCES WHO 2016 Verbal Autopsy Instrument http: //www. who. int/healthinfo/statistics/verbalautopsystandards/en/
 Medical uncertainty
Medical uncertainty Underlying cause and immediate cause
Underlying cause and immediate cause Greylag goose egg-retrieval behavior
Greylag goose egg-retrieval behavior Proximate and ultimate causes of behaviour
Proximate and ultimate causes of behaviour Proximate cause and ultimate cause
Proximate cause and ultimate cause National board of certified medical interpreters
National board of certified medical interpreters Assimilation linguistics
Assimilation linguistics What are abiotic factors
What are abiotic factors Section 2 dealing with other nations
Section 2 dealing with other nations Call center stress
Call center stress Dealing with competition in marketing
Dealing with competition in marketing It is genre of speculative fiction
It is genre of speculative fiction Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Dealing with competition marketing management
Dealing with competition marketing management Unit 1 dealing with incoming calls
Unit 1 dealing with incoming calls Dealing with anger bible
Dealing with anger bible Dealing successfully with difficult changes in your life.
Dealing successfully with difficult changes in your life.