Challenges on Referrals A case study of Misdiagnosed

- Slides: 22
Challenges on Referrals: A case study of Misdiagnosed Ruptured Uterus PRESENTER: DR MATOVELO DISMAS BMC/CUHAS 2016
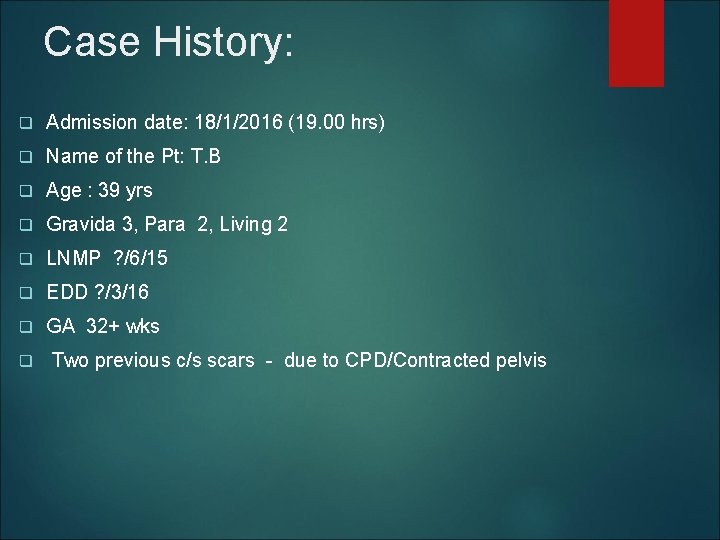
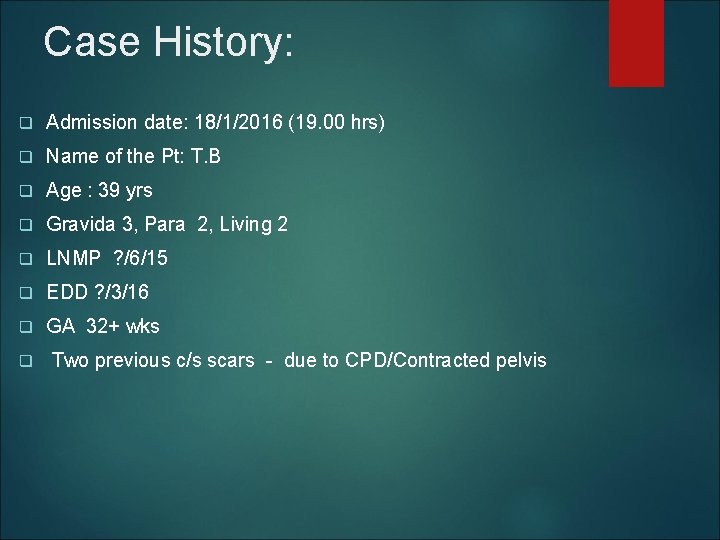
Case History: q Admission date: 18/1/2016 (19. 00 hrs) q Name of the Pt: T. B q Age : 39 yrs q Gravida 3, Para 2, Living 2 q LNMP ? /6/15 q EDD ? /3/16 q GA 32+ wks q Two previous c/s scars - due to CPD/Contracted pelvis
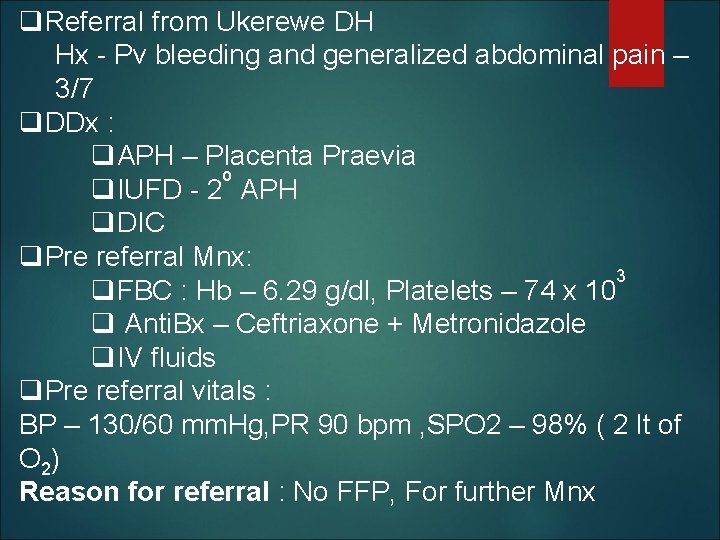
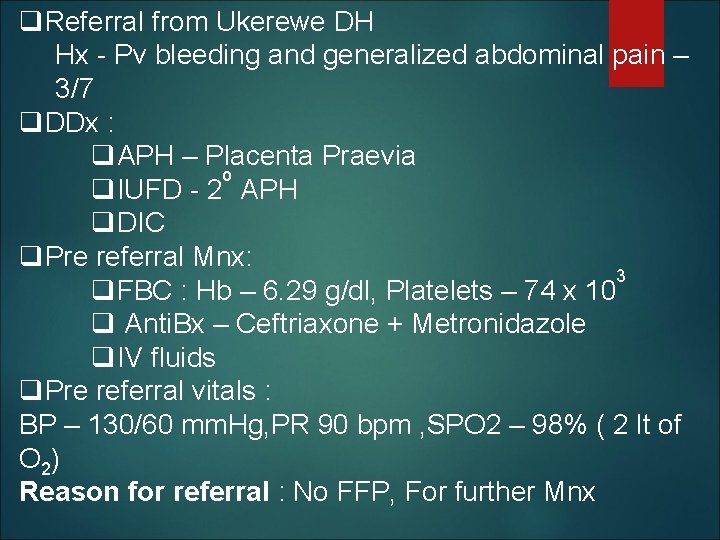
q. Referral from Ukerewe DH Hx - Pv bleeding and generalized abdominal pain – 3/7 q. DDx : q. APH – Placenta Praevia o q. IUFD - 2 APH q. DIC q. Pre referral Mnx: 3 q. FBC : Hb – 6. 29 g/dl, Platelets – 74 x 10 q Anti. Bx – Ceftriaxone + Metronidazole q. IV fluids q. Pre referral vitals : BP – 130/60 mm. Hg, PR 90 bpm , SPO 2 – 98% ( 2 lt of O 2) Reason for referral : No FFP, For further Mnx
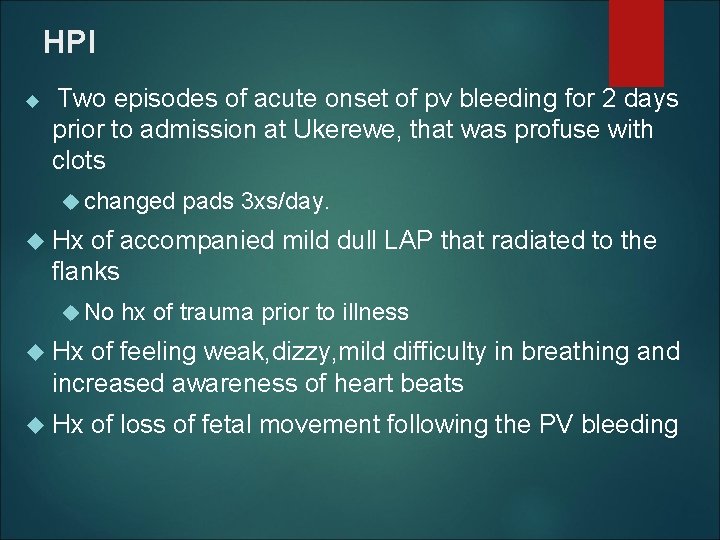
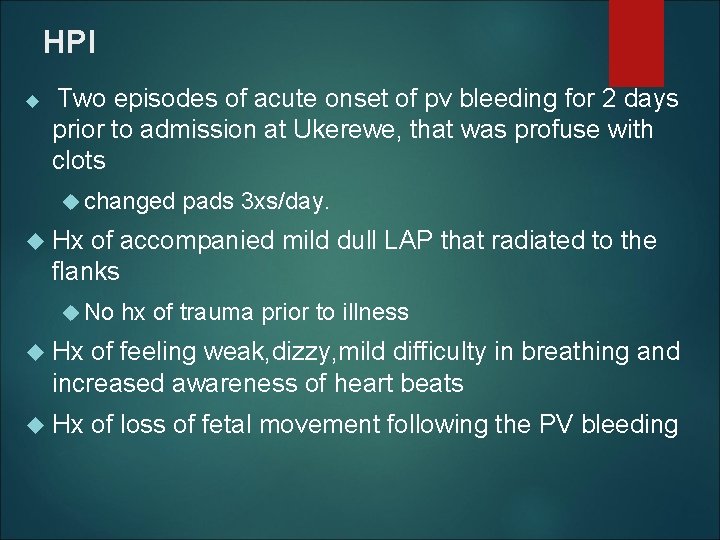
HPI Two episodes of acute onset of pv bleeding for 2 days prior to admission at Ukerewe, that was profuse with clots changed pads 3 xs/day. Hx of accompanied mild dull LAP that radiated to the flanks No hx of trauma prior to illness Hx of feeling weak, dizzy, mild difficulty in breathing and increased awareness of heart beats Hx of loss of fetal movement following the PV bleeding
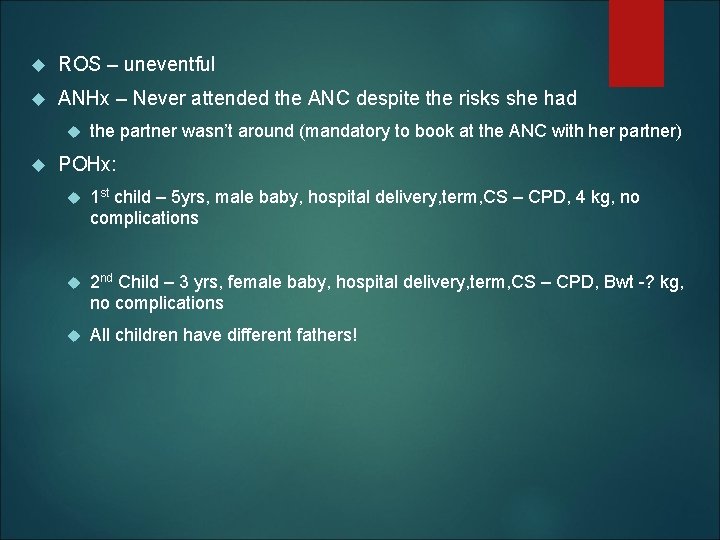
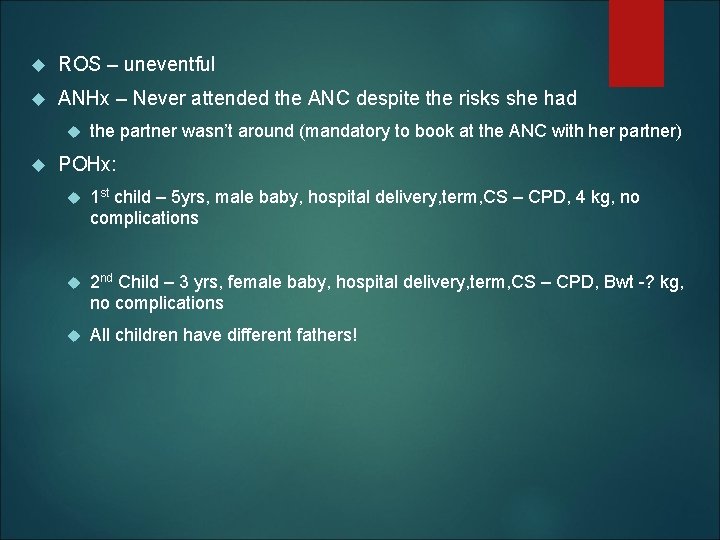
ROS – uneventful ANHx – Never attended the ANC despite the risks she had the partner wasn’t around (mandatory to book at the ANC with her partner) POHx: 1 st child – 5 yrs, male baby, hospital delivery, term, CS – CPD, 4 kg, no complications 2 nd Child – 3 yrs, female baby, hospital delivery, term, CS – CPD, Bwt -? kg, no complications All children have different fathers!

GHx: MHx - ? /28/5, normal flow, 2 pads/day No hx of contraception PMHx – Uneventful No hx of bleeding tendencies on trivial injury FSHx Single parent, with multiple partners, peasant, Ø alcohol, Ø smoking, Ø chronic illness in her family.
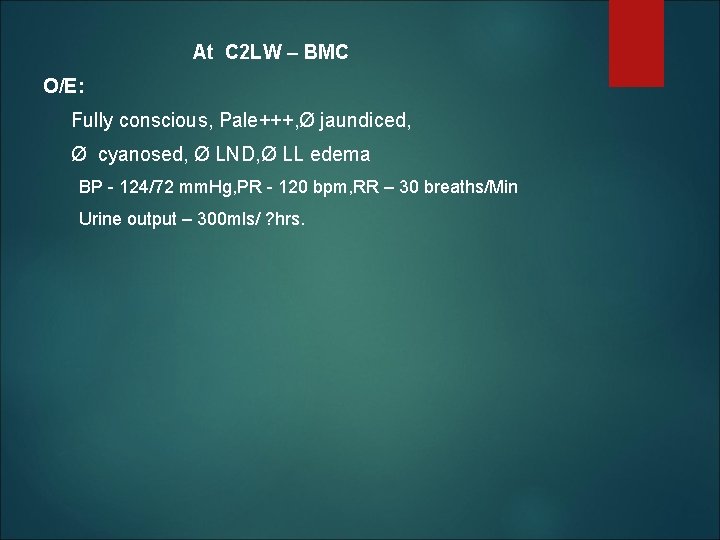
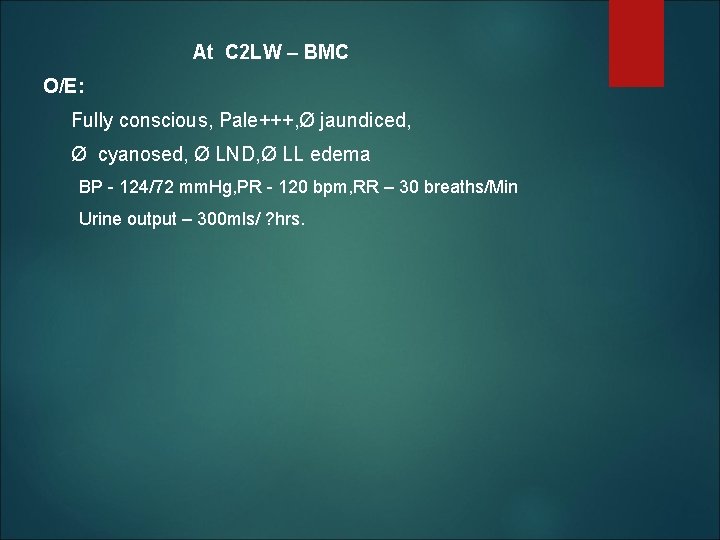
At C 2 LW – BMC O/E: Fully conscious, Pale+++, Ø jaundiced, Ø cyanosed, Ø LND, Ø LL edema BP - 124/72 mm. Hg, PR - 120 bpm, RR – 30 breaths/Min Urine output – 300 mls/ ? hrs.
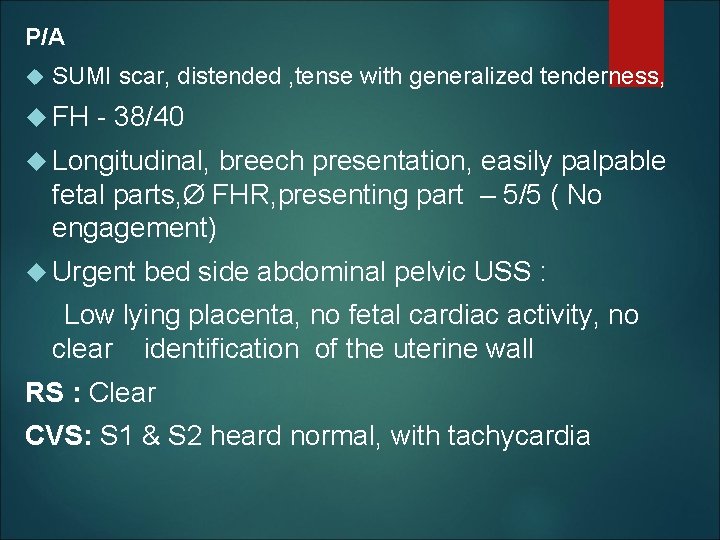
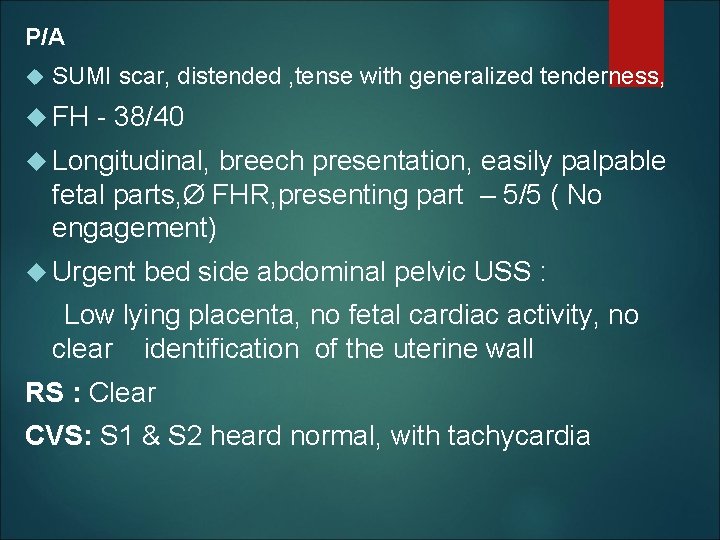
P/A SUMI scar, distended , tense with generalized tenderness, FH - 38/40 Longitudinal, breech presentation, easily palpable fetal parts, Ø FHR, presenting part – 5/5 ( No engagement) Urgent bed side abdominal pelvic USS : Low lying placenta, no fetal cardiac activity, no clear identification of the uterine wall RS : Clear CVS: S 1 & S 2 heard normal, with tachycardia
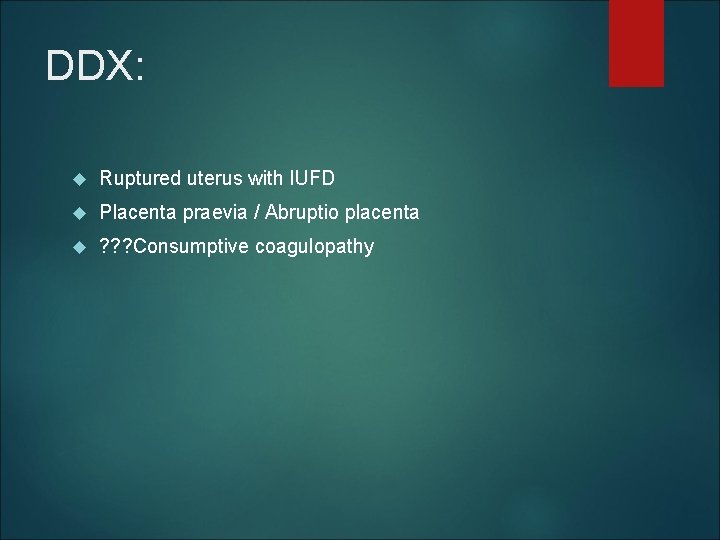
DDX: Ruptured uterus with IUFD Placenta praevia / Abruptio placenta ? ? ? Consumptive coagulopathy
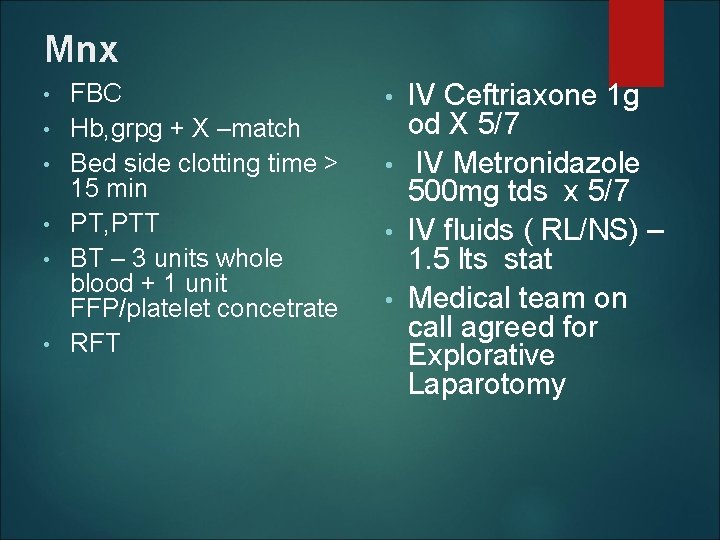
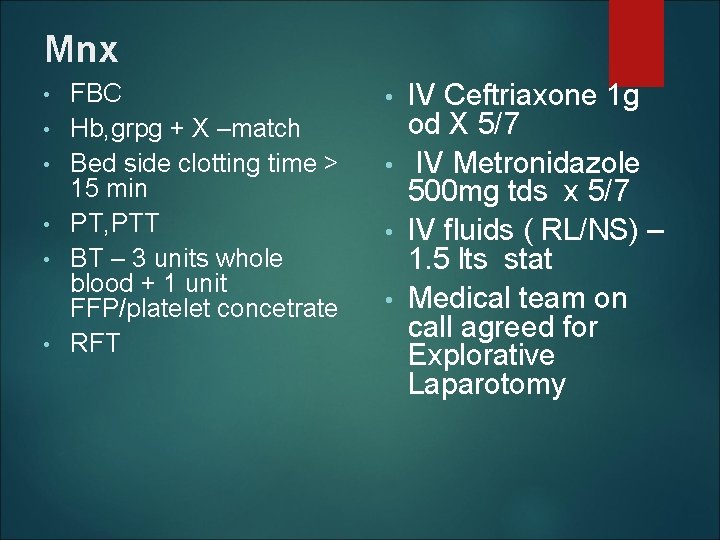
Mnx • • • FBC Hb, grpg + X –match Bed side clotting time > 15 min PT, PTT BT – 3 units whole blood + 1 unit FFP/platelet concetrate RFT IV Ceftriaxone 1 g od X 5/7 • IV Metronidazole 500 mg tds x 5/7 • IV fluids ( RL/NS) – 1. 5 lts stat • Medical team on call agreed for Explorative Laparotomy •
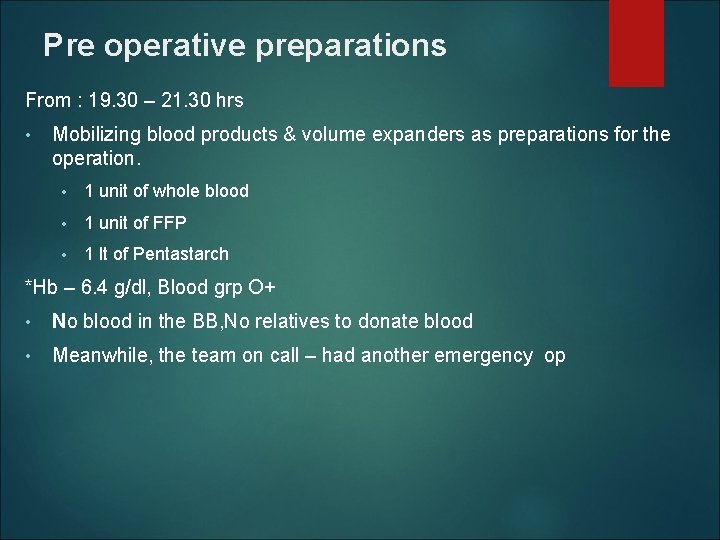
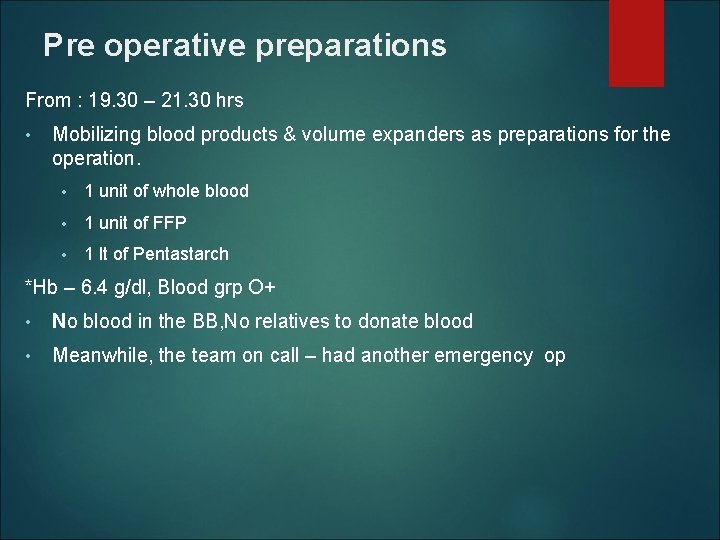
Pre operative preparations From : 19. 30 – 21. 30 hrs • Mobilizing blood products & volume expanders as preparations for the operation. • 1 unit of whole blood • 1 unit of FFP • 1 lt of Pentastarch *Hb – 6. 4 g/dl, Blood grp O+ • No blood in the BB, No relatives to donate blood • Meanwhile, the team on call – had another emergency op
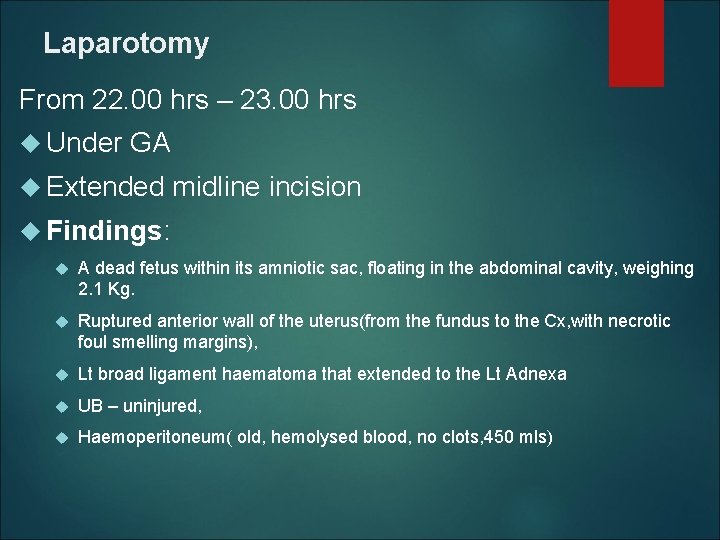
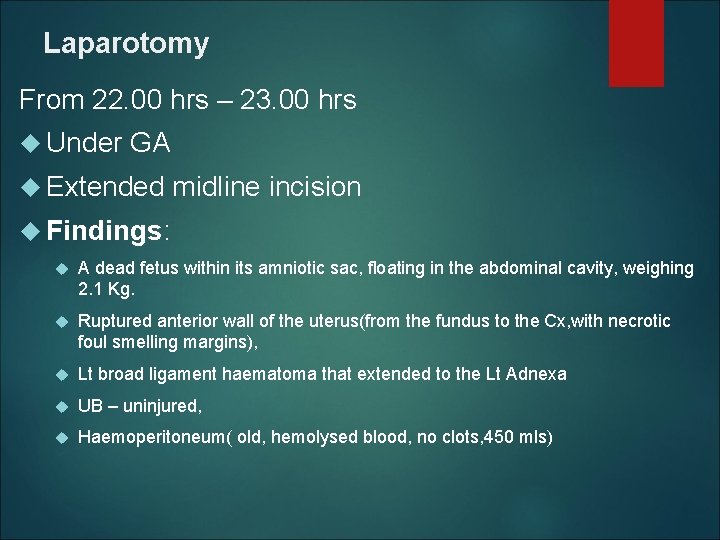
Laparotomy From 22. 00 hrs – 23. 00 hrs Under GA Extended midline incision Findings: A dead fetus within its amniotic sac, floating in the abdominal cavity, weighing 2. 1 Kg. Ruptured anterior wall of the uterus(from the fundus to the Cx, with necrotic foul smelling margins), Lt broad ligament haematoma that extended to the Lt Adnexa UB – uninjured, Haemoperitoneum( old, hemolysed blood, no clots, 450 mls)
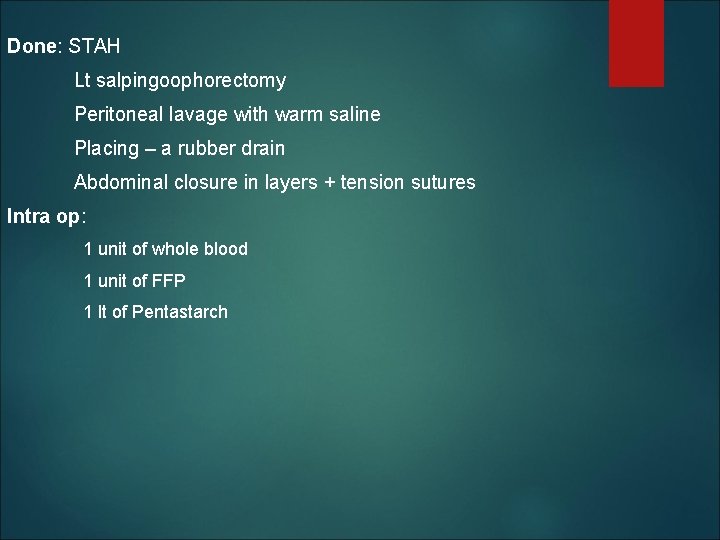
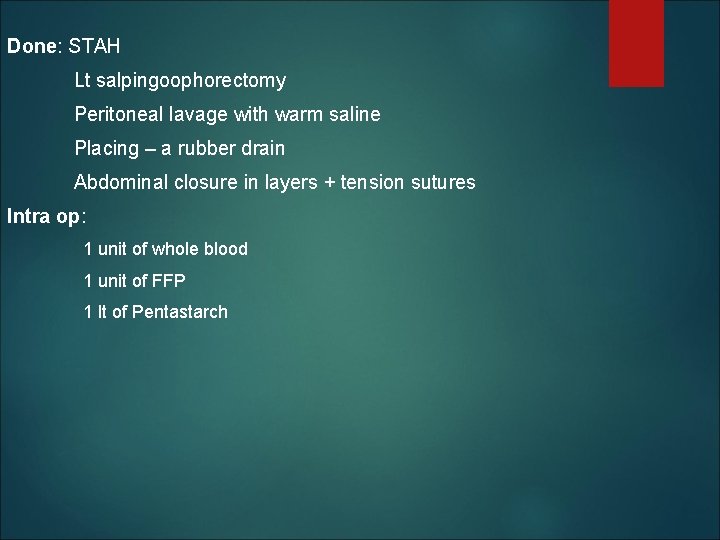
Done: STAH Lt salpingoophorectomy Peritoneal lavage with warm saline Placing – a rubber drain Abdominal closure in layers + tension sutures Intra op: 1 unit of whole blood 1 unit of FFP 1 lt of Pentastarch
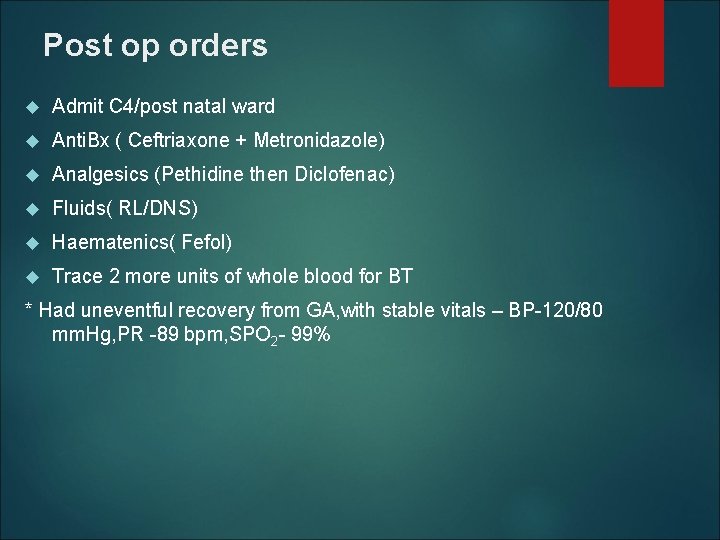
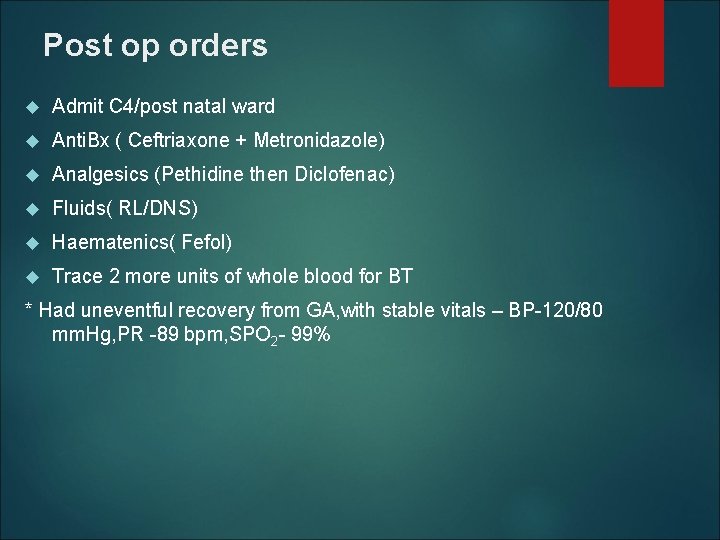
Post op orders Admit C 4/post natal ward Anti. Bx ( Ceftriaxone + Metronidazole) Analgesics (Pethidine then Diclofenac) Fluids( RL/DNS) Haematenics( Fefol) Trace 2 more units of whole blood for BT * Had uneventful recovery from GA, with stable vitals – BP-120/80 mm. Hg, PR -89 bpm, SPO 2 - 99%
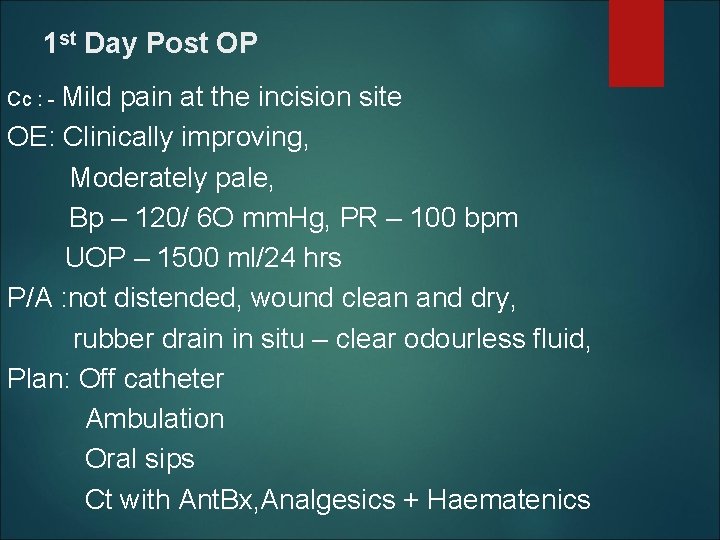
1 st Day Post OP Cc : - Mild pain at the incision site OE: Clinically improving, Moderately pale, Bp – 120/ 6 O mm. Hg, PR – 100 bpm UOP – 1500 ml/24 hrs P/A : not distended, wound clean and dry, rubber drain in situ – clear odourless fluid, Plan: Off catheter Ambulation Oral sips Ct with Ant. Bx, Analgesics + Haematenics
Challenges: No antenatal care services received Single mother All babies with different partners no financial & non-financial support Delay in decision making at home Delayed in accessing health services: bleeding at home for 2 days No individual and Community health seeking behavior
Challenges: Delay in receiving appropriate intervention? ? Diagnosis of Uterine rupture was missed No blood products available Questions to the audience: Time spent to transfer the patient 3 -4 hours? Mode of transport? Was it important for Ukerewe Medical Team to provide initial intervention to the patient and later refer to BMc for advanced care needed?
Challenges: No Pre-referral communication Receiving facility be ready in terms of supplies, equipment's and expertise to avoid delays Will the patient receive care needed What measure should be attempted before referral is made Is this referral cost conscious?
Challenges: For BMC medical Team: Are were prepared enough to handle such cases? Blood products: FFP, Platelets concentrates etc Delay again in receiving appropriate care Mobilization of blood products was a hustle Do we have backup plan in case the team on call is overwhelmed? Cuts across all departments!
Recommendations: This is a “near-miss” maternal death!!!! Regular feedback to referring Centre/Medical team involve Advise on issues pertaining to complication readiness: Blood products Refresh back our clinical skills On job training, attend CMEs & sharing updates on obstetric emergencies approaches to management Case consultations & introduction to e-medicine
Recommendations: Review our approaches to continuum of care: Pregnant mother must attend with their partners to ANC Do we need to be flexible as health workers? For BMC Medical Team: Blood products available do not meet the demand BMC MUST take initiatives to begin its own blood screening lab: any task force formed?
Thanks for Listening COMMENTS?
 Prms referrals
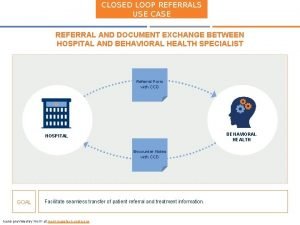
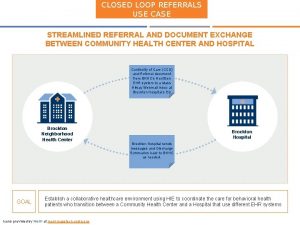
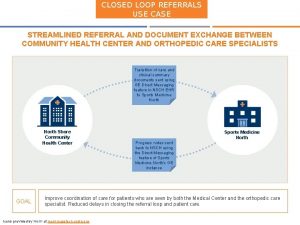
Prms referrals Closed loop referrals
Closed loop referrals What is third party referral in health and social care
What is third party referral in health and social care Best case worst case average case
Best case worst case average case Crm failure case study
Crm failure case study Short case vs long case
Short case vs long case Linear search average performance
Linear search average performance Case western reserve university case school of engineering
Case western reserve university case school of engineering Bubble sort algorithm pseudocode
Bubble sort algorithm pseudocode Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case Ambiguous case of the law of sines
Ambiguous case of the law of sines Zara technology case study
Zara technology case study Sheryl fleisch
Sheryl fleisch Kf motorcycle accident
Kf motorcycle accident Swot analysis of whole foods
Swot analysis of whole foods Action research vs case study
Action research vs case study Volkswagen of america: managing it priorities
Volkswagen of america: managing it priorities Valuation of plant and machinery
Valuation of plant and machinery Mini case study examples
Mini case study examples Starbucks foreign direct investment case study
Starbucks foreign direct investment case study Case study 11
Case study 11 Uml case study
Uml case study