CERTIFYING PERINATAL DEATHS MEDICAL CERTIFICATION OF CAUSE OF





- Slides: 17
CERTIFYING PERINATAL DEATHS MEDICAL CERTIFICATION OF CAUSE OF DEATH, TONGA NOVEMBER, 2018
PERINATAL DEATHS Scope of perinatal deaths: - neonatal deaths - stillbirths Neonatal Definition: A child who is born of any age who shows signs of life who dies between 0 -27 completed days - 0 -7 days: early neonatal death - 8 -27 days: late neonatal death Stillbirth (or fetal death): A child who is born who does not show any signs of life - WHO definition states between 22 weeks completed gestation and 500 grams birth weight - check with your legislative requirements in-country on definition
PERINATAL DEATHS • Neonatal deaths generally form the majority of infant deaths • High quality data helps us address maternal and infant health • Related to SDG 3:
PERINATAL DEATHS • 2 types of death certificates possible: • General death certificate • Perinatal death certificate • WHO recommends general death certificate • Demographic information is extremely important for perinatal deaths
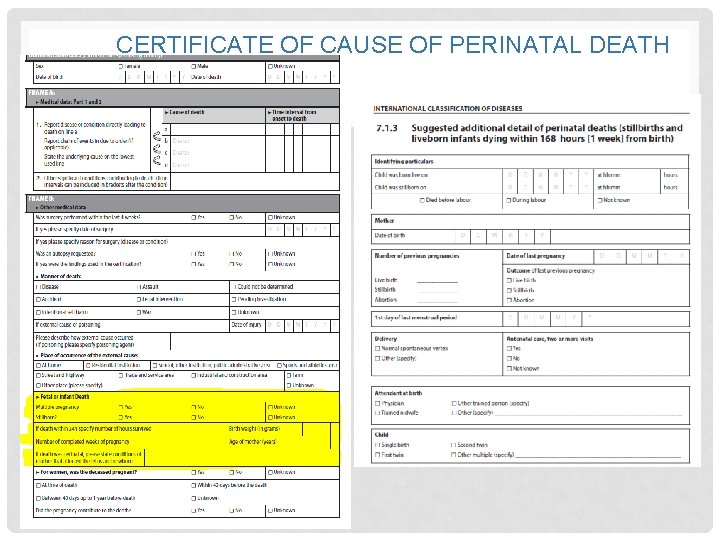
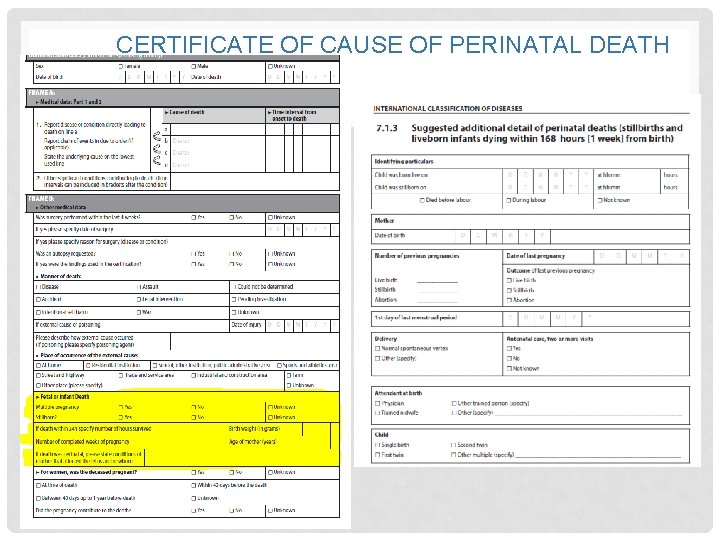
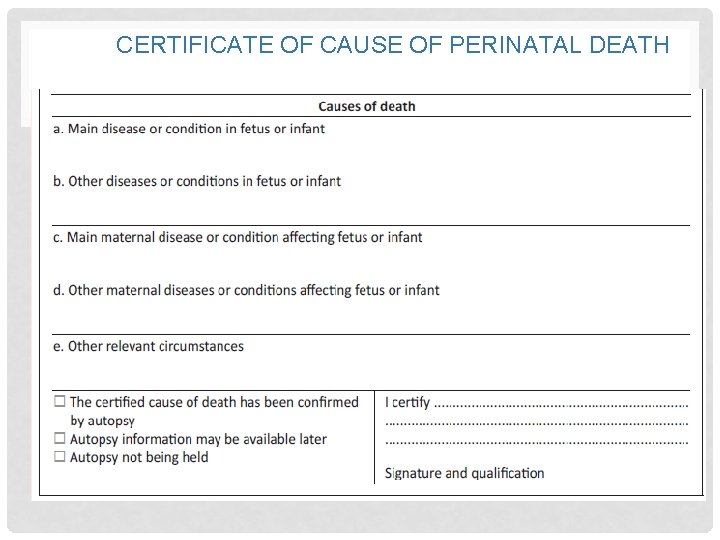
CERTIFICATE OF CAUSE OF PERINATAL DEATH
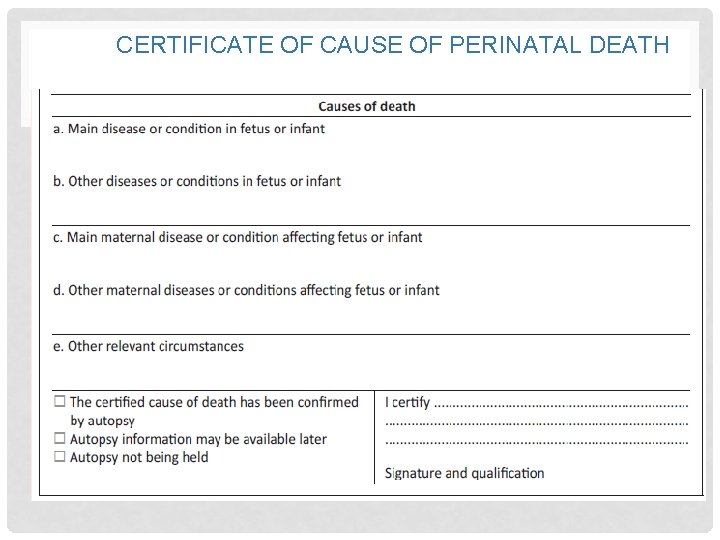
CERTIFICATE OF CAUSE OF PERINATAL DEATH

ENFORCE, IMPLEMENT & EVALUATE 7
PERINATAL DEATHS • Activity: Look at your own country’s death certificate and document what recommended variables are missing. Record what type of death certificate you are using (i. e. general death certificate or perinatal)
PERINATAL DEATHS • Conditions in mother versus baby • • Very important interaction Be aware of causes which can occur in both mother and baby E. g. hypertension, haemorrhage Need to give more exact terms e. g. pre-eclampsia, abruption of placenta, maternal hypertension • Are conditions pre-existing? • E. g. diabetes (state whether gestational or existing, hypertension, other circulatory conditions)
PERINATAL DEATHS • Communicate conditions in mother that may have caused condition in baby • E. g. prematurity • Tell the coder why – early onset of labour from incompetent cervix? Placental abruption? (this helps interventions) • External versus natural • Asphyxia (cord accident, bedclothes over baby) • Congenital versus acquired • E. g. pulmonary hypoplasia, hydrocephalus
SPECIFIC CONDITIONS • Pre-term labour • Use if no clear pathology (e. g. chorioamnionitis) of labour before 37 weeks • Growth restriction • Use best diagnostic tools available • Difficult in many settings • Prematurity • Avoid using without pathology known • Obstructed labour • Enter as main condition if reason is related to mother (transverse pelvis) but enter as secondary condition if reason is for transverse fetus • HIV • Always enter if existent in mother
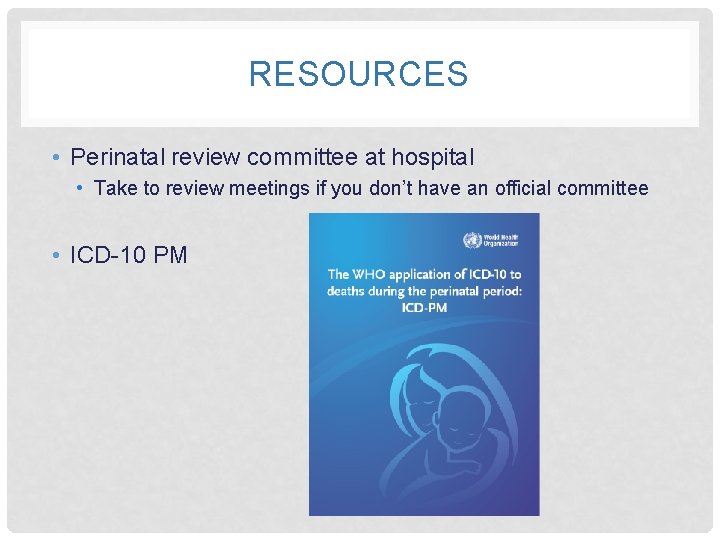
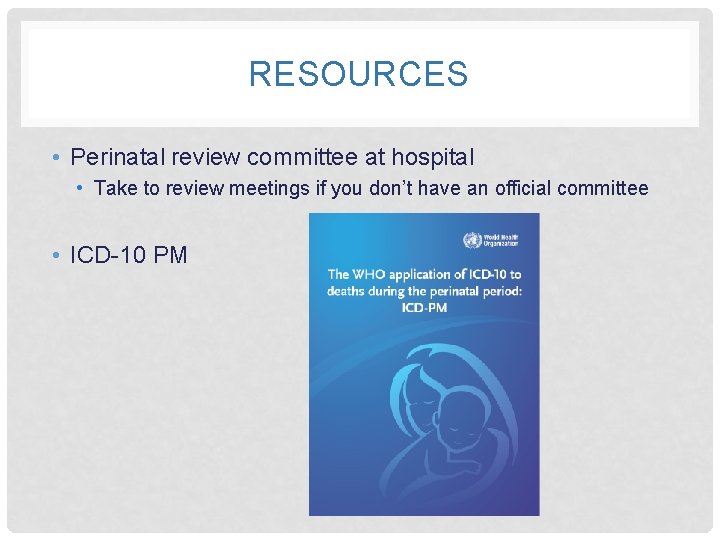
RESOURCES • Perinatal review committee at hospital • Take to review meetings if you don’t have an official committee • ICD-10 PM
FILLING OUT DEATH CERTIFICATE • Need to consider certificate used in your country • Sequence needs to take into account mother and baby • If different from WHO standard consider how to communicate relevant information • Maternal care, existing conditions in mother and maternal conditions all need to be taken into account • Don’t forget to fill out a birth notification and medical cause of death certificate for perinatal deaths

ACTIVITY Do exercises provided – fill out once on WHO recommended certificate. Fill out again on own country certificate and consider how to communicate all relevant information if variables are not included on the death certificate.

ACTIVITY 1 A pregnant mother with poorly controlled Diabetes Mellitus delivered a infant weighing 3. 5 kg at 37 weeks of gestation. The baby developed hypoglycaemia and had a loud murmur and a large heart on chest x ray. The echocardiogram showed multiple anomalies in the heart. The baby died on the second day of life.

ACTIVITY 2 A 1, 480 -gram male infant was born at 32 -weeks gestation to a 20 -year -old primiparous woman. The infant developed respiratory distress syndrome and required mechanical ventilation for 7 days. Despite receiving adequate calories for growth, the infant gained weight poorly and had persistent diarrhea. Steatorrhea was confirmed upon microscopic examination. Results from a sweat chloride test given on the 21 st day after birth were negative, but the patient had an elevated sweat chloride concentration of 85 millimoles per liter when the test was repeated at 35 days of age. On the 37 th day after birth, the infant became lethargic and was noted to be oedematous. Escherichia coli was cultured from the infant’s cerebral spinal fluid, total serum proteins were reported to be low, and clotting studies were prolonged. The infant died at 45 days of age despite appropriate life-saving efforts. Gross autopsy confirmed the clinical impression of cystic fibrosis.

ACTIVITY 3 The patient was a 30 year old woman with a healthy four year old boy. She had a normal second pregnancy apart from hydramnios. Ultrasound examination of the fetus at 36 weeks noted the presence of anencephaly. Labour was induced. A stillborn anencephalic fetus weighing 1500 g was delivered.
 Geeky medics certify death
Geeky medics certify death Perinatal asphyxia
Perinatal asphyxia Perinatal asphyxia
Perinatal asphyxia Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Clear perinatal quality
Clear perinatal quality Perinatal risk factors
Perinatal risk factors Perinatal asphyxia
Perinatal asphyxia Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Perinatal matrices
Perinatal matrices Perinatal period
Perinatal period Perinatal audit
Perinatal audit Ccqi perinatal standards
Ccqi perinatal standards Fatin organ
Fatin organ Waiter's tip deformity
Waiter's tip deformity Ruta materno perinatal
Ruta materno perinatal Cem samut
Cem samut South dakota perinatal association
South dakota perinatal association Dr abeer deaths
Dr abeer deaths