Advance Directives Overcoming Completion Hurdles in a Family
- Slides: 46
Advance Directives: Overcoming Completion Hurdles in a Family Medicine Residency Clinic Baylor Family Medicine Residency at Garland Stephanie Cudjoe, MD Mojdeh Zahedi, MD Shashi Mittal, MD Kathleen Bennett, LSW
Objectives n Background of Advance directives n Impact on Residency Programs n Quality Improvement Study n Results n Discussion
What is an Advance Directive? n A document that tells physicians and ancillary staff the treatment preferences desired in the event of a critical illness. n Activated when a patient is deemed terminally ill or to have an irreversible illness/condition by a physician.
End of Life Decision Making n Advance Directives n n Living will Durable Power of Attorney for healthcare n Resuscitative Efforts (AD ≠ DNR) n Withholding/withdrawing life-sustaining therapies n Critical. Care Nurse Vol 25, No. 6 Dec 2005.
Advance Directives n lawyer is not required to complete n can be modified at anytime by the patient. n Cannot be overridden by anyone else except the patient in sound mind
Why do a Study on Advance Directives Completion? n The Patient Self Determination Act 1991 n Decreased futile care n Less ethical dilemmas n Less suffering n Increased quality of life n Improved comfort at the end of life n Completion rates of advanced directives remain low nationwide despite an aging American population Hospice Foundation of America
Effect on Medicare n A majority of patients aged 65 y or older has some form of medicare n 2001 - $63 of the $242 billion medicare budget was spent on care given during the last 12 months of life. n $34 billion – last 2 months of life C Hogan, J Lunney, J Gabel, and J Lyn. Medicare beneficiaries; costs of care in the last year of life. Health Affairs, July/August 2001; 20(4): 188 -195.
ICU Cure Mentality n 46% of patients without completed AD spent their last 3 days of life on a mechanical ventilator in the SUPPORT trial n Antibiotics n IV pressor support JAMA 1995; 274: 1591 -8
Patient Barriers n Vague language of currently n n printed AD forms Lack of communication between patients and their surrogates. Medical/legal concerns Anticipated disagreements between doctors and the patient / family Timing – is it too late? n Cultural beliefs n Family will be upset by the planning process n Fear of burdening family members n General discomfort /apathy with the topic n Procrastination Hospice Foundation of America
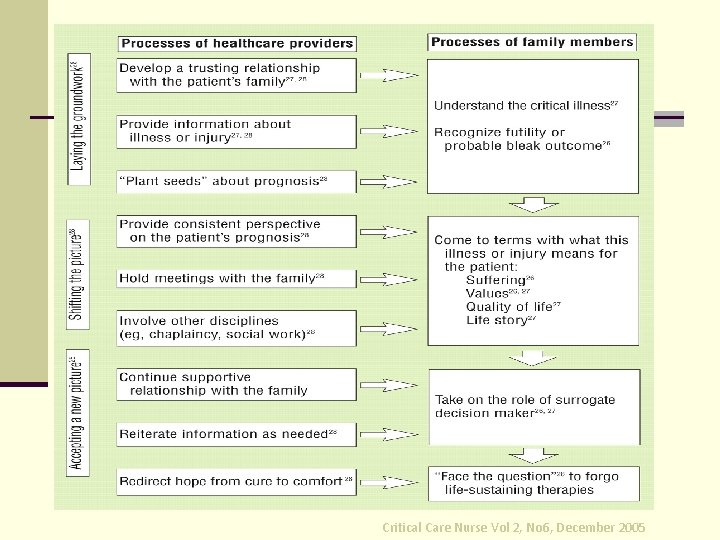
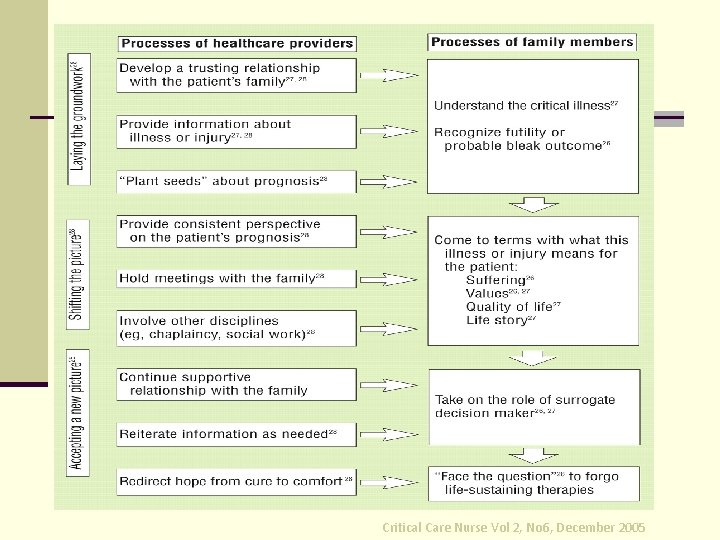
Critical Care Nurse Vol 2, No 6, December 2005
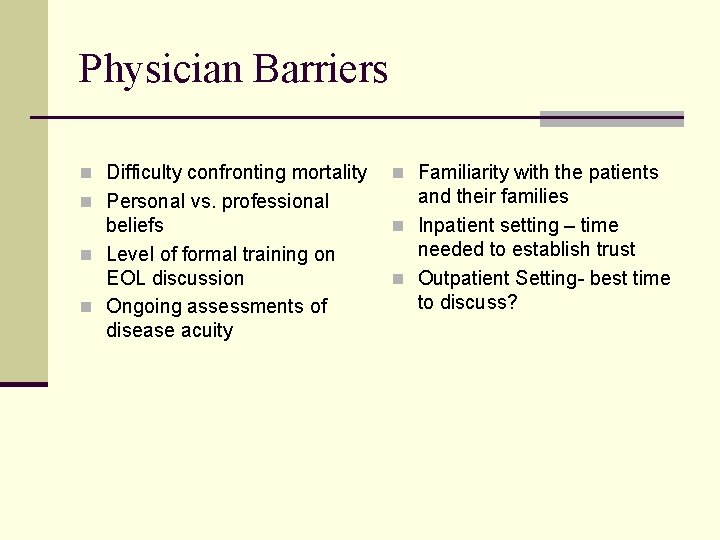
Physician Barriers n Difficulty confronting mortality n Familiarity with the patients n Personal vs. professional and their families n Inpatient setting – time needed to establish trust n Outpatient Setting- best time to discuss? beliefs n Level of formal training on EOL discussion n Ongoing assessments of disease acuity
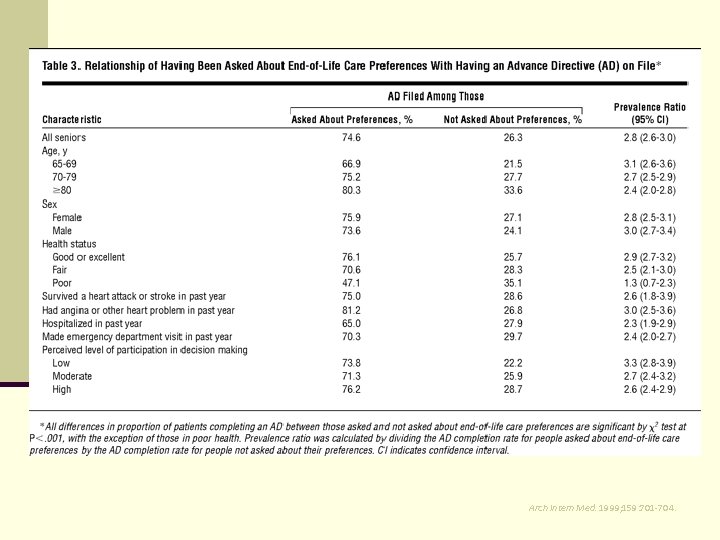
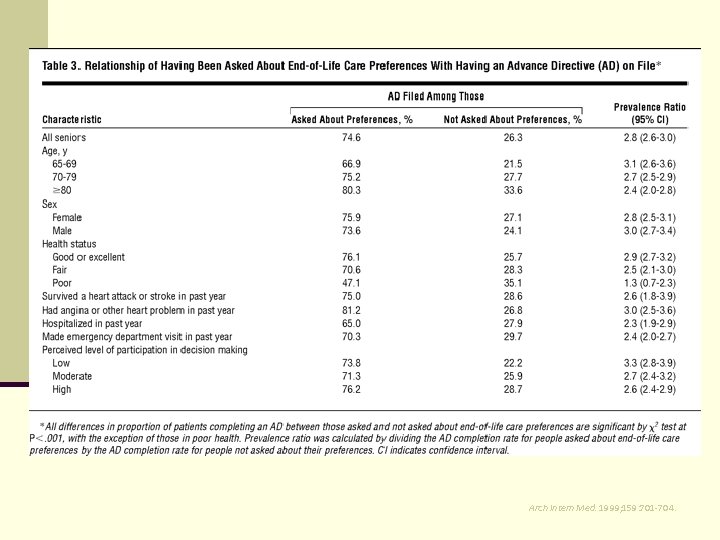
Arch Intern Med. 1999; 159: 701 -704.
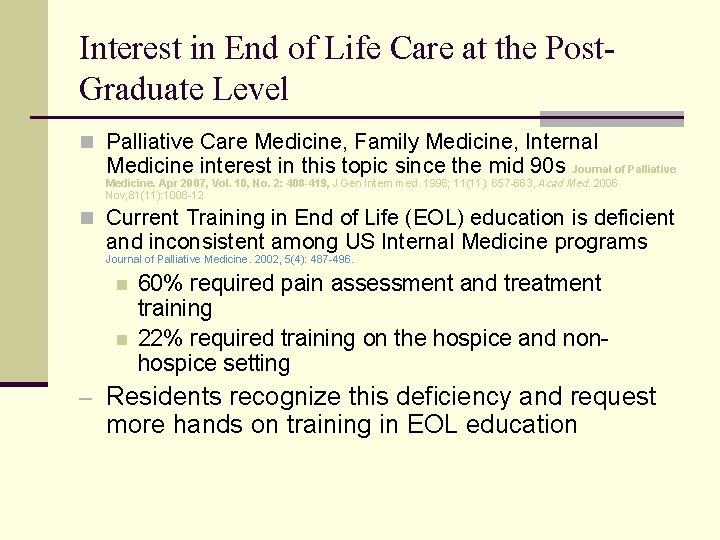
Interest in End of Life Care at the Post. Graduate Level n Palliative Care Medicine, Family Medicine, Internal Medicine interest in this topic since the mid 90 s Journal of Palliative Medicine. Apr 2007, Vol. 10, No. 2: 408 -419, J Gen Intern med. 1996; 11(11): 657 -663, Acad Med. 2006 Nov; 81(11): 1008 -12 n Current Training in End of Life (EOL) education is deficient and inconsistent among US Internal Medicine programs Journal of Palliative Medicine. 2002, 5(4): 487 -496. n n 60% required pain assessment and treatment training 22% required training on the hospice and nonhospice setting – Residents recognize this deficiency and request more hands on training in EOL education
Residency Curriculum on End of Life Issues n Schwartz et al. n 37% of New York City FM residents believed they received “little or no” support or precepting in end of life care n Stevens et al. n 79% of residents in the critical care setting believed they received “none” or “too little” instruction in how to lead an end of life discussion before their ICU rotation. n During the ICU rotation, the residents felt “unsupported” and “without role models” in leading EOL discussions
Residency Barriers to Use of Advance Directives n Morison et al. - Questionairres sent to 460 IM residents and attendings in New York, NY 1. 2. 3. 4. 5. Lack of understanding Beliefs about appropriateness Time constraints Discomfort with the subject Compensation concerns n Although supportive of the concept of AD, minimal use of AD was reported in appropriate situations Arch Intern Med. October 24, 1994; 154 (20) , Journal of Palliative Medicine. 2006, 9(4): 964 -967.
Baylor Family Medicine Residency Program at Garland n n Suburban community northeast of Dallas, Tx 17 residents 6 faculty ~40% Medicare population
Methodology
AIM n Increase knowledge and awareness of Advanced Medical Planning (AMP) among physicians at Baylor Medical Center in Garland (BMCG) and among residents of Baylor Family Medicine Residency at Garland (BFMRP), Texas. n Provide education to patients of BFMRP and people in the community regarding AMP. n To evaluate the impact of reminders and increased patient and physician education about AMP on completion of advanced directives (AD) at Baylor Family Medicine Residency Program in Garland, Texas (BFMRP).
Design n A Practice Improvement Project n Outcome: -- The number of completed AD at BFMRP -- Awareness and knowledge regarding AMP among medical staff, nurses and residents of the Baylor Family Medicine Residency Program.
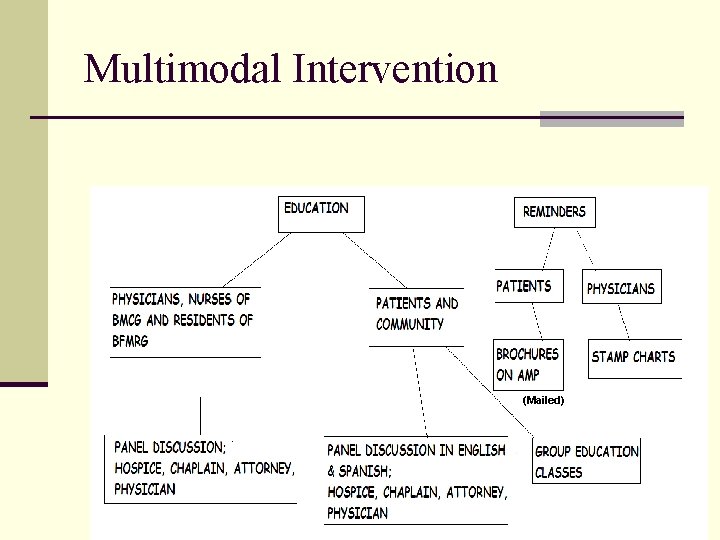
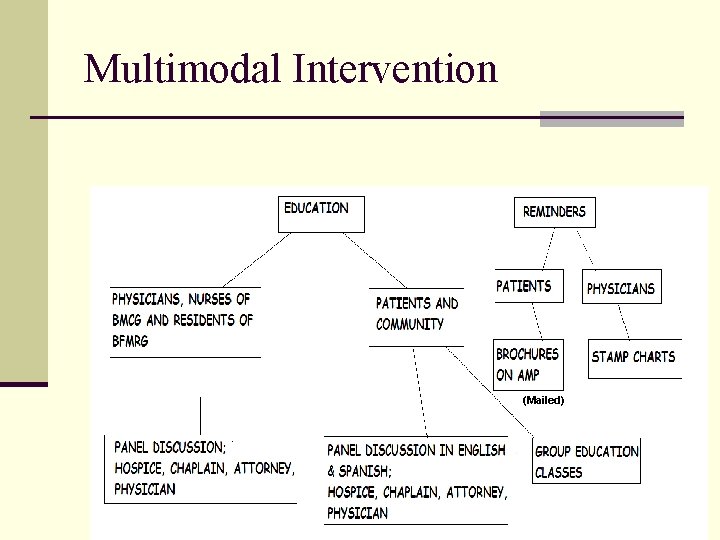
Multimodal Intervention (Mailed)
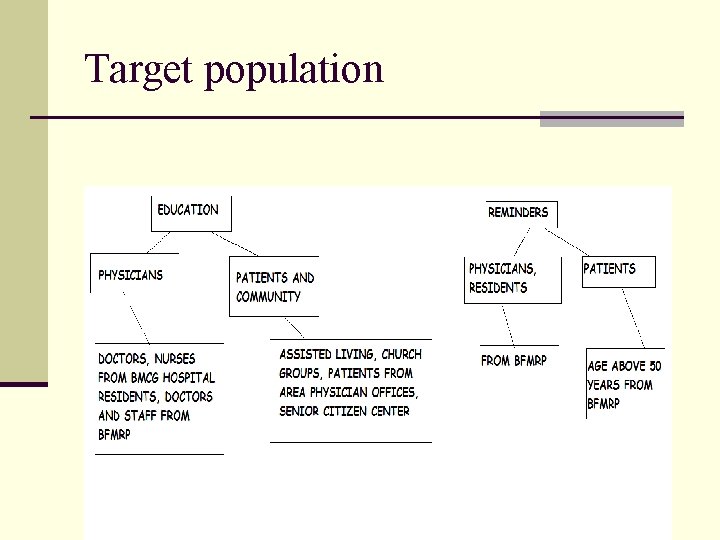
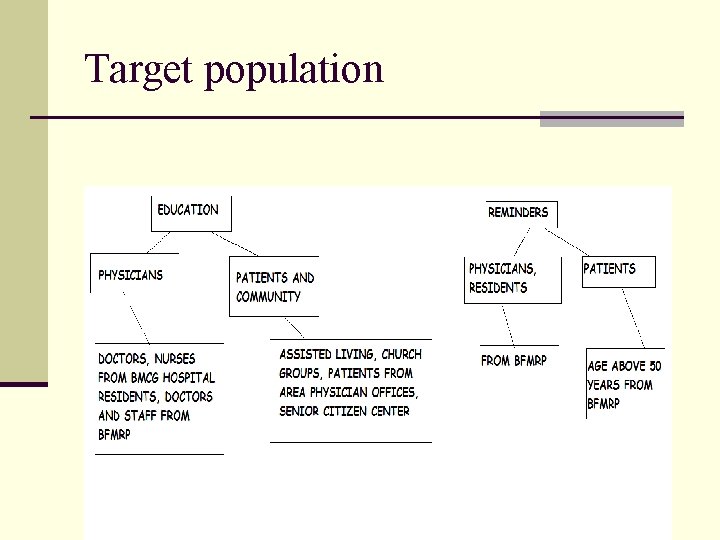
Target population
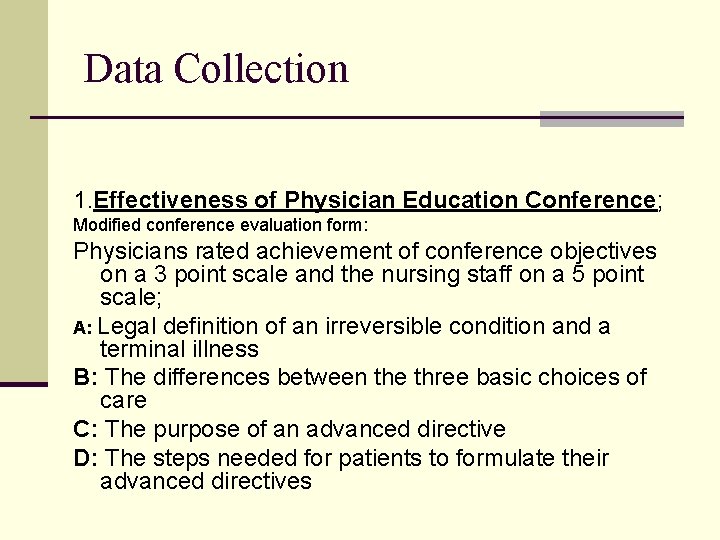
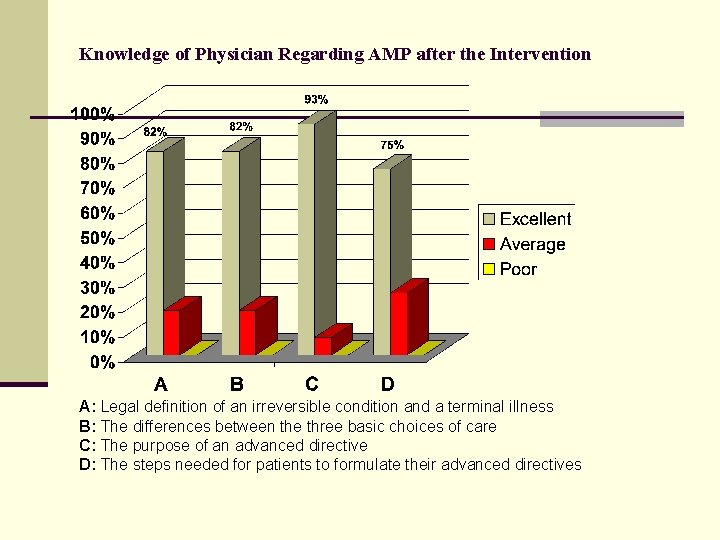
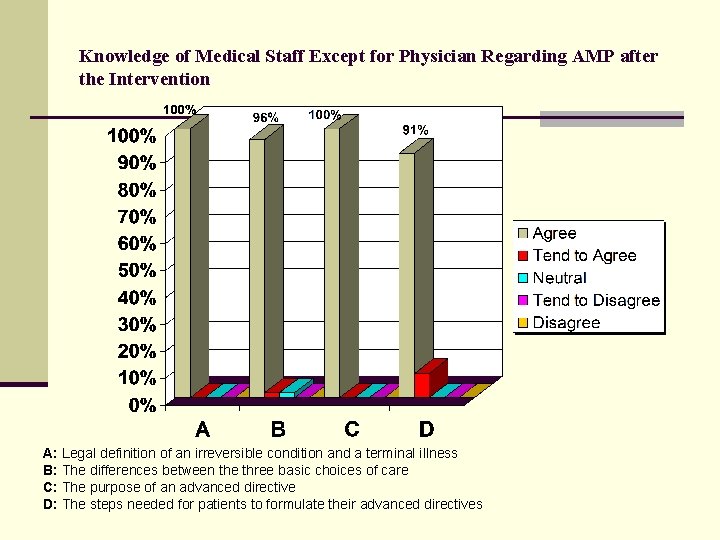
Data Collection 1. Effectiveness of Physician Education Conference; Modified conference evaluation form: Physicians rated achievement of conference objectives on a 3 point scale and the nursing staff on a 5 point scale; A: Legal definition of an irreversible condition and a terminal illness B: The differences between the three basic choices of care C: The purpose of an advanced directive D: The steps needed for patients to formulate their advanced directives
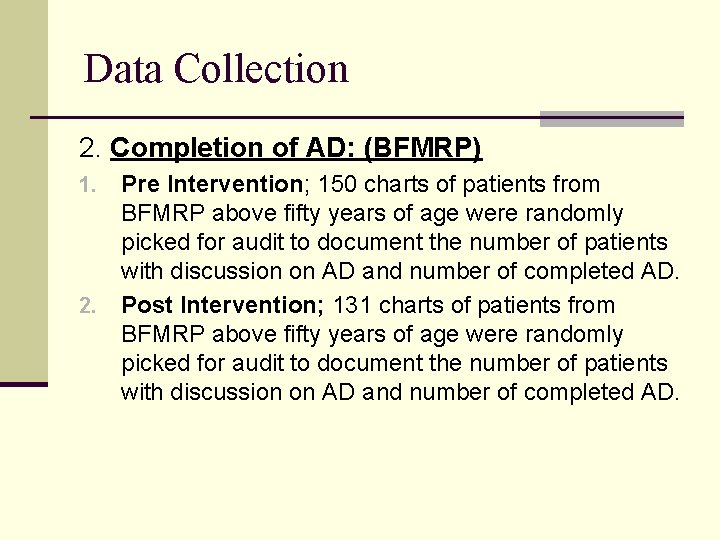
Data Collection 2. Completion of AD: (BFMRP) Pre Intervention; 150 charts of patients from BFMRP above fifty years of age were randomly picked for audit to document the number of patients with discussion on AD and number of completed AD. 2. Post Intervention; 131 charts of patients from BFMRP above fifty years of age were randomly picked for audit to document the number of patients with discussion on AD and number of completed AD. 1.
RESULTS
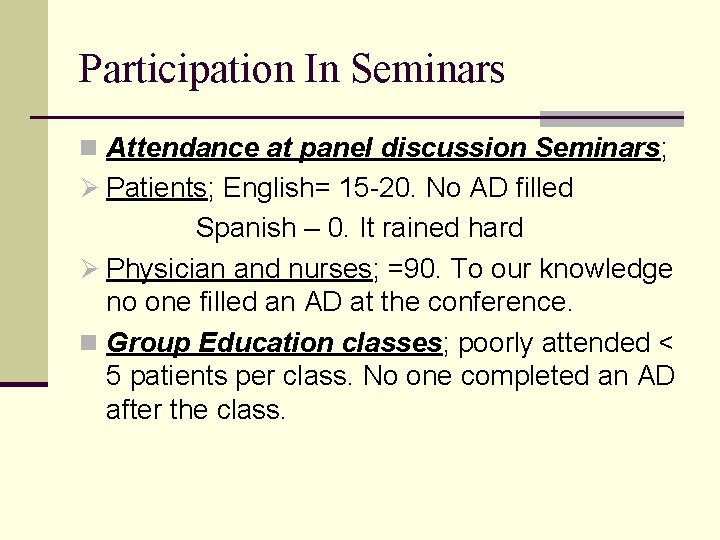
Participation In Seminars n Attendance at panel discussion Seminars; Ø Patients; English= 15 -20. No AD filled Spanish – 0. It rained hard Ø Physician and nurses; =90. To our knowledge no one filled an AD at the conference. n Group Education classes; poorly attended < 5 patients per class. No one completed an AD after the class.
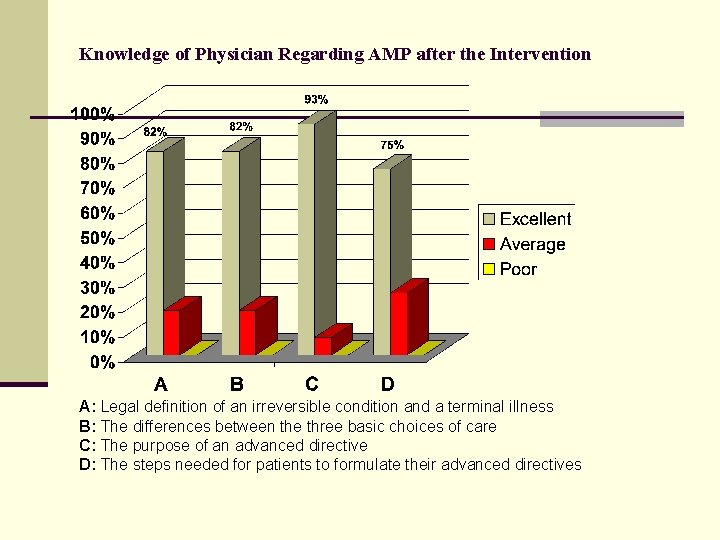
Knowledge of Physician Regarding AMP after the Intervention A: Legal definition of an irreversible condition and a terminal illness B: The differences between the three basic choices of care C: The purpose of an advanced directive D: The steps needed for patients to formulate their advanced directives
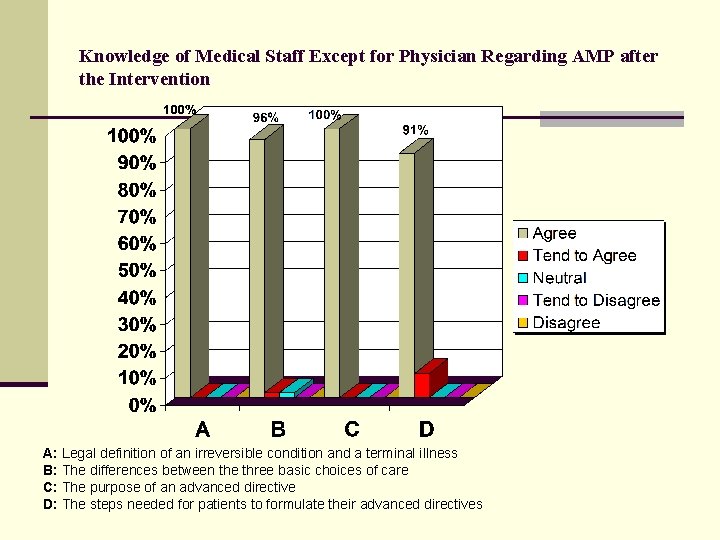
Knowledge of Medical Staff Except for Physician Regarding AMP after the Intervention A: Legal definition of an irreversible condition and a terminal illness B: The differences between the three basic choices of care C: The purpose of an advanced directive D: The steps needed for patients to formulate their advanced directives
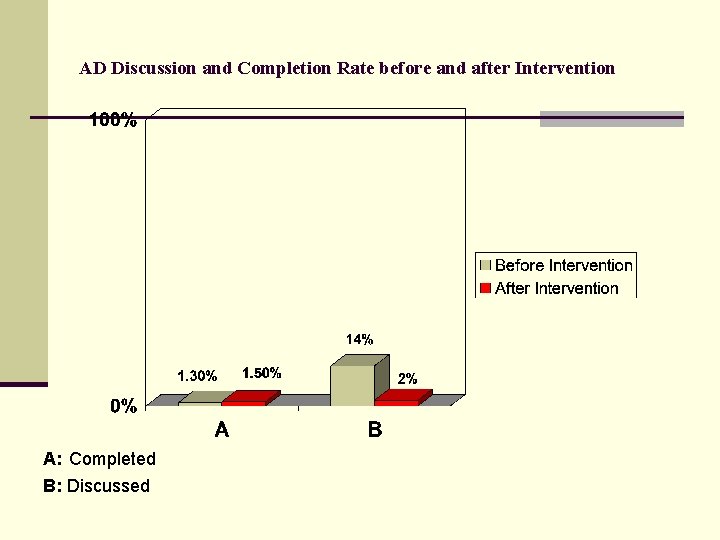
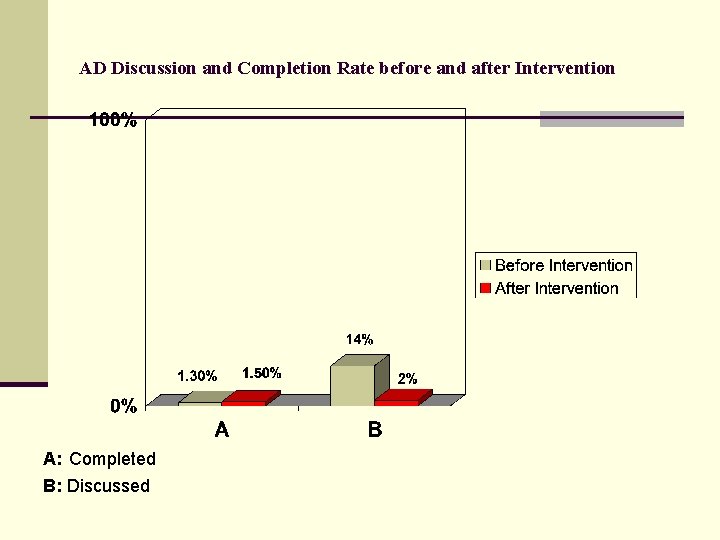
AD Discussion and Completion Rate before and after Intervention A: Completed B: Discussed
DISCUSSION
Effectiveness of Seminars n This suggests that the conference was effective in providing cognitive skills to physicians, residents and nurses. n Compares with other studies which have shown improvement in DNR discussions even when residents receive short didactics on end of life care. ( Acad Med, 2006 Nov; 81(11): 1008 -12. ) n Other factors such as physician attitude (comfort), communication and affective skills are also key when counseling patients on AD. These were not addressed in the seminar. (Acad Med, 2005 Jul; 80(7): 622 -633).
Participation in seminars Ø Doctors, residents and nurses; Good show suggests possible: - interest within medical community concerning AMP. Ø Patients; Fair participation in English panel discussion seminar but very poor patient participation in the group education classes - lack of interest - procrastination, - lack of transport
Completion of AD Ø This study did not show any significant improvement in completion of AD or increase in discussions on AD. Ø Several factors contributed to this - Few charts had stamp reminders - Physician and residents failed to discuss AD even when reminders were present - Patients failed to question their doctors on AD even after receiving mailed reminders.
Ø Our study was not successful in providing counseling to patients both in the group and individual setting. Ø Prior research has shown that passive education using written material without direct interaction with a provider or an opportunity to ask questions did not increase completion rates on AD in primary care settings. (systematic review. J Am Geriatr Soc, 2007 Feb; 55(2): 277 -283)
n Sulmasy et al had similar results in a study conducted in an Internal Medicine residency program. Patient education was combined with resident education which failed to show increase in AD completion rates between intervention and control groups over a 18 month period. n Further suggesting that perhaps the usual interventions are not effective for AD completion in residency programs. (J Gen Intern med. 1996; 11(11): 657 -663).
Hurdles to completion n Nursing issues; There was poor buy-in from the nurses to stamp the charts of patients above 50 yrs of age to remind physicians to discuss AD with the patients; possibly due to - increased staff turnover - time constraints - Gave AD lower importance when other acute issues were present at the visit.
HURDLES n Resident and physician issues Failed to discuss AD with patients; possibly because; Ø Ø Ø Time constraints. Pressure to increase productivity which may relate to time constraints. Lack of continuity relationship. Poor communication skills and comfort with such discussions. Perhaps they are unsure of the natural progression of disease process and wait to discuss these issues when the disease is further in its course or when patient is terminal. There may be hesitation to discuss AD in healthy patients.
n Several of these barriers have been identified by other researchers including time constraints, poor communication skills, lack of comfort and lack of continuity relationships. (systematic review. J Am Geriatr Soc, 2007 Feb; 55(2): 277 -283) n Patients want their doctors to initiate AMP while they are in good health and at an earlier stage of the disease. (Nurse pract. 2003; 28: 38 -47), (Arch intn Med 1995; 155: 1025 -1030) n Well known media cases were reported in young previously healthy patients. ( Terry Schiavo). n A Systematic review showed that completion rate of AD was similar among pts with chronic illness compared to those with terminal illness. (J Crit care. 2004 Mar; 19(1): 1 -9)
Other Hurdles n Too short a time for intervention studies have shown multiple physician-provider interactions to be more effective in completing AD. (J Am Geriatr Soc, 2007 Feb; 55(2): 277 -283) n Patient Factors - Denial - Procrastination - Fear of not getting good medical care once AD is in place. (Myths) Others have noted similar patient barriers. (systematic review. J Am Geriatr Soc, 2007 Feb; 55(2): 277 -283), (Nurs Pract. 2007 Aug; 38, 39: 41 -43)
PUZZLING FINDINGS n Poor patient interest and attendance in educational classes; Ø Possibly lack of transportation, not wanting to miss work or laying that responsibility on the physician may have contributed. Ø Prior research has shown that patients would like their physicians to discuss AD and feel it is the physicians responsibility to initiate such discussion. (Nurse pract. 2003; 28: 38 -47), (Arch intn Med 1995; 155: 1025 -1030)
LIMITATIONS Ø Patient education material and reminders were sent to all patients above 50 yrs of age who had been seen in the clinic in the last 6 months and not to patient who had appointments coming up. Ø We looked for chart stamps to determine if AD was discussed or completed. It is possible that Physicians had discussed AD and documented the same in their progress notes leading to underestimation. Ø We did not evaluate knowledge of physicians and nurses with pre and post conference tests.
IMPLICATIONS n Need formal curriculum in residency programs. n Incorporate a culture that promotes discussions. n Incentives to physician in form of reimbursement for individual and group counseling on AD. n Incorporate AD discussions into guidelines of management of chronic disease and or health maintenance as an essential element. n Enhanced educational messages in the media on AD to improve pt awareness.
CONCLUSION n Our study suggests that the medical community has interest in learning about AD and probably possess the cognitive skills to counsel patients. n We were surprised to find that our patients interest in education on AD topics was low. n Although we were unable to document increased AD discussion and completion rates we provide valuable insight into future intervention studies on AD, in residency programs.
FUTURE PDSA cycles n More structured and frequent short didactics for residents to include role playing. n structured scripts to assist discussions. n Medical assistant & nurses team players; Frequent short in services and reminders to stamp charts during their weekly meetings.
REFERENCES 1. Ramsaroop S, et al. Completing an Advanced Directive in the Primary care setting: what do we need for success? J Am Geriatr Soc, 2007 Feb; 55(2): 277 -283). 2. Patel R, Sinuff T, Cook D. Influencing advanced directive completion rates in non-terminally ill patients: a systematic review. J Crit care. 2004 Mar; 19(1): 1 -9 3. Alexander SC, et al. A controlled trial of a short course to improve residents’ communication with patients at the end of life. Acad Med, 2006 Nov; 81(11): 1008 -12. 4. Gorman T, et al. Residents’ End-of life decision making with adult hospitalized Patients: A review of the literature. Acad Med, 2005 Jul; 80(7): 622 -633 5. Maxfield CL, et al. Advanced directives. A guide for patient discussion. Nurse pract. 2003; 28: 38 -47. 6. Roessel L. Protecting your patients rights with Advanced Directives. Nurs Pract. 2007 Aug; 38, 39: 41 -43 7. Johnston SC, et al. The discussion about advance directives: Patient and physician opinions regarding when and how it should be conducted. Arch intern Med 1995; 155: 1025 -1030
References n n n The SUPPORT Principle Investigators. A controlled trial to improve care for seriously ill hospitalzed patients: the study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA 1995; 274: 1591 -8[Published erratum in JAMA 1996; 175: 1232. http: //www. hospicefoundation. org/end. Of. Life. Info/Ivd. asp Critical. Care Nurse Vol 25, No. 6 Dec 2005. C Hogan, J Lunney, J Gabel, and J Lyn. Medicare beneficiaries; costs of care in the last year of life. Health Affairs, July/August 2001; 20(4): 188 -195. David E. Weissman, Bruce Ambuel, Charles F. Von Gunten, Susan Block, Eric Warm, James Hallenbeck, Robert Milch, Karen Brasel, Patricia B. Mullan Journal of Palliative Medicine. Apr 2007, Vol. 10, No. 2: 408 -419 J Gen Intern med. 1996; 11(11): 657 -663. n n n n Strategies to promote the use of advance directives in a residency outpatient practice. Acad Med. 2006 Nov; 81(11): 1008 -12 Arch Intern Med. 1999; 159: 701 -704. Patricia B. Mullan, David E. Weissman, Bruce Ambuel, Charles von Gunten. Journal of Palliative Medicine. 2002, 5(4): 487 -496. Arch Intern Med. October 24, 1994; 154 (20) Christian Davis Furman, Barbara Head, Bonnie Lazor, Barbara Casper, Christine Seel Ritchie. Journal of Palliative Medicine. 2006, 9(4): 964 -967. Acad Med. 2005 Jul; 80(7): 622 -33 CMAJ • November 14, 2000; 163 (10)
QUESTIONS? SUGGESTIONS
 Disadvantages of advance directives
Disadvantages of advance directives What are the types of advance directives
What are the types of advance directives Advance directives
Advance directives What are the types of advance directives
What are the types of advance directives 4 hurdles of causality
4 hurdles of causality Professor roz shafran
Professor roz shafran Coalescing and compaction in os
Coalescing and compaction in os Overcoming glossophobia
Overcoming glossophobia Words with literal and figurative meanings
Words with literal and figurative meanings Overcoming trials and temptations
Overcoming trials and temptations I'd rather take baths with a man-eating shark
I'd rather take baths with a man-eating shark Overcoming life issues
Overcoming life issues Overcoming the dark side of leadership
Overcoming the dark side of leadership Overcoming the monster examples
Overcoming the monster examples Overcoming hindrances to spiritual development
Overcoming hindrances to spiritual development Major hurdles of pipelining
Major hurdles of pipelining Organizational hurdles
Organizational hurdles Writing a narrative about overcoming a challenge
Writing a narrative about overcoming a challenge Overcoming barriers to employment
Overcoming barriers to employment How did helen keller overcome adversity
How did helen keller overcome adversity Overcoming communication barriers in pharmacy
Overcoming communication barriers in pharmacy Political hurdle
Political hurdle Overcoming challenges essay
Overcoming challenges essay Scripture about overcoming adversity
Scripture about overcoming adversity Iec directives
Iec directives Simple sic assembler
Simple sic assembler Ce directives
Ce directives Mike towr
Mike towr Page directive in jsp
Page directive in jsp Fsis directives
Fsis directives What is assembler directives in 8086 microprocessor
What is assembler directives in 8086 microprocessor New approach directives
New approach directives Forest service office of tribal relations
Forest service office of tribal relations Brigade staff
Brigade staff Advanced assembler directives in system programming
Advanced assembler directives in system programming Directive control examples
Directive control examples Personal directives act
Personal directives act Assembly language programming
Assembly language programming Assembly language programming 8051
Assembly language programming 8051 What is discrimination
What is discrimination Ptr operator in assembly language
Ptr operator in assembly language Aabe ethiopia website
Aabe ethiopia website Completion problem effect
Completion problem effect Matrix completion
Matrix completion Subsea well completion
Subsea well completion Difference between bore hole latrine and dug well latrine
Difference between bore hole latrine and dug well latrine Ba_ba_bac_acb_cbac
Ba_ba_bac_acb_cbac