Care of the Masters Athlete Todd S Shatynski




- Slides: 58
Care of the Masters Athlete Todd S. Shatynski, MD, CAQSM tshatynski@caportho. com NYSAFP Winter Weekend Saratoga Springs, NY January 28, 2017
Objectives • Understand the physiologic changes that take place as an athlete ages and how exercise can affect said changes • Explain basic training and nutrition principles and recommendations for older athletes • Describe the approach to cardiac preparticipation screening in older athletes • Understand a basic treatment algorithm for degenerative arthritis and tendinopathy in older athletes • Try and balance the depression with optimism!
“Exceptionally Successful Aging”? ! Wright. Sports Med Arthrosc Rev 2013. • Dara Torres – Olympic swimming silver, 41 yo • Mark Recchi – 3 rd Hockey Stanley Cup title, 20 years after his first • Nolan Ryan – first of several baseball pitchers to throw well into 40 s • Tom Watson – nearly winning British Open less than a year out from total hip replacement • Dave Scott – 6 x champion of Ironman World Championships, returned from retirement to take 2 nd at age 40
“Masters” Athletes Tayrose, et al. Sports Health 2015. Concannon, et al. PM&R 2012. • Masters = 35+ yo – Cardiac morbidity increases – Body changes – Lifestyle changes • Trains for or participates in athletic competitions specifically designed for older participants
Exceptionally Successful Aging Tayrose, et al. Sports Health 2015. Wright. Sports Med Arthrosc Rev 2013. National Senior Games (50+) • 1987 – 2500 athletes • 2011 – 10, 100 athletes – Despite more stringent qualifying standards NYC Marathon • 119% increase in 50+ yo from 1983 -99 Triathlon • 2011: 2. 9 million participants – 63% >35 yo, 43% >40 yo – 38% women, 47% of Ironman women By 2030, 20% of Americans (70 million) will be >65 yo and will outnumber children
Geriatric Athletes “The Geriatric Athlete”, ACSM Sports Medicine 2013 Rosenbloom, Dunaway. Clin Sports Med 2007. • 1 -2% of American marathon runners (>65) • 23% of health club members (>50) – More likely to go regularly! • Benefits of exercise shift – Recreation/Cardiovascular fitness – Preservation of function • • Physical Cognitive Social Emotional
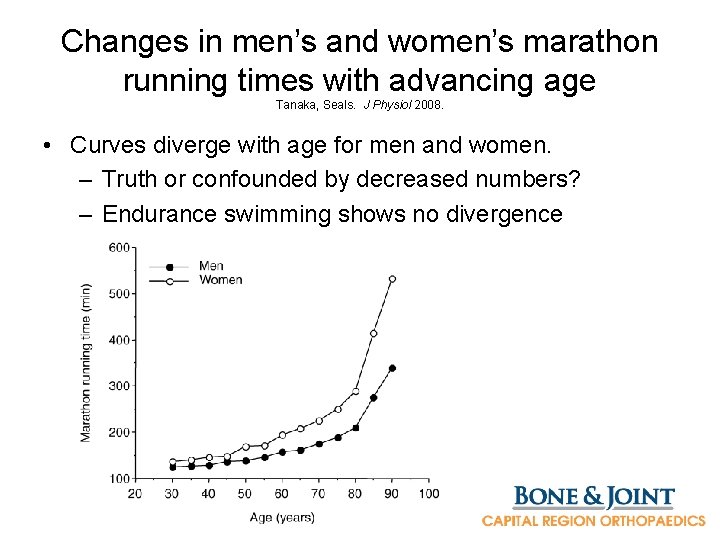
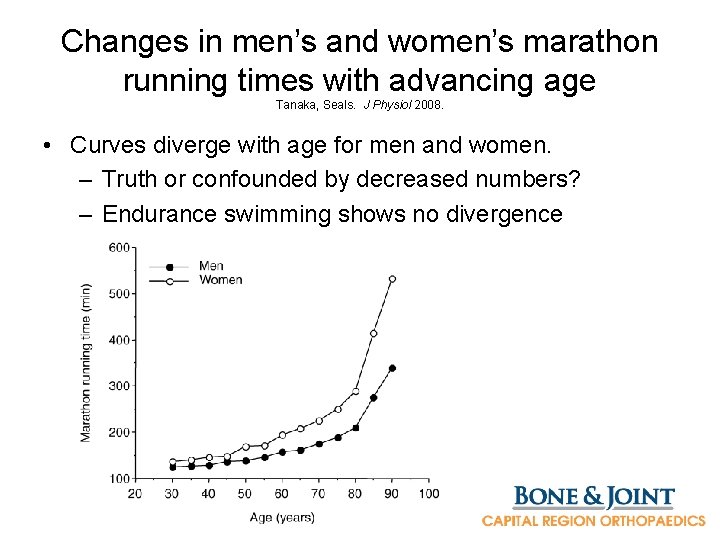
Changes in men’s and women’s marathon running times with advancing age Tanaka, Seals. J Physiol 2008. • Curves diverge with age for men and women. – Truth or confounded by decreased numbers? – Endurance swimming shows no divergence
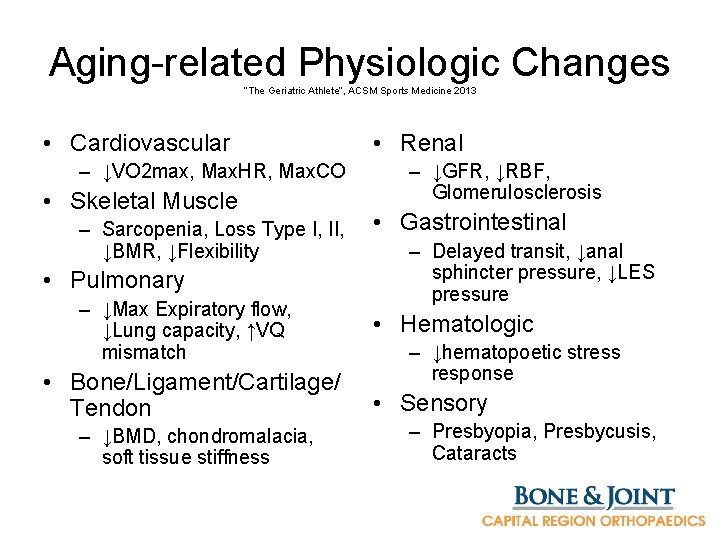
Aging-related Physiologic Changes “The Geriatric Athlete”, ACSM Sports Medicine 2013 • Cardiovascular – ↓VO 2 max, Max. HR, Max. CO • Skeletal Muscle – Sarcopenia, Loss Type I, II, ↓BMR, ↓Flexibility • Pulmonary – ↓Max Expiratory flow, ↓Lung capacity, ↑VQ mismatch • Bone/Ligament/Cartilage/ Tendon – ↓BMD, chondromalacia, soft tissue stiffness • Renal – ↓GFR, ↓RBF, Glomerulosclerosis • Gastrointestinal – Delayed transit, ↓anal sphincter pressure, ↓LES pressure • Hematologic – ↓hematopoetic stress response • Sensory – Presbyopia, Presbycusis, Cataracts
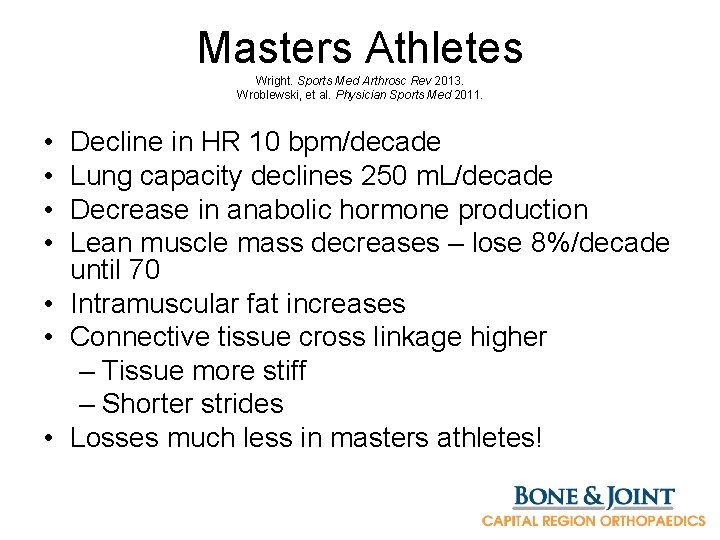
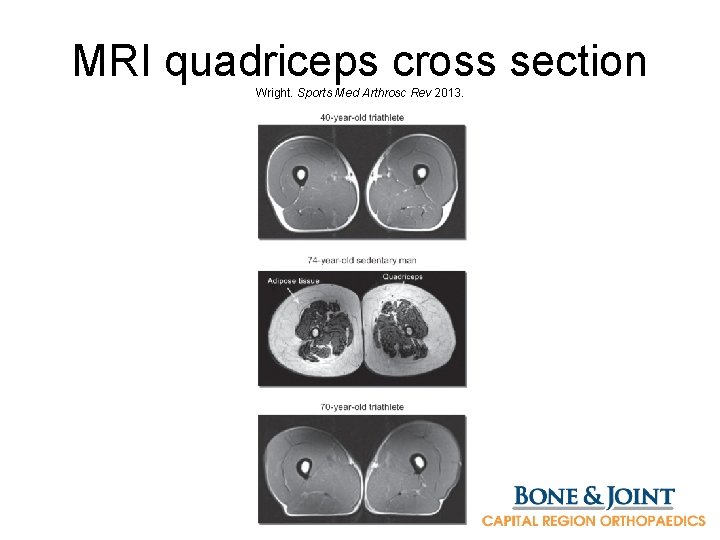
Masters Athletes Wright. Sports Med Arthrosc Rev 2013. Wroblewski, et al. Physician Sports Med 2011. • • Decline in HR 10 bpm/decade Lung capacity declines 250 m. L/decade Decrease in anabolic hormone production Lean muscle mass decreases – lose 8%/decade until 70 • Intramuscular fat increases • Connective tissue cross linkage higher – Tissue more stiff – Shorter strides • Losses much less in masters athletes!
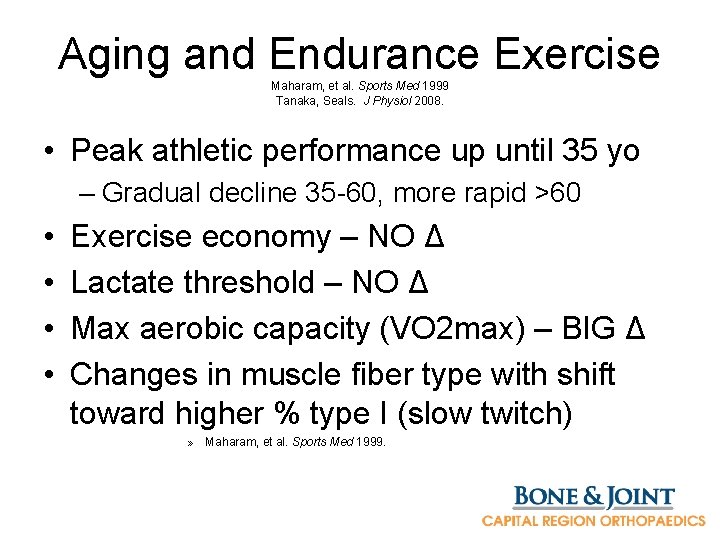
Aging and Endurance Exercise Maharam, et al. Sports Med 1999 Tanaka, Seals. J Physiol 2008. • Peak athletic performance up until 35 yo – Gradual decline 35 -60, more rapid >60 • • Exercise economy – NO Δ Lactate threshold – NO Δ Max aerobic capacity (VO 2 max) – BIG Δ Changes in muscle fiber type with shift toward higher % type I (slow twitch) » Maharam, et al. Sports Med 1999.
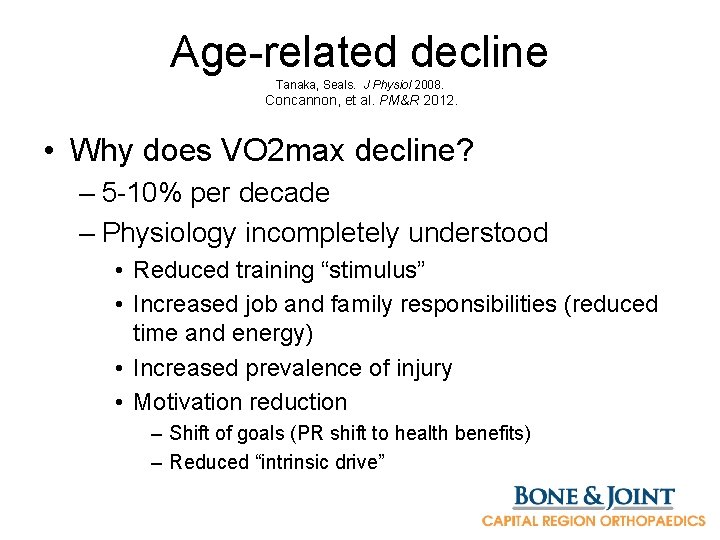
Age-related decline Tanaka, Seals. J Physiol 2008. Concannon, et al. PM&R 2012. • Why does VO 2 max decline? – 5 -10% per decade – Physiology incompletely understood • Reduced training “stimulus” • Increased job and family responsibilities (reduced time and energy) • Increased prevalence of injury • Motivation reduction – Shift of goals (PR shift to health benefits) – Reduced “intrinsic drive”
Muscle changes • Sarcopenia, Muscle atrophy – Decreased Testosterone, GH – Cardiac muscle deconditioning – Chronic disuse – exercise staves off decline » Wroblewski, et al. Phys Sportsmed 2011. • Same fatigue level as younger – Slower recovery
Masters Triathletes Wright. Sports Med Arthrosc Rev 2013. Lepers, et al. Sports Med 2013. • Train less than younger athletes • 89% report injuries after 50 yo. • Cycling decreases slower than running – Concentric muscle activation in cycling versus eccentric in running • Less concentric decreases with aging
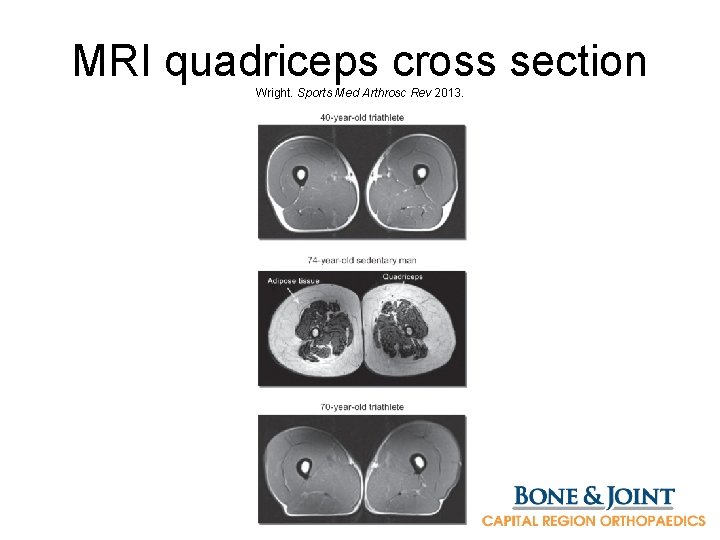
MRI quadriceps cross section Wright. Sports Med Arthrosc Rev 2013.
Motivation Franklin, et al. Curr Sports Med Rep 2004 • Advantages: experience, advanced level of self understanding • Disadvantages: day to day diversions (family, professional, social responsibilities) • Age adjusted tables for performance – http: //www. runnersworld. com/tools/ – Compare to prior performances of “younger self” – Refine competition goals without diminishing the competitive spirit
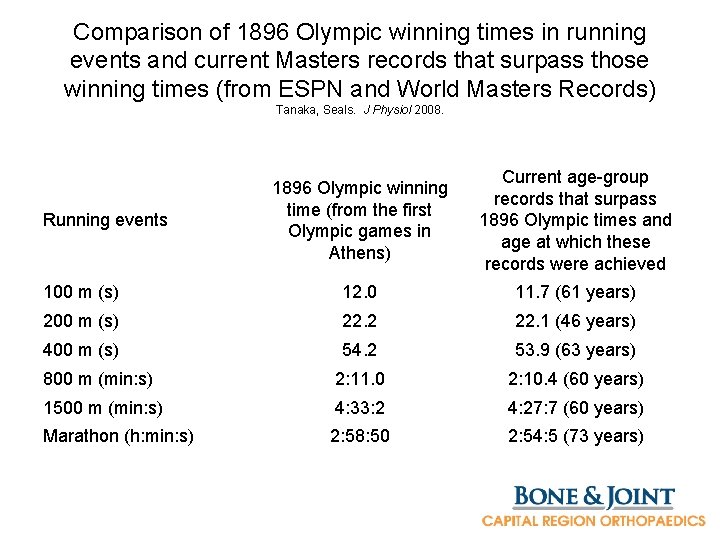
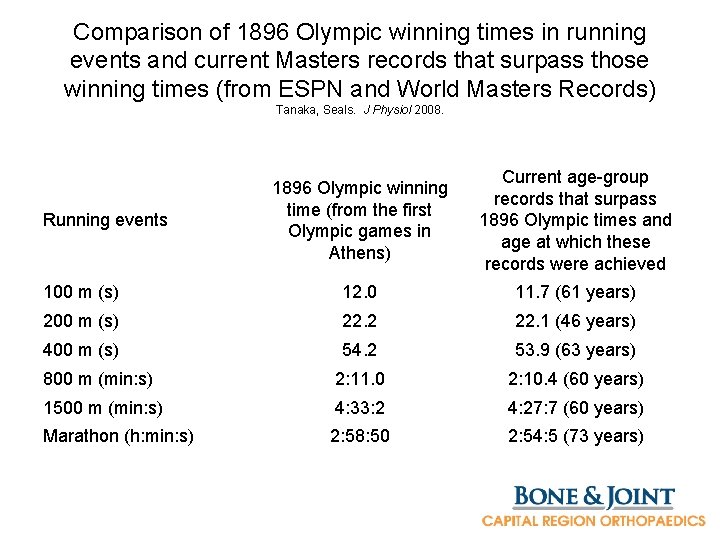
Comparison of 1896 Olympic winning times in running events and current Masters records that surpass those winning times (from ESPN and World Masters Records) Tanaka, Seals. J Physiol 2008. 1896 Olympic winning time (from the first Olympic games in Athens) Current age-group records that surpass 1896 Olympic times and age at which these records were achieved 100 m (s) 12. 0 11. 7 (61 years) 200 m (s) 22. 2 22. 1 (46 years) 400 m (s) 54. 2 53. 9 (63 years) 800 m (min: s) 2: 11. 0 2: 10. 4 (60 years) 1500 m (min: s) 4: 33: 2 4: 27: 7 (60 years) Marathon (h: min: s) 2: 58: 50 2: 54: 5 (73 years) Running events
Why are they getting faster? Tanaka, Seals. J Physiol 2008. • Increasing numbers of participants • Training practices evolving • Nutritional practices evolving
Training Principles Franklin, et al. Curr Sports Med Rep 2004 • • 3 -5 days/week 55 -90% of max heart rate 20 -60 minutes aerobic activity/day Mode: Large muscle groups, maintained, rhythmical and aerobic • Resistance: 8 -10 exercises targeting major muscle groups, 2 -3 xs/week, 8 -10 reps to fatigue • Flexibility training: 2 -3 days/week

Special Considerations for Masters athletes Wright. Sports Med Arthrosc Rev 2013. • 4 components of total fitness (F. A. C. E. ) 1. Flexibility 2. Aerobic intensity 3. Resistance training (Carrying a load) 4. Equilibrium and Balance – Less frequent but higher intensity regimen – Resistance training to include balance and total body

Multidisciplinary Care • • PCP Sports medicine Orthopedics Physiatry Physical therapist Trainers Coaches Nutritionists
Should we worry? Franklin, et al. Curr Sports Med Rep 2004 • PCP needs consistent, cost-effective means of evaluation prior to recommending vigorous/competitive physical activity • Risk of Sudden Cardiac Death = Diseased or Susceptible heart + Exercise – 1/15, 000 runners per year >35 yo – 1/50, 000 marathon participants overall • History and Physical Examination • Family History • Personal History (AHA 12 points)
Cardiovascular Risk in Masters Endurance Athletes (Boston MASTER) Shapero, et al. Sports Medicine 2016 • Masters Athletes Survey To Evaluate Risk – 66% response, 591 athletes • 2/3 have >=1 CV risk factor • Established CV disease 9% (AFib, CAD) • 1/7 express dissatisfaction over healthcare system – Concerns dismissed due to status as an athlete, inadequate knowledge, attention
Cardiac risks in Masters Shapero, et al. Sports Medicine 2016 • Atrial fibrillation associated with years of cumulative exercise exposure +/- HTN • ? High levels of exercise may be susceptible to CV disease – Mortality benefits dissipate with high level exercise • Needs to address patiet-provider mismatch
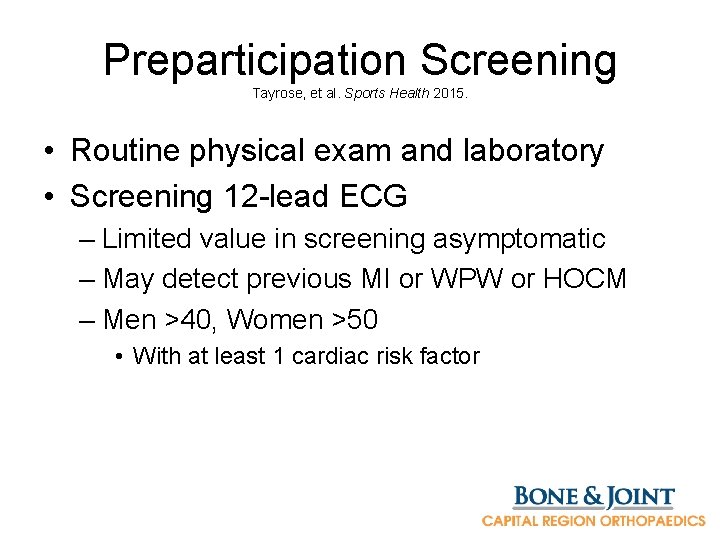
Preparticipation Screening Tayrose, et al. Sports Health 2015. • Routine physical exam and laboratory • Screening 12 -lead ECG – Limited value in screening asymptomatic – May detect previous MI or WPW or HOCM – Men >40, Women >50 • With at least 1 cardiac risk factor
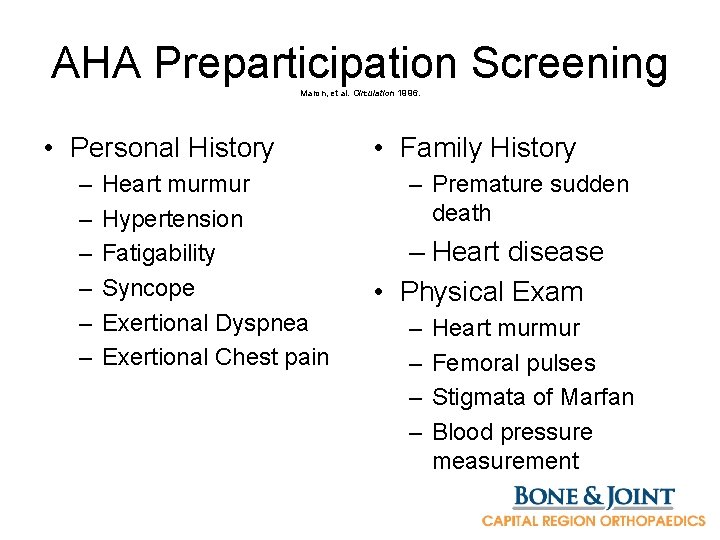
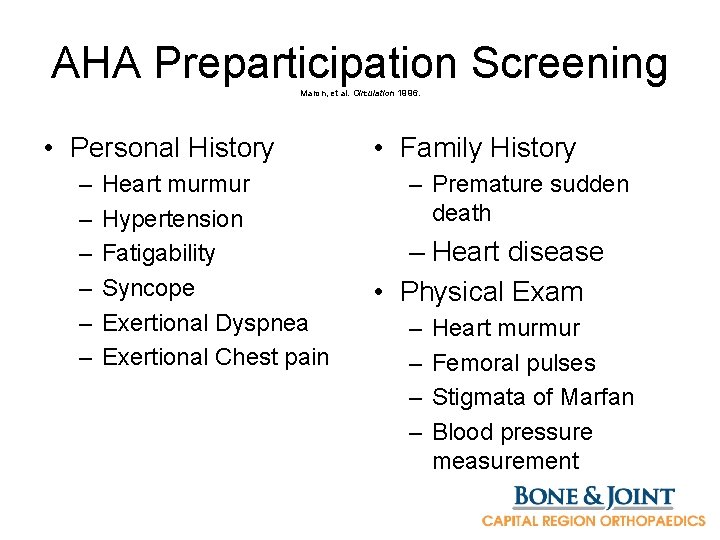
AHA Preparticipation Screening Maron, et al. Circulation 1996. • Personal History – – – Heart murmur Hypertension Fatigability Syncope Exertional Dyspnea Exertional Chest pain • Family History – Premature sudden death – Heart disease • Physical Exam – – Heart murmur Femoral pulses Stigmata of Marfan Blood pressure measurement
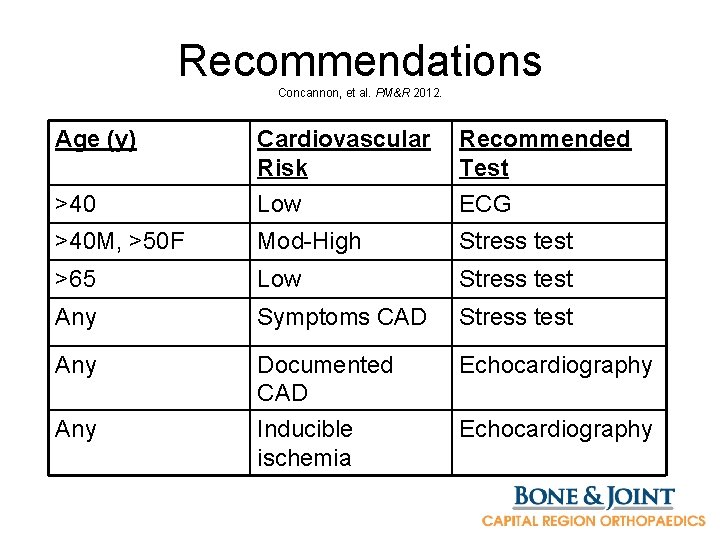
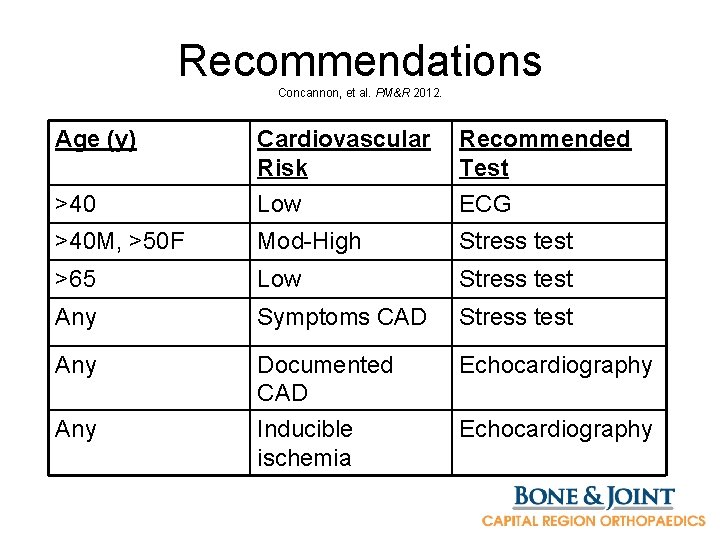
Recommendations Concannon, et al. PM&R 2012. Age (y) >40 Cardiovascular Risk Low Recommended Test ECG >40 M, >50 F Mod-High Stress test >65 Low Stress test Any Symptoms CAD Stress test Any Documented CAD Inducible ischemia Echocardiography Any Echocardiography
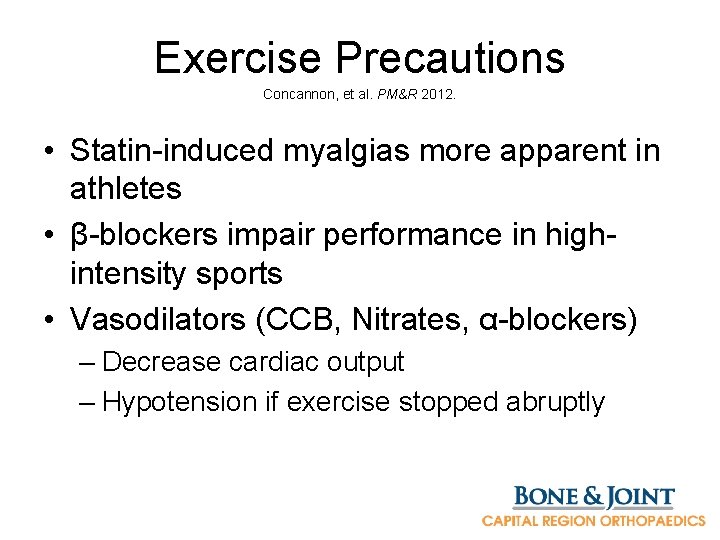
Exercise Precautions Concannon, et al. PM&R 2012. • Statin-induced myalgias more apparent in athletes • β-blockers impair performance in highintensity sports • Vasodilators (CCB, Nitrates, α-blockers) – Decrease cardiac output – Hypotension if exercise stopped abruptly
Nutritional Considerations Striegel, et al. Int J Sports Med 2006. • Questionaires 2004 World Championships – 61% participants reported use of nutritional supplements – Vitamins, minerals – Per advice from medical community – Higher health consciousness than younger athletes – “Health reasons” vs “performance in sports” (pros) – Possible contamination by banned (anabolic) substances
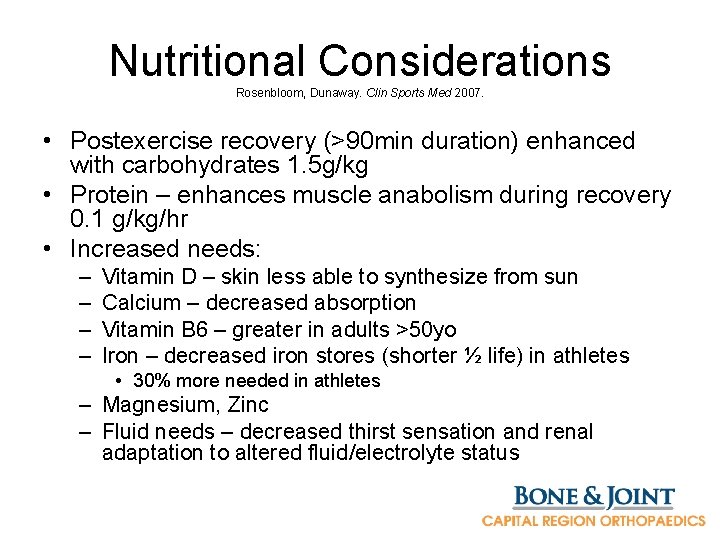
Nutritional Considerations Rosenbloom, Dunaway. Clin Sports Med 2007. • Postexercise recovery (>90 min duration) enhanced with carbohydrates 1. 5 g/kg • Protein – enhances muscle anabolism during recovery 0. 1 g/kg/hr • Increased needs: – – Vitamin D – skin less able to synthesize from sun Calcium – decreased absorption Vitamin B 6 – greater in adults >50 yo Iron – decreased iron stores (shorter ½ life) in athletes • 30% more needed in athletes – Magnesium, Zinc – Fluid needs – decreased thirst sensation and renal adaptation to altered fluid/electrolyte status
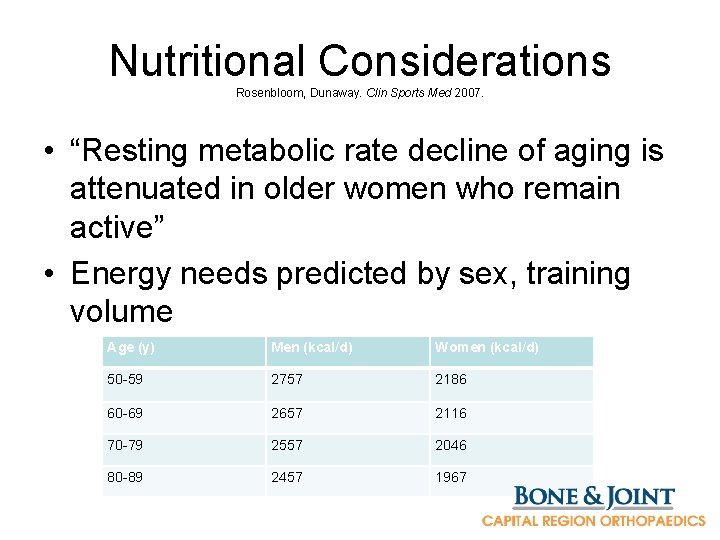
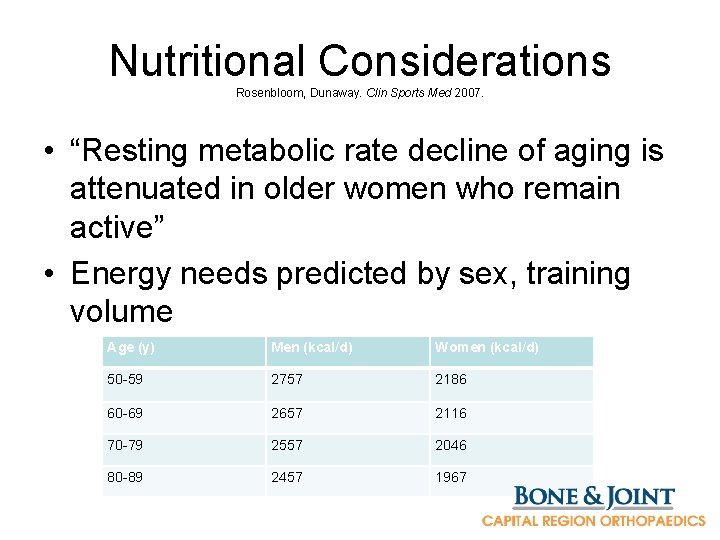
Nutritional Considerations Rosenbloom, Dunaway. Clin Sports Med 2007. • “Resting metabolic rate decline of aging is attenuated in older women who remain active” • Energy needs predicted by sex, training volume Age (y) Men (kcal/d) Women (kcal/d) 50 -59 2757 2186 60 -69 2657 2116 70 -79 2557 2046 80 -89 2457 1967
Degenerative Conditions Tayrose, et al. Sports Health 2015. • Rotator cuff injury • Tendinopathy – Patellar – Achilles • Degnerative meniscus tear • Osteoarthritis • 1/3 of medical visits to doctor
Tendinopathy Harmon, Rao. Hematology 2013. • Tendinopathy continuum – Tendon excessive load -> Progressive Degradation -> Disrepair -> Degenerative Tendinopathy • Treatment: Rest, Eccentric exercises, Extracorporeal shock wave therapy, Needling/Tenotomy, Autologous blood injections, PRP
Osteoarthritis Adams, et al. Sports Med Arthrosc Rev 2013 Vannini, et al. Knee Surg Sports Traumatol Arthrosc 2016. • 27 million in US with OA affecting quality of life • Soccer – OA incidence between 16 -80% – 5 -12 xs more frequent and 4 -5 years earlier
Osteoarthritis Tayrose, et al. Sports Health 2015. • No consensus on relationship between high level exercise and OA • High joint loading, high impact VS • Muscular strength, mass, range of motion • Weight maintenance • Traumatic injury risk
“Does running lead to cartilage damage? ” Luke, et al. Am J Sports Med 2010. • High-Field MRI of articular cartilage before and after a marathon • Cohort, Level 2 • 3 MRIs – 2 wks before, 48 hrs after, 10+ wks after (compared w/ non runners) – Measure markers of early cartilage breakdown • Runners showed elevations in biomarkers – Most normalized by 3 months
“Effects of Running and Walking on Osteoarthritis and Hip Replacement Risk” Williams, Paul T. Med Sci Sports and Exerc 2013 • National Runners’ and Walkers’ Health Studies • Prospective cohort, ~90, 000 subjects • 73 k runners, 14 k walkers – 863, >60 mi/wk – Many run marathons – BMI walkers > runners
So… get to the point! • Osteoarthritis of the hip less likely in runners than walkers! • Hip replacement risk lower in runners! • Decreased risk even when controlled for BMI • Running more than 13 km/wk protective • Marathon frequency, intensity, 10 k intensity did not predict increased risk!
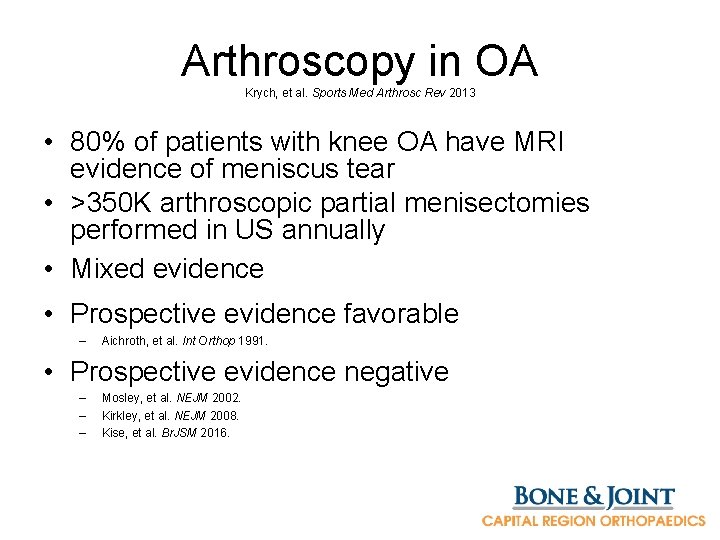
Arthroscopy in OA Krych, et al. Sports Med Arthrosc Rev 2013 • 80% of patients with knee OA have MRI evidence of meniscus tear • >350 K arthroscopic partial menisectomies performed in US annually • Mixed evidence • Prospective evidence favorable – Aichroth, et al. Int Orthop 1991. • Prospective evidence negative – – – Mosley, et al. NEJM 2002. Kirkley, et al. NEJM 2008. Kise, et al. Br. JSM 2016.

Arthroscopy in OA – Me. Te. OR trial Katz, et al. NEJM 2013 Katz, et al. JBJS 2016. • 7 center RCT, >45 yo, knee symptoms, severe OA excluded • 4 recent RCTs compared arthroscopy to conservative/PT – 3/4 showed no significant benefit to surgery – 1/3 of subjects crossed over to surgery arm before primary outcome assessment • No difference between those randomized to surgery initially • Men more likely to opt for surgical treatment • More pain, acute presentation • Lower educational status (SPORT trial) – Delitto, et al. Ann Intern Med 2015
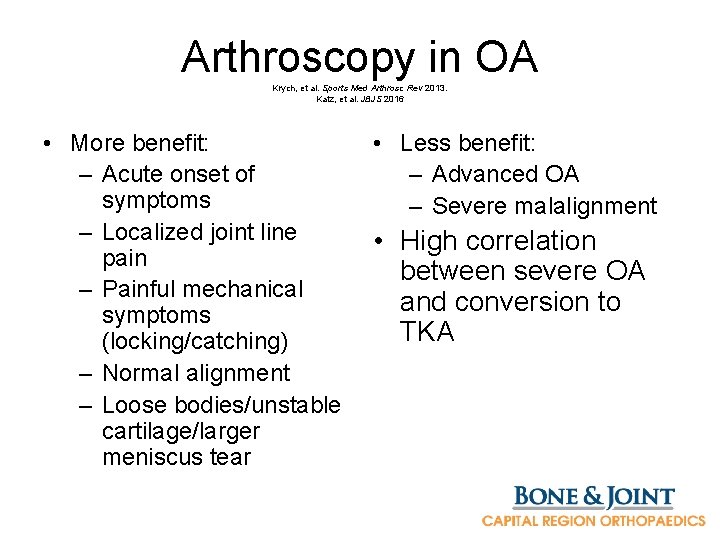
Arthroscopy in OA Krych, et al. Sports Med Arthrosc Rev 2013. Katz, et al. JBJS 2016 • More benefit: – Acute onset of symptoms – Localized joint line pain – Painful mechanical symptoms (locking/catching) – Normal alignment – Loose bodies/unstable cartilage/larger meniscus tear • Less benefit: – Advanced OA – Severe malalignment • High correlation between severe OA and conversion to TKA
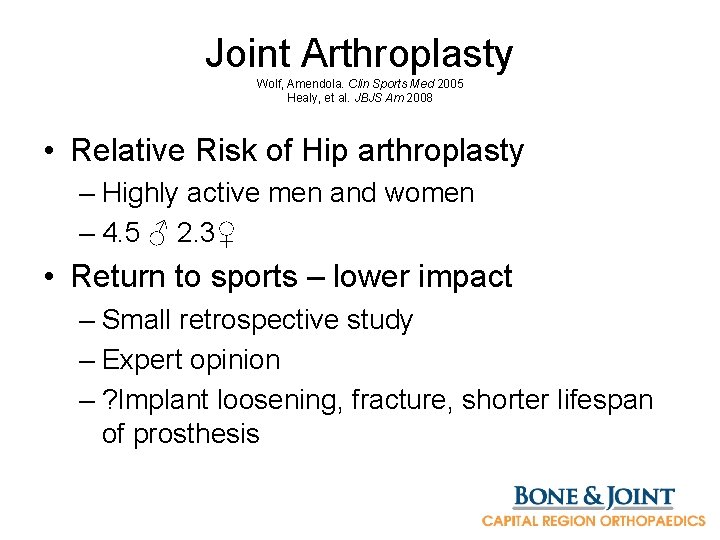
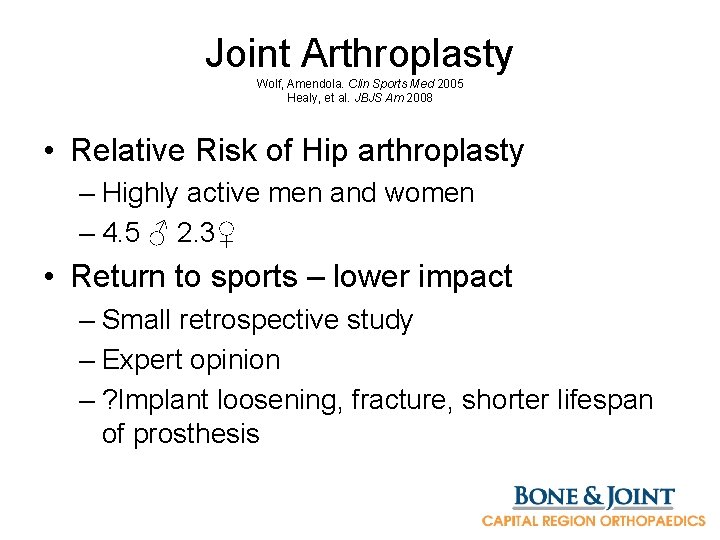
Joint Arthroplasty Wolf, Amendola. Clin Sports Med 2005 Healy, et al. JBJS Am 2008 • Relative Risk of Hip arthroplasty – Highly active men and women – 4. 5 ♂ 2. 3♀ • Return to sports – lower impact – Small retrospective study – Expert opinion – ? Implant loosening, fracture, shorter lifespan of prosthesis
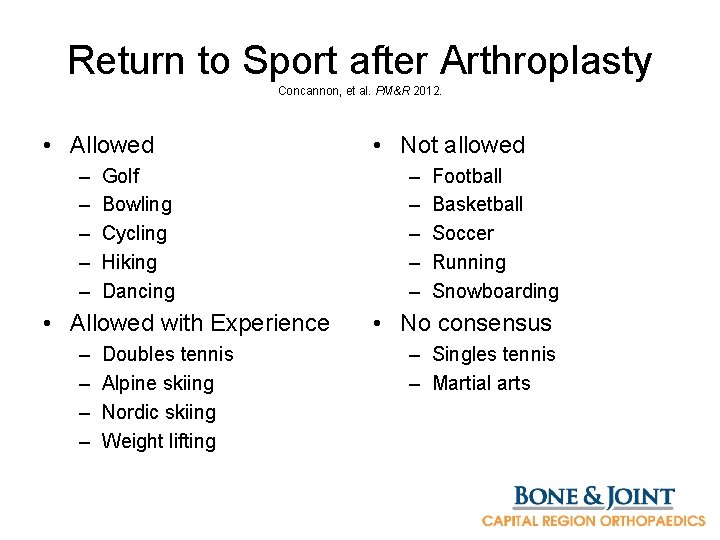
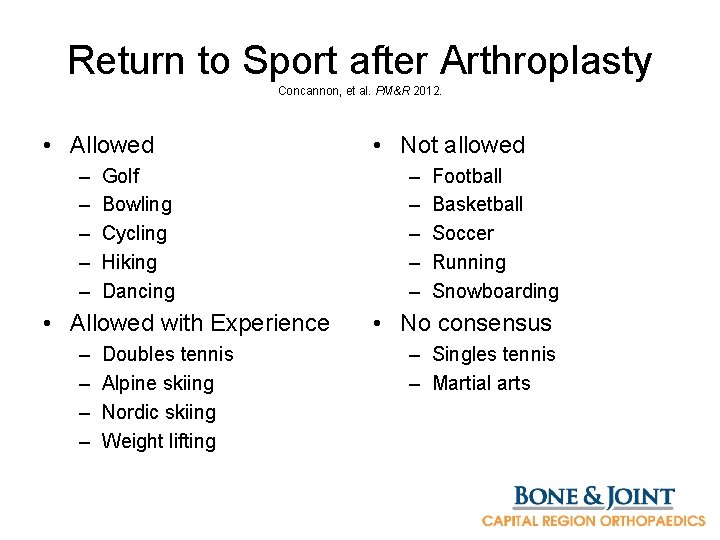
Return to Sport after Arthroplasty Concannon, et al. PM&R 2012. • Allowed – – – Golf Bowling Cycling Hiking Dancing • Allowed with Experience – – Doubles tennis Alpine skiing Nordic skiing Weight lifting • Not allowed – – – Football Basketball Soccer Running Snowboarding • No consensus – Singles tennis – Martial arts

Hip/Knee Arthroplasty Options Mc. Keon, Rand. Sports Med Arthrosc Rev 2013. • Hip resurfacing (Birmingham) – Less high-impact restriction – Metal-on-metal • Unicompartmental knee arthroplasty – Early recovery – More natural function – Patient satisfaction – Higher rate of revision to total knee arthroplasty • Especially from patients outside specialty centers
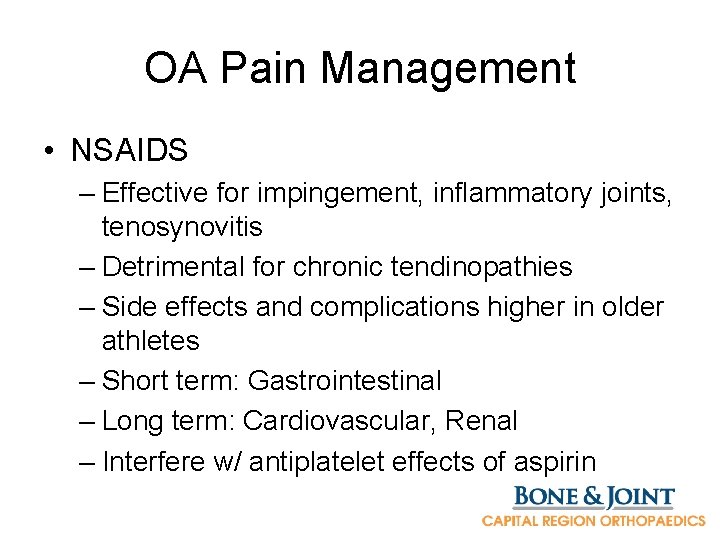
OA Pain Management • NSAIDS – Effective for impingement, inflammatory joints, tenosynovitis – Detrimental for chronic tendinopathies – Side effects and complications higher in older athletes – Short term: Gastrointestinal – Long term: Cardiovascular, Renal – Interfere w/ antiplatelet effects of aspirin
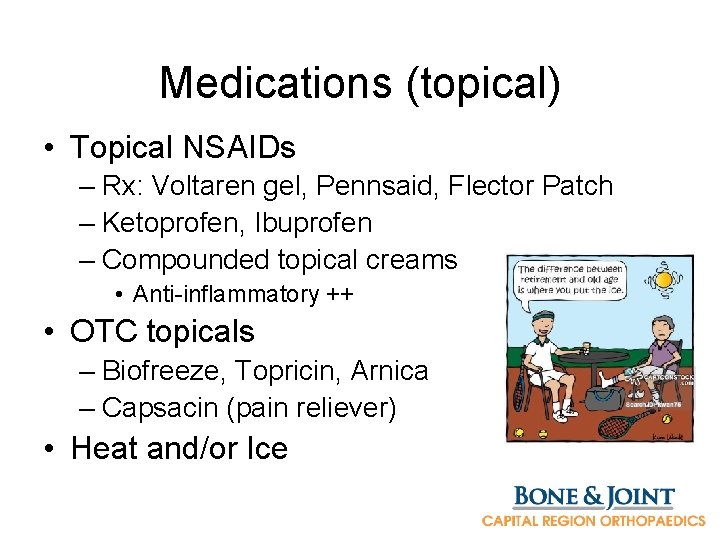
Medications (topical) • Topical NSAIDs – Rx: Voltaren gel, Pennsaid, Flector Patch – Ketoprofen, Ibuprofen – Compounded topical creams • Anti-inflammatory ++ • OTC topicals – Biofreeze, Topricin, Arnica – Capsacin (pain reliever) • Heat and/or Ice
Supplements • Flavonoids – Flavocoxid (Limbrel) • • • Glucosamine Chondroitin MSM Hyaluronate Sam-e • Flax seed oil • Fish oil • Avocado soybean unsaponifiables • Cherry juice extract • Rosehip • Tumeric – 500 mg twice daily
Bracing for OA Briem, Ramsey. Sports Med Arthorsc Rev 2013. • Predominately for knee, ankle, wrist/hand • Support joint to give improved proprioception • Less sensation of instability • Knee unloader bracing (varus or valgus) – Improves pain, exercise tolerance • Orthotics
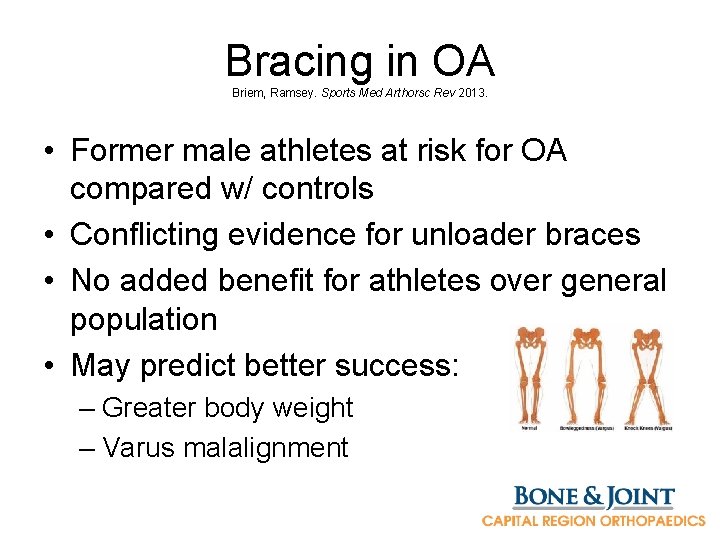
Bracing in OA Briem, Ramsey. Sports Med Arthorsc Rev 2013. • Former male athletes at risk for OA compared w/ controls • Conflicting evidence for unloader braces • No added benefit for athletes over general population • May predict better success: – Greater body weight – Varus malalignment
Physical Therapy for OA Adams, et al. Sports Med Arthrosc Rev 2013 • Manual therapy: soft tissue mobility restrictions and adhesions • Therapeutic exercise: address altered/ compensatory movement patterns – Lower extremity strength/ROM disparities • Modalities: – Electrical Stim (TENS) + – Therapeutic Ultrasound + – Low Level Laser +
Physical therapy Vannini, et al. Knee Surg Sports Traumatol Arthrosc 2016. • Therapeutic exercises – Weak hip abductors compromise mediallateral pelvis stability during single leg stance – Increase load on medial knee joint loading (OA)
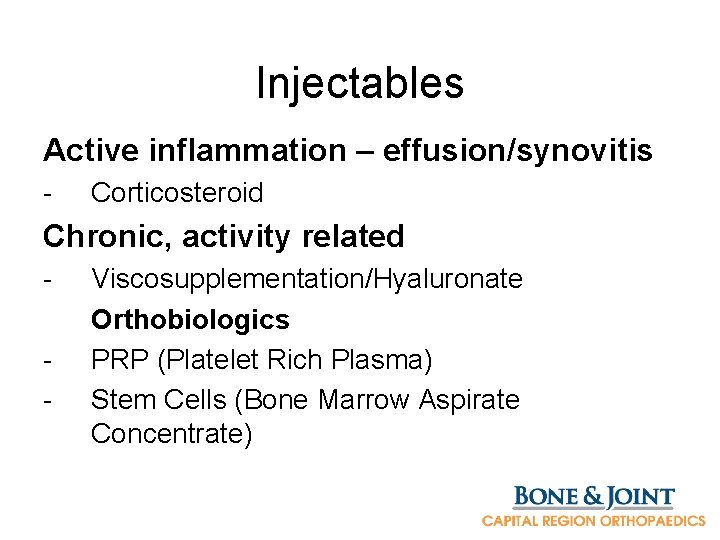
Injectables Active inflammation – effusion/synovitis - Corticosteroid Chronic, activity related - Viscosupplementation/Hyaluronate Orthobiologics PRP (Platelet Rich Plasma) Stem Cells (Bone Marrow Aspirate Concentrate)
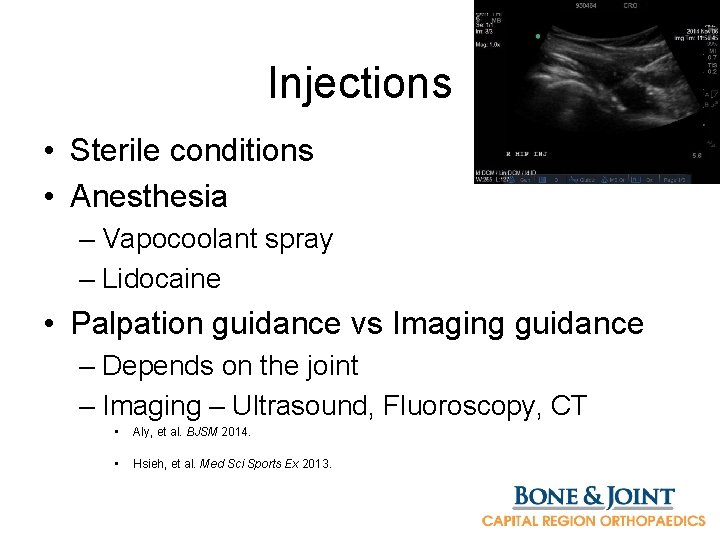
Injections • Sterile conditions • Anesthesia – Vapocoolant spray – Lidocaine • Palpation guidance vs Imaging guidance – Depends on the joint – Imaging – Ultrasound, Fluoroscopy, CT • Aly, et al. BJSM 2014. • Hsieh, et al. Med Sci Sports Ex 2013.
Future OA monitoring Vannini, et al. Knee Surg Sports Traumatol Arthrosc 2016. • Biomarkers – Knee OA, early degeneration – Serum cartilage oligomeric protein (s. COMP) – Urinary C-telopeptide of type II collagen (u. CTX-II) – Helpful for diagnosis, treatment monitoring?
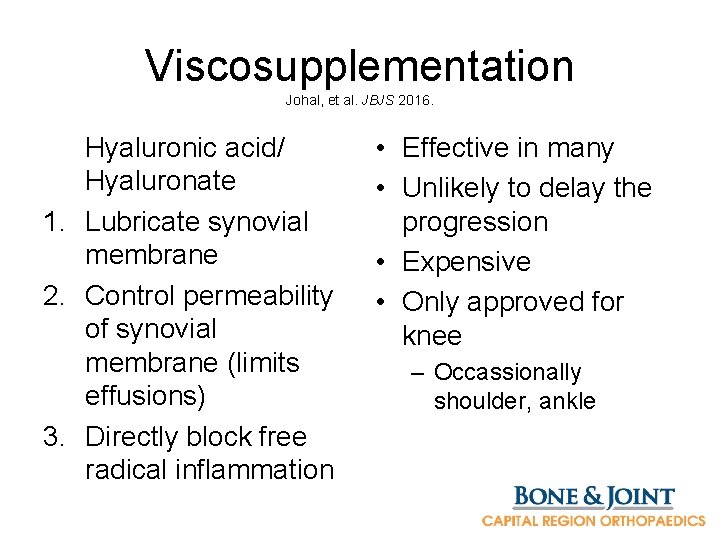
Viscosupplementation Johal, et al. JBJS 2016. Hyaluronic acid/ Hyaluronate 1. Lubricate synovial membrane 2. Control permeability of synovial membrane (limits effusions) 3. Directly block free radical inflammation • Effective in many • Unlikely to delay the progression • Expensive • Only approved for knee – Occassionally shoulder, ankle
Platelet Rich Plasma (PRP) Patel, et al. AJSM 2013. Forogh, et al. J Sports Med Phys Fit 2015. Sampson, et al. Am J Phys Med Rehabil 2010. • Venous blood draw (60 -120 cc) • Centrifugation – Separates buffy coat • Injected back into joint/tendon • PRP rich in growth factors, cytokines – Recruits stem cells
Platelet Rich Plasma (PRP) Harmon, Rao. Hematology 2013. • Studies show benefit – Inconsistent • More effective than visco in OA • Early evidence – not currently covered by insurance • Leukocyte-rich PRP (Soft tissue) vs Leukocytepoor PRP (OA) • PRP should not be first line treatment, use in “off season”
Stem Cell Therapy Crane, et al. Phys Med Rehabil Clinics N Am 2016. Centeno, et al. Biomed Research Int 2014. Kopka, Bradley. J Knee Surg 2016. • Multi-potent stem cells • Bone Marrow Aspirate (or Lipoaspirate) – Prepared similar to PRP • • Injected into joint, capsule Early evidence promising Many variables FDA: “minimal manipulation”
Conclusions • Exercise is good for all ages • Performances continue to improve • Be aware that even “fit” people can get sick and need screening • Degenerative conditions are quite prevalent but should rarely preclude participation in sports
 Athlete's circle of care
Athlete's circle of care Primary secondary tertiary care definition
Primary secondary tertiary care definition Physics javelin projectile motion
Physics javelin projectile motion Pulse rate group
Pulse rate group Back pain kings park
Back pain kings park Narrative and lyric poetry
Narrative and lyric poetry Pelergo
Pelergo Refers to the path raised by a projectile during its motion
Refers to the path raised by a projectile during its motion Athlete plural possessive
Athlete plural possessive Occupational athletics
Occupational athletics Purpose of circuit training
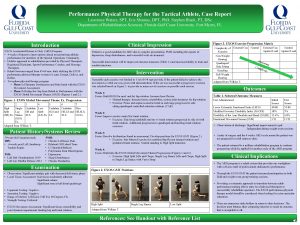
Purpose of circuit training Modified tactical athlete performance assessment
Modified tactical athlete performance assessment Matthews motshwarateu
Matthews motshwarateu Olympic athlete
Olympic athlete To an athlete dying young theme
To an athlete dying young theme Corporate athlete model
Corporate athlete model The athlete machine
The athlete machine Action head bumps ball reaction
Action head bumps ball reaction Which athlete has the most olympic gold medals
Which athlete has the most olympic gold medals Register my athlete login
Register my athlete login Communicable and noncommunicable diseases venn diagram
Communicable and noncommunicable diseases venn diagram Amuse suffix
Amuse suffix Athlete marketing plan
Athlete marketing plan Athlete possessive form
Athlete possessive form My favorite athlete is
My favorite athlete is Tablić masters
Tablić masters Masters thesis structure
Masters thesis structure Wmu school of social work
Wmu school of social work Masters in clinical psychology uae
Masters in clinical psychology uae Classification de master
Classification de master Sindrom masters allen
Sindrom masters allen Department of anthropology
Department of anthropology Florida state university computer science
Florida state university computer science Kennesaw online masters
Kennesaw online masters Cven intranet
Cven intranet Masters in infrastructure planning and management
Masters in infrastructure planning and management John henry bmt
John henry bmt Jpsm short courses
Jpsm short courses And this is the confidence
And this is the confidence Masters level writing
Masters level writing Isu masters program
Isu masters program Crecine gatech
Crecine gatech Uwa masters of education
Uwa masters of education The economics masters
The economics masters Utsa online masters
Utsa online masters Qtem network
Qtem network Arlington aquatic club
Arlington aquatic club Siop jobnet
Siop jobnet Gus lego masters
Gus lego masters Approaches meets masters
Approaches meets masters Masters in lifestyle medicine
Masters in lifestyle medicine Qtem masters network
Qtem masters network James masters elementary
James masters elementary Kinesiology ucf catalog
Kinesiology ucf catalog Ucla masters entry nursing
Ucla masters entry nursing American masters whitman and dickinson
American masters whitman and dickinson George gray by edgar lee masters
George gray by edgar lee masters Ucf mpa program
Ucf mpa program Approaches meets masters
Approaches meets masters