Covid19 Update Phase I Prepare Triaging patients and

- Slides: 12
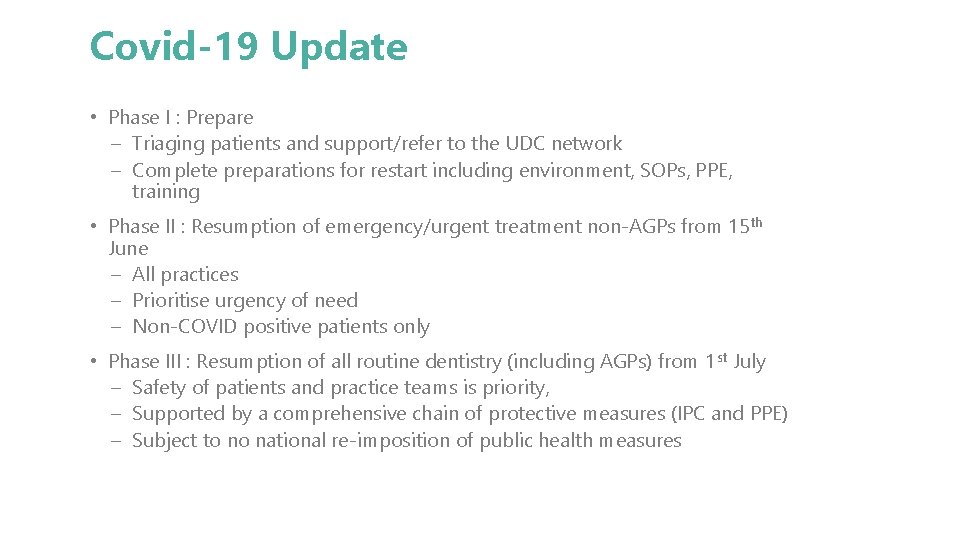
Covid-19 Update • Phase I : Prepare – Triaging patients and support/refer to the UDC network – Complete preparations for restart including environment, SOPs, PPE, training • Phase II : Resumption of emergency/urgent treatment non-AGPs from 15 th June – All practices – Prioritise urgency of need – Non-COVID positive patients only • Phase III : Resumption of all routine dentistry (including AGPs) from 1 st July – Safety of patients and practice teams is priority, – Supported by a comprehensive chain of protective measures (IPC and PPE) – Subject to no national re-imposition of public health measures
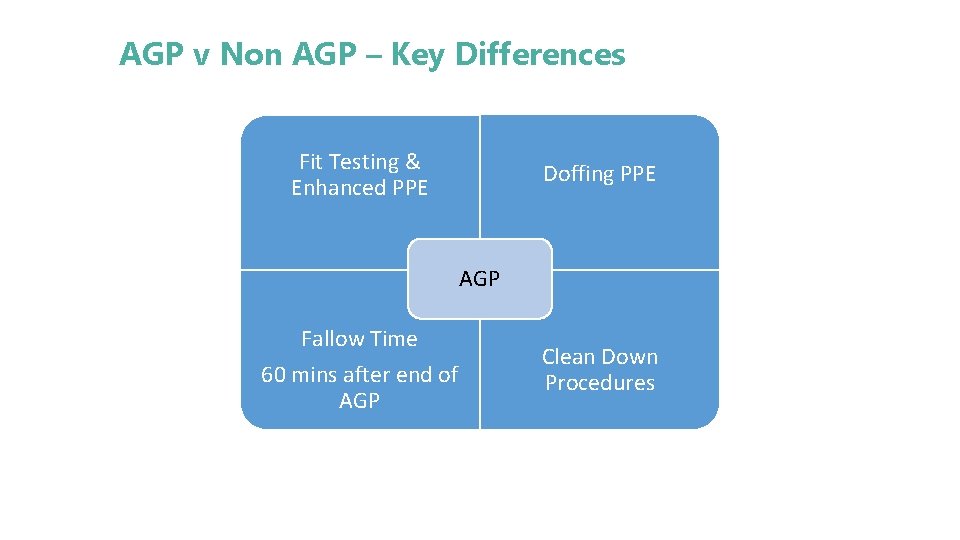
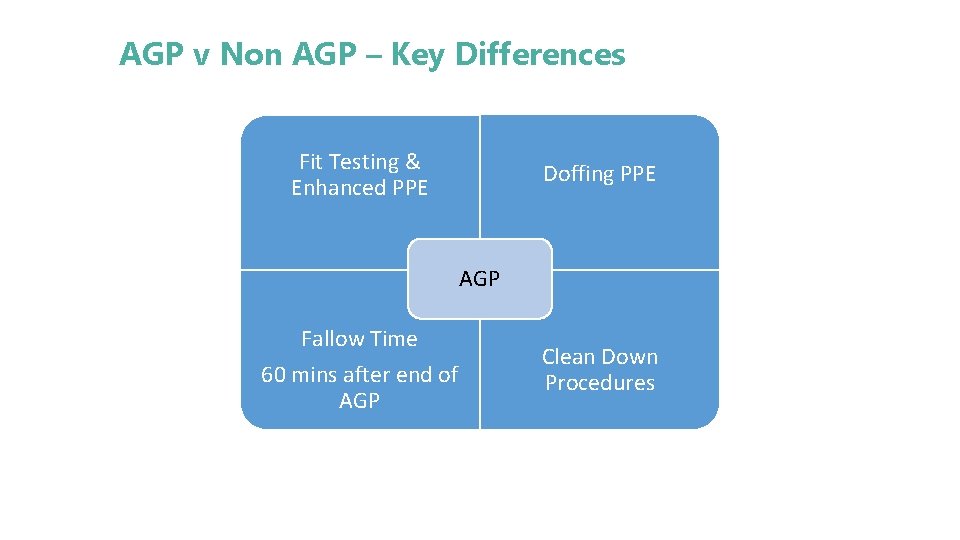
AGP v Non AGP – Key Differences Fit Testing & Enhanced PPE Doffing PPE AGP Fallow Time 60 mins after end of AGP Clean Down Procedures
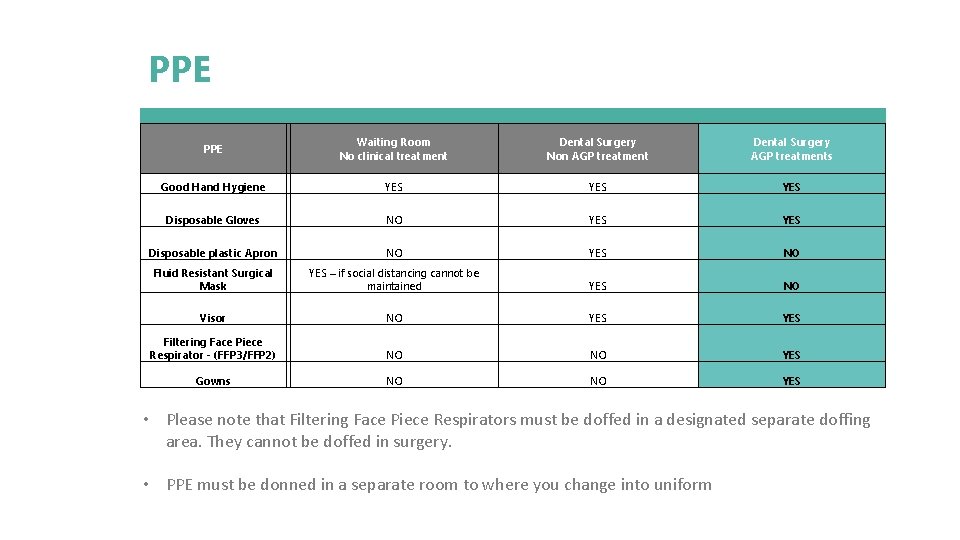
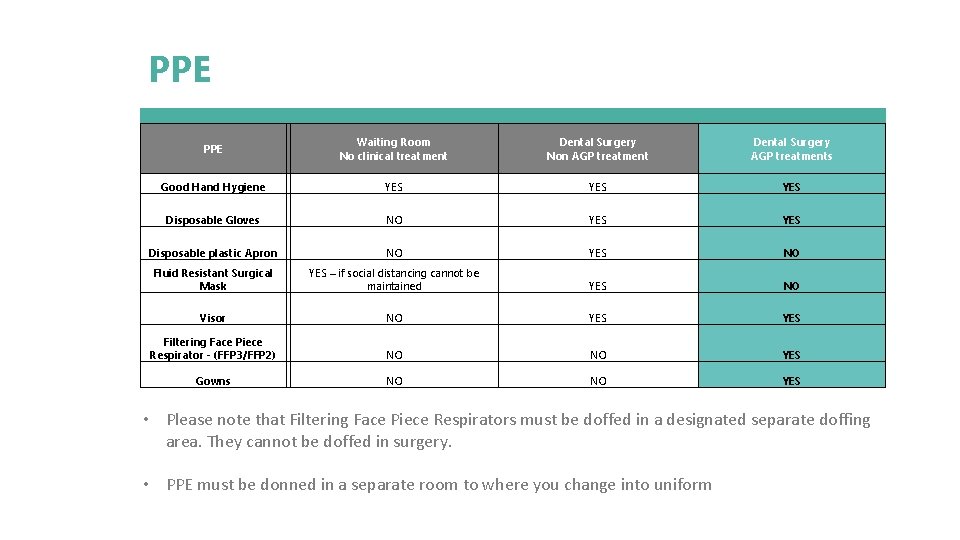
PPE Waiting Room No clinical treatment Dental Surgery Non AGP treatment Dental Surgery AGP treatments Good Hand Hygiene YES YES Disposable Gloves NO YES Disposable plastic Apron NO YES NO Fluid Resistant Surgical Mask YES – if social distancing cannot be maintained YES NO Visor NO YES Filtering Face Piece Respirator - (FFP 3/FFP 2) NO NO YES Gowns NO NO YES • Please note that Filtering Face Piece Respirators must be doffed in a designated separate doffing area. They cannot be doffed in surgery. • PPE must be donned in a separate room to where you change into uniform
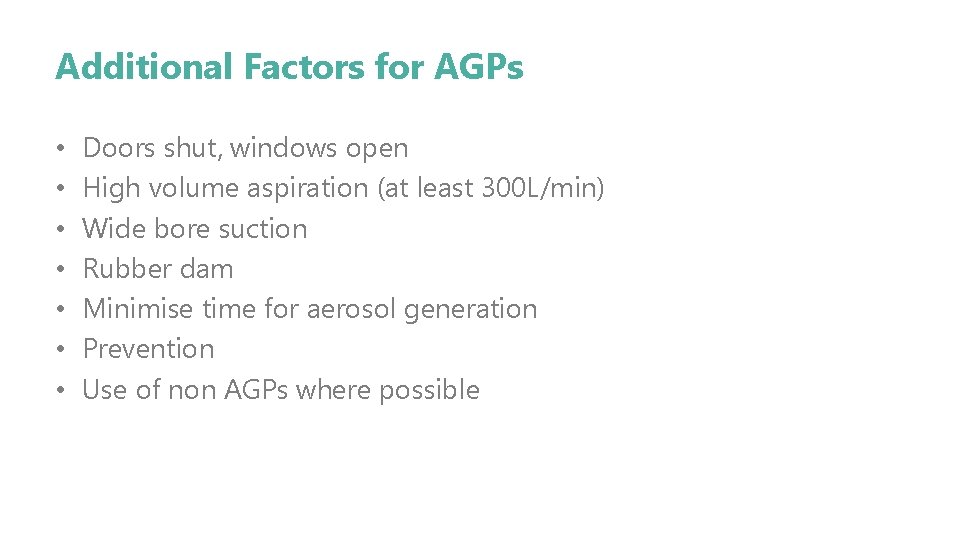
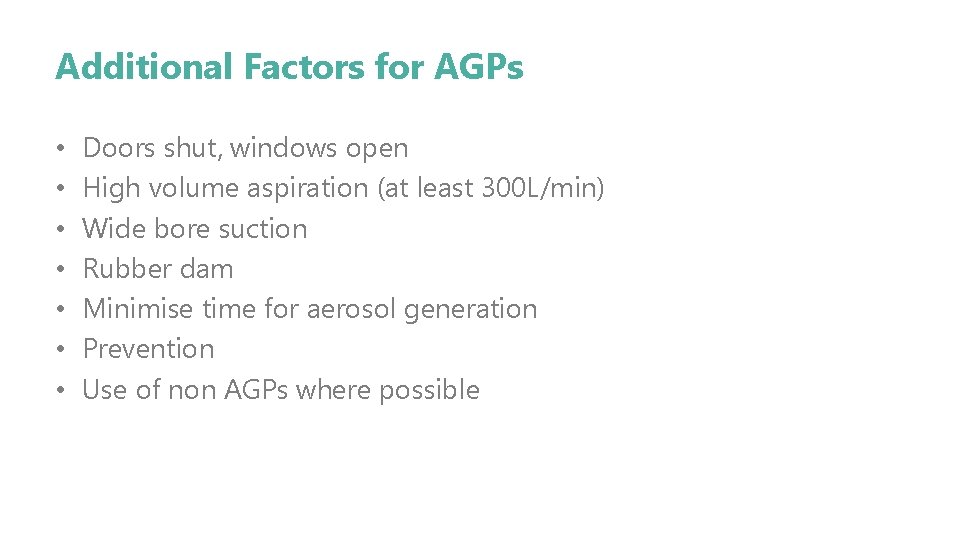
Additional Factors for AGPs • • Doors shut, windows open High volume aspiration (at least 300 L/min) Wide bore suction Rubber dam Minimise time for aerosol generation Prevention Use of non AGPs where possible
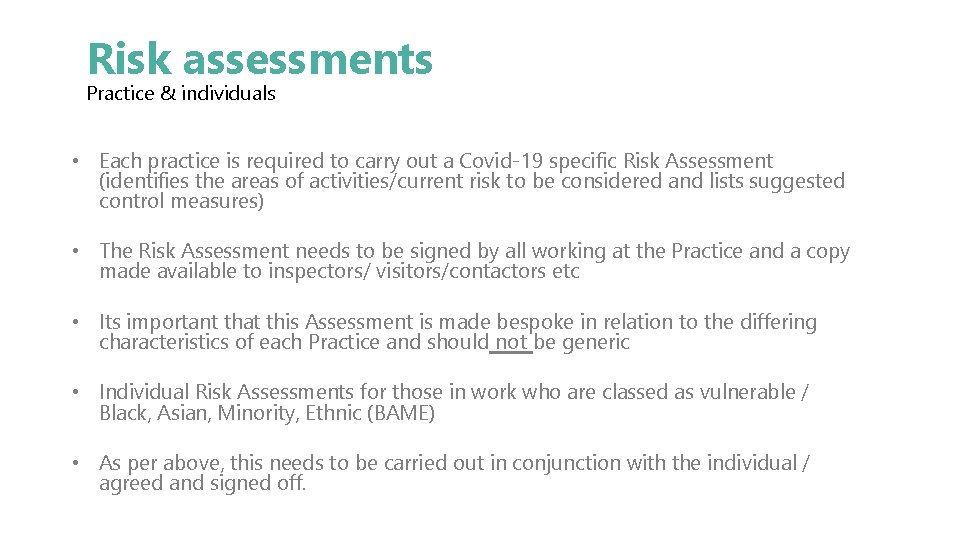
Risk assessments Practice & individuals • Each practice is required to carry out a Covid-19 specific Risk Assessment (identifies the areas of activities/current risk to be considered and lists suggested control measures) • The Risk Assessment needs to be signed by all working at the Practice and a copy made available to inspectors/ visitors/contactors etc • Its important that this Assessment is made bespoke in relation to the differing characteristics of each Practice and should not be generic • Individual Risk Assessments for those in work who are classed as vulnerable / Black, Asian, Minority, Ethnic (BAME) • As per above, this needs to be carried out in conjunction with the individual / agreed and signed off.
Infection Prevention and Control • All standard infection prevention and control measures still stand following HTM 01 -05 • Additional robust infection prevention and control procedures in line with government advice must be adhered to. • PPE protocols in line with government advice must be adhered to. • Practices should appoint a COVID-19 lead. The COVID-19 lead is responsible for the co-ordination of activities within a dental service, training and communication with the dental team. • Dental teams working at the practice should be aware of the SOP the current national and local COVID-19 guidance • All patients should be prioritised according to need
Transmission Based Precautions • Transmission Based Precautions (TBPs) are applied when standard infection control precautions (SICPs) alone are insufficient to prevent cross transmission of an infectious agent. They are additional infection control precautions required when caring for a patient with a known or suspected infectious agent. • The transmission of COVID-19 is thought to occur mainly through respiratory droplets generated by coughing and sneezing, and through contact with contaminated surfaces. Interrupting transmission in the dental surgery needs to be by undertaking contact, droplet and aerosol precautions. • Contact precautions: used to prevent and control infection transmission via direct contact or indirectly from the immediate care environment. • Droplet precautions: used to prevent and control infection transmission over short distances via droplets (>5μm) from the patient to a mucosal surface or the conjunctivae of a dental team member. A distance of approximately 1 metre around the infected individual is the area of risk for droplet transmission which is why dental teams routinely wear fluid resistant surgical masks (FRSM) and eye protection for treating patients. However, a distance of 2 metres has been defined as the area of risk. Thus, distancing of 2 metres should be facilitated wherever this is possible. This includes all staff adhering to social distancing wherever possible, particularly if not wearing a facemask or visor and when in non-clinical areas such as communal areas and during work breaks. • Airborne precautions: used to prevent and control infection transmission via aerosols (≤ 5μm) from the respiratory tract of the patient directly onto a mucosal surface or conjunctivae of one of the dental team without necessarily having close contact. If an aerosol generating procedure (AGP) is being undertaken then airborne precautions are required in addition to contact and droplet precautions.

Hand Hygiene and Respiratory Hygiene • For staff, hand washing must be performed immediately before every episode of direct patient care and after any activity or contact that potentially results in hands becoming contaminated, including donning (putting on) and doffing (removing) PPE, equipment decontamination, and waste handling. Hand washing should be extended to include both forearms. Wash the forearms first and then wash the hands. • Respiratory and cough hygiene should be observed by staff, patients and visitors. Disposable tissues should be available and used to cover the nose and mouth when sneezing, coughing or wiping and blowing the nose – ‘Catch it, bin it, kill it’.
Uniforms and Workwear • Staff and clinicians should attend the practice in their own clothes and get changed into clinical clothes and shoes at work. This should be a different area to those used for donning on and doffing off PPE. • Uniforms and workwear should be transported home in a disposable plastic bag or cloth bag/pillow case. The plastic bag should be disposed of into the household waste. Uniforms and workwear should be laundered: separately from other household linen, in a load not more than half the machine capacity and at the maximum temperature the fabric can tolerate, then ironed or tumbled-dried.
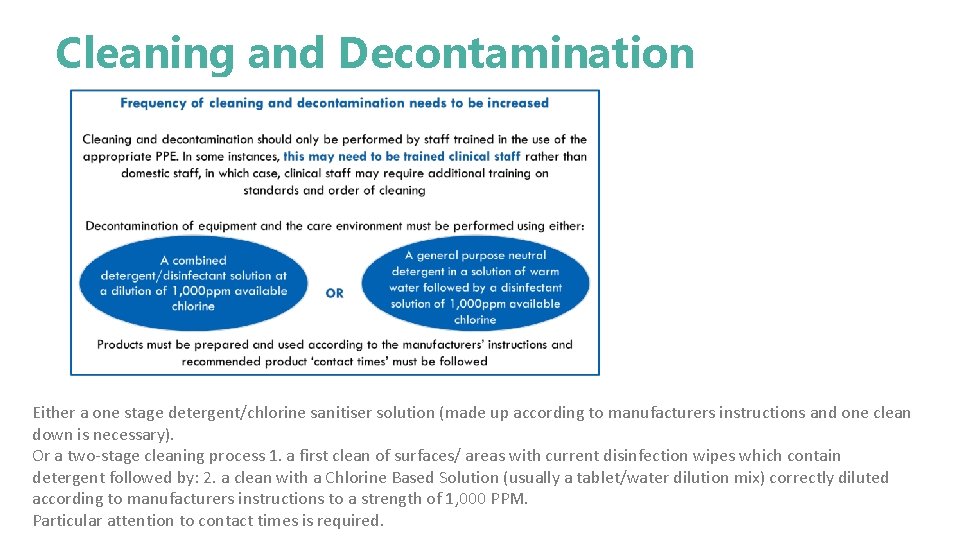
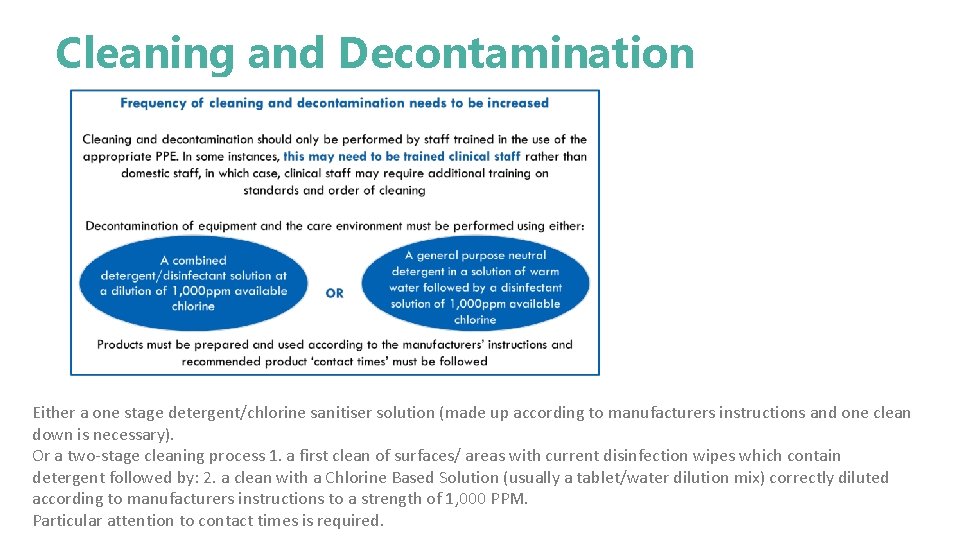
Cleaning and Decontamination Either a one stage detergent/chlorine sanitiser solution (made up according to manufacturers instructions and one clean down is necessary). Or a two-stage cleaning process 1. a first clean of surfaces/ areas with current disinfection wipes which contain detergent followed by: 2. a clean with a Chlorine Based Solution (usually a tablet/water dilution mix) correctly diluted according to manufacturers instructions to a strength of 1, 000 PPM. Particular attention to contact times is required.
• In addition to your routine surgery infection control cleaning procedures thorough cleaning between each patient should be carried out as per the infection control policy cleaning from highest surface to the lowest surface • Any clutter and non essential items should be removed and surfaces kept clean • Social distancing should be maintained including in non clinical areas. Where 2 m can’t be adhered to additional measures should be adopted.
CQC Inspections following Covid-19 • Transformation management assessment TMA to be new CQC measurement. • Most will to be done remotely via a teams/zoom type meeting and then will visit practice for a shorter period.