CARTILAGE AND BONE Similarities Living cells embedded in
CARTILAGE AND BONE Similarities • Living cells embedded in a matrix produced by themselves • Cells occupy spaces in the matrix called lacunae • Both develop from mesenchyme • Both are covered by connective tissue Differences • Nutrition of cells • Growth
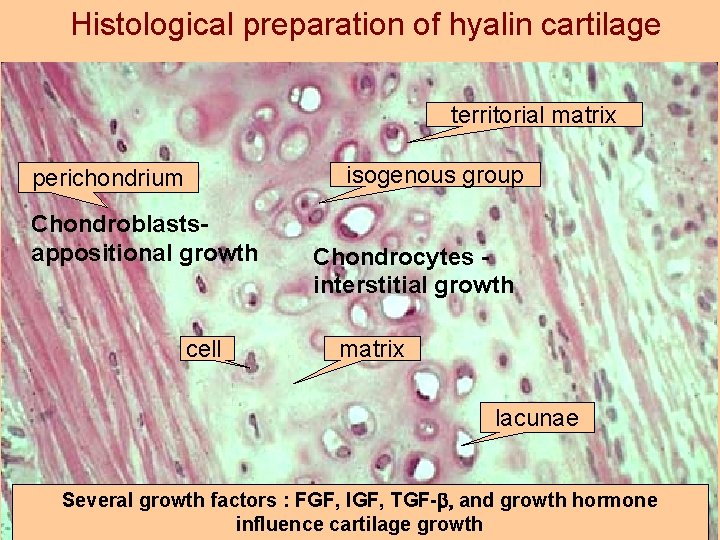
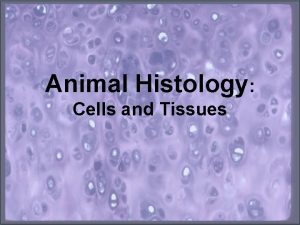
Histological preparation of hyalin cartilage territorial matrix isogenous group perichondrium Chondroblastsappositional growth cell Chondrocytes interstitial growth matrix lacunae Several growth factors : FGF, IGF, TGF-b and growth hormone influence cartilage growth
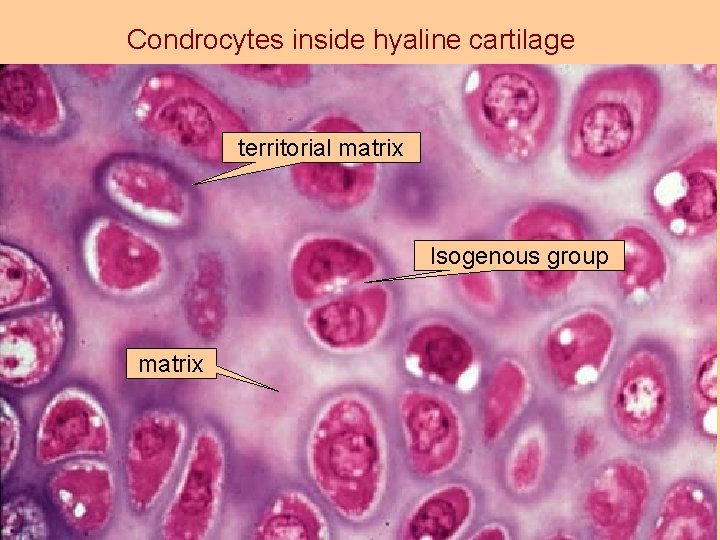
Condrocytes inside hyaline cartilage territorial matrix Isogenous group matrix
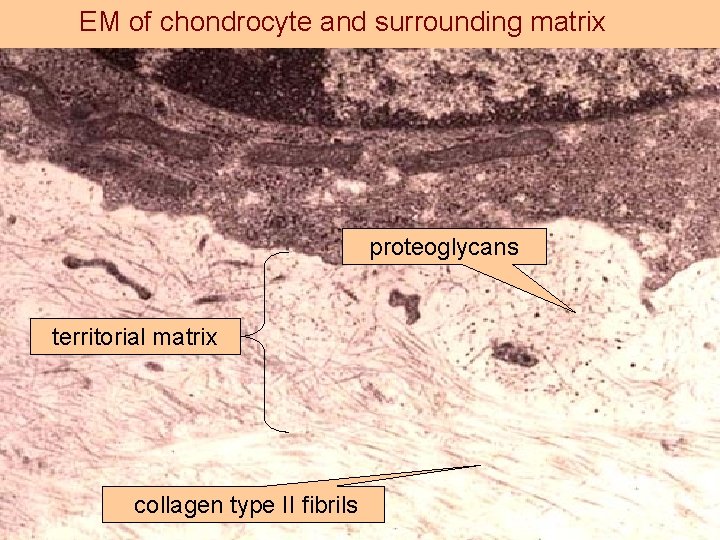
EM of chondrocyte and surrounding matrix proteoglycans territorial matrix collagen type II fibrils
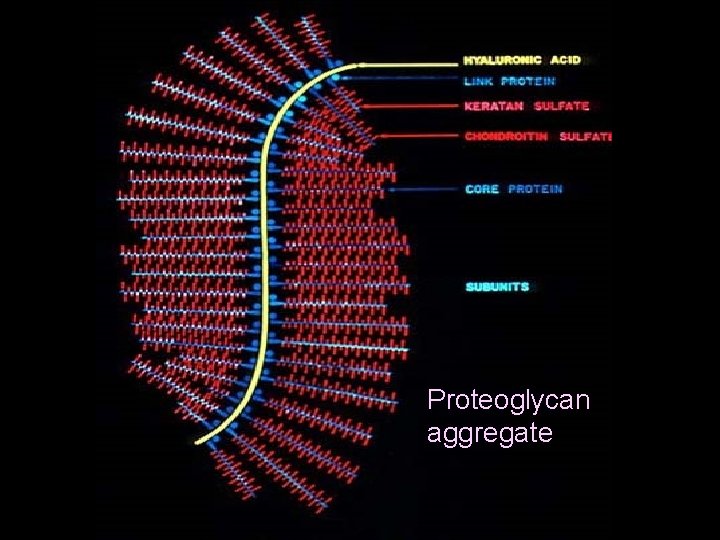
piokl Proteoglycan aggregate
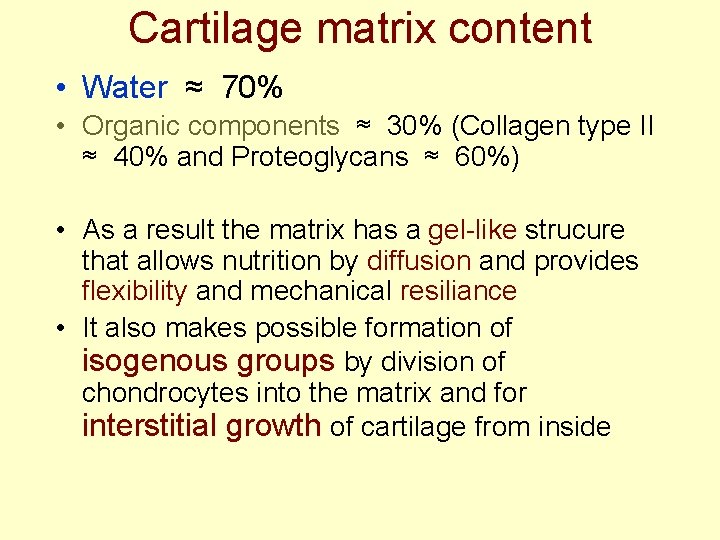
Cartilage matrix content • Water ≈ 70% • Organic components ≈ 30% (Collagen type II ≈ 40% and Proteoglycans ≈ 60%) • As a result the matrix has a gel-like strucure that allows nutrition by diffusion and provides flexibility and mechanical resiliance • It also makes possible formation of isogenous groups by division of chondrocytes into the matrix and for interstitial growth of cartilage from inside
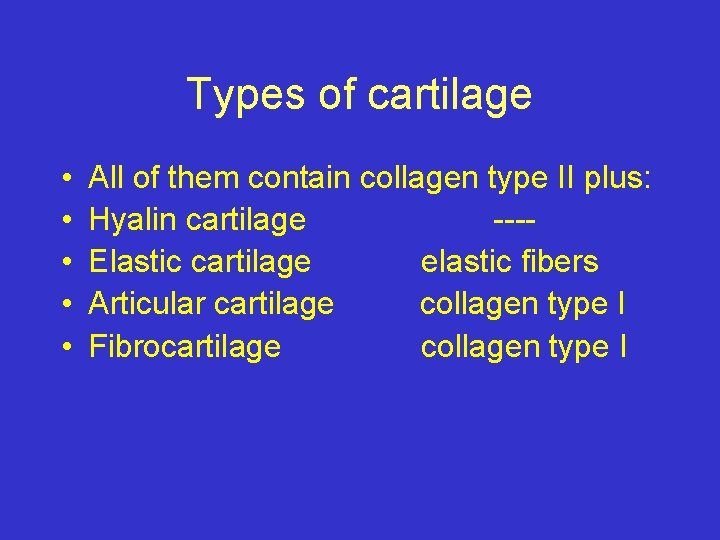
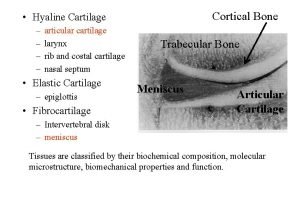
Types of cartilage • • • All of them contain collagen type II plus: Hyalin cartilage ---Elastic cartilage elastic fibers Articular cartilage collagen type I Fibrocartilage collagen type I
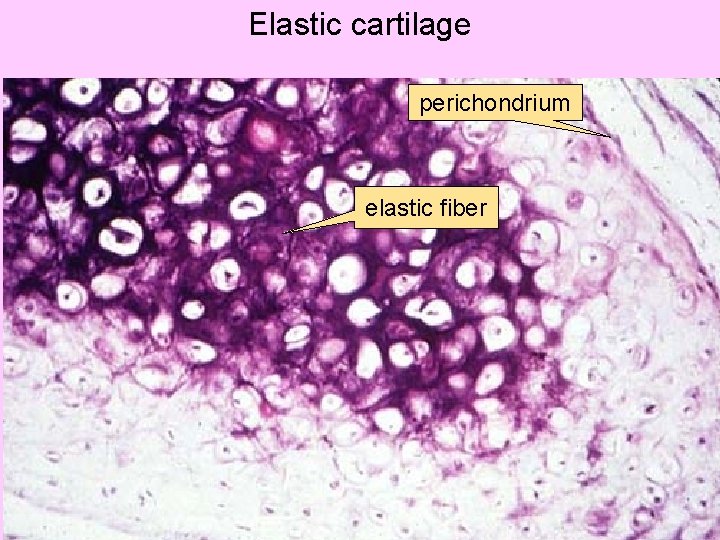
Elastic cartilage perichondrium elastic fiber
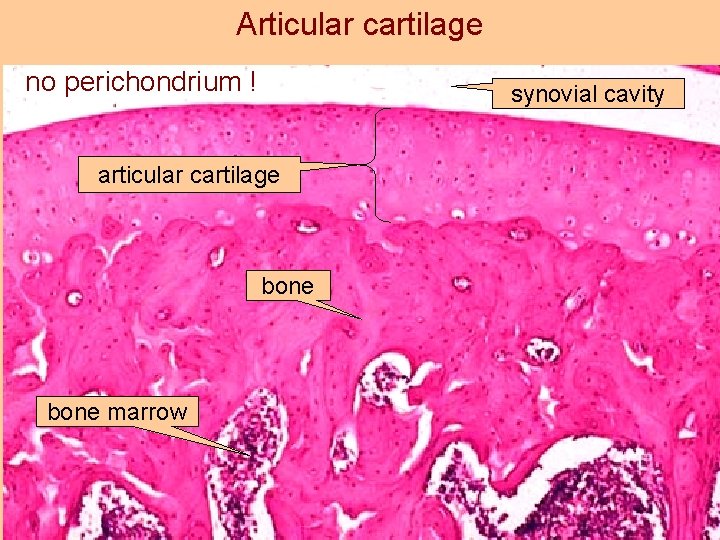
Articular cartilage no perichondrium ! synovial cavity articular cartilage bone marrow
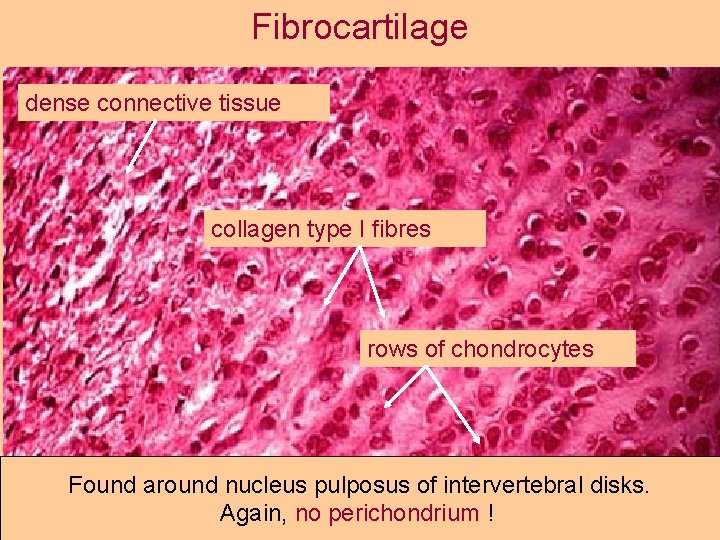
Fibrocartilage dense connective tissue collagen type I fibres rows of chondrocytes Found around nucleus pulposus of intervertebral disks. Again, no perichondrium !
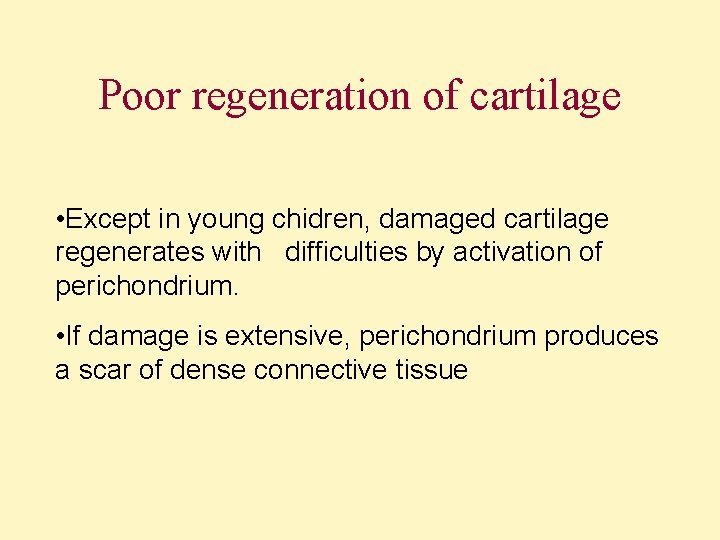
Poor regeneration of cartilage • Except in young chidren, damaged cartilage regenerates with difficulties by activation of perichondrium. • If damage is extensive, perichondrium produces a scar of dense connective tissue
BONE Bone

Bone
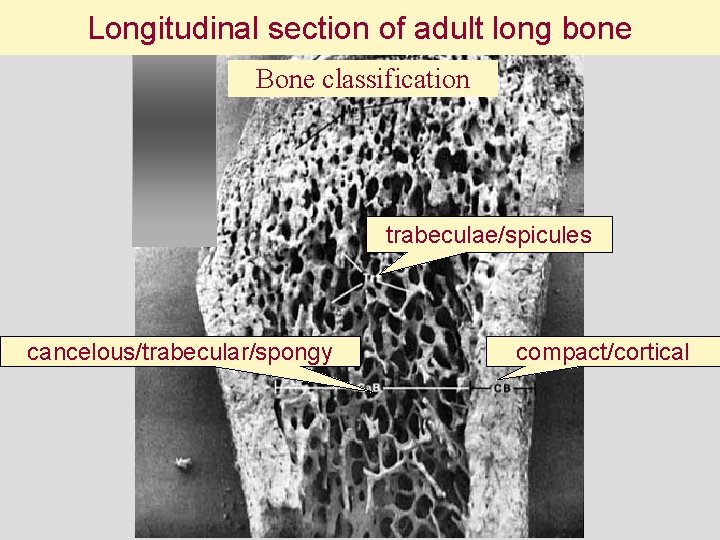
Longitudinal section of adult long bone Bone classification trabeculae/spicules cancelous/trabecular/spongy compact/cortical
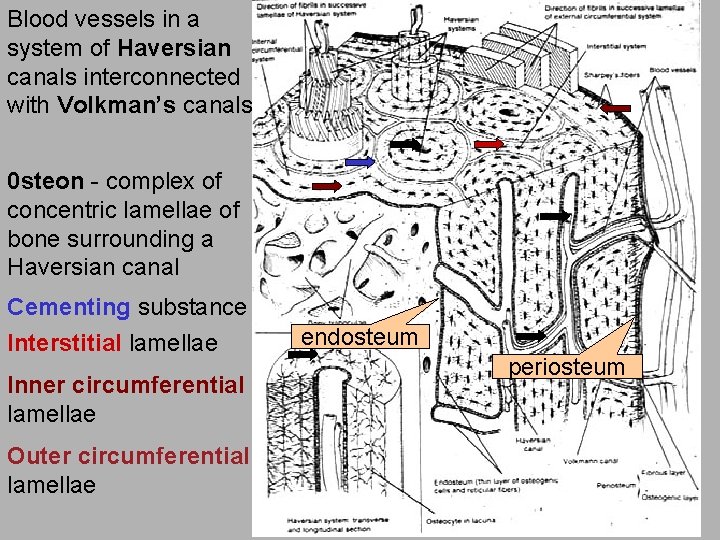
Blood vessels in a system of Haversian canals interconnected with Volkman’s canals 0 steon - complex of concentric lamellae of bone surrounding a Haversian canal Cementing substance Interstitial lamellae Inner circumferential lamellae Outer circumferential lamellae endosteum periosteum

Thin section of calcified bone Osteon with Haversian canal Interstitial lamellae Lacunae of osteocytes Cement line
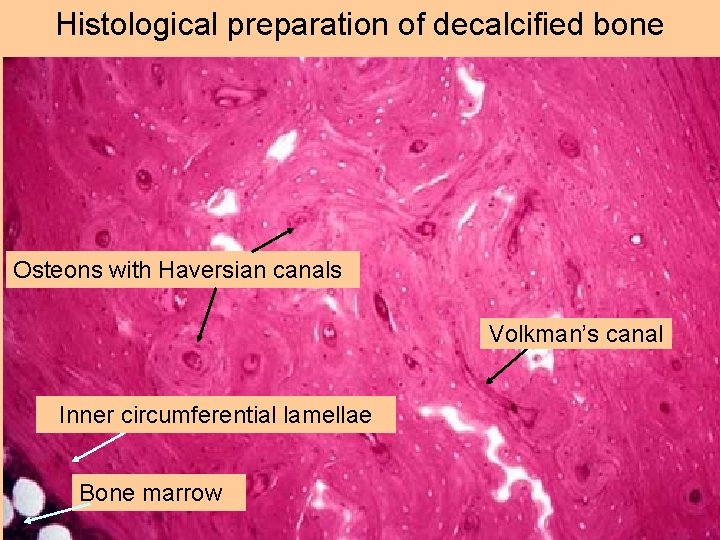
Histological preparation of decalcified bone Osteons with Haversian canals Volkman’s canal Inner circumferential lamellae Bone marrow
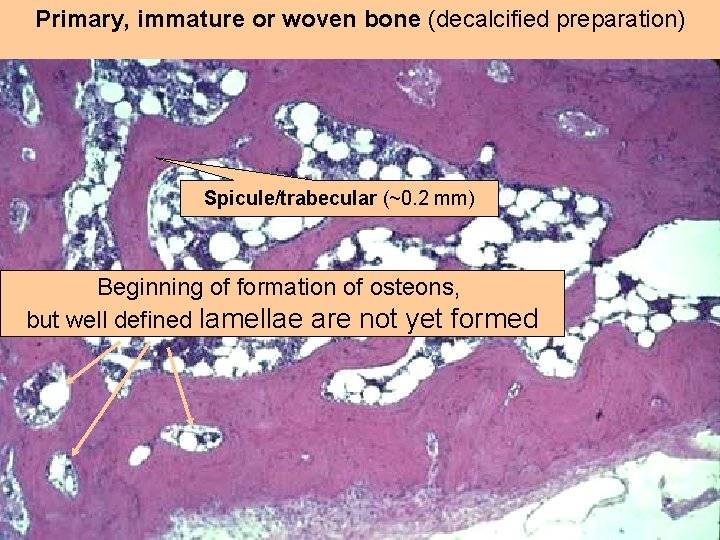
Primary, immature or woven bone (decalcified preparation) Spicule/trabecular (~0. 2 mm) Beginning of formation of osteons, but well defined lamellae are not yet formed

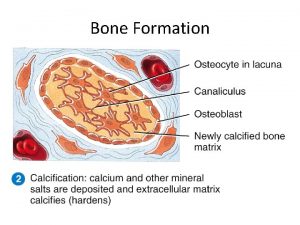
CELLS OF BONE Mesenchymal cells differentiating into osteoblasts Capillary Not calcified bone matrix osteoid Osteocytes in lacunae with their processes interconnected Calcified bone matrix is penetrated by canaliculi

Calcification/mineralization of of bone matrix • Inorganic matter is ≈ 50% of the dry weight of bone matrix mainly in form of hydroxyapatite crystals Ca 10(PO 4)6(OH)2 • Initial mineralization in woven bone or cartilage by matrix vesicles deposited by osteobalsts and chondrocytes and enriched in alkaline phosphatase and acidic phospholipids • Mineralization front - mineralization of matrix synthesized at already calcified mature bone surface • Deficiency of Ca and vitamin D negatively influence normal calcification process

osteocytes canaliculi calcified bone matrix osteoclast blood vessel flat/resting osteoblasts

ruffled border clear/adhesion zone

Howship’s lacunae osteoblasts making new bone
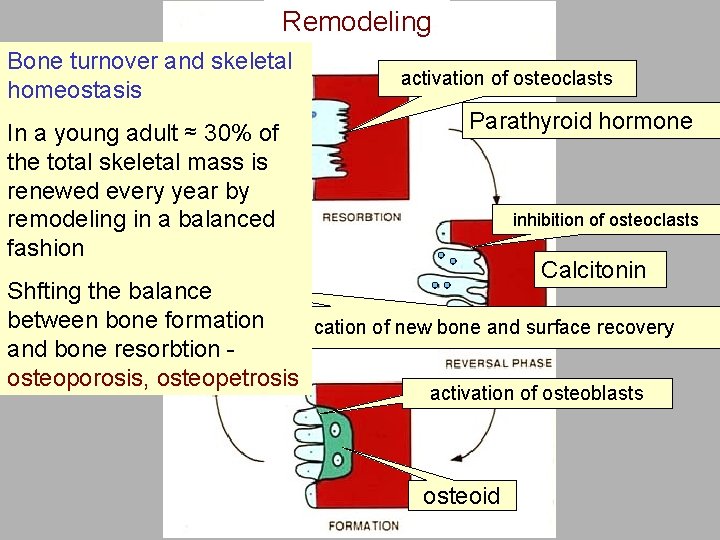
Remodeling Bone turnover and skeletal homeostasis In a young adult ≈ 30% of the total skeletal mass is renewed every year by remodeling in a balanced fashion activation of osteoclasts Parathyroid hormone inhibition of osteoclasts Calcitonin Shfting the balance between bone formation. Calcification of new bone and surface recovery and bone resorbtion osteoporosis, osteopetrosis activation of osteoblasts osteoid
FORMATION OF HAVERSIAN CANAL Activation of osteoclasts Second concentric layer First concentric layer Inhibition of osteoclasts Activation of osteoblasts
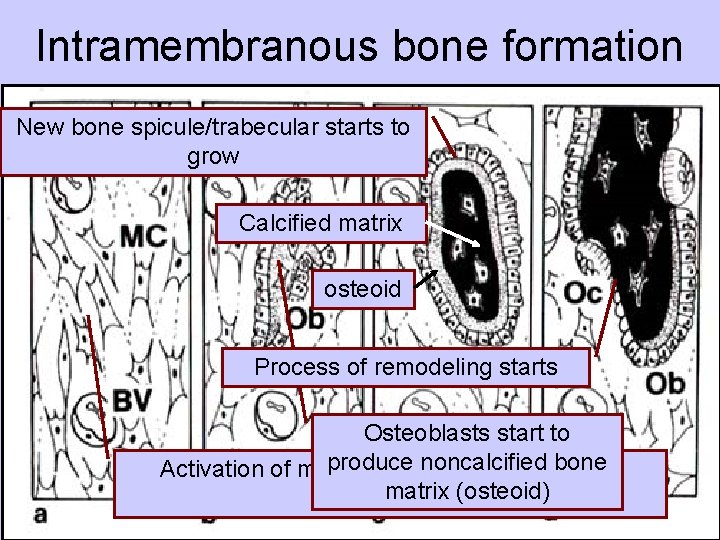
Intramembranous bone formation New bone spicule/trabecular starts to grow Calcified matrix osteoid Process of remodeling starts Osteoblasts start to produce noncalcified bone Activation of mesenchymal cells to turn into matrix (osteoid) osteoblasts
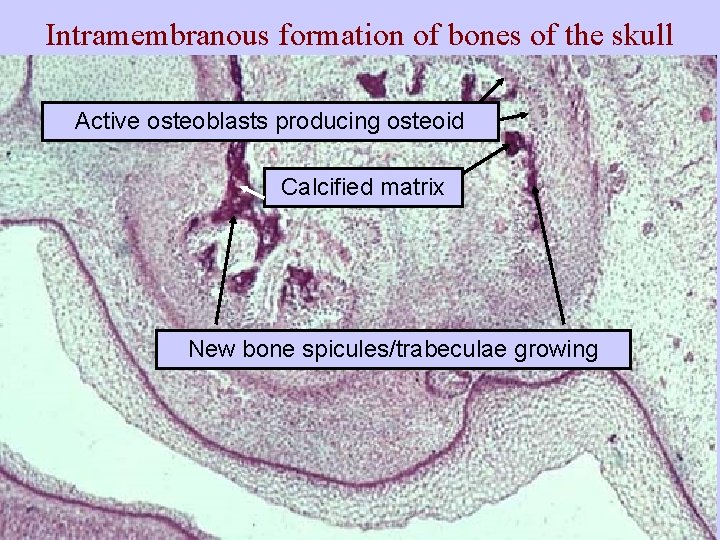
Intramembranous formation of bones of the skull Active osteoblasts producing osteoid Calcified matrix New bone spicules/trabeculae growing
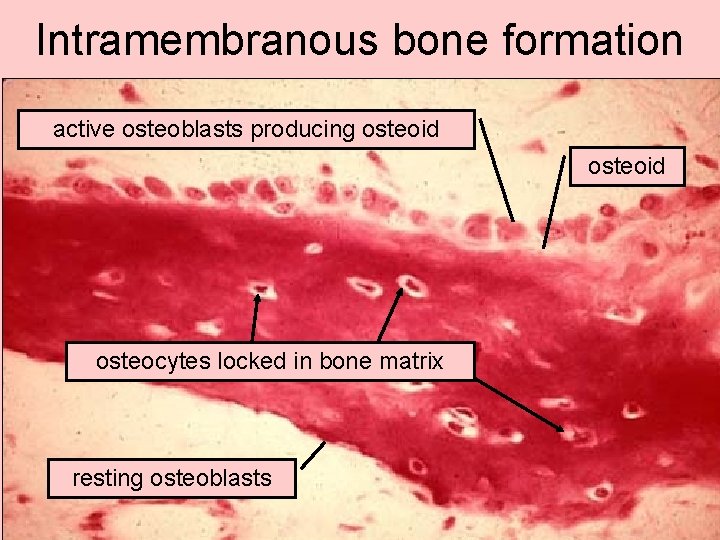
Intramembranous bone formation active osteoblasts producing osteoid osteocytes locked in bone matrix resting osteoblasts
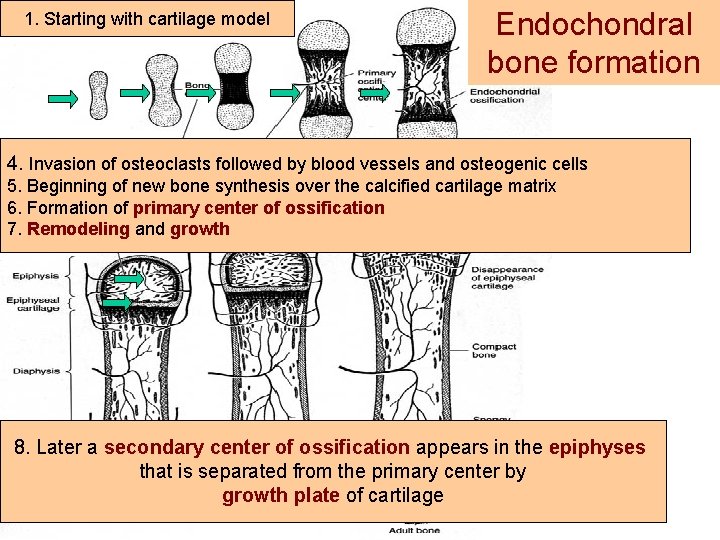
1. Starting with cartilage model Endochondral bone formation 4. 2. Invasion of osteoclasts followed blood vessels and osteogenic cells Formation of bony collar atby the middle of diaphysis 5. Beginning of new bone synthesis over the calcified cartilage matrix 6. Formation of primary center offollowed ossification 3. Hypertrophy of chondrocytes by calcification 7. their Remodeling and growth of marix and their death 8. Later a secondary center of ossification appears in the epiphyses that is separated from the primary center by growth plate of cartilage

Starting with cartilage model Hypertrophy and degeneration of chondrocytes

Bony collar on the surface at the middle of diaphysis formed by intramembranous bone formation Beginning of formation of primary center of ossification
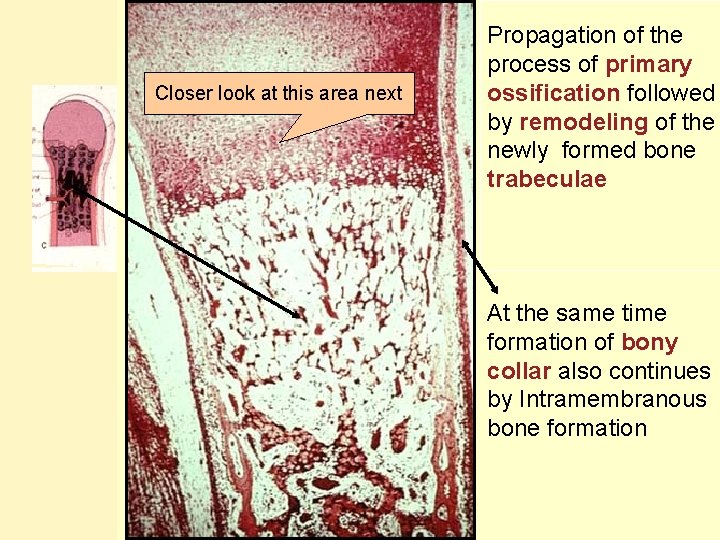
Closer look at this area next Propagation of the process of primary ossification followed by remodeling of the newly formed bone trabeculae At the same time formation of bony collar also continues by Intramembranous bone formation
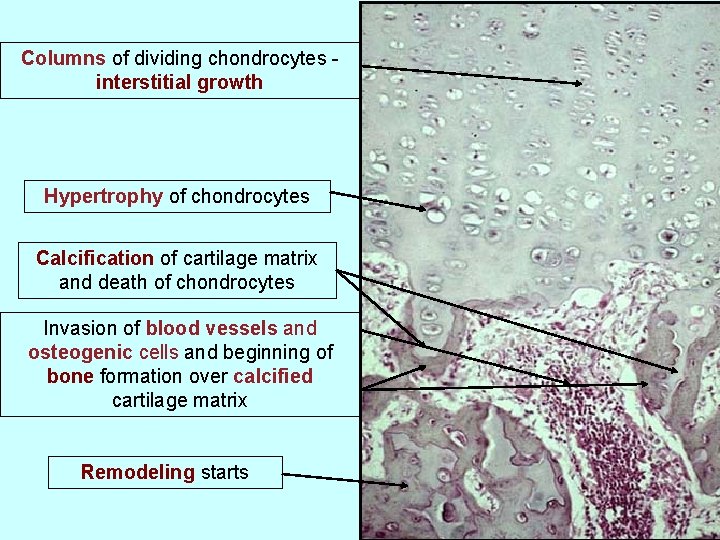
Columns of dividing chondrocytes interstitial growth Hypertrophy of chondrocytes Calcification of cartilage matrix and death of chondrocytes Invasion of blood vessels and osteogenic cells and beginning of bone formation over calcified cartilage matrix Remodeling starts
Formation of secondary center of ossification
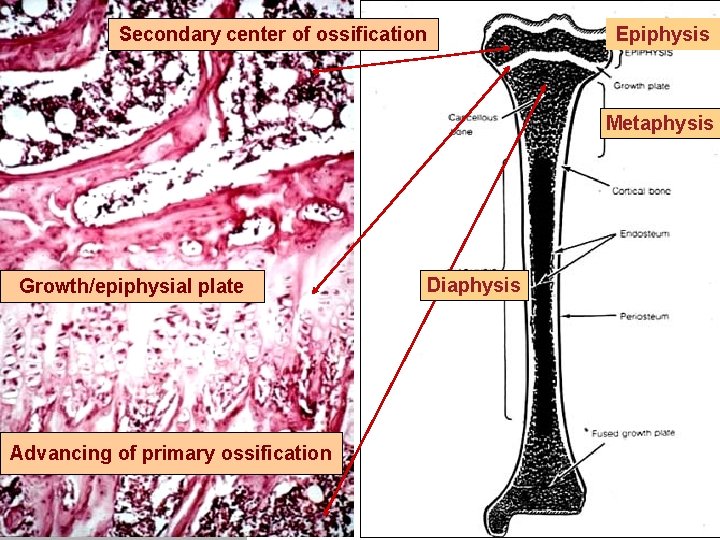
Secondary center of ossification Epiphysis Metaphysis Growth/epiphysial plate Advancing of primary ossification Diaphysis

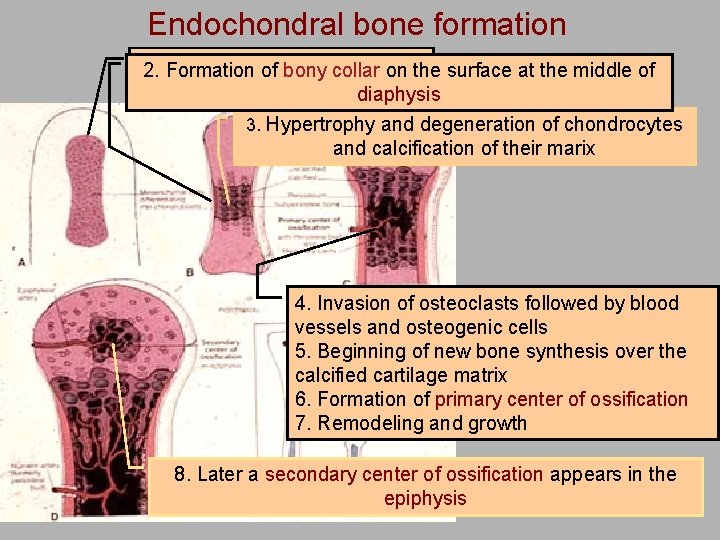
Endochondral bone formation 1. Formation Starting with model 2. of cartilage bony collar on the surface at the middle of diaphysis 3. Hypertrophy and degeneration of chondrocytes and calcification of their marix 4. Invasion of osteoclasts followed by blood vessels and osteogenic cells 5. Beginning of new bone synthesis over the calcified cartilage matrix 6. Formation of primary center of ossification 7. Remodeling and growth 8. Later a secondary center of ossification appears in the epiphysis
- Slides: 37