Clinical Validation A Denials Perspective Kathy Shumpert RN

- Slides: 33
Clinical Validation: A Denials Perspective Kathy Shumpert, RN, MSN, CCDS
Objectives 1) Need for organizational clinical markers 2) Importance of semantics in the physician documentation 3) Common clinical validation denials
What is Clinical Validation, Why do We Do What We Do? It has implications for diagnostic documentation, coding, claims submission, payer review, audits and denials, recovery audit programs, regulatory compliance, and sanctions, and it sometimes raises concerns about false claims, with potential legal consequences (Pinson, 2016) The Official Coding Guidelines doesn't just apply to coders but has legal and regulatory status for all clinicians engaged in health care transactions (Pinson, 2016) If clinicians do not consider the clinical validity of diagnoses for the codes submitted on claims, they will not be in compliance with CMS regulations and policy, will be potentially exposed to claims denials, may be subject to regulatory inquiry and sanctions, and in rare circumstances may be vulnerable to serious allegations of submitting false claims (Pinson, 2016)
Clinical criteria and code assignment ICD-10 -CM/PCS Coding Clinic, Fourth Quarter ICD-10 2016 Pages: 147 -149 The guideline noted addresses coding, not clinical validation. It is appropriate for facilities to ensure that documentation is complete, accurate, and appropriately reflects the patient's clinical conditions. Although ultimately related to the accuracy of the coding, clinical validation is a separate function from the coding process and clinical skill. The distinction is described in the Centers for Medicare & Medicaid (CMS) definition of clinical validation from the Recovery Audit Contractors Scope of Work document and cited in the AHIMA Practice Brief ("Clinical Validation: The Next Level of CDI") published in the August issue of JAHIMA: "Clinical validation is an additional process that may be performed along with DRG validation. Clinical validation involves a clinical review of the case to see whether or not the patient truly possesses the conditions that were documented in the medical record. Clinical validation is performed by a clinician (RN, CMD, or therapist). Clinical validation is beyond the scope of DRG (coding) validation, and the skills of a certified coder. This type of review can only be performed by a clinician or may be performed by a clinician with approved coding credentials. "
Use of Coding Clinic as clinical criteria for code assignment ICD-9 -CM Coding Clinic, Third Quarter 2008 Page: 16 Background material published in Coding Clinic cannot be used as clinical criteria for code assignment. As stated in Coding Clinic, Second Quarter 1998, pages 4 -5: "Any clinical information published in Coding Clinic, is provided as background material to aid the coder's understanding of disease processes. The information is intended to provide the coder with "clues" to identify possible gaps in documentation where additional physician query may be necessary. It is not intended to replace the need for specific physician documentation to substantiate code assignment
Clinical Validation Denials Diagnosis with uncertain or emerging clinical guidelines Single CC/MCC Empiric treatment Inconsistent documentation Copy and paste Absence of clinical indicators with lack of additional supporting documentation Absence of documented manifestation and etiology
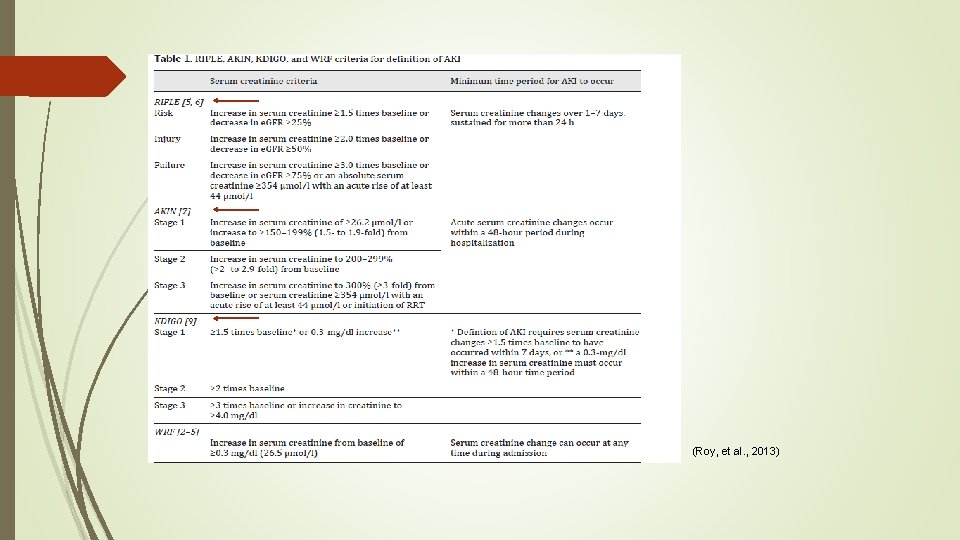
Acute Kidney Injury Reviewers equated AKI and ARF as synonyms One creatinine measurement Is there a baseline creatinine? How do you demonstrate a CC without monitoring? I&O Nursing Measure for AKI What is the etiology?
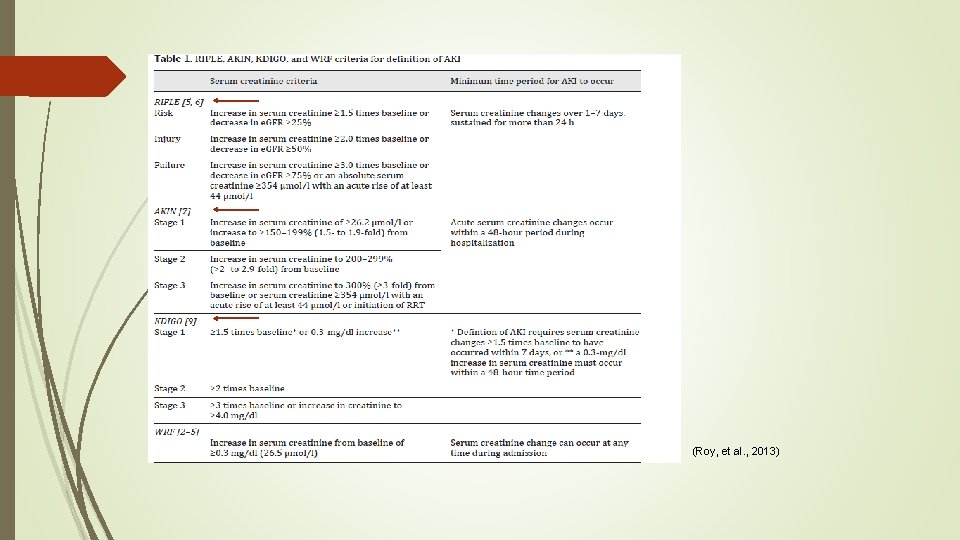
(Roy, et al. , 2013)
Acute Tubular Necrosis Hypotension IV Contrast Sepsis Major Surgery Shock Rhabdomyolysis with myoglobinuria Drugs (NSAIDS) and toxins (2017 CDI Pocket Guide, 2017) Are you validating these conditions as well?
Meets AKI criteria Expected to take more than 72 hours for renal function to return toward baseline following IV fluid resuscitation Urine chemistries Urine sodium > 40 m. Eq/L Fractional excretion of sodium (FENa) > 2% Fractional excretion of urea (FEUrea) 50 -65% for patients on diuretics Urinalysis muddy brown, granular casts Absent in 20 -30% of patients with ATN (2017 CDI Pocket Guide, 2017)
Encephalopathy Reviewers commonly state AMS inherent to a condition If inherent, should the AMS have been resolved? Physical examination There may be fluctuation! Nursing assessment GCS Pre-existing dementia Baseline mentation? High risk for encephalopathy Is it delirium? Etiology and manifestation
Encephalopathy Case Scenario # 1 Presented to ED from Urgent Care due to reported confusion Patient alert and oriented well enough for interview ED ROS is completed. ED Physical examination: alert & oriented x 4 H&P HPI completed with patient interview “alert, awake, oriented” ROS is completed Physical Exam Alert, oriented to person, place and time.
Assessment Toxic metabolic encephalopathy/confusion likely from infectious process likely PNA Does encephalopathy/confusion mean encephalopathy and confusion, encephalopathy versus confusion, or encephalopathy manifested as confusion? Discharge summary hospital course “This is an 80 -year-old male with a past medical history of CAD, CKD– 3, hypothyroidism, hyperlipidemia, hypertension who was sent to this facility from urgent care because of confusion. During this conversation the patient is appropriate, answers questions appropriately, follows simple requests”. Key Points Clarify encephalopathy/confusion. It is not clear if these are comparative or contrasting diagnoses The confusion seems to have resolved prior to arrival to the ED-is the MCC capture appropriate for this scenario? Did the fall with the injury to his forehead contribute?
Encephalopathy Case Scenario #2 This is a case of an 85 year old male who presented with AMS and being combative toward staff and residents in the nursing home. There was a history of diabetes, metabolic acidosis, and dementia. The patient was in acute renal failure with a creatinine > 4. 0/ The AMS was due to delirium from the medical condition and the code for encephalopathy is not justified Progress Note: AMS/Combativeness-likely secondary to sundowning from dementia. Discharge Summary: Brought back from rehab facility with AMS, combativeness and being aggressive toward staff. Patient is still having sundowning with dementia
Sundown syndrome ICD-9 -CM Coding Clinic, Third Quarter 2003 Page: 19 to 20 Effective with discharges: November 1, 2003 Sundown syndrome or sundowning is a phenomenon by which a person with dementia may become more confused, restless, combative, suspicious, upset or disoriented, especially at night. The person may even see, hear or believe things that aren't real. No one is sure what causes sundowning, although it seems to result from brain disease. Assign a code for the specific brain disease (i. e. , Alzheimer's, dementia, etc. ). Do not assign a separate code for sundowning.
Heart Failure Exacerbation of symptoms, i. e. dyspnea at rest or with exertion, orthopnea, nocturnal dyspnea, fatigue, edema IV diuretics Supplemental oxygen Pulmonary edema, congestion, or increasing (or new) pleural effusion BNP > 500 or Pro-BNP > 3, 000 (if no renal impairment) Daily weights? Physical therapy Decreased function or endurance? (2017 CDI Pocket Guide, 2017)
Malnutrition Nutritional Consult Trigger Supplementation Calorie counts Aggressive treatment (for severe malnutrition) Physical examination Emaciation Cachexia Muscle/adipose wasting (temporal wasting, thenar atrophy) Monitor intake (2017 CDI Pocket Guide, 2017)
Malnutrition Documented weight loss BMI Diminished functional status Hand grip strength PT/OT Edema Causation? What is the discharge plan? “A multidisciplinary team approach is recommended for patient assessment and might include a speech therapist, dietitian, physical therapist, occupational therapist, and social worker” Agarwal 2016 Failure to Thrive in Elderly Adults: Evaluation Up. To. Date
Malnutrition Case Scenario Denial letter The clinical evidence in the medical record did not support assignment of E 43. It was noted that the physician documented severe protein calorie malnutrition in the progress note. While it is recognized that this patient’s underlying medical condition placed them at risk for malnutrition, the patient was not severely malnourished. According to consensus criteria, severe malnutrition is defined by BMI <16, clinically significant weight loss, and the characteristic clinical signs. In addition, secondary conditions must be addressed by the treating physicians with a plan of management. The patient’s BMI was 17. 36, confirmed weight loss over the last 3 months, no muscle wasting or loss of subcutaneous fat documented.
History & Physical HPI Patient states loss of weight over the past 3 months states she used to weigh 120 pounds and now current weighs 98 -99 pounds, has decreased appetite and has to force herself to eat ROS Constitutional: + weight loss General: Alert, in no acute distress Physical Examination: General: Alert, no acute cardiopulmonary distress GI: Abdomen soft, non-tender, non-distended Normal bowel sounds Skin No rashes, lesions, petechiae, or purpura. No edema Musculoskeletal: No cyanosis or clubbing, no gross deformities, Normal range of motion
Progress Note Subjective Diarrhea better. Informed pt. of her labs, Talked to daughter at length. She is unable to care for patient as she works and patient has had recent multiple hospitalizations Physical Exam: General: Alert, in no acute cardiopulmonary distress A/P: Malnutrition (Severe)
Nutritional Consult Current Nutrition: Regular Referral for BMI 17. 38. Spoke to daughter at bedside. States patient has had difficulty maintaining weight over the past few months with ongoing gradual weight loss. Says patient is eating about 45% of breakfast which she says is her usual intake. Agreeable to Ensure. Monitor/Evaluation: Follow-up 7 days Nutritional Goal 1: Consumes at least 75% of meals/supplements

PT Evaluation: Pt seen for PT eval. Pt ambulated with no AD 150 ft x 2. She had no LOB with activity. She was able to complete balance activities independently-feet together, turn over each shoulder, pick an object off the ground etc. Discharge Summary: Follow-Up/Discharge Instructions PCP No, in 10 days Side note: Discharged to home. Did not meet criteria for SNF. Sent back home with daughter. Daughter had expressed concern that her mother was alone 10+ hours/day and she didn’t feel it was safe for the patient to go home. “Per daughter, patient is on a fixed income” Daughter has limited finances as well
Sepsis Case Scenario Severe sepsis Placed in observation initially *Conflicts with the severity of the severe sepsis* “Observation care is a well-defined set of specific, clinically appropriate services, which include ongoing short term treatment, assessment, and reassessment before a decision can be made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital ” Medicare Benefit Policy Manual Chapter 6, 20. 6
Pneumonia and Sepsis Limjoco, C. 2006.
Pneumonia Symptoms Fever Chills Cough Sputum Dyspnea Pleuritic chest pain Physical Examination Rales, rhonchi, bronchial breath sounds, dullness, pleural rubs, chest wall splitting WBC may be low, normal, or elevated (2017 CDI Pocket Guide, 2017)
Acute Respiratory Failure Symptoms Use of accessory muscles Dyspnea Nasal flaring Tachypnea Intercostal retractions Respiratory distress Cyanosis Labored breathing Lethargy Wheezing Grunting Stridor (2017 CDI Pocket Guide, 2017)
Acute Respiratory Failure What does nursing and respiratory therapy documentation reflect? Assist with ADLs? Assistance with ambulation? Is the patient consuming meals without difficulty? Physical therapy Decreased endurance? Decreased functional status? Refusing therapy? Causation *Oxygen increased markedly without any documentation of decompensation or desaturation* 96% on room air, no documented respiratory distress, 99% on 15 liters
Acute Respiratory Failure Case Scenario COPD with home oxygen presents with COPD exacerbation and hypoxia ABG p. H 7. 43, p. CO 2 34. 8, p. O 2 54, 3 liters O 2 In COPD typically a 10 -15 mm. Hg drop in in p. O 2 or a p. CO 2> 50 with p. H<7. 3 Confliction in documentation of home oxygen, ED physician noted home O 2, pulmonology documented no home O 2 ABG obtained 2 days after admission, appears that the patient was having bronchospasms with episodes of hypoxia Oxygen was titrated from 5 liters down to 2. 5 liters without an order for oxygen. Oxygen is not considered a nursing comfort measure and a protocol for oxygen must be signed and ordered within the medical record. This is a common Joint Commission target for nursing
Acute Respiratory Failure Case Scenario Admitted for cellulitis Uses home O 2 at 2 -3 liters. On 2 -3 liters while hospitalized Pulmonologist documented, “Asked by family and pt. to continue to monitor pt. while in the hospital No other documented reason for consultation Increased to 5 liters overnight without documentation of hypoxemia. Was supposed to have CPAP as at home, but CPAP was not documented No exacerbation of COPD or CHF, no acute pulmonary condition documented
Acute on Chronic Diastolic Heart Failure Echo (initial hand written note) “LV function preserved, LV diastolic dysfunction E-A reversal” Dictated Echo report “LV function is normal 60 -65%. LV thickness is normal. Mild mitral regurgitation. Rest of this study is normal. 4 day stay. Patient weighed on admission and following day. No Daily weights Urine output inconsistently measured. Accurate I&O incomplete
Documentation Conundrums Confliction between providers regarding acute or chronic conditions AKI or CKD CHF Compensated, normal exam Decompensated “He appears to have decompensated recently but I do not think his issues are of recent onset”. Sepsis due to bacteremia Blood culture contaminated Documentation of conditions continue through the medical record without resolution i. e. Patient septic on day of discharge *copy/paste* PDx with monitoring and limited tx Symptoms can be explained by another diagnosis