Anxiety Disorders Pharmacy department East London NHS Foundation




- Slides: 36
Anxiety Disorders Pharmacy department East London NHS Foundation Trust Page 1
Teaching / Learning Objectives • To define anxiety • To have a knowledge of the main pharmacological agents used in the treatment of anxiety • To have an appreciation of the NICE Guidelines (UK) on the treatment of anxiety disorders
Anxiety • Anxiety – normal but unpleasant emotional state • Natural, usually self limiting emotion • Varies in degree from mild unease to intense dread • Subjectively intolerable and disabling anxiety – pathological – treatment • Anxiety disorder will affect approx 1 in 5 people in UK at some point during their adult lives. • Psychological or physical symptoms

Anxiety – symptoms (Diagnosis can be difficult!) • Psychological poor concentration, bad dreams, night terrors, insomnia, restlessness, sensitivity to noise, fear, irritability, feeling worried all the time, avoidance or loss of interest in others • Physical throbbing neck, nausea, epigastric pain, indigestion, chills, poor appetite, trembling, palpitations, sweating, butterflies in stomach, hot flushes, tingling in hands and feet, feeling faint or dizziness, frequent diarrhoea for no reason, pain over heart • Respiratory tightness over the chest, difficulty inhaling, dizziness, breathlessness, faintness • Musculoskeletal Backache, headache, neck ache, shoulder pain, muscle tension
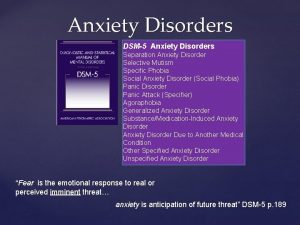
Anxiety - Types • Generalised anxiety disorder (GAD) • Phobic disorders (specific phobia, Social phobia) • Panic disorders • Obsessive Compulsive Disorders (OCD) • Mixed Anxiety and Depression (MAD) • Post Traumatic Stress Disorder (PTSD)
• Differentiation between the disorders is difficult and co-morbidity is very common. • Co-morbidity might be with other anxiety disorders or depression and other affective (mood) disorders East London NHS Foundation Trust 6
Generalised Anxiety Disorder (GAD) • A persistent, excessive anxiety, apprehension or inappropriate worry present for at least 6 months • Physical symptoms include restlessness, fatigue, difficulty concentrating, irritability, muscle tension, disturbed sleep • Chronic condition with acute episodes ~peaks and higher peaks • Often begins in early adulthood • Twice as common in women than men East London NHS Foundation Trust 7
Panic disorder • Repeated unpredictable attacks of severe anxiety occurring without warning and unrelated to a specific situation • Can peak within 10 minutes with many somatic / physical symptoms, duration around 30 -45 minutes • Anticipatory fear of having another attack • Panic attacks are discrete periods of intense fear or discomfort, accompanied by multiple physical or psychological anxiety symptoms East London NHS Foundation Trust 8
Phobic Disorders • Irrational fear out of all proportion to a situation or object • Sub-divided – agoraphobia – social phobia – specific phobia East London NHS Foundation Trust 9
Obsessive Compulsive Disorder • A time consuming obsession (the thoughts that make you anxious) and compulsion (the things you do to reduce your anxiety) which interferes with a person’s day to day functioning, work or relationship • OCD is characterised by recurrent obsessive ruminations, and/or physical or mental rituals • If compulsion is resisted anxiety levels are increased • Life time prevalence of 2% • Males and females equally affected East London NHS Foundation Trust 10
Post Traumatic Stress Disorder • PTSD is characterise by a history of exposure to trauma • Intense and prolonged and sometimes delayed response to a particular trauma • Characterised by emotional numbness, detachment, flashbacks, recurring memories and vivid dreams. • Do not have to be personally involved can be a bystander or rescue worker East London NHS Foundation Trust 11
Mixed disorders • Both anxiety and depression present East London NHS Foundation Trust 12
Treatment options Discuss in a full and frank manner with the patient and his/her family/ carers etc and give the following menu: �� Psychological therapy �� Pharmacological therapy �� Self-help East London NHS Foundation Trust 13
Before medication is considered. . . 1. Is the anxiety harmful? 2. Check other potential comorbid disorders 3. Will the medication under consideration produce unwanted side effects? 4. For how long will the medication be required? 5. Will it be effective? 6. Will it produce dependence – is it likely to be abused? 7. Would non- pharmacological strategies be more appropriate?

Good things about medicines • Rapid symptomatic relief • May improve compliance with psychological treatment Not so good things about medicines • Rapid symptomatic relief – non-compliance with psychological treatment • Impaired learning, memory and concentration which is required for psychological treatment • Dependence on prescriber to “Cure” – reduced responsibility for their own involvement
Management of anxiety disorders General Management: �� Shared decision making between the patient and individual promotes concordance and optimises outcomes �� Appropriate and usable information should be given to patients, carers, family members etc; medication information must be included �� Patient’s families etc should be informed of all appropriate self-help, support groups etc. East London NHS Foundation Trust 16
Treatment • Presence of coexisting depressive symptoms, often guide treatment choice towards antidepressant rather than BDZ • It should be emphasised treatment response is not immediate East London NHS Foundation Trust Page 17

Treatment duration As with depression… • First episode : 6 months • Recurrent : 1 -2 years
Ideal Drug • • • Effective in all anxiety disorders Quick acting Long lasting Licensed for all Anxiety Disorders Not be too sedating Address the full range of symptoms Not cause tolerance/dependence Have no abuse potential No interaction with food/drug/alcohol No side effects Safe in overdose Effective in preventing relapse Does this exist? --- No…
Which Drugs? • Benzodiazepines • Antidepressants • B-Blockers • Antipsychotics • Antihistamines East London NHS Foundation Trust Page 20
Benzodiazepines �� Indicated for the short term relief (2 -4 weeks only) of anxiety that is severe and disabling. Use for mild anxiety is inappropriate and unsuitable �� Useful for immediate action while awaiting other treatment to work ~ eg: Antidepressant, CBT, IPT, ‘flooding’ / exposure etc �� Respiratory depression can occur at high dose (How is this treated in an emergency situation? ) East London NHS Foundation Trust 21
Benzodiazepine Side Effects • Sedation/ light headedness the next day • Confusion • Dependence • Paradoxical increase in aggression • Ataxia esp. in the elderly East London NHS Foundation Trust 22
Benzodiazepines • Examples - Diazepam – long acting - Lorazepam – short acting useful in elderly, hepatic impairment East London NHS Foundation Trust 23
SSRIs �� Response may take up to 4 to 6 weeks and the full response may take 12 weeks’. �� First episode up to 6 months �� Recurrent: 1 to 2 years or more �� 40% of patients ‘activation syndrome’ East London NHS Foundation Trust 24
SSRI side effects • Anticholinergic • Nausea • Sexual dysfunction • Weight gain • Hyponatraemia • Serotonin syndrome East London NHS Foundation Trust 25
Other treatments: • Beta Blockers – only treat physical symptoms • Antihistamines – alternative to benzodiazepines, less habit-forming • Buspirone – complex mode of action, takes time to work • Tricyclic Antidepressants – e. g. clomipramine, many adverse effects • MAOIs – for resistant cases • Antipsychotics – emotional blunting? East London NHS Foundation Trust 26

Summary of NICE guidelines for the Treatment of GAD, Panic Disorder & OCD • Psychological therapy and pharmacological therapy have broadly similar efficacy in acute treatment • Psychological therapy should be used 1 st line. • Take account of Pt clinical features, needs, preferences, and local service availability in when choosing treatment • Pharmacological therapy is also effective. Most evidence supports the use of SSRIs East London NHS Foundation Trust 27
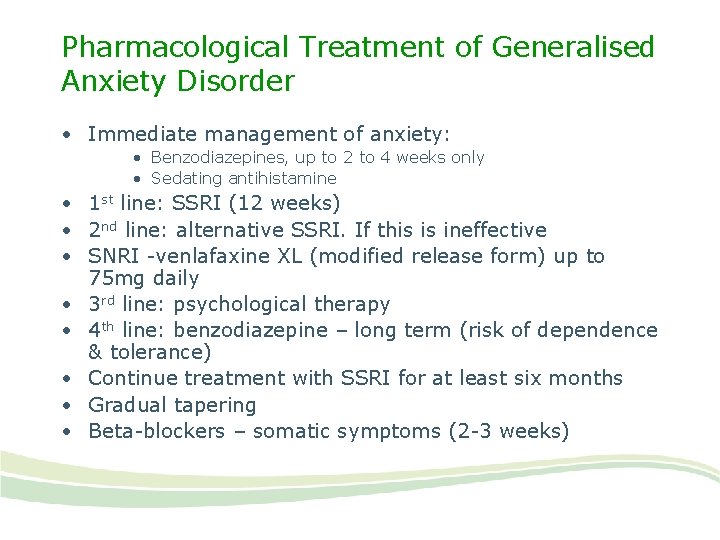
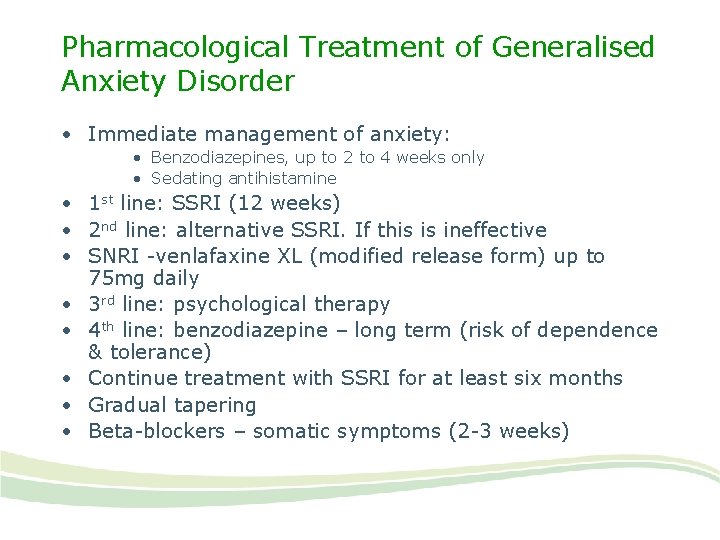
Pharmacological Treatment of Generalised Anxiety Disorder • Immediate management of anxiety: • Benzodiazepines, up to 2 to 4 weeks only • Sedating antihistamine • 1 st line: SSRI (12 weeks) • 2 nd line: alternative SSRI. If this is ineffective • SNRI -venlafaxine XL (modified release form) up to 75 mg daily • 3 rd line: psychological therapy • 4 th line: benzodiazepine – long term (risk of dependence & tolerance) • Continue treatment with SSRI for at least six months • Gradual tapering • Beta-blockers – somatic symptoms (2 -3 weeks)
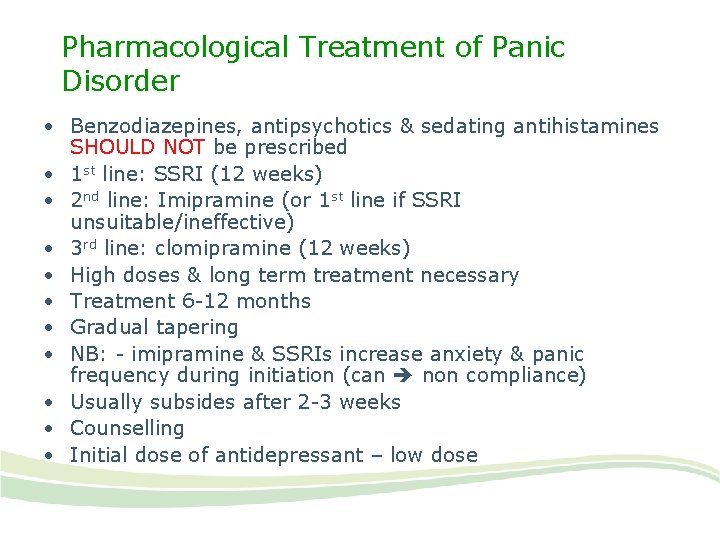
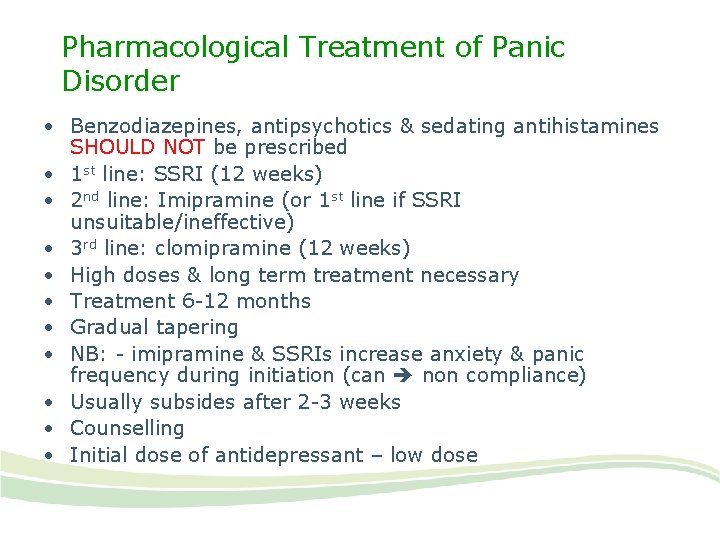
Pharmacological Treatment of Panic Disorder • Benzodiazepines, antipsychotics & sedating antihistamines SHOULD NOT be prescribed • 1 st line: SSRI (12 weeks) • 2 nd line: Imipramine (or 1 st line if SSRI unsuitable/ineffective) • 3 rd line: clomipramine (12 weeks) • High doses & long term treatment necessary • Treatment 6 -12 months • Gradual tapering • NB: - imipramine & SSRIs increase anxiety & panic frequency during initiation (can non compliance) • Usually subsides after 2 -3 weeks • Counselling • Initial dose of antidepressant – low dose
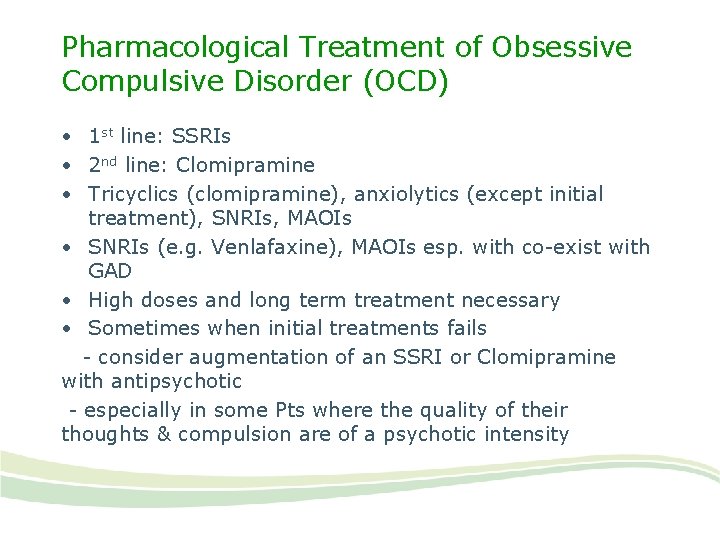
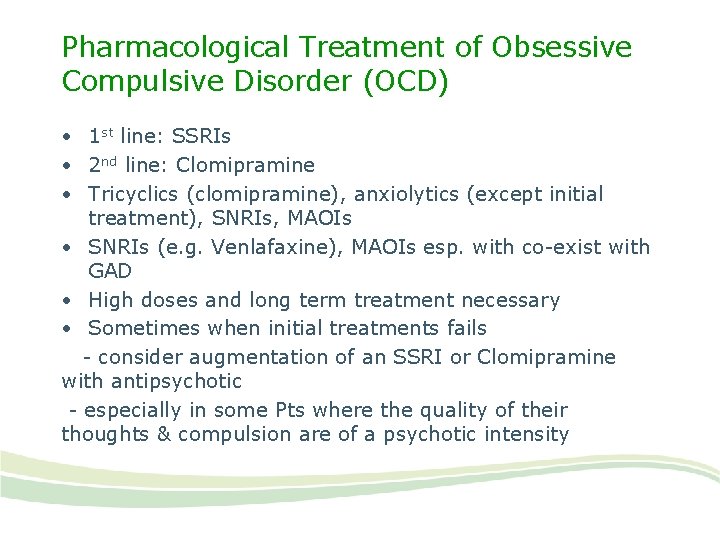
Pharmacological Treatment of Obsessive Compulsive Disorder (OCD) • 1 st line: SSRIs • 2 nd line: Clomipramine • Tricyclics (clomipramine), anxiolytics (except initial treatment), SNRIs, MAOIs • SNRIs (e. g. Venlafaxine), MAOIs esp. with co-exist with GAD • High doses and long term treatment necessary • Sometimes when initial treatments fails - consider augmentation of an SSRI or Clomipramine with antipsychotic - especially in some Pts where the quality of their thoughts & compulsion are of a psychotic intensity
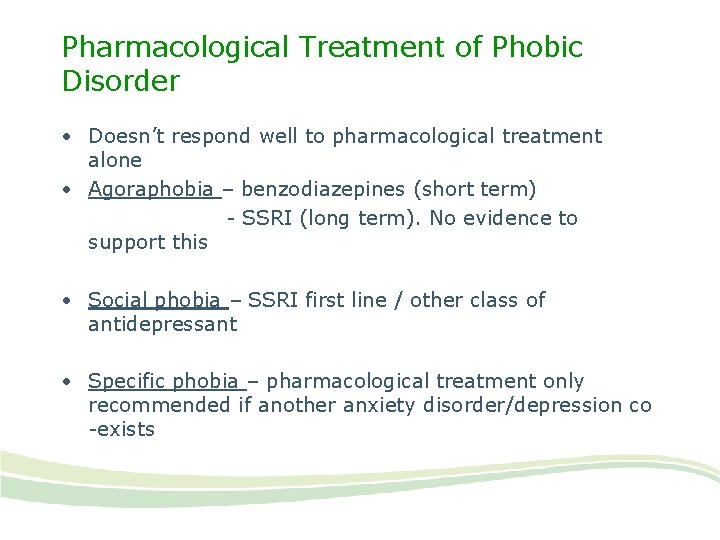
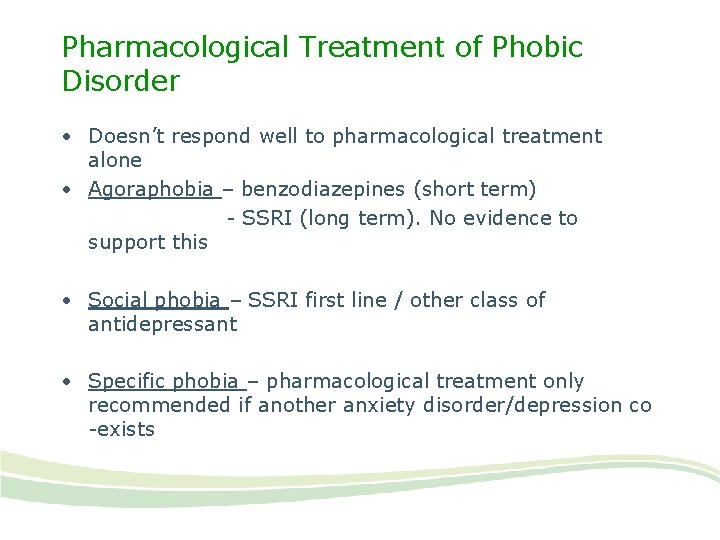
Pharmacological Treatment of Phobic Disorder • Doesn’t respond well to pharmacological treatment alone • Agoraphobia – benzodiazepines (short term) - SSRI (long term). No evidence to support this • Social phobia – SSRI first line / other class of antidepressant • Specific phobia – pharmacological treatment only recommended if another anxiety disorder/depression co -exists
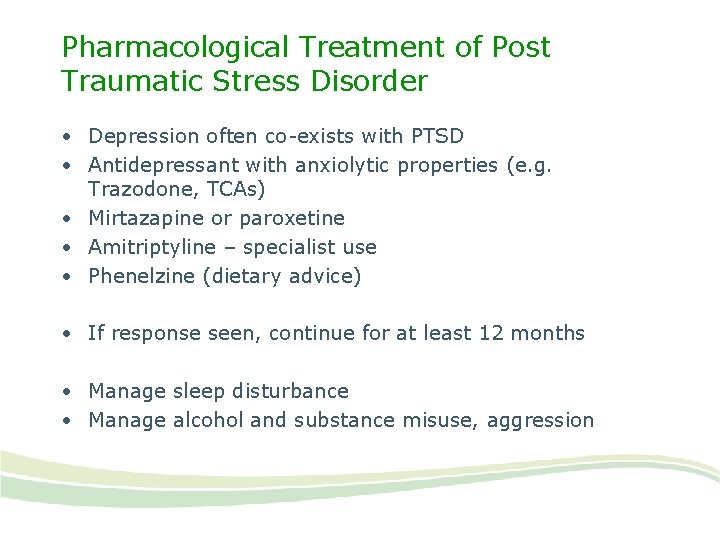
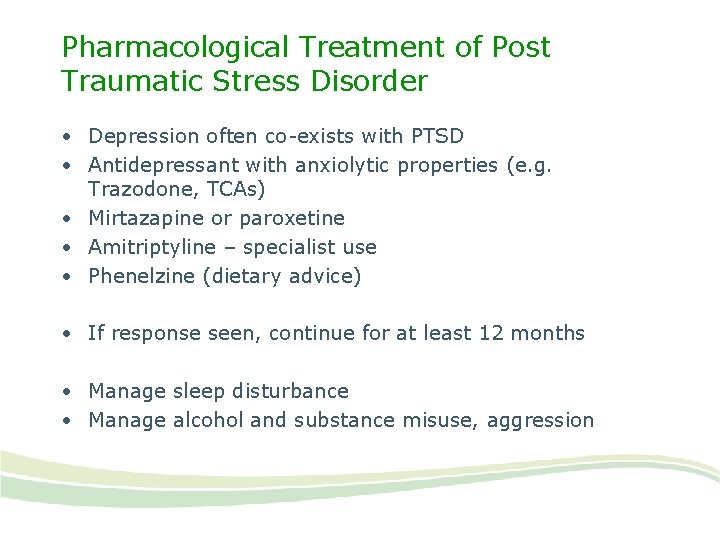
Pharmacological Treatment of Post Traumatic Stress Disorder • Depression often co-exists with PTSD • Antidepressant with anxiolytic properties (e. g. Trazodone, TCAs) • Mirtazapine or paroxetine • Amitriptyline – specialist use • Phenelzine (dietary advice) • If response seen, continue for at least 12 months • Manage sleep disturbance • Manage alcohol and substance misuse, aggression
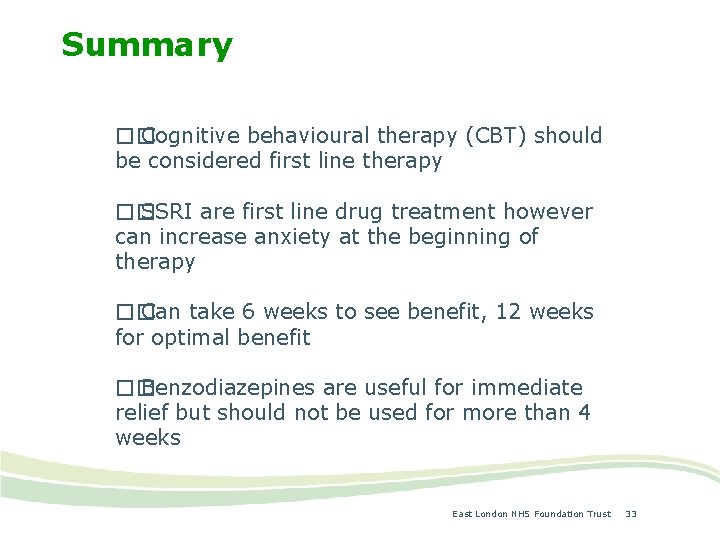
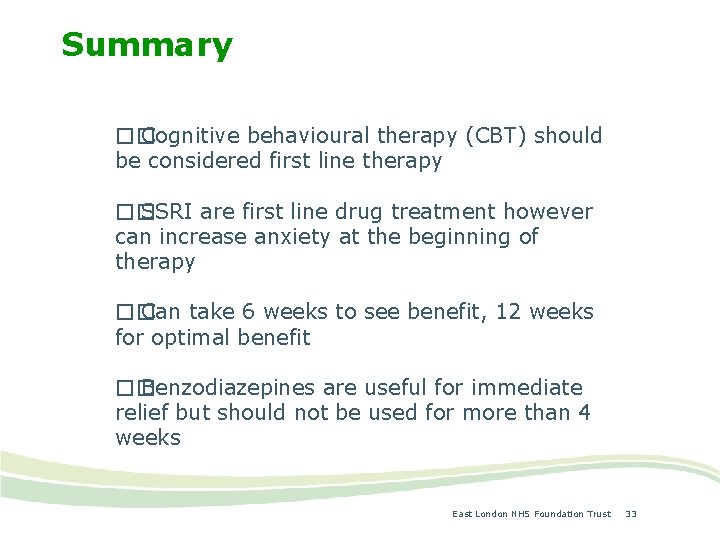
Summary �� Cognitive behavioural therapy (CBT) should be considered first line therapy �� SSRI are first line drug treatment however can increase anxiety at the beginning of therapy �� Can take 6 weeks to see benefit, 12 weeks for optimal benefit �� Benzodiazepines are useful for immediate relief but should not be used for more than 4 weeks East London NHS Foundation Trust 33
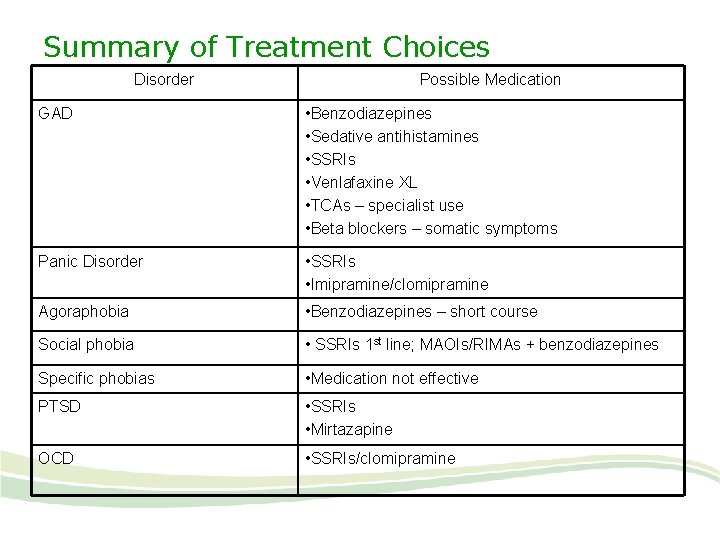
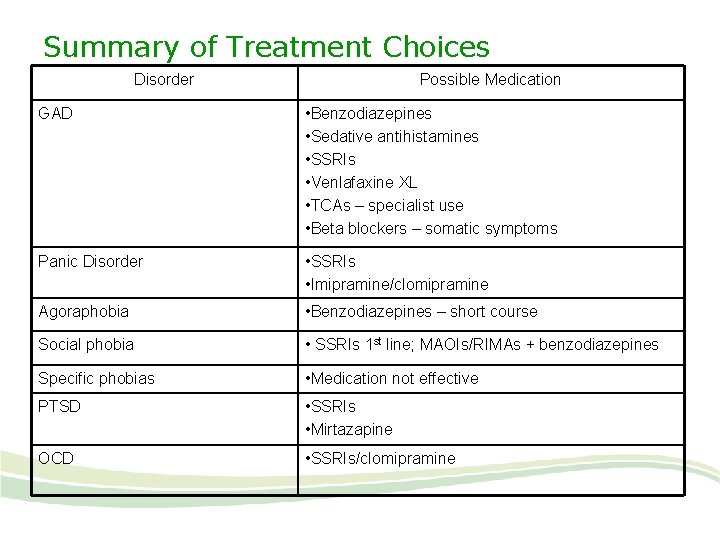
Summary of Treatment Choices Disorder Possible Medication GAD • Benzodiazepines • Sedative antihistamines • SSRIs • Venlafaxine XL • TCAs – specialist use • Beta blockers – somatic symptoms Panic Disorder • SSRIs • Imipramine/clomipramine Agoraphobia • Benzodiazepines – short course Social phobia • SSRIs 1 st line; MAOIs/RIMAs + benzodiazepines Specific phobias • Medication not effective PTSD • SSRIs • Mirtazapine OCD • SSRIs/clomipramine
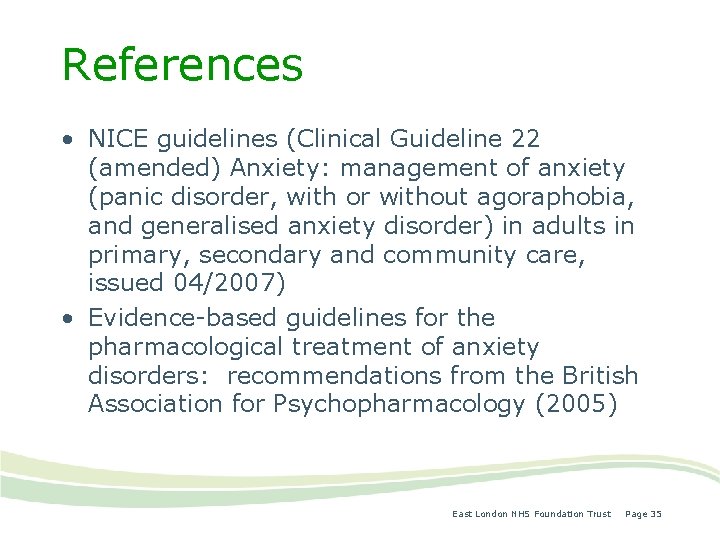
References • NICE guidelines (Clinical Guideline 22 (amended) Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care, issued 04/2007) • Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology (2005) East London NHS Foundation Trust Page 35
Thank you
 Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Anxiety disorders def
Anxiety disorders def Icd 10 cemas
Icd 10 cemas Multipath model of anxiety disorders
Multipath model of anxiety disorders Nhs community pharmacy contractual framework
Nhs community pharmacy contractual framework North east nhs
North east nhs Nhs north east hampshire and farnham ccg
Nhs north east hampshire and farnham ccg Process governance
Process governance London specialist pharmacy
London specialist pharmacy Outer north east london
Outer north east london Orthopaedic surgery south east london
Orthopaedic surgery south east london East london port
East london port East london housing partnership
East london housing partnership South east london stp
South east london stp East cantonments pharmacy
East cantonments pharmacy Wind is horizontal movement of air
Wind is horizontal movement of air Kalahari desert on africa map
Kalahari desert on africa map East is east and west is west
East is east and west is west Shallow pad foundation
Shallow pad foundation Composition of urine slideshare
Composition of urine slideshare East syracuse police department
East syracuse police department How anxiety affects eyewitness testimony
How anxiety affects eyewitness testimony Relaxation techniques test anxiety
Relaxation techniques test anxiety Anxiety symptoms
Anxiety symptoms I'm a perfect example of someone who has math anxiety
I'm a perfect example of someone who has math anxiety Neurotic anxiety example
Neurotic anxiety example Define neurotic
Define neurotic Anxiety disorder nursing diagnosis
Anxiety disorder nursing diagnosis Examples of generalized anxiety disorder
Examples of generalized anxiety disorder Chapter 8 managing stress and anxiety
Chapter 8 managing stress and anxiety Free floating anxiety
Free floating anxiety Ocd prevalence
Ocd prevalence University of wisconsin integrative medicine anxiety
University of wisconsin integrative medicine anxiety Astrid zamora
Astrid zamora Frustration anxiety and tension
Frustration anxiety and tension Mecbal
Mecbal Generalized anxiety disorder dsm 5
Generalized anxiety disorder dsm 5