Arogya Manthan Working Group 2 Monitoring Fraud and
- Slides: 24
Arogya Manthan Working Group 2 Monitoring, Fraud and Abuse Control 30 th September 2019
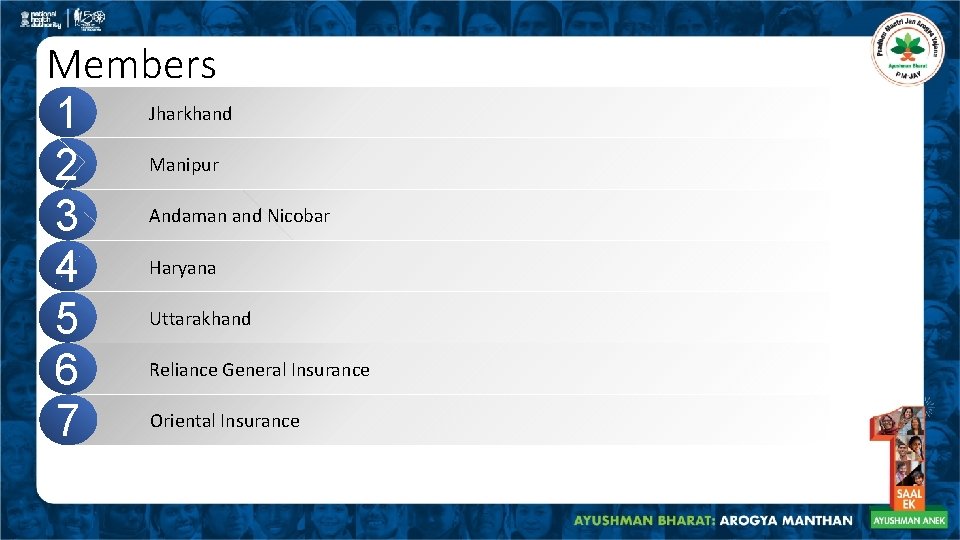
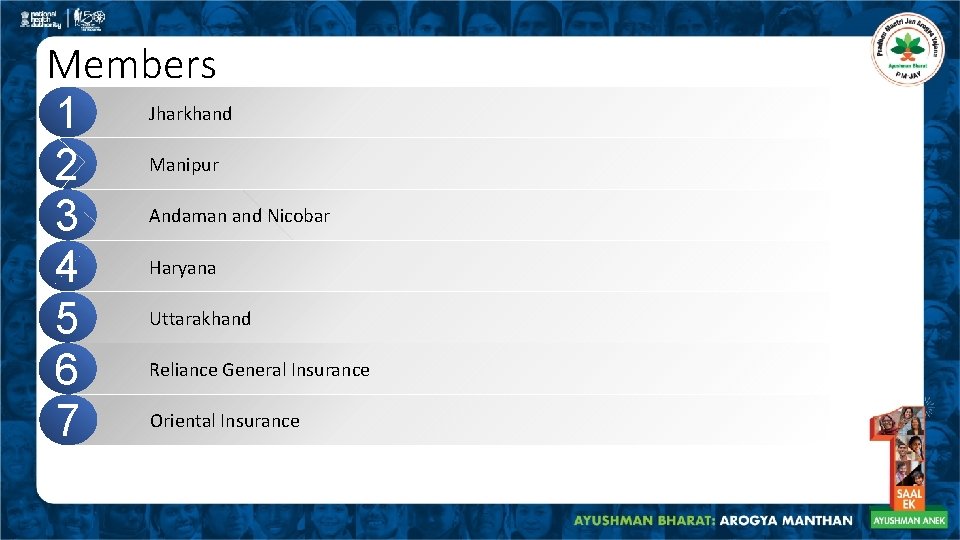
Members Jharkhand 1 Manipur 2 Andaman and Nicobar 3 Haryana 4 Uttarakhand 5 Reliance General Insurance 6 Oriental Insurance 7
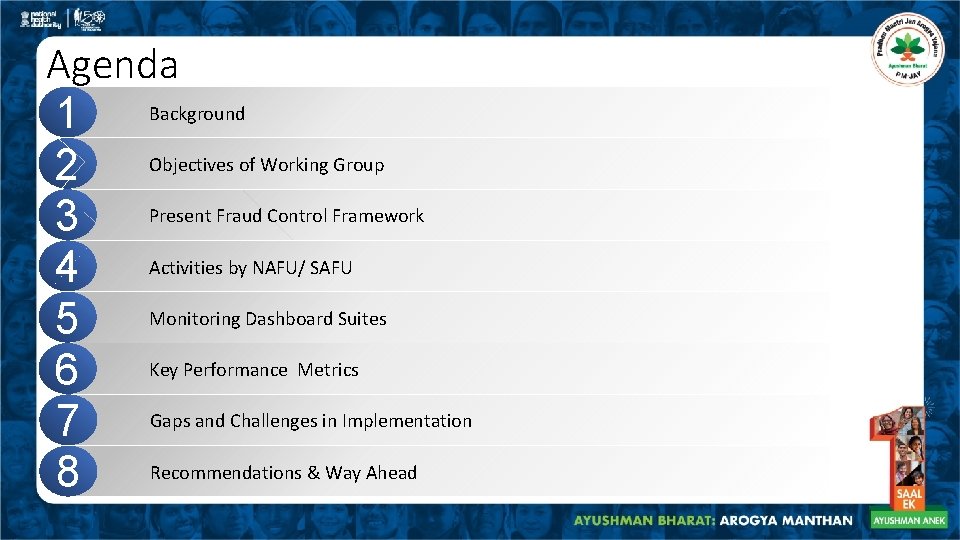
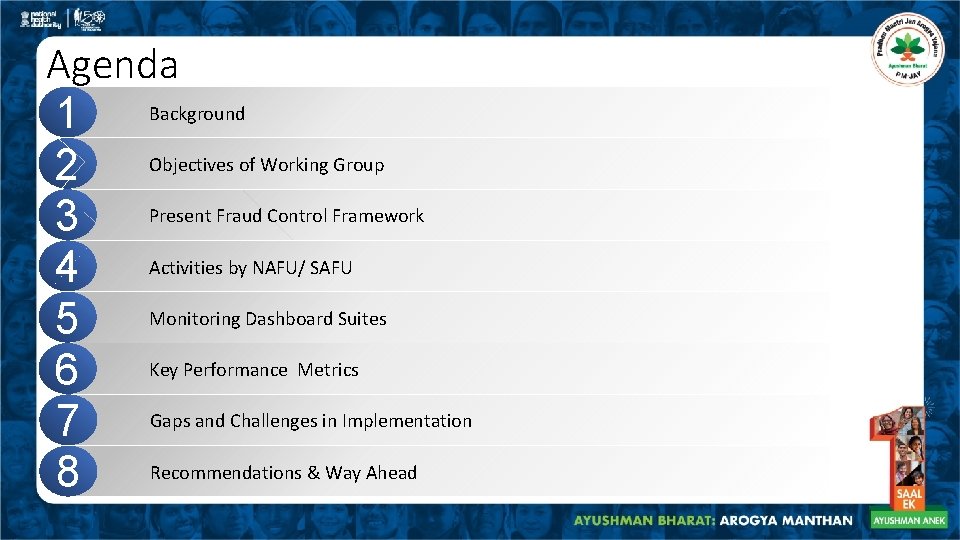
Agenda Background 1 Objectives of Working Group 2 Present Fraud Control Framework 3 Activities by NAFU/ SAFU 4 Monitoring Dashboard Suites 5 Key Performance Metrics 6 Gaps and Challenges in Implementation 7 Recommendations & Way Ahead 8
Background AB-PMJAY involves a multitude of stakeholders, working jointly for 50 crore beneficiaries to avail free treatment at empaneled healthcare providers (EHCPs) 1 2 3 It has a robust mechanisms for monitoring performance and utilization trends, ensuring adherence to guiding principles to control fraud and abuse A Working Group on Monitoring, Fraud and Abuse Control comprises officials from five State Health Agencies (SHAs) and two Insurance Companies
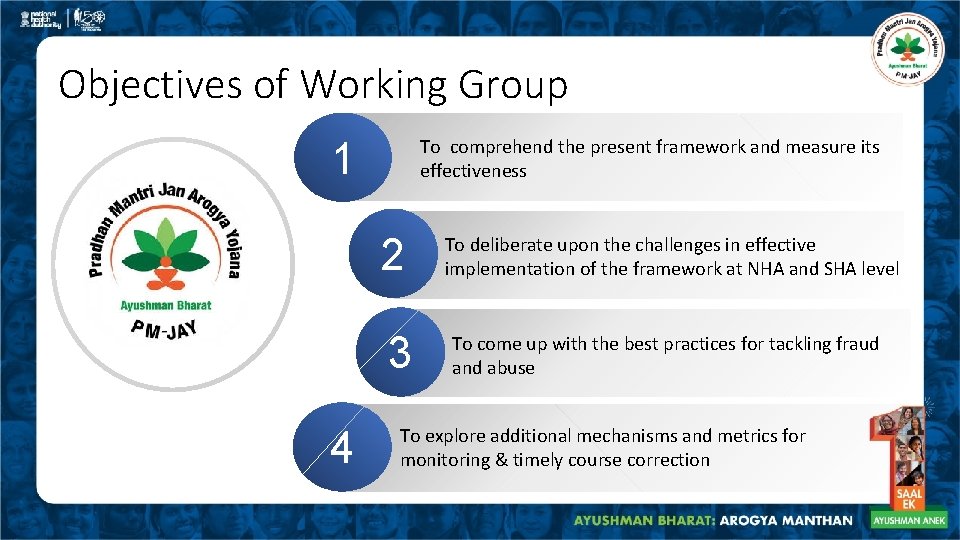
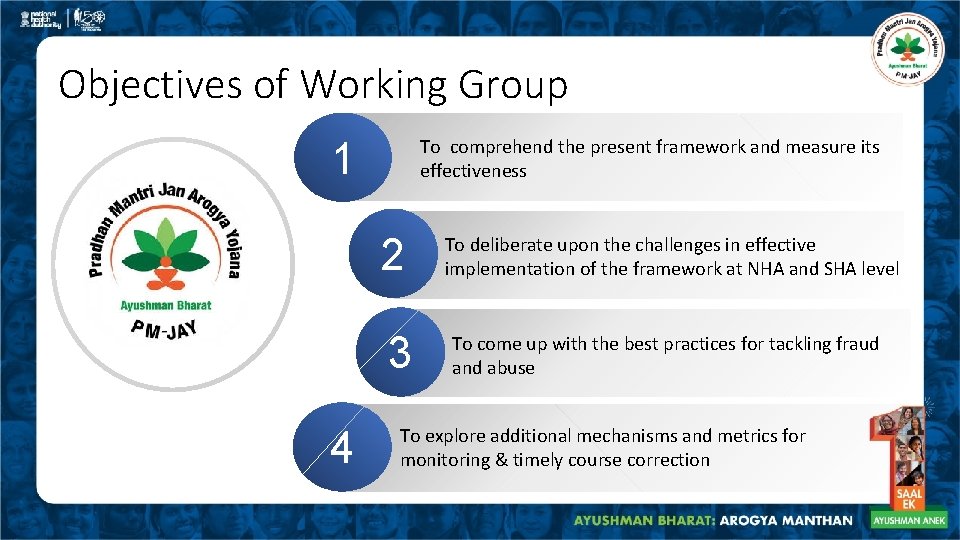
Objectives of Working Group 1 To comprehend the present framework and measure its effectiveness 2 3 4 To deliberate upon the challenges in effective implementation of the framework at NHA and SHA level To come up with the best practices for tackling fraud and abuse To explore additional mechanisms and metrics for monitoring & timely course correction
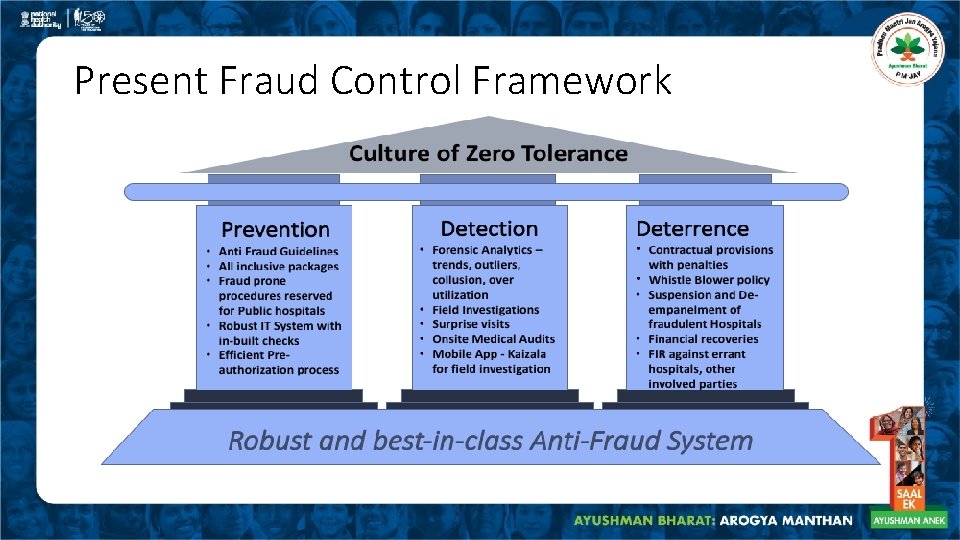
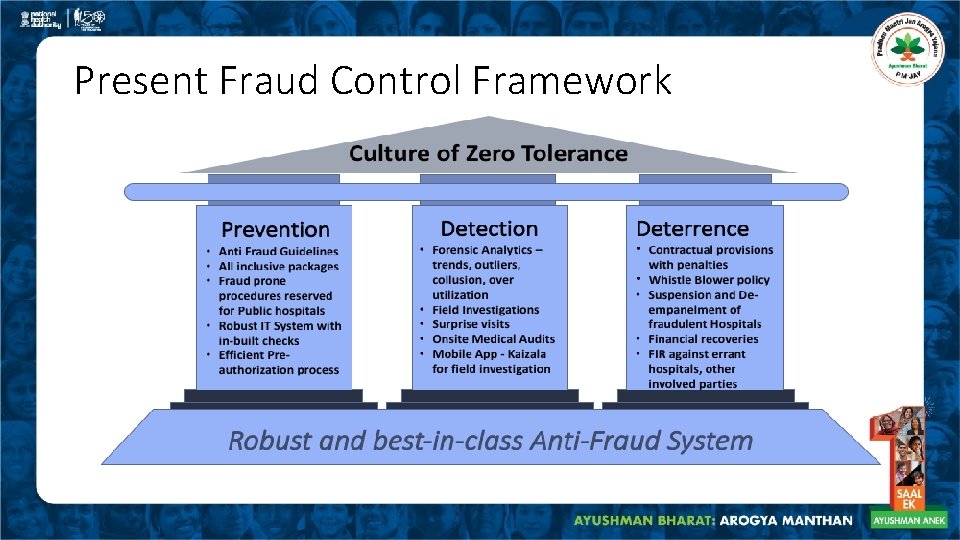
Present Fraud Control Framework
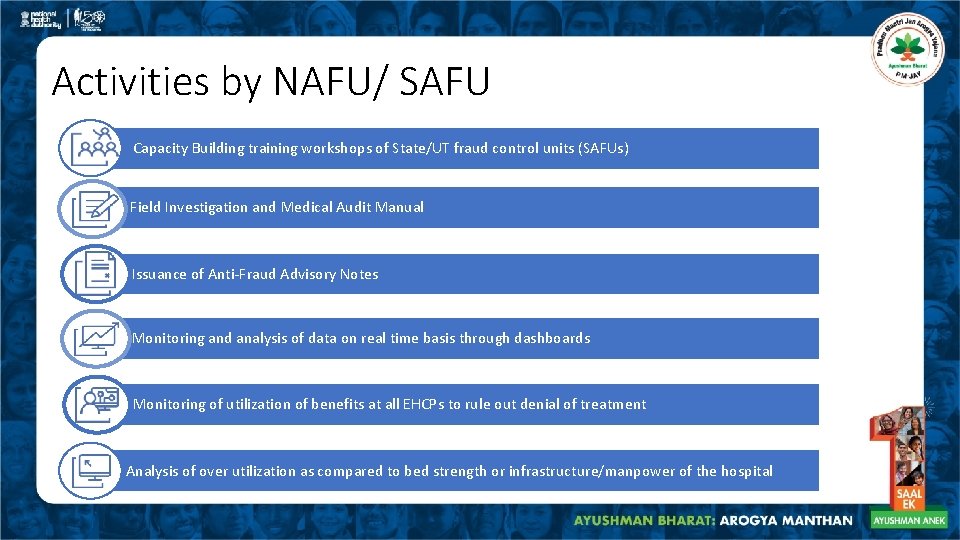
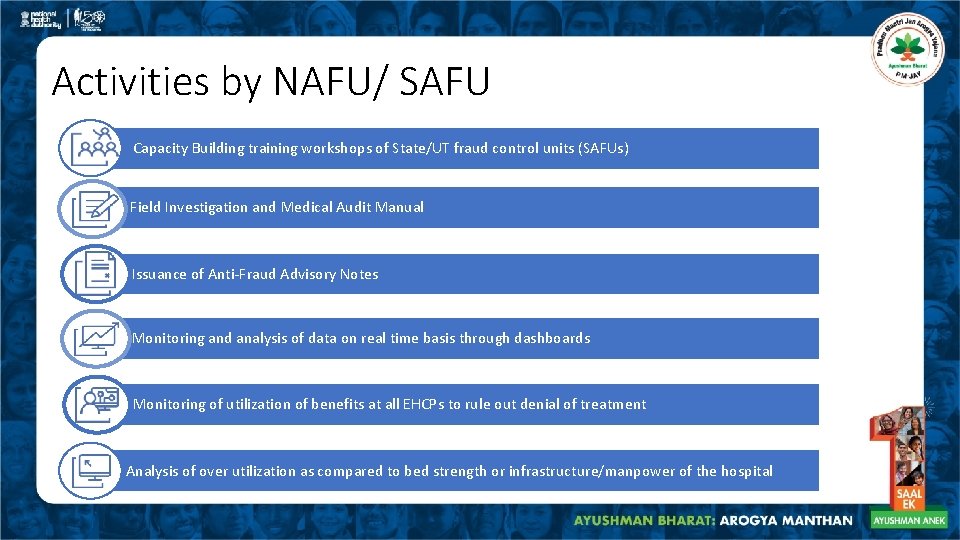
Activities by NAFU/ SAFU Capacity Building training workshops of State/UT fraud control units (SAFUs) Field Investigation and Medical Audit Manual Issuance of Anti-Fraud Advisory Notes Monitoring and analysis of data on real time basis through dashboards Monitoring of utilization of benefits at all EHCPs to rule out denial of treatment Analysis of over utilization as compared to bed strength or infrastructure/manpower of the hospital
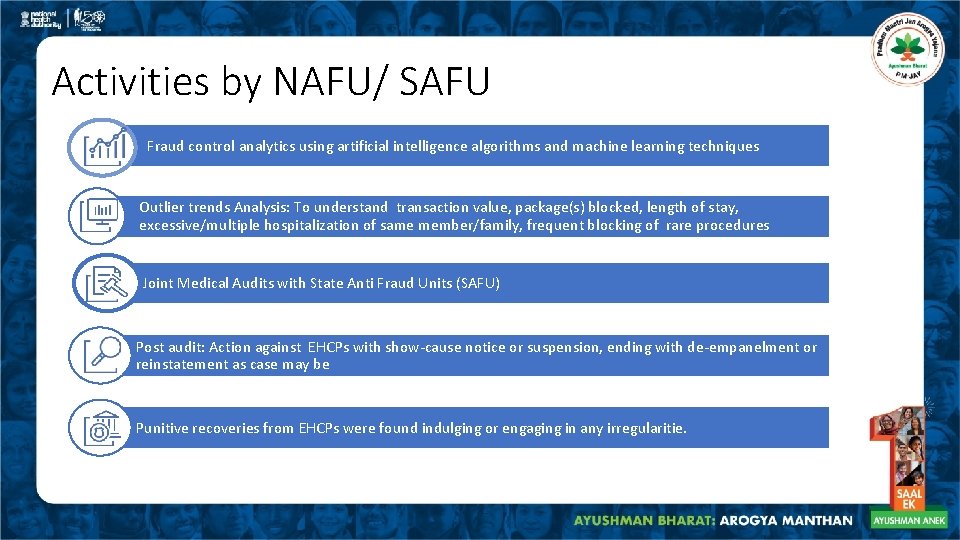
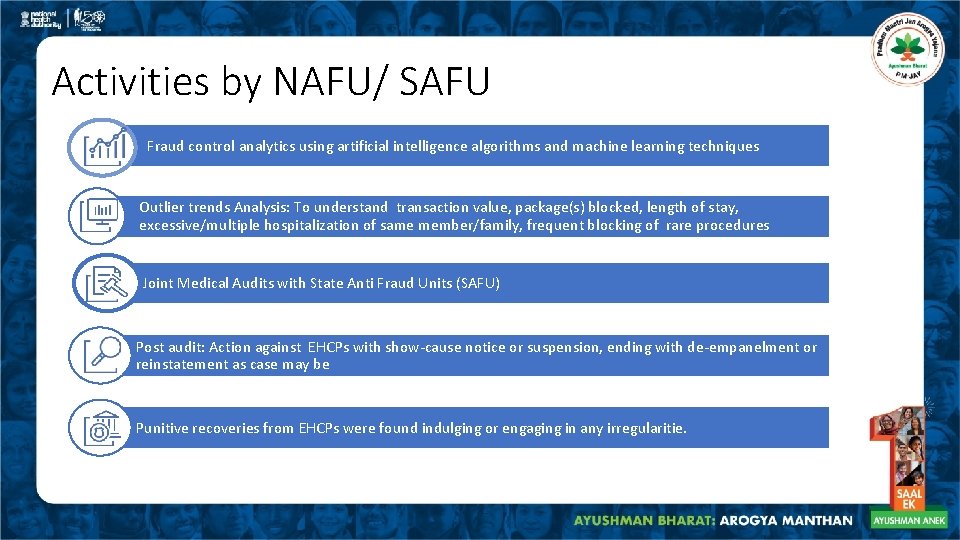
Activities by NAFU/ SAFU Fraud control analytics using artificial intelligence algorithms and machine learning techniques Outlier trends Analysis: To understand transaction value, package(s) blocked, length of stay, excessive/multiple hospitalization of same member/family, frequent blocking of rare procedures Joint Medical Audits with State Anti Fraud Units (SAFU) Post audit: Action against EHCPs with show-cause notice or suspension, ending with de-empanelment or reinstatement as case may be Punitive recoveries from EHCPs were found indulging or engaging in any irregularitie.
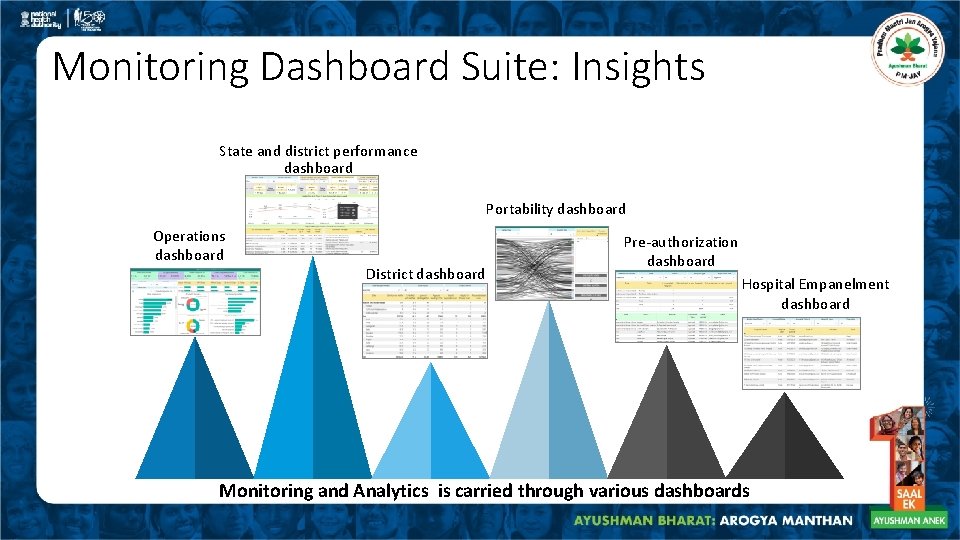
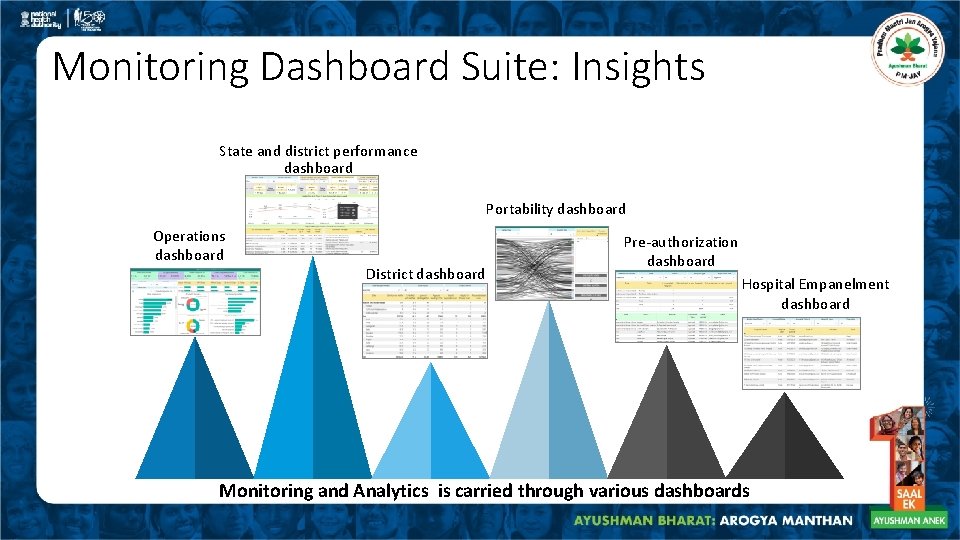
Monitoring Dashboard Suite: Insights State and district performance dashboard Portability dashboard Operations dashboard District dashboard Pre-authorization dashboard Hospital Empanelment dashboard Monitoring and Analytics is carried through various dashboards
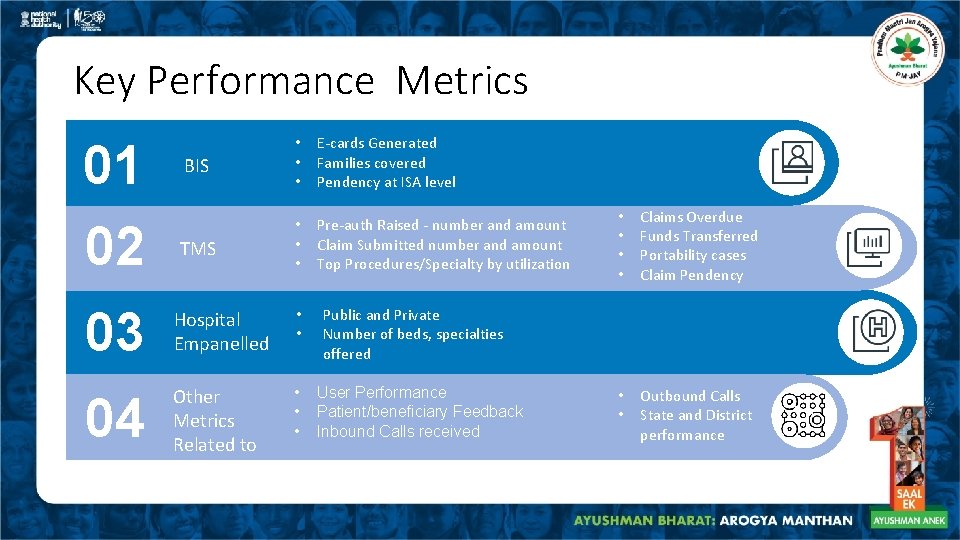
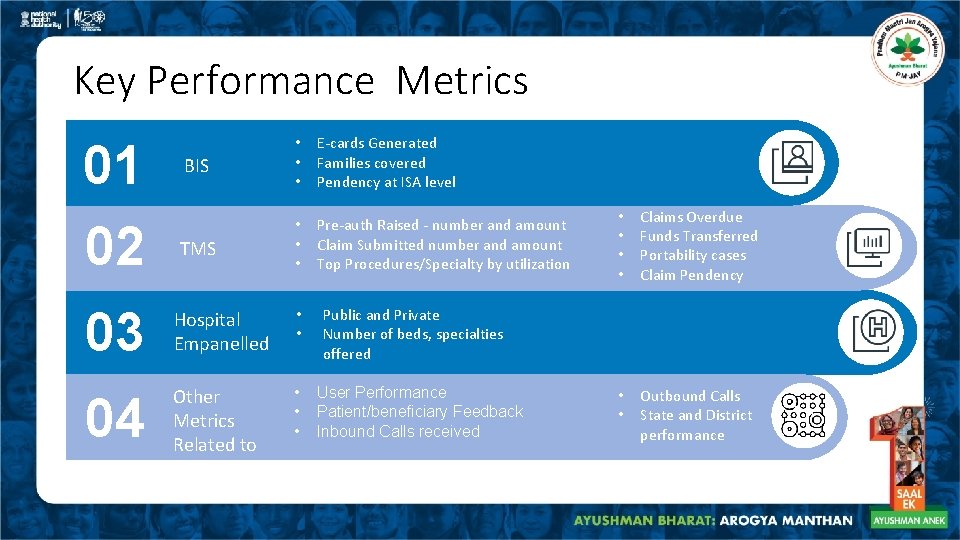
Key Performance Metrics 01 02 BIS • • • E-cards Generated Families covered Pendency at ISA level TMS • • • Pre-auth Raised - number and amount Claim Submitted number and amount Top Procedures/Specialty by utilization 03 Hospital Empanelled • • 04 Other Metrics Related to • • Claims Overdue Funds Transferred Portability cases Claim Pendency • • Outbound Calls State and District performance Public and Private Number of beds, specialties offered User Performance Patient/beneficiary Feedback Inbound Calls received
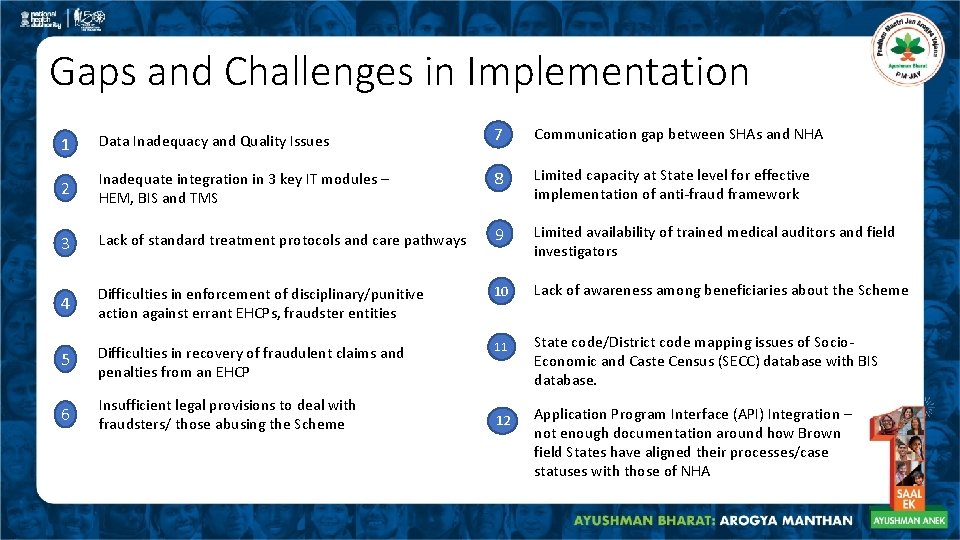
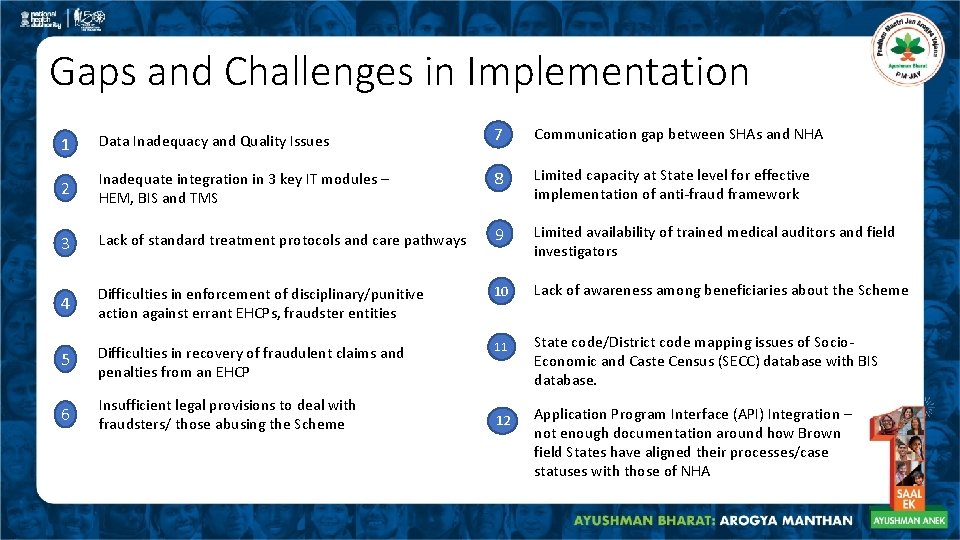
Gaps and Challenges in Implementation 1 Data Inadequacy and Quality Issues 7 Communication gap between SHAs and NHA 2 Inadequate integration in 3 key IT modules – HEM, BIS and TMS 8 Limited capacity at State level for effective implementation of anti-fraud framework 3 Lack of standard treatment protocols and care pathways 9 Limited availability of trained medical auditors and field investigators 4 Difficulties in enforcement of disciplinary/punitive action against errant EHCPs, fraudster entities 10 Lack of awareness among beneficiaries about the Scheme 5 Difficulties in recovery of fraudulent claims and penalties from an EHCP 11 6 Insufficient legal provisions to deal with fraudsters/ those abusing the Scheme 12 State code/District code mapping issues of Socio. Economic and Caste Census (SECC) database with BIS database. Application Program Interface (API) Integration – not enough documentation around how Brown field States have aligned their processes/case statuses with those of NHA
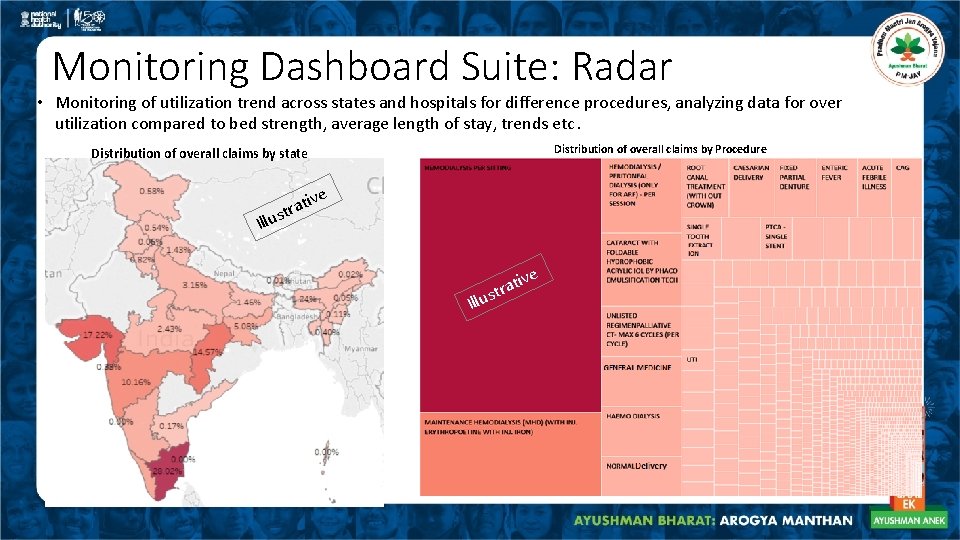
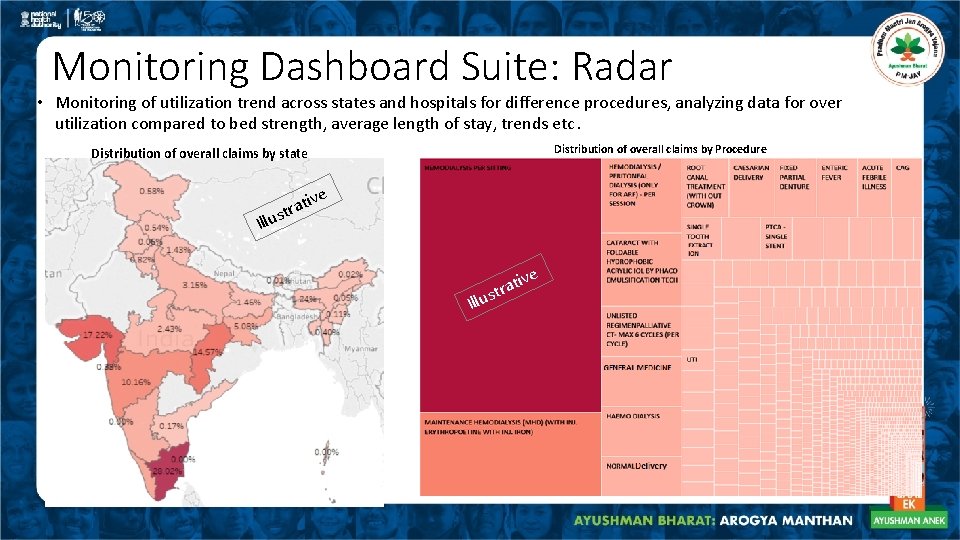
Monitoring Dashboard Suite: Radar • Monitoring of utilization trend across states and hospitals for difference procedures, analyzing data for over utilization compared to bed strength, average length of stay, trends etc. Distribution of overall claims by Procedure Distribution of overall claims by state Illu ve ti a r t s
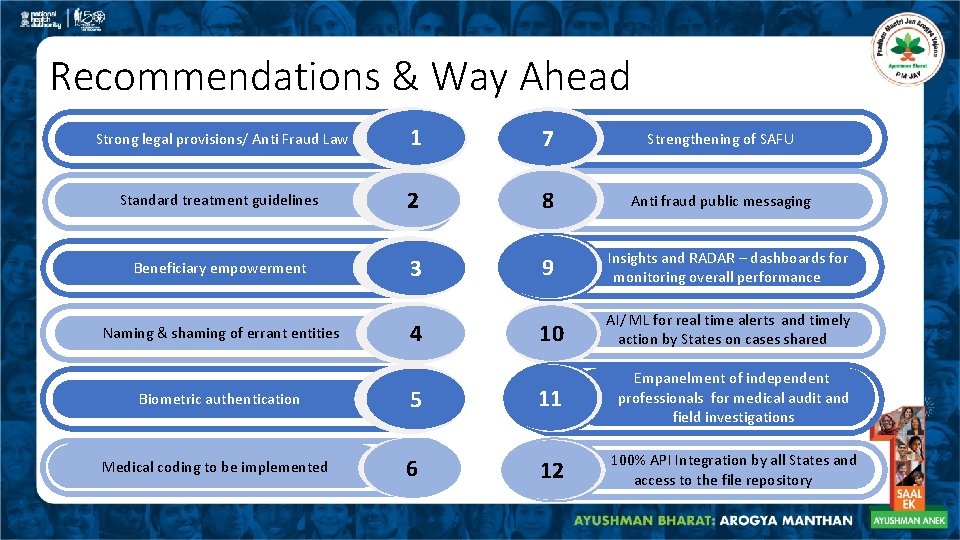
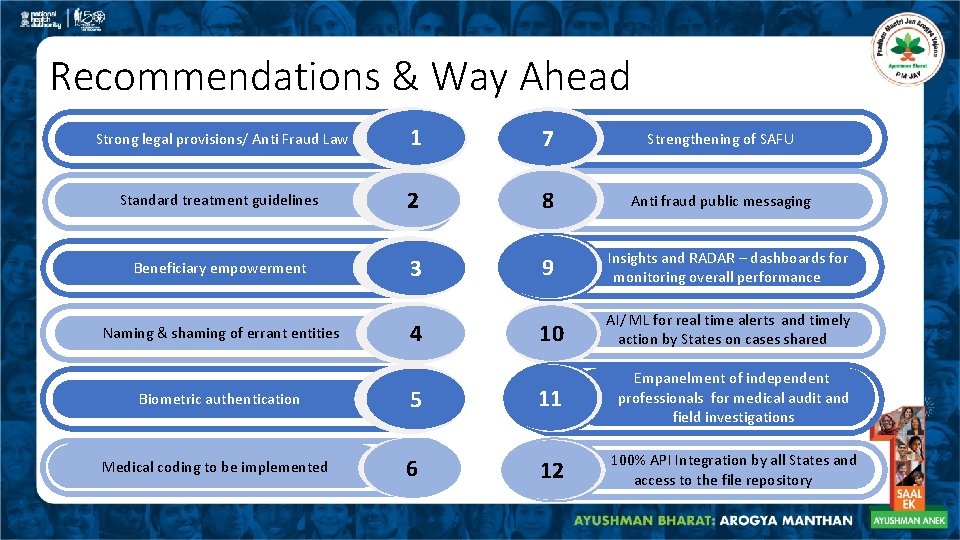
Recommendations & Way Ahead Strong legal provisions/ Anti Fraud Law 1 7 Strengthening of SAFU Standard treatment guidelines 2 8 Anti fraud public messaging Beneficiary empowerment 3 9 Insights and RADAR – dashboards for monitoring overall performance Naming & shaming of errant entities 4 10 AI/ ML for real time alerts and timely action by States on cases shared Biometric authentication 5 11 Empanelment of independent professionals for medical audit and field investigations Medical coding to be implemented 6 12 100% API Integration by all States and access to the file repository
Thank you
Annexures
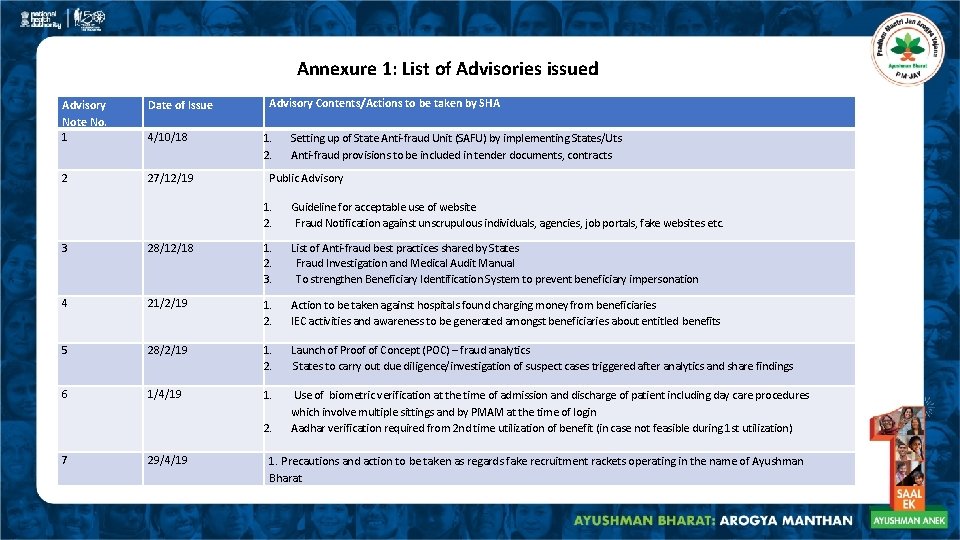
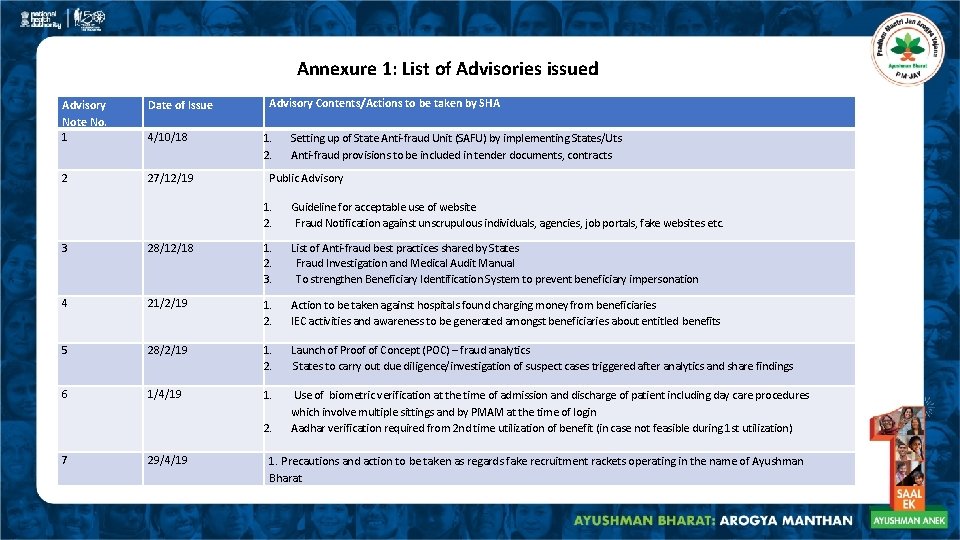
Annexure 1: List of Advisories issued Advisory Contents/Actions to be taken by SHA Advisory Note No. 1 Date of Issue 4/10/18 1. 2. 2 27/12/19 Public Advisory 1. Guideline for acceptable use of website 2. Fraud Notification against unscrupulous individuals, agencies, job portals, fake websites etc. 3 28/12/18 1. List of Anti-fraud best practices shared by States 2. Fraud Investigation and Medical Audit Manual 3. To strengthen Beneficiary Identification System to prevent beneficiary impersonation 4 21/2/19 1. 2. 5 28/2/19 1. Launch of Proof of Concept (POC) – fraud analytics 2. States to carry out due diligence/investigation of suspect cases triggered after analytics and share findings 6 1/4/19 1. 2. 7 29/4/19 Setting up of State Anti-fraud Unit (SAFU) by implementing States/Uts Anti-fraud provisions to be included in tender documents, contracts Action to be taken against hospitals found charging money from beneficiaries IEC activities and awareness to be generated amongst beneficiaries about entitled benefits Use of biometric verification at the time of admission and discharge of patient including day care procedures which involve multiple sittings and by PMAM at the time of login Aadhar verification required from 2 nd time utilization of benefit (in case not feasible during 1 st utilization) 1. Precautions and action to be taken as regards fake recruitment rackets operating in the name of Ayushman Bharat
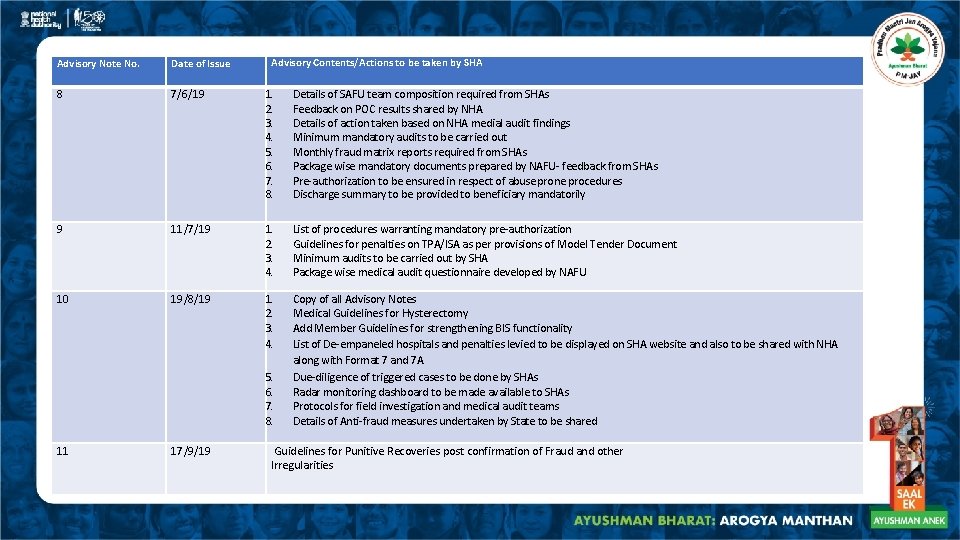
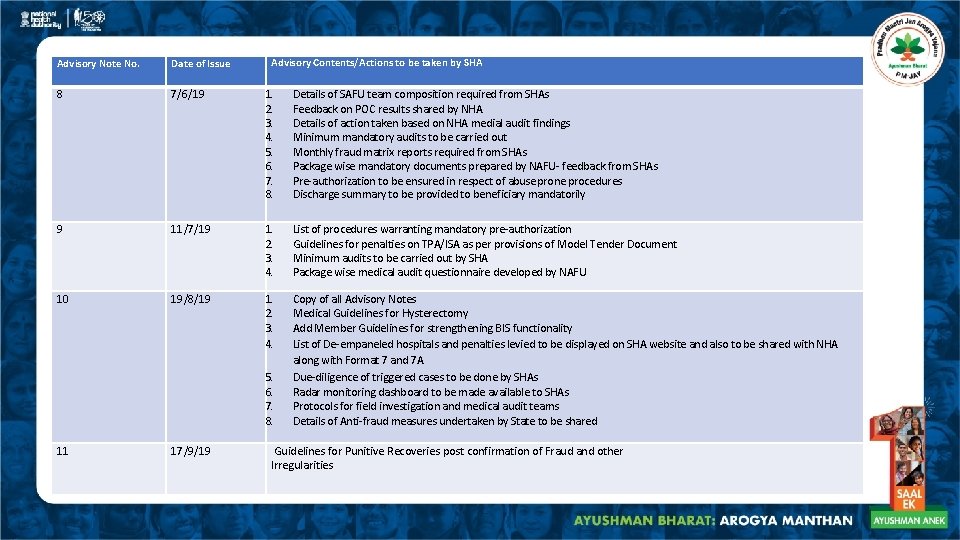
Advisory Contents/Actions to be taken by SHA Advisory Note No. Date of Issue 8 7/6/19 1. 2. 3. 4. 5. 6. 7. 8. Details of SAFU team composition required from SHAs Feedback on POC results shared by NHA Details of action taken based on NHA medial audit findings Minimum mandatory audits to be carried out Monthly fraud matrix reports required from SHAs Package wise mandatory documents prepared by NAFU- feedback from SHAs Pre-authorization to be ensured in respect of abuse prone procedures Discharge summary to be provided to beneficiary mandatorily 9 11/7/19 1. 2. 3. 4. List of procedures warranting mandatory pre-authorization Guidelines for penalties on TPA/ISA as per provisions of Model Tender Document Minimum audits to be carried out by SHA Package wise medical audit questionnaire developed by NAFU 10 19/8/19 1. 2. 3. 4. Copy of all Advisory Notes Medical Guidelines for Hysterectomy Add Member Guidelines for strengthening BIS functionality List of De-empaneled hospitals and penalties levied to be displayed on SHA website and also to be shared with NHA along with Format 7 and 7 A Due-diligence of triggered cases to be done by SHAs Radar monitoring dashboard to be made available to SHAs Protocols for field investigation and medical audit teams Details of Anti-fraud measures undertaken by State to be shared 5. 6. 7. 8. 11 17/9/19 Guidelines for Punitive Recoveries post confirmation of Fraud and other Irregularities
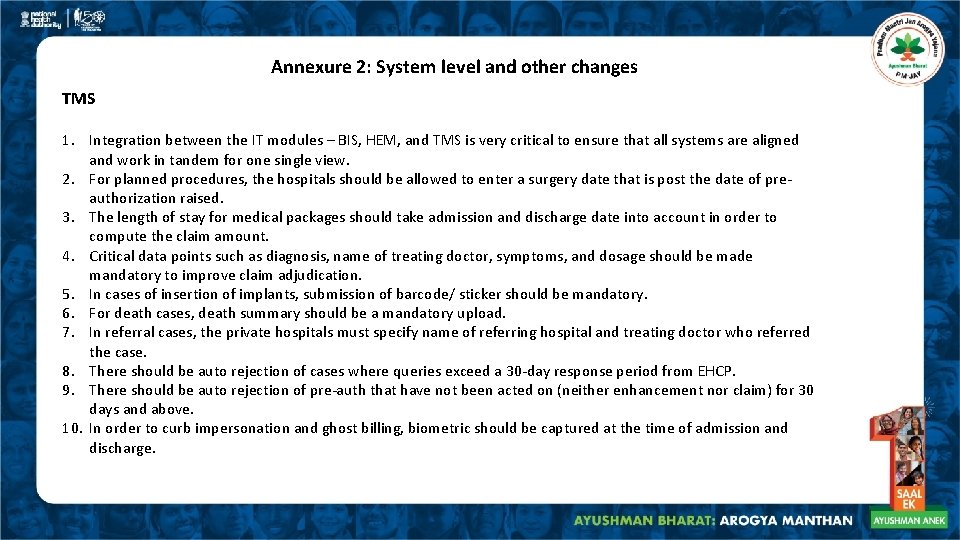
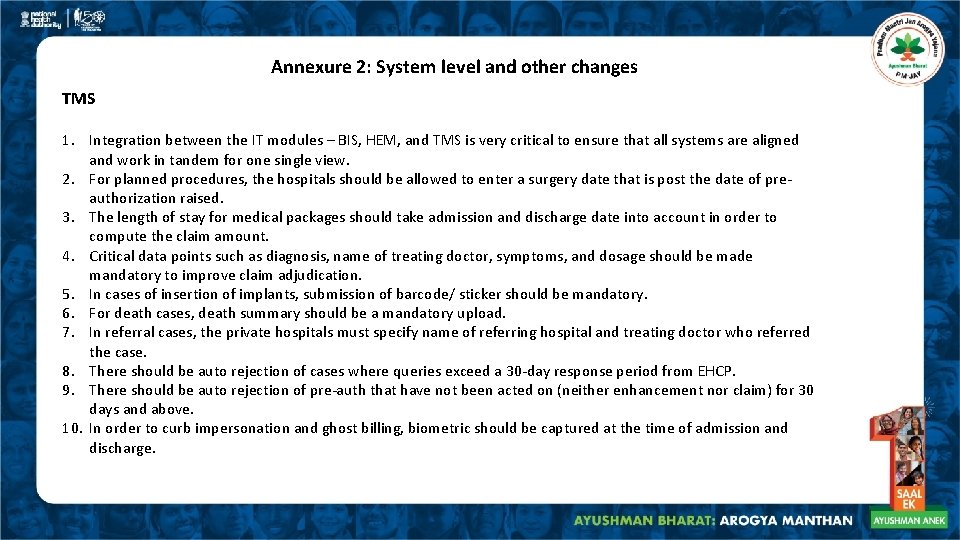
Annexure 2: System level and other changes TMS 1. Integration between the IT modules – BIS, HEM, and TMS is very critical to ensure that all systems are aligned and work in tandem for one single view. 2. For planned procedures, the hospitals should be allowed to enter a surgery date that is post the date of preauthorization raised. 3. The length of stay for medical packages should take admission and discharge date into account in order to compute the claim amount. 4. Critical data points such as diagnosis, name of treating doctor, symptoms, and dosage should be made mandatory to improve claim adjudication. 5. In cases of insertion of implants, submission of barcode/ sticker should be mandatory. 6. For death cases, death summary should be a mandatory upload. 7. In referral cases, the private hospitals must specify name of referring hospital and treating doctor who referred the case. 8. There should be auto rejection of cases where queries exceed a 30 -day response period from EHCP. 9. There should be auto rejection of pre-auth that have not been acted on (neither enhancement nor claim) for 30 days and above. 10. In order to curb impersonation and ghost billing, biometric should be captured at the time of admission and discharge.
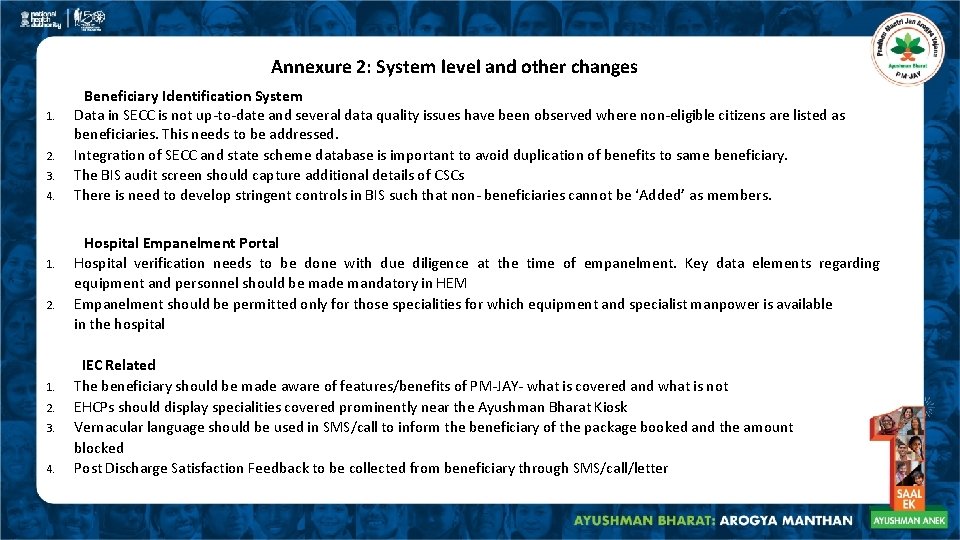
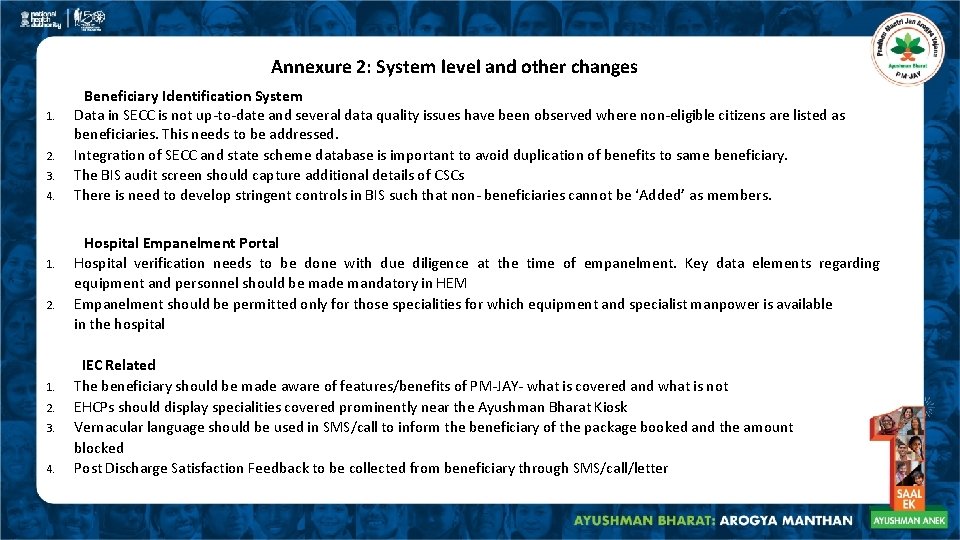
Annexure 2: System level and other changes 1. 2. 3. 4. 1. 2. Beneficiary Identification System Data in SECC is not up-to-date and several data quality issues have been observed where non-eligible citizens are listed as beneficiaries. This needs to be addressed. Integration of SECC and state scheme database is important to avoid duplication of benefits to same beneficiary. The BIS audit screen should capture additional details of CSCs There is need to develop stringent controls in BIS such that non- beneficiaries cannot be ‘Added’ as members. Hospital Empanelment Portal Hospital verification needs to be done with due diligence at the time of empanelment. Key data elements regarding equipment and personnel should be made mandatory in HEM Empanelment should be permitted only for those specialities for which equipment and specialist manpower is available in the hospital IEC Related 1. The beneficiary should be made aware of features/benefits of PM-JAY- what is covered and what is not 2. EHCPs should display specialities covered prominently near the Ayushman Bharat Kiosk 3. Vernacular language should be used in SMS/call to inform the beneficiary of the package booked and the amount blocked 4. Post Discharge Satisfaction Feedback to be collected from beneficiary through SMS/call/letter
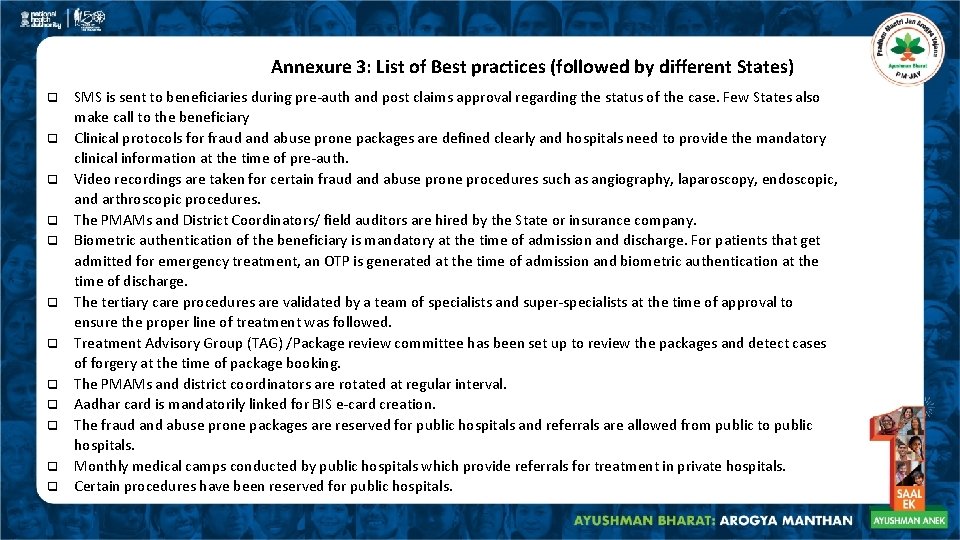
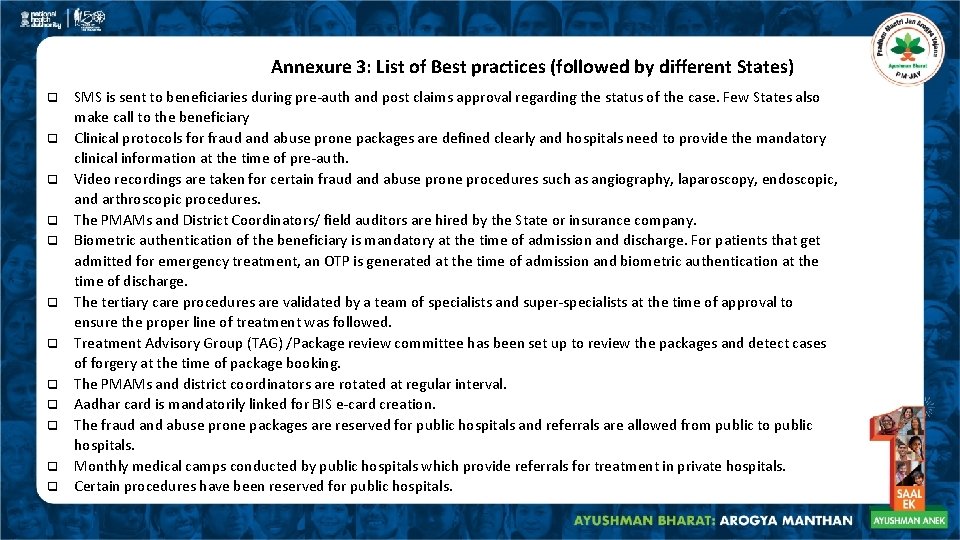
Annexure 3: List of Best practices (followed by different States) q q q SMS is sent to beneficiaries during pre-auth and post claims approval regarding the status of the case. Few States also make call to the beneficiary Clinical protocols for fraud and abuse prone packages are defined clearly and hospitals need to provide the mandatory clinical information at the time of pre-auth. Video recordings are taken for certain fraud and abuse prone procedures such as angiography, laparoscopy, endoscopic, and arthroscopic procedures. The PMAMs and District Coordinators/ field auditors are hired by the State or insurance company. Biometric authentication of the beneficiary is mandatory at the time of admission and discharge. For patients that get admitted for emergency treatment, an OTP is generated at the time of admission and biometric authentication at the time of discharge. The tertiary care procedures are validated by a team of specialists and super-specialists at the time of approval to ensure the proper line of treatment was followed. Treatment Advisory Group (TAG) /Package review committee has been set up to review the packages and detect cases of forgery at the time of package booking. The PMAMs and district coordinators are rotated at regular interval. Aadhar card is mandatorily linked for BIS e-card creation. The fraud and abuse prone packages are reserved for public hospitals and referrals are allowed from public to public hospitals. Monthly medical camps conducted by public hospitals which provide referrals for treatment in private hospitals. Certain procedures have been reserved for public hospitals.
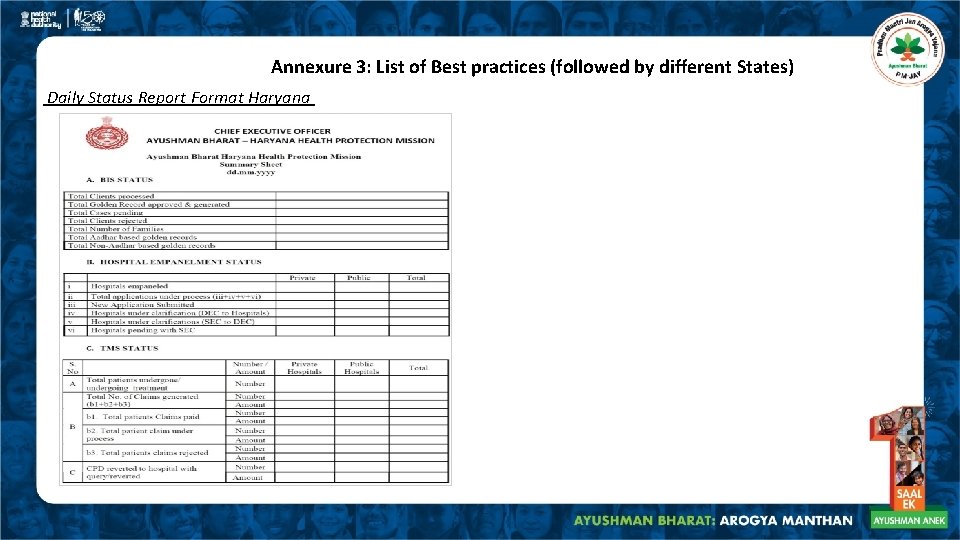
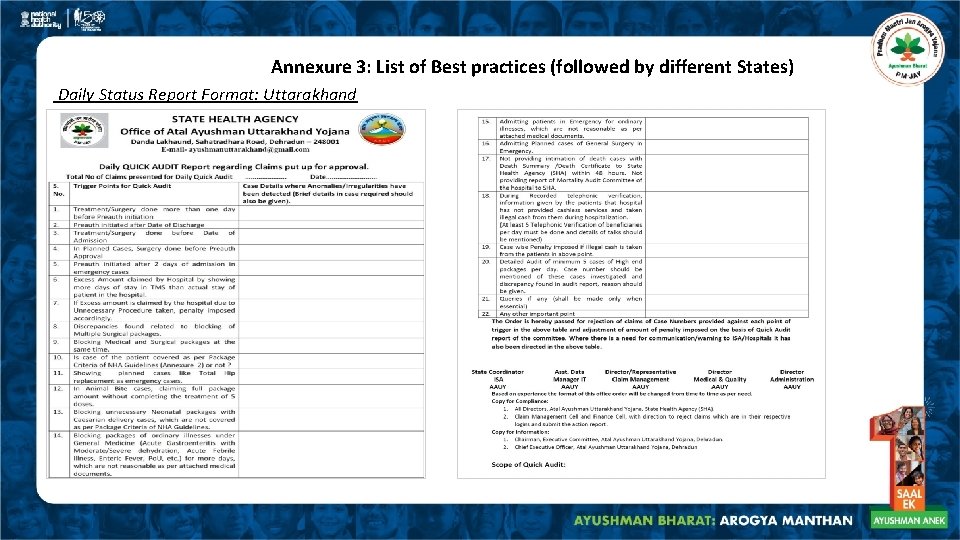
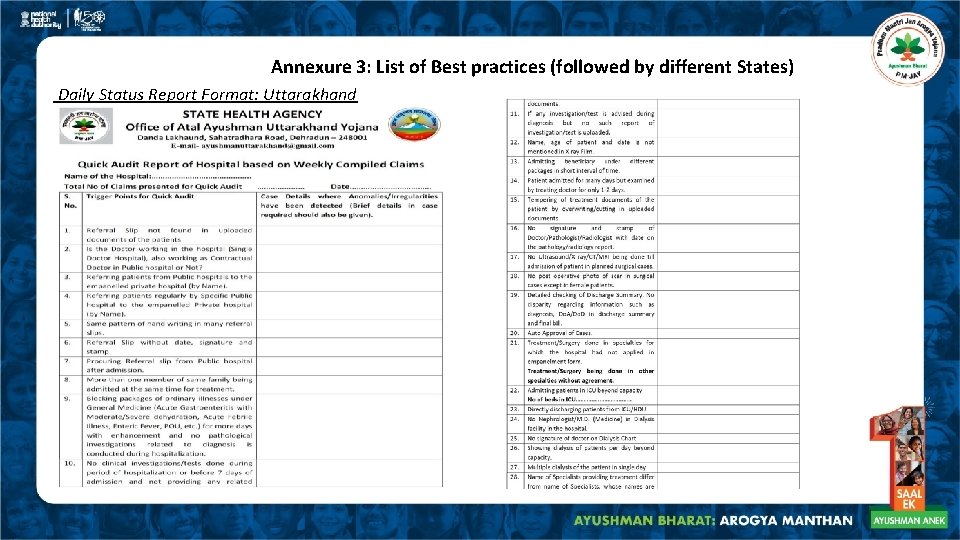
Annexure 3: List of Best practices (followed by different States) q q q q q Certain procedures have been reserved for public hospitals. The capacity of public hospitals is mapped in to measure bed strength, manpower, etc. and only then referrals are approved to private hospitals. Referral by public hospital is mandatory for treatment at private hospital except in case of emergency. Random physical verification of claims is done through State/District Medical Cell. Standing medical committee of SHA/IC/ISA is set up for approval of unspecified cases of high value Mandatory cross checking of TMS data and documents uploaded by EHCPs, quick audit check list is used before approval of each claim. Specific triggers are used to identify potential fraud cases The un-specified procedures are prone to abuse by private hospitals. For instance, packages reserved for public hospitals may booked as unspecified packages by private hospitals, few States have developed guidelines for the same. Some states have created a daily status report format for regular monitoring of the scheme. A few examples from States such as Haryana and Uttarakhand are show in the next slides
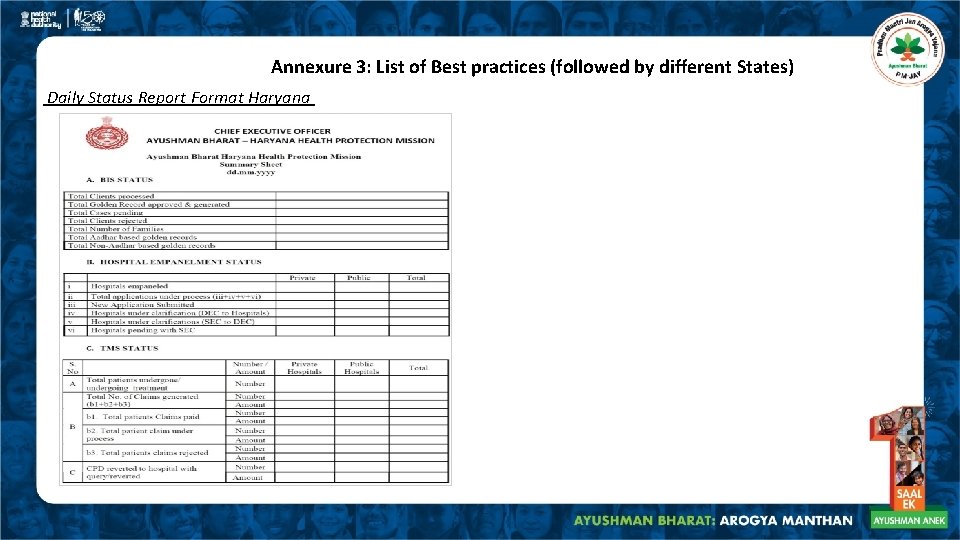
Annexure 3: List of Best practices (followed by different States) Daily Status Report Format Haryana
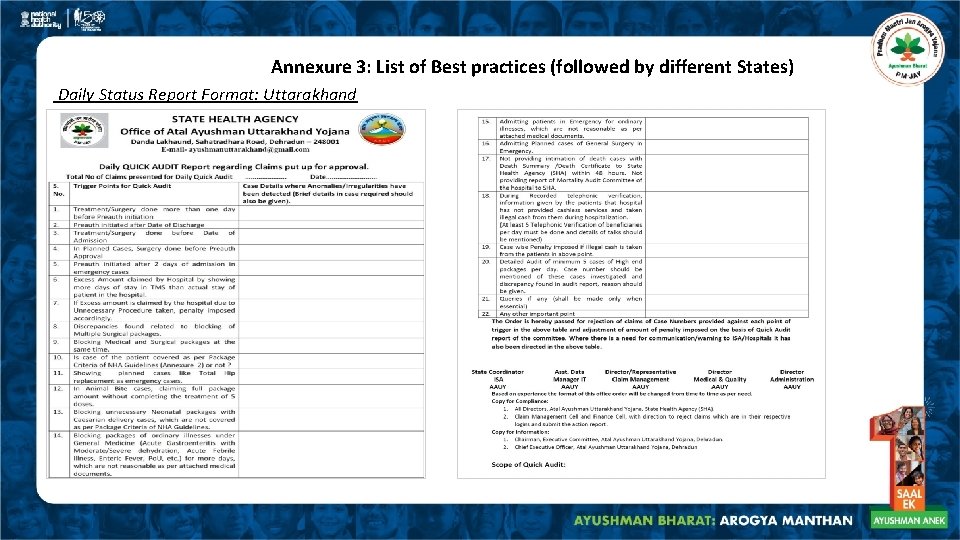
Annexure 3: List of Best practices (followed by different States) Daily Status Report Format: Uttarakhand
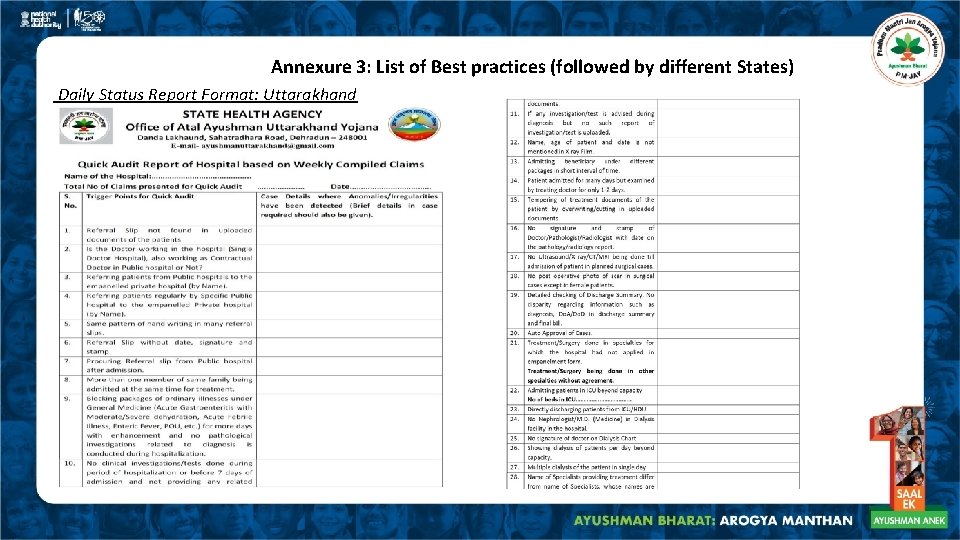
Annexure 3: List of Best practices (followed by different States) Daily Status Report Format: Uttarakhand
 How do fraud symptoms help in detecting fraud
How do fraud symptoms help in detecting fraud Suvarna arogya suraksha trust hospital list
Suvarna arogya suraksha trust hospital list Suvarna arogya suraksha trust hospital list
Suvarna arogya suraksha trust hospital list Dmhp trivandrum
Dmhp trivandrum Mahila arogya samiti
Mahila arogya samiti Fraud monitoring report
Fraud monitoring report Hot working and cold working difference
Hot working and cold working difference Hot working and cold working
Hot working and cold working Machining operations
Machining operations Proses pembentukan logam
Proses pembentukan logam Smart vs hard working
Smart vs hard working Ecommerce security issues
Ecommerce security issues Verifyny
Verifyny Fraud and abuse module
Fraud and abuse module E commerce security and fraud protection
E commerce security and fraud protection E-commerce security and fraud protection
E-commerce security and fraud protection Computer fraud and abuse techniques
Computer fraud and abuse techniques Sas 78/coso
Sas 78/coso Anti bribery and corruption analytics
Anti bribery and corruption analytics Fraud, internal control, and cash
Fraud, internal control, and cash Ethics and internal controls in accounting
Ethics and internal controls in accounting Fraud waste and abuse training answers
Fraud waste and abuse training answers Fraud waste and abuse training answers
Fraud waste and abuse training answers Computer fraud and security
Computer fraud and security Difference between fraud and misrepresentation
Difference between fraud and misrepresentation